Abstract
After the outbreak of COVID-19, many dental clinics use dry fogging of hydrogen peroxide (H2O2) to disinfect the air and surfaces. Inhalation of highly concentrated solutions of H2O2 may cause severe respiratory problems. This study aimed to estimate the health risk assessments of inhalation exposure to dry fogging of H2O2 in a dental clinic. This cross-sectional, descriptive-analytical study was performed to determine the inhalation exposure and health risk of 9 dental clinic staff with H2O2 in six rooms. Occupational exposure to H2O2 was assessed using the OSHA VI-6 method and a personal pump with the flow rate of 500 mL/min connected to the midget fritted-glass impinger containing 15 mL of TiOSO4 collecting solution. The health effects of H2O2 exposure were assessed using a respiratory symptoms questionnaire. The health risk assessment of inhaled exposure to H2O2 was also performed using the method provided by the Singapore occupational health department. The mean respiratory exposure of clinic staff to H2O2 was ranged from 1.3 to 2.83 ppm for six rooms which was above the limits recommended by international organizations. Dyspnea (44.4%), cough (33.3%), and nasal burning (22.2%) were the most prevalent health problems. The results also showed a medium risk for endodontics and surgery, and lower risk for periodontics, restorative care, orthodontics, and prosthetics. The results of this study indicate that when using an automated hydrogen peroxide–vapor fogger, calculating the spraying time based on room volume and using the rooms after 30 min of fogging is very important and can greatly reduce the risk ranking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In late 2019, the outbreak of COVID-19 caused by SARS-CoV2 in Wuhan, China was reported and spread rapidly around the world. SARS-CoV2 is a member of the β-corona family of viruses that affects pulmonary gas exchange and triggers cytokine storm. Severe inflammation, excessive coagulation, decreased lymphocyte count, and the increased neutrophil count are seen in the second week after the onset of the disease. Fever, dry cough, sneezing, shortness of breath, and respiratory distress are symptoms of COVID-19 (Noureen et al. 2022). Among the patients, men, the elderly, and those who have a variety of clinical problems such as cardiovascular disease and diabetic mellitus are at higher risk (Qureshi et al. 2021).
Preliminary studies have shown that the virus infects people through the inhalation route, directly/ indirectly (Peng et al. 2020). At direct exposure, the person exposes to the respiratory droplets released from the infected person. At indirect exposure, the person contacts to the infected surfaces (Barbato et al. 2020).
Due to their small size, respiratory droplets can remain suspended in the air for a long time. To prevent the transmission of the virus, it is necessary to disinfect the indoor air and surfaces. Air and surface disinfection systems were widely used in the COVID-19 pandemic. These systems disinfect the environment by spraying or fumigating disinfectants into the air (Raeiszadeh &Adeli 2020). Many public places such as restaurants, hotels, airports, stores, and hospitals have used these systems to control COVID-19 (Kimball et al. 2014).
Dry fogging is one of the methods that use compressed air for atomizing the disinfectant liquid into the air. The generated very small droplets can remain suspended in the indoor atmosphere for a long time, causing a higher disinfection rate (Bhandare &Goodridge 2021, Krishnan et al. 2012). Dry fogging with H2O2 has been used in various sectors including laboratories, biotech food production, and healthcare in recent years (Krishnan et al. 2012; Møretrø et al. 2019). However, the outbreak of the novel coronavirus sparked the need for this technology to be used in many other public facilities, such as airports, train stations, hospitals, and malls (Kaklauskas et al. 2021). Because the ultrafine droplet of the dry fog remains in the air for hours, there is a possibility of respiratory exposure to H2O2. Exposure to lower concentrations of H2O2 leads to coughing and transient dyspnea, while severe irritation, inflammation of mucous membranes, coughing and dyspnea appear at higher levels. Shock, coma, convulsions, and pulmonary edema may occur up to 24–72 h post-exposure (Advenier &de la Grandmaison 2018, Watt et al. 2004). Chronic exposure to lower levels of H2O2 in the workplace may result in chronic disorders such as chronic bronchitis, fibrosis, and lung cancer (Rahimi 2021).
Due to the patient’s open oral cavity, instruments contact with saliva, blood, and other body fluids, many dental clinics use dry fogging to disinfect the air and surfaces (Manea et al. 2021; Miglani et al. 2020, Sher &Mulder 2020). Given the adverse effects of H2O2 on health care workers, assessing the health risk of respiratory exposure to H2O2 in the COVID-19 pandemic is essential. Health risk assessment as a monitoring tool is used to estimate the probability of adverse effects on the health of a group of people over a time (Atamaleki et al. 2021; Behrooz et al. 2021). To our knowledge, no study has been performed to evaluate the health effects of respiratory exposure to H2O2 emitted by dry fog in the workplaces. Accordingly, the present study was conducted to assess the respiratory exposure of dental clinic staff to H2O2. Moreover, the health risk of respiratory exposure and the control strategies are estimated.
Materials and methods
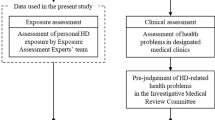
Study information
This cross-sectional, descriptive-analytical study was performed in one of the dental clinics in Tehran, Iran. The clinic has 9 staff members working in 7 rooms of endodontics, periodontics, orthodontics, prosthetics, restorative care, and surgery.
The air and surface of rooms were disinfected using the automated hydrogen peroxide vapor fogger (Nocospray: Oxypharm, France). Disinfection was performed before each patient’s visit. For this purpose, the vapor fogger is turned on for 4 min in an empty, enclosed room. The clinic does not have a heating, ventilation, and air conditioning (HVAC) system. The cooling system was also turned off because the study was conducted in the cold season. For disinfection to occur, it is recommended a minimum contact time of 30 min which was not considered due to a large number of patients.
Sample collection and analysis
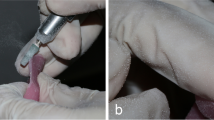
To determine the clinic staff’s exposure to H2O2, personal air sampling was performed after the dental clinic staff entered the room. Since the sampling period was 30 min, air sampling was performed at 0 to 30, 30 to 60, 60 to 90, and 90 to 120 min. The OSHA VI-6 method was used to measure H2O2 concentrations in the rooms (OSHA 1978). Samples were collected from the respiratory area of the clinic staff by drawing air through a midget fritted-glass impinger containing 15 mL of TiOSO4 collecting solution. A blank sample was also considered for each room. Sampling pumps were calibrated at approximately 500 mL/min before and after sampling with a digital calibrator. The H2O2 concentration of the sample is determined by the UV–vis spectrophotometer (Agilent, USA) set at 410 nm (Moradpour et al. 2021; OSHA 1978).
Determination of respiratory complaints
The respiratory symptoms questionnaire provided by the American Thoracic Society (ATS) was used to assess the health effects of H2O2 exposure (Jalali et al. 2021). The ATS questionnaire is an 8-item query about the respiratory status (coughing, wheezing, dyspnea, and chest compression), nasal, and eye burning. The two items of exercise and walking were not considered in the present study. The validity and reliability of the questionnaire have been investigated in previous studies (Cronbach’s alpha = 0.86) (Cassidy et al. 2015). Data were collected through face-to-face interviews involving clinic staff.
Health risk assessment
Semi-quantitative health risk assessment related to H2O2 was performed according to the method provided by the Singapore Occupational Health Department (ministry of manpower 2005). The risk levels were calculated based on the hazard ratings (HR) and exposure ratings (ER), as shown in Eq. (1):
The HR is assigned based on the carcinogenicity classifications established by the American Conference of Governmental Industrial Hygienists (ACGIH). ACGIH has indicated that H2O2 is a confirmed animal carcinogen with unknown relevance to human carcinogenicity (A3) (ACGIH 2021).
The ER is based on the ratio of the exposure level (E) to permissible exposure limit (PEL) or occupational exposure limit (OEL). The E was calculated using Eq. (2):
where E is the rate of weekly exposure in mg/m3 or ppm, F is the frequency of exposure per week, M is the rate of exposure in mg/m3 or ppm, D is the average duration of each exposure in terms of hours, and W is average working hours per week.
According to the ACGIH, the occupational exposure limit for H2O2 is 1 ppm. For unusual work shifts, the OEL was adjusted with Eq. (3) (Verma 2000):
where RF is the weekly reduction factor, and hr is the number of hours worked in 1 week.
The risk of occupational exposure to H2O2 was ranked using the risk level (Table 1).
Statistical analysis
Statistical analyses were performed using SPSS Version 16. All continuous data are presented as the mean ± standard deviation (SD) and median. Categorical data are presented as numbers and percentages.
Results and discussion
The occupational exposure to H2O2 in the dental clinic at different times after fogging is shown in Table 2. The time average concentration of H2O2 was in the range of 1.3 to 2.83 ppm for six rooms, which was above the exposure limit provided by the OSHA, NIOSH, ACGIH, and Iran’s national occupational exposure limit (1 ppm) (ACGIH 2021). The results showed that the highest mean individual exposure was related to endodontics (2.83 ppm) and then surgery (2.52 ppm). The lowest mean occupational exposure was also determined for periodontics (1.3 ppm).
The differences observed in the results of different rooms can be due to differences in room volume. The endodontics and surgery rooms have a volume equal to half of the periodontics, which resulted in a twice exposure. According to the manufacturer’s instructions, the spraying time should be calculated based on the volume of the room (3.6 s/m3) (Dorobanțu et al. 2015). Given this guide, spraying time is calculated to be 3.6 min for periodontics (60 m3) and 1.8 min for endodontics and surgery (30 m3). However, these calculations have not been performed, and the spraying time was considered 4 min for all the rooms. The lack of calculation for spraying time has caused the clinic staff to be exposed to the high concentration of H2O2. Fu et al. reported that the mean respiratory exposure of hospital staff with H2O2 was 1.3 ± 0.4 ppm with a maximum reading of 4.5 ppm in a 50-m3 room in St. George’s Hospital, London (Fu et al. 2012). The results of this study are in line with the results of the present study.
The health problems associated with exposure to H2O2 are presented in Table 3. Surveying about the health problems due to the exposure showed that dyspnea (44.4%), cough (33.3%), and nasal burning (22.2%) had the highest prevalence. Also, the problems were more common in endodontics and surgery rooms that had more H2O2 than others (7, 7, and 3 symptoms for endodontics, surgery, and others, respectively). Human studies have also shown that respiratory exposure to H2O2 stimulates the nose and lungs. Yang and Liu found that exposure to highly concentrated H2O2 in a short term caused chest tightness, cough, general malaise, and piercing pain in the throat, (Yang &Liu 2021). Watt et al. found that inhalation of highly concentrated solutions of H2O2 can cause severe irritation and inflammation of mucous membranes, with coughing and dyspnea (Watt et al. 2004). ACGIH has reported that exposure to hydrogen peroxide stimulates the upper respiratory tract (ACGIH 2021). The results of this study also showed coughing, dyspnea, and nasal burning are common in the clinic staff, which are symptoms associated with upper respiratory tract irritation.
The results of the health risk assessment are presented in Table 4. In terms of carcinogenicity, H2O2 is classified in group A3 in the ACGIH classification. Therefore, according to the method provided by the Singapore Occupational Health Department, HR for H2O2 is 3. The calculated ER based on 8 h of work per day and 6 days per week was compared with the adjusted permissible limit of H2O2 (0.78). The results showed the range of risk levels in the clinic staff was 2.16 to 3.19. The highest risk level was found in endodontics (3.19). The lowest risk level belonged to the periodontics (2.16). The results of risk ranking showed a medium risk for endodontics and surgery and low risk for periodontics, restorative care, orthodontics, and prosthetics (Table 3). To our knowledge, it has been found that no study has been performed to evaluate the risk of respiratory exposure to H2O2 in dental clinics. Hong et al. determined the health risk of exposure to VOCs in dental clinics. Unlike the carcinogenic compounds, methylene methacrylate (2.8 ppm) and acetone (0.176 ppm), as non-carcinogenic ones indicated higher risks for human health (Hong et al. 2015).
Given that HR is 3 for all the rooms, the factor influencing the risk level is ER. Table 2 shows the maximum exposure that occurs in the first 30 min (3.48 to 7.11 ppm). According to the manufacturer’s instructions and fogging disinfection guide, the room can be used after 30 min after fogging. In such circumstances, the estimated risk changes as shown in Table 5. The results show that if the clinic staff does not have exposure for the first 30 min, the risk ranking will change to lower rank.
One of the limitations of this work is conducting the study in only one clinic. It is expected that conducting studies in more clinics with different characteristics (HVAC, volume, exposure time, etc.) will help to better understand the personnel exposure.
Conclusion
The results of this study indicate that the dental clinic staff’s exposure to H2O2 was higher than that recommended by international organizations and leads to the problems in respiratory tracts. Although the risk ranking in this study was medium and low, following the manufacturer’s instructions and fogging disinfection guide, such as calculating the spraying time based on the room volume and using the room after 30 min of fogging, can greatly reduce the risk ranking.
Data availability
All the data generated or analyzed during this study are included in this published article.
References
ACGIH (2021): TLVs and BEIs threshold limit values for chemical substances and physical agents and biological exposure indices. American Conference of Governmental Industrial Hygienists,, Cincinnati, pp. 36
Advenier A-S, de la Grandmaison GL (2018) Pulmonary acute lesions after caustic exposure. J Lung Health Dis 2:6–9
Atamaleki A, Yazdanbakhsh A, Fallah S, Hesami M, Neshat A, Fakhri Y (2021) Accumulation of potentially harmful elements (PHEs) in lettuce (Lactuca sativa L.) and coriander (Coriandrum sativum L.) irrigated with wastewater: a systematic review and meta-analysis and probabilistic health risk assessment. Environ Sci Pollut Res 28:13072–13082
Barbato L, Bernardelli F, Braga G, Clementini M, Di Gioia C, Littarru C, Oreglia F, Raspini M, Brambilla E, Iavicoli I (2020): Surface disinfection and protective masks for SARS‐CoV‐2 and other respiratory viruses:a review by SIdP COVID‐19 task force. Oral Dis 0, 1–9
Behrooz RD, Kaskaoutis D, Grivas G, Mihalopoulos N (2021) Human health risk assessment for toxic elements in the extreme ambient dust conditions observed in Sistan. Iran Chemosphere 262:127835
Bhandare S, Goodridge L (2021) Bacteriophages as bio-sanitizers in food production and healthcare settings. Biology, Technology, Therapy, Bacteriophages, pp 769–788
Cassidy RN, Roberts ME, Colby SM (2015) Validation of a respiratory symptom questionnaire in adolescent smokers. Tobacco Regul Sci 1:121–128
Dorobanțu D, Arsene C, Lupu E, Radu A, Oltean G, Chelmuș R (2015) Disinfection air and surfaces: contemporary fine by forming a 5 mm without wetting on the basis of hydrogen peroxide–nocolyse generated by nebulizer Nocospray Procesul de dezinfectare al aerului şi suprafeţelor prin formarea unei ceţi foarte fine de 5 µm, fără umezire, pe baza de peroxid de hydrogen–nocolyse. Vet Drug 9:60–63
Fu T, Gent P, Kumar V (2012) Efficacy, efficiency and safety aspects of hydrogen peroxide vapour and aerosolized hydrogen peroxide room disinfection systems. J Hosp Infect 80:199–205
Hong Y-J, Huang Y-C, Lee I-L, Chiang C-M, Lin C, Jeng HA (2015) Assessment of volatile organic compounds and particulate matter in a dental clinic and health risks to clinic personnel. J Environ Sci Health A Environ Sci Eng 50:1205–1214
Jalali M, Moghadam SR, Baziar M, Hesam G, Moradpour Z, Zakeri HR (2021) Occupational exposure to formaldehyde, lifetime cancer probability, and hazard quotient in pathology lab employees in Iran: a quantitative risk assessment. Environ Sci Pollut Res 28:1878–1888
Kaklauskas A, Zavadskas EK, Lepkova N, Raslanas S, Dauksys K, Vetloviene I, Ubarte I (2021) Sustainable construction investment, real estate development, and COVID-19: a review of literature in the field. Sustainability 13:7420
Kimball S, Bodurtha P, Dickson EFG (2014): A roadmap for investigation and validation of dry fogging as a decontamination technology. chemistry 613, 144–161
Krishnan J, Fey G, Stansfield C, Landry L, Nguy H, Klassen S, Robertson C (2012) Evaluation of a dry fogging system for laboratory decontamination. Appl Biosaf 17:132–141
Manea A, Crisan D, Baciut G, Baciut M, Bran S, Armencea G, Crisan M, Colosi H, Colosi I, Vodnar D (2021) The importance of atmospheric microbial contamination control in dental offices: raised awareness caused by the SARS-CoV-2 pandemic. Appl Sci 11:2359
Miglani S, Ansari MI, Ahuja B, Gupta A (2020) Use of newer protective and disinfection strategies: a simple tool guide for the dentists during the COVID-19 pandemic. Int J Cur Res and Rev 12:151–154
ministry of manpower (2005): A semi-quantitative method to assess occupational exposure to harmful chemicals. In: Division oSaH (Hrsg.). ministry of manpower, Singapore
Moradpour Z, Helmi Kohnehshahri M, Vahabi Shekarloo M, Jalili V, Zendehdel R (2021) Peroxidase-like reaction by a synergistic inorganic catalyst colloid: a new method for hydrogen peroxide detecting in air samples. Colloid Polym Sci 299:1567–1575
Møretrø T, Fanebust H, Fagerlund A, Langsrud S (2019) Whole room disinfection with hydrogen peroxide mist to control Listeria monocytogenes in food industry related environments. Int J Food Microbiol 292:118–125
Noureen S, Rehman K, Akash H (2022): Natural immunity boosters as therapeutic interventions in the era of COVID-19 pandemic. Endocrine, Metabolic & Immune Disorders Drug Targets
OSHA (1978): OSHA Method No. VI-6, Hydrogen peroxide. Occupational Safety and Health Administration, Salt Lake City, Utah
Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B (2020) Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci 12:1–6
Qureshi QH, Ashraf T, Rehman K, Khosa MK, Akash MSH (2021) Therapeutic interventions of remdesivir in diabetic and nondiabetic COVID-19 patients: a prospective observational study conducted on Pakistani population. J Med Virol 93:6732–6736
Raeiszadeh M, Adeli B (2020) A critical review on ultraviolet disinfection systems against COVID-19 outbreak: applicability, validation, and safety considerations. ACS Photonics 7:2941–2951
Rahimi J (2021) Effect of hydrogen peroxide on the respiratory system of dairy industry workers. Iran Occup Health 18:341–352
Sher M, Mulder R (2020) Comparison of aerosolized hydrogen peroxide fogging with a conventional disinfection product for a dental surgery. J Contemp Dent Pract 21:1308–1311
Verma DK (2000) Adjustment of occupational exposure limits for unusual work schedules. Am Ind Hyg Assoc J 61:367–374
Watt BE, Proudfoot AT, Vale JA (2004) Hydrogen peroxide poisoning. Toxicol Rev 23:51–57
Yang X-Y, Liu H-Y (2021) Hydrogen peroxide is a risk factor for occupational chemical poisoning. Chin Med J (engl) 134:881–882
Acknowledgements
The researchers would like to acknowledge and thank the Shahid Beheshti University of Medical Sciences.
Funding
This project was approved and financially supported by Shahid Beheshti University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
Ghasem Hesam: investigation, writing original draft, and writing—review and editing. Masoomeh Vahabi Shekarloo: sampling and writing. Ali Atamaleki: writing—review, and editing. Mahdi Jalali: sampling and writing. Behnam Hajipour-Verdom: writing—review, and editing. Zahra Moradpour: investigation, writing original draft, and writing—review and editing.
Corresponding author
Ethics declarations
Ethical approval
The present study was approved by the Ethics Committee of the Shahid Beheshti University of Medical Sciences through the ethical code: IR.SBMU.RETECH.REC.1399.800.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hesam, G., Vahabi Shekarloo, M., Atamaleki, A. et al. Health risk assessment of inhalation exposure to dry fogging of hydrogen peroxide in a dental clinic during the COVID-19 pandemic. Environ Sci Pollut Res 29, 75338–75343 (2022). https://doi.org/10.1007/s11356-022-21174-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-022-21174-1