Abstract
This global level ecological study aimed to investigate the correlation between environmental factors and the COVID-19 indices. This survey is an ecological study, so all studied variables are aggregate variables. To collect the variables in the study, a data set was provided, which includes the information of each country based on the cumulative deaths, case fatality rate, recovery rate, and the number of performed COVID-19 tests. Scatter plots of environmental factors for the studied countries were drawn based on cumulative incidence rate of cases, cumulative incidence rate of death, tests, recovery rate, and case fatality rate of COVID-19. Furthermore, Spearman correlation coefficient was also used to verify the correlation between environmental factors and indicators related to COVID-19. The results of this ecological study showed that among all countries surveyed, Montenegro (60,310.56 per million) and Luxembourg (54,807.89 per million) had the highest cumulative incidence rates of COVID-19 cases, when Tanzania (8.42 per million) and Vietnam (13.78 per million) had the lowest cumulative incidence rates of COVID-19. In addition, in this study, it was shown that the cumulative incidence rate of cases, the cumulative incidence rate of deaths, and performed COVID-19 tests had significant direct correlations with the access to drinking water and the access to sanitation services (p < 0.001). The findings of the present study showed an inverse correlation between the mortality rate due to unhealthy water consumption, poor health status, and a positive correlation between access to drinking water and health services with the cumulative incidence and mortality rates of COVID-19. The differences between our findings and many other studies could be due to the ecological nature of the study. Nevertheless, our findings will help health policymakers to develop timely strategies to reduce the mortality and incidence rate of COVID-19.
Similar content being viewed by others
Introduction
COVID-19 is a potentially fatal respiratory disease named after the coronavirus detected in December 2019 in Wuhan, China (Hamidian Jahromi et al. 2020; Hu et al. 2020; Kalteh et al. 2020). The disease marks the third outbreak of beta-coronaviruses in the twenty-first century, sparking a worldwide public health crisis. The previous outbreaks of this viral family occurred in 2002 and 2012 (Shahriarirad et al. 2020). Although COVID-19 mortality is lower than SARS (severe acute respiratory syndrome), it is a highly contagious disease spreading rapidly throughout the world. Some people with COVID-19 infection remain asymptomatic, while others often show mild to moderate to severe symptoms including fever, cough, and shortness of breath within 2 to 14 days of exposure to the virus (Daneshfar et al. 2020; Gharakhanlou and Hooshangi 2020; McMichael et al. 2020; Struyf et al. 2020). As of December 23rd, 2020, 76,858,506 confirmed cases of COVID-19 had been identified, of which 1,711,498 were deceased. Of these, 33,251,796 were in the USA, 24,379,383 were in Europe, 11,710,770 were in Southeast Asia, and 4,731,359 were in the eastern Mediterranean region (Organization, 2020).
Various factors play important roles in the transmission of this virus, including factors related to human behavior, along with environmental factors such as air quality, the presence of safe water, wastewater collection, and effective hygiene in the COVID-19 epidemic which play essential roles in maintaining human health (Eslami and Jalili 2020). One study conducted in the USA identified air pollutants, particularly NO2 as an important factor associated with susceptibility against COVID-19 and its mortality(Sarmadi et al. 2021). Air temperature has also been expressed as an influential environmental factor in the development of COVID-19 (Babu et al., 2020; Tosepu et al. 2020; Zhu et al. 2020). According to the World Health Organization (WHO), in 2017, 71% of the world’s population (5.3 billion people) used safe drinking water services, and about 785 million people did not even have access to any basic drinking water services.
According to the studies conducted in 60 countries which have had the highest health risks for COVID-19, one out of every two schools lacked basic water and sewage services (Organization 2017). The results of a study also showed that inequalities in access to the necessities of life, including water, sanitary equipment, and food storage, can neutralize the preventive measures taken against COVID-19 and increase the incidence and spread of the disease (Ekumah et al. 2020). Considering that the studies on the relationship between environmental factors and the rate of coronavirus transmission are more in the field of air and atmosphere (Poirier et al. 2020; Shi et al. 2020; Vantarakis et al. 2020), studies on the impact of water status and safe health services in coronavirus transmission are very rare. Also, hygiene and regular hand washing are two of the main factors in preventing the transmission of coronavirus to a person, which could be achieved only in the context of access to safe water services and safe health conditions. Therefore, the aim of this study was to investigate the correlation between environmental factors (access to drinking water, access to sanitary bathroom facilities, the mortality rate of unsafe water and PM 2.5 pollution) and the epidemiological indices of COVID-19, including new cases, recovery rate, mortality rate, and the number of tests taken.
Methods
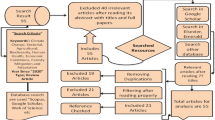
Study design and data collection
This survey is an ecological study, so all of the studied parameters are aggregate variables. To collect the variables in the study, a data set was provided which included the information of each country about the cumulative incidence rate of cases, cumulative incidence rate of deaths, case fatality rate, recovery rate, and the number of performed COVID-19 tests per million of the population. Information about COVID-19 for each country was retrieved from https://www.worldometers.info/ for the period of time from the date of the first reported case until November 30th, 2020. The data regarding the cumulative incidence rate of cases, cumulative incidence rate of deaths, and cumulative tests performed per million were available for 164 (Montenegro, Luxembourg, Bahrain, Belgium, Qatar, Czech Republic, Armenia, USA, Panama, Switzerland, Israel, Slovenia, Spain, Georgia, France, Kuwait, Croatia, Austria, Argentina, the Netherlands, Brazil, North Macedonia, Peru, Portugal, Chile, Bosnia and Herzegovina, Costa Rica, Moldova, Italy, Poland, Colombia, Romania, Sweden, Oman, Maldives, UK, Lithuania, Hungary, Malta, Jordan, Bulgaria, Serbia, Slovak Republic, Cabo Verde, the Bahamas, Lebanon, United Arab Emirates, Ukraine, Iceland, Russia, Ireland, Belize, Belarus, Denmark, Albania, Dominican Republic, South Africa, Iraq, Germany, Bolivia, Libya, Azerbaijan, Paraguay, Iran, Kyrgyz Republic, Honduras, Ecuador, Saudi Arabia, Greece, Singapore, Canada, Morocco, Estonia, Latvia, Suriname, Cyprus, Mexico, Tunisia, Nepal, Turkey, Kazakhstan, Guyana, India, Guatemala, Norway, El Salvador, Djibouti, Eswatini, Namibia, Trinidad and Tobago, Finland, Sao Tome and Principe, Botswana, Gabon, the Philippines, Malaysia, Jamaica, Equatorial Guinea, RB Venezuela, Bangladesh, Guinea-Bissau, Uzbekistan, Indonesia, Algeria, Mauritania, Pakistan, Myanmar, Ghana, Uruguay, Kenya, the Gambia, Tajikistan, Afghanistan, Japan, Egypt, Sri Lanka, Australia, Guinea, Lesotho, Barbados, Senegal, Zambia, Ethiopia, Cameroon, Nicaragua, Haiti, Cuba, Comoros, the republic of Korea, Zimbabwe, Madagascar, Bhutan, Mozambique, Angola, Rwanda, Syrian Arab Republic, Uganda, New Zealand, Mauritius, Sudan, Togo, Nigeria, Liberia, Malawi, Sierra Leone, Somalia, South Sudan, Benin, Mongolia, Mali, Burkina Faso, Chad, Republic of Yemen, Papua New Guinea, Democratic Republic of Congo, Niger, China, Thailand, Burundi, Fiji, Timor-Leste, Cambodia, Vietnam, and Tanzania), 160 (all countries that had cumulative incidence rate of cases except Bhutan, Mongolia, Timor-Leste, and Cambodia), and 152 (all countries that had cumulative incidence rate of cases except Comoros, Tajikistan, Burkina Faso, Chad, Somalia, Sierra Leone, Nicaragua, Algeria, Sudan, Syrian Arab Republic, Tanzania, and Democratic Republic of Congo) countries respectively. Recovery rate data were available for 159 (all countries that had cumulative incidence rates of cases except UK, Sweden, the Netherlands, and Democratic Republic of Congo) countries, and case fatality rate data was accessed for 160 (all countries that had cumulative incidence rate of cases except Bhutan, Mongolia, Timor-Leste, and Cambodia) nations. Data on access to drinking water services, access to sanitary bathroom facilities, the mortality rate of unsafe water, and PM 2.5 pollution were taken from the World Bank website (De Angelis et al. 2021a, b; Odih et al. 2020; Rodriguez-Villamizar et al. 2021a, b; Yao et al. 2020).
In this study, accessible drinking water services was defined as the existence of a source of drinking water from an improved resource, provided that the collection time is not more than 30 min for a round trip. This definition encompasses both sources of essential drinking water and those with safely managed drinking water services. Improved water sources included piped water, boreholes, protected dug wells, protected springs, and packaged or delivered water (Contini and Costabile 2020). Also, accessible sanitary services were defined as improved bathroom facilities that are not shared with other households. This definition encompasses both facilities with basic and safely managed sanitation services. Improved sanitation facilities include flush/pour flush to piped sewer systems, septic tanks or pit latrines, and improved ventilated pit latrines, composing of toilets or pit latrines with slabs (Ekumah et al. 2020). The mortality rate of unsafe water was defined as the deaths attributable to consumption of unsafe water, as well as sanitation and hygiene focusing on inadequate wash services, expressed per 100,000 people. Death rates were calculated by dividing the number of deaths by the total population (Nwobodo and Chukwu 2020). Living under PM 2.5 pollution was also defined as living in places where mean annual concentrations of PM 2.5 are greater than 15 μg per cubic meter. The WHO Air Quality Guideline (AQG) recommends 10 μg per cubic meter as the minimum concentration over which adverse health effects due to PM 2.5 exposure have been observed (Anim and Ofori-Asenso 2020).
Statistical analysis
Scatter plots of environmental factors for the studied countries were drawn based on cumulative incidence rate of cases, cumulative incidence rate of deaths, tests performed per million, recovery rate, and case fatality rate of COVID-19. Furthermore, Spearman correlation coefficient was also used to verify the correlation between environmental factors and indices related to COVID-19.
Results
The results of this ecological study showed that among all surveyed countries, Montenegro (60,310.56 per million) and Luxembourg (54,807.89 per million) had the highest cumulative incidence rates of COVID-19, when Tanzania (8.42 per million) and Vietnam (13.78 per million) had the lowest cumulative incidence rates of COVID-19. Also, it revealed that Belgium (1425.15 per million) followed by Spain (1118.96 per million) had the highest cumulative incidence rates of deaths due to COVID-19, when Burundi (0.08 per million) and Tanzania (0.35 per million) had the lowest cumulative incidence rates of deaths due to COVID-19. Luxembourg (2,180,641.18 per million) and United Arab Emirates (1,682,880.81 per million) were the countries with the highest numbers of performed COVID-19 tests per million among the studied countries.
The lowest number of performed COVID-19 tests per million belonged to Yemen (560.05 per million) and Niger (1885.52 per million). The highest recovery rates were in Timor-Leste (100%) and Singapore (99.86%), when the lowest recovery rates were seen in Belgium (6.48%) and France (7.28%). In addition, the highest case fatality rates of COVID-19 were in Yemen (28.34%), followed by Mexico (9.54%), while, the lowest case fatality rates of COVID-19 were in Singapore (0.05%) and Burundi (0.15%). Table 1 shows the correlation coefficient between the indicators related to COVID-19 and the environmental health indices. This study showed that the cumulative incidence rate of cases, the cumulative incidence rate of deaths, and the performed COVID-19 tests per million had a significant direct correlation with accessible drinking water services and accessible sanitation services (p < 0.001). Thus, increasing these two indicators would lead to increased cumulative incidence rate of cases, cumulative incidence rate of deaths, and performed tests per million. However, there were inverse significant correlations between the cumulative incidence rate of cases, the cumulative incidence rate of deaths, and performed tests per million with mortality rate attributed to unsafe water, unsafe sanitation, lack of hygiene, and PM 2.5 pollution (p < 0.001).
The recovery rate was directly and significantly correlated with the mortality rate attributed to unsafe water, unsafe sanitation and lack of hygiene, and PM 2.5 pollution. Case fatality rate had a significant inverse correlation with accessible sanitation services and direct correlations with mortality rate attributed to unsafe water, unsafe sanitation, and lack of hygiene. Figures 1, 2, 3 to 4 show the scatter plots of environmental health indicators by cumulative incidence rate of cases, cumulative incidence rate of deaths, performed tests per million, recovery rate, and case fatality rate in all countries and countries with a population more than 10 million.
Discussion
The present study is an ecological study that examined the correlation between the environmental factors with the incidence of COVID-19, performed COVID-19 tests, lethality, and recovery rates of COVID-19 in 164 countries. The coronavirus is now a serious threat to the whole world (Nwobodo and Chukwu 2020). One of the ways by which the disease is transmitted is by contact of the contaminated hands with eyes and nose. As a result, regular hygiene, hand washing, and personal hygiene are highly recommended to control the spread of the virus (Anim and Ofori-Asenso 2020). This would be possible if sufficient water and the required sanitary resources were available (Nwobodo and Chukwu 2020).
Based on the results of the present study, there is a direct correlation between the level of access to health services and drinking water with the cumulative incidence rate, the cumulative death rate, and the number of tests performed per million of the population. Other studies have shown that the lack of adequate sanitation facilities in rural communities increases the prevalence of COVID-19 (Bourgonje et al. 2020; Stoler et al. 2020). There is a widespread inequality in access to some sanitary equipment as well as sanitary water, which has increased the vulnerability of some people to COVID-19 (Ekumah et al. 2020).
According to the WHO, 663 million people in Africa and Asia (Odih et al. 2020) including 71% of people in Nigeria do not have access to clean and safe water or even water disinfectants (Nwobodo and Chukwu 2020). United Nations (UN) estimates that about 3 billion people do not have the facilities to wash their hands (Lal et al. 2020). A study in sub-Saharan Africa found that 46% of the surveyed households did not have access to basic necessities of life, including sanitation (Ekumah et al. 2020). Some people have been infected with COVID-19 without contact with infected people, indicating other modes of transmission than respiratory route (Odih et al. 2020). The virus can attack the gastrointestinal tract directly through the angiotensin converting enzyme 2, and the virus has also been found in the fecal samples of newly discharged patients (Silva et al. 2020). In areas that do not have adequate sanitation facilities, there are feces around the sewage (Odih et al. 2020), and it enters the surface water and pollutes it, so it is essential to provide people with a sanitary toilet (Purnama and Susanna, 2020). Furthermore, between 60 and 90% of Africans do not have a proper sewage system and defecate outdoors, causing these pollutants to enter surface water (Odih et al. 2020), and about one billion people in the world drink from public tap water and wells or use surface water sources (Stoler et al. 2020).
Betany and colleagues estimated in their study that more than one billion people worldwide go outside to get the water they need and that 9% of the world’s population defecates outdoors and 8% (627 million) use a facility shared with at least another one (Caruso & Freeman, 2020). However, Renata et al. stated that the incidence and morbidity of COVID-19 are significantly related to the overall index of safe water supply services, as well as the rate of mortality with wastewater treatment index (Silva et al. 2020). These hypotheses are based on the suspicion of the oral fecal transmission of COVID-19 and indicate that the lack of sanitary water and adequate sanitation facilities increase the rate of mortality and the incidence of COVID-19 cases; we must keep in mind that there are many other factors that contribute to this method of transmission. Transmissions are effective, in the context of rainfall, which causes sewage to overflow and transmit more viruses (Odih et al. 2020). The number of viruses required for oral transmission is also very high. In addition, in areas where people use rationalized water, they have to stand in crowded queues without abiding by social distancing to receive their water ration, and, since they do not wash their hands to save water, the incidence of COVID-19 is higher (Odih et al. 2020). We must keep in mind that the main route of transmission of COVID-19 is by respiration of infective droplets and that the gastrointestinal transmission is a minor route; however, the reason for the difference between the results of our study and many other studies can be due to the fact that our study is an ecological study and only shows correlations and cannot give us an accurate causal relationship. On the other hand, in our study, information about all countries with appropriate and inadequate health levels was piled up and then examined, which could be a reason for erroneous study results.
Additionally, based on the results of our study, there was an inverse and moderate correlation between the amount of PM 2.5 in the air with the cumulative incidence rate of cases and the cumulative incidence rate of deaths. Also, there was a weak inverse correlation between performed tests per million and PM 2.5 in the air. PM 2.5 is one of the most important environmental health hazards that cause the mortality of many people around the world every year (Contini & Costabile, 2020). An ecological study in Colombia found a positive correlation between PM 2.5 and the mortality due to COVID-19 (Laura A Rodriguez-Villamizar et al. 2021a, b). Numerous studies have measured the effects of air quality on the incidence and mortality rate of COVID-19. The results of the studies in Canada, Spain, and Turkey showed that there is a strong positive correlation between PM 2.5 concentration and the number of new daily cases of COVID-19 (Sarwar et al. 2021; Shahzad et al. 2021; K. Shahzad et al. 2020a, b). A study in the UK also showed that with each microgram increase in PM 2.5, the mortality of COVID-19 increased by 12%, and the risk of infection also increased (Travaglio et al. 2021).
Angelis et al. also showed that with each 10-μg increase in PM 2.5, the incidence and mortality due to COVID-19 increased by 8% and 23%, respectively (Elena De Angelis et al. 2021a, b). Another study in China showed that for each 10-μg increase in PM 2.5, the lethality of COVID-19 increased by 24% (Yao et al. 2020). Other studies have shown this direct and positive relationship (Conticini et al. 2020; Yao et al. 2020), while Laura et al. reported that there was no significant association between long-term exposure to PM 2.5 and the mortality due to COVID-19 [37]. Other studies in China and New Jersey, USA have shown a positive and direct correlation between incidence rate of COVID-19 and the concentration of PM 2.5 (Doğan et al. 2020; Fareed et al. 2020). The results of a study in China showed a positive correlation in some states, while in other states a negative correlation was seen (F. Shahzad et al. 2020a, b). The reason for the difference between the results of our study and other studies can be due to various factors, for example, the differences in population density of different regions, the different climatic conditions, and even the existence of different industries and different pollutants in each region that can affect the results. It should be noted that quarantining people and restricting their activities can help reduce environmental pollutants and thus reduce the incidence of COVID-19. (K. Shahzad et al. 2020a, b).
Regarding the reason for the direct relationship between PM 2.5 and the incidence and mortality of COVID-19, various speculations have been expressed, including that these particles cause inflammation in the lungs and other organs of the body through inflammatory and oxidation mechanisms (Contini & Costabile, 2020; Elena De Angelis et al. 2021a, b).
In this way, by increasing the inflammation in the pulmonary cells, they intensify the symptoms of the disease (Comunian et al. 2020). On the other hand, these particles have adverse effects on other (Contini & Costabile, 2020) body systems, including the cardiovascular system, blood, and respiratory system in a way that they weaken the immune system and thus predispose people to COVID-19 (Contini & Costabile, 2020). Another hypothesis has been stated that the angiotensin-converting enzyme 2 facilitates the entry of these particles into the lungs, resulting in inflammation and exacerbation of COVID-19 (Comunian et al. 2020; Daminov et al. 2021; Elena De Angelis et al. 2021a,b; Pezeshgi et al. 2021). Moreover, although this hypothesis is yet to be proven, some researchers have suggested that SARS-CoV-2 may attach to PM 2.5 particles in the air, enter the lungs, and cause the disease (Laura A Rodriguez-Villamizar et al. 2021a, b). Despite all the hypotheses that there should be a direct correlation between PM 2.5 and COVID-19 incidence, an inverse correlation has been found in our study, which may be due to the ecological nature of our research. We should also note that we have studied different countries of the world together in which the age and sex composition, economic and social status and development, and executive control policies are different, all of which can affect the type of correlation seen. On the other hand, it is hypothesized that PM 2.5 only indirectly changes the course and severity of the disease from mild to severe and is effective on the prognosis of the disease and thus increases the mortality rate (Yao et al. 2020). Also, the duration of exposure to these particles, the relative weight of these particles, and other underlying diseases in people can be factors influencing the incidence of this disease.
Limitations
One of the strengths of the present study is that for the first time, the relationship between environmental health factors and COVID-19 indices, including the cumulative incidence rate of cases, the cumulative incidence rate of deaths, cumulative tests performed per million, recovery rate, and the case fatality rate were examined in 164 countries, but the limitation of this study is ecologic fallacy due to its ecological nature.
Conclusion
The findings of the present study showed an inverse correlation between the mortality rate due to unhealthy water consumption, poor health status, and a positive correlation between access to drinking water and health services with the cumulative incidence and mortality rate of COVID-19. The differences between our findings and many other studies could be due to the ecological nature of the study. Nevertheless, our findings will help health policymakers to develop timely strategies to reduce the mortality and the incidence rates of COVID-19. However, it is essential that health policymakers develop strategies to identify rural and high-risk areas that do not have access to these services and provide safe drinking water. Also, facilitating the access to health services in those areas is vital. Furthermore, the necessary training on the importance of hand washing, safe drinking water, and proper and hygienic disposal to residents of these areas should be done with more emphasis.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SARS:
-
Severe acute respiratory syndrome
- WHO:
-
World Health Organization
- AQG:
-
Air Quality Guideline
- UN:
-
United Nations
References
Anim, D. O., & Ofori-Asenso, R. (2020). Water scarcity and COVID-19 in sub-Saharan Africa. The Journal of infection
Babu SR, Rao NN, Kumar SV, Paul S, Pani SK (2020) Plausible role of environmental factors on COVID-19 transmission in the Megacity Delhi. Aerosol and Air Quality Research, India, p 20
Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, Bolling MC, Dijkstra G, Voors AA, Osterhaus AD (2020) Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol 251(3):228–248
Caruso BA, Freeman MC (2020) Shared sanitation and the spread of COVID-19: risks and next steps. The Lancet Planetary Health 4(5):e173
Comunian S, Dongo D, Milani C, Palestini P (2020) Air pollution and Covid-19: the role of particulate matter in the spread and increase of Covid-19’s morbidity and mortality. Int J Environ Res Public Health 17(12):4487
Conticini E, Frediani B, Caro D (2020) Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut 261:114465. https://doi.org/10.1016/j.envpol.2020.114465
Contini D, Costabile F (2020) Does air pollution influence COVID-19 outbreaks? Multidisciplinary Digital Publishing Institute, Basel
Daminov, B., Abdullaev, S., Sharapov, O., & Igamberdieva, R. (2021). Epidemiological, clinical and morphological aspects of kidney damage in COVID-19. Journal of Renal Injury Prevention, 10(3).
Daneshfar M, Dadashzadeh N, Ahmadpour M, Haghi HR, Rahmani V, Frouzesh M, Valizadeh R (2020) Lessons of mortality following COVID-19 epidemic in the United States especially in the geriatrics. Journal of Nephropharmacology 10(1):e06–e06
De Angelis E, Renzetti S, Volta M, Donato F, Calza S, Placidi D, Lucchini RG, Rota M (2021a) COVID-19 incidence and mortality in Lombardy, Italy: an ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environ Res 195:110777. https://doi.org/10.1016/j.envres.2021.110777
De Angelis E, Renzetti S, Volta M, Donato F, Calza S, Placidi D, Lucchini RG, Rota M (2021) COVID-19 incidence and mortality in Lombardy, Italy: an ecological study on the role of air pollution, meteorological factors, demographic and socioeconomic variables. Environmental research 195:110777
Doğan B, Ben Jebli M, Shahzad K, Farooq TH, Shahzad U (2020) Investigating the effects of meteorological parameters on COVID-19: case study of New Jersey. United States Environ Res 191:110148. https://doi.org/10.1016/j.envres.2020.110148
Ekumah B, Armah FA, Yawson DO, Quansah R, Nyieku FE, Owusu SA, Odoi JO, Afitiri A-R (2020) Disparate on-site access to water, sanitation, and food storage heighten the risk of COVID-19 spread in Sub-Saharan Africa. Environ Res 189:109936–109936. https://doi.org/10.1016/j.envres.2020.109936
Eslami H, Jalili M (2020) The role of environmental factors to transmission of SARS-CoV-2 (COVID-19). AMB Express 10:1–8
Fareed Z, Iqbal N, Shahzad F, Shah SGM, Zulfiqar B, Shahzad K, Hashmi SH, Shahzad U (2020) Co-variance nexus between COVID-19 mortality, humidity, and air quality index in Wuhan, China: new insights from partial and multiple wavelet coherence. Air Qual Atmos Health 13(6):673–682. https://doi.org/10.1007/s11869-020-00847-1
Gharakhanlou NM, Hooshangi N (2020) Spatio-temporal simulation of the novel coronavirus (COVID-19) outbreak using the agent-based modeling approach (case study: Urmia, Iran). Informatics in Medicine Unlocked 20:100403
Hamidian Jahromi, A., Mazloom, S., & Ballard, D. (2020). What the European and American health care systems can learn from China COVID-19 epidemic; action planning using purpose designed medical telecommunication, courier services, home-based quarantine, and COVID-19 walk-in centers. Immunopathol Persa. 2020; 6 (2): e17. https://doi.org/10.34172/ipp. 2020. 17. By failing to prepare, you are preparing to fail.
Hu L, Chen S, Fu Y, Gao Z, Long H, Ren H-W, Zuo Y, Wang J, Li H, Xu Q-B (2020) Risk factors associated with clinical outcomes in 323 coronavirus disease 2019 (COVID-19) hospitalized patients in Wuhan. China Clinical Infectious Diseases 71(16):2089–2098
Kalteh EA, Sofizadeh A, Fararooei M, Ghojogh MG, Aljalili S (2020) Measures of mortality in coronavirus (COVID-19) compared with SARS and MERS. Journal of Cellular & Molecular Anesthesia 5(2):97–101
Lal, A., Lucas, R. M., & Slatyer, A. (2020). Water access as a required public health intervention to fight COVID-19 in the Pacific Islands. The Lancet Regional Health-Western Pacific, 1.
McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, Lewis J, Baer A, Kawakami V, Lukoff MD (2020) Epidemiology of Covid-19 in a long-term care facility in King County. Washington New England Journal of Medicine 382(21):2005–2011
Nwobodo TN, Chukwu KE (2020) COVID-19 Era and water supply: challenges for rural communities in Eastern, Nigeria. Journal of Geoscience and Environment Protection 8(7):219–233
Odih EE, Afolayan AO, Akintayo I, Okeke IN (2020) Could water and sanitation shortfalls exacerbate SARS-CoV-2 transmission risks? Am J Trop Med Hyg 103(2):554–557
Organization, W. H. (2017). Progress on drinking water, sanitation and hygiene: 2017 update and SDG baselines.
[Record #15 is using a reference type undefined in this output style.]
Pezeshgi A, Mubarak M, Djamali A, Mostafavi L, Moghadam-Kia S, Alimohammadi N, Peymani P, Pezeshgi S (2021) COVID-19-associated glomerulopathy and high-risk apol1 genotype; basis for a two-hit mechanism of injury? A narrative review on recent findings. Journal of Nephropathology 10(2):1–7
Poirier C, Luo W, Majumder MS, Liu D, Mandl KD, Mooring TA, Santillana M (2020) The role of environmental factors on transmission rates of the COVID-19 outbreak: an initial assessment in two spatial scales. Sci Rep 10(1):1–11
Purnama, S. G., & Susanna, D. (2020). Hygiene and sanitation challenge for covid-19 prevention in Indonesia. Kesmas: Jurnal Kesehatan Masyarakat Nasional (National Public Health Journal).
Rodriguez-Villamizar LA, Belalcázar-Ceron LC, Fernández-Niño JA, Marín-Pineda DM, Rojas-Sánchez OA, Acuña-Merchán LA, Ramírez-García N, Mangones-Matos SC, Vargas-González JM, Herrera-Torres J (2021) Air pollution, sociodemographic and health conditions effects on COVID-19 mortality in Colombia: an ecological study. Science of The Total Environment 756:144020
Rodriguez-Villamizar LA, Belalcázar-Ceron LC, Fernández-Niño JA, Marín-Pineda DM, Rojas-Sánchez OA, Acuña-Merchán LA, Ramírez-García N, Mangones-Matos SC, Vargas-González JM, Herrera-Torres J, Agudelo-Castañeda DM, Piñeros Jiménez JG, Rojas-Roa NY, Herrera-Galindo VM (2021b) Air pollution, sociodemographic and health conditions effects on COVID-19 mortality in Colombia: an ecological study. Sci Total Environ 756:144020. https://doi.org/10.1016/j.scitotenv.2020.144020
Sarmadi M, Moghanddam VK, Dickerson AS, Martelletti L (2021) Association of COVID-19 distribution with air quality, sociodemographic factors, and comorbidities: an ecological study of US states. Air Qual Atmos Health 14(4):455–465
Sarwar S, Shahzad K, Fareed Z, Shahzad U (2021) A study on the effects of meteorological and climatic factors on the COVID-19 spread in Canada during 2020. J Environ Health Sci Eng. https://doi.org/10.1007/s40201-021-00707-9
Shahriarirad R, Khodamoradi Z, Erfani A, Hosseinpour H, Ranjbar K, Emami Y, Mirahmadizadeh A, Lotfi M, Yeganeh BS, Nejad AD (2020) Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infect Dis 20(1):1–12
Shahzad F, Shahzad U, Fareed Z, Iqbal N, Hashmi SH, Ahmad F (2020a) Asymmetric nexus between temperature and COVID-19 in the top ten affected provinces of China: a current application of quantile-on-quantile approach. Sci Total Environ 736:139115. https://doi.org/10.1016/j.scitotenv.2020.139115
Shahzad, K., Farooq, T. H., Doğan, B., Zhong Hu, L., & Shahzad, U. (2021). Does environmental quality and weather induce COVID-19: case study of Istanbul, Turkey. Environmental Forensics, 1-12. https://doi.org/10.1080/15275922.2021.1940380
Shahzad K, Shahzad U, Iqbal N, Shahzad F, Fareed Z (2020b) Effects of climatological parameters on the outbreak spread of COVID-19 in highly affected regions of Spain. Environ Sci Pollut Res Int 27(31):39657–39666. https://doi.org/10.1007/s11356-020-10551-3
Shi, P., Dong, Y., Yan, H., Li, X., Zhao, C., Liu, W., He, M., Tang, S., & Xi, S. (2020). The impact of temperature and absolute humidity on the coronavirus disease 2019 (COVID-19) outbreak-evidence from China. MedRxiv.
Silva, R. R. d., Santos, M. B. d., Santos, A. D. d., Tavares, D. d. S., & Santos, P. L. d. (2020). Coronavirus disease and basic sanitation: too early to be worried? Revista da Sociedade Brasileira de Medicina Tropical, 53.
Stoler, J., Jepson, W. E., & Wutich, A. (2020). Beyond handwashing: water insecurity undermines COVID-19 response in developing areas. Journal of Global Health, 10(1).
Struyf, T., Deeks, J. J., Dinnes, J., Takwoingi, Y., Davenport, C., Leeflang, M. M., Spijker, R., Hooft, L., Emperador, D., & Dittrich, S. (2020). Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID‐19 disease. Cochrane Database of Systematic Reviews(7).
Tosepu R, Gunawan J, Effendy DS, Lestari H, Bahar H, Asfian P (2020) Correlation between weather and Covid-19 pandemic in Jakarta. Indonesia. Science of The Total Environment 725:138436
Travaglio M, Yu Y, Popovic R, Selley L, Leal NS, Martins LM (2021) Links between air pollution and COVID-19 in England. Environmental Pollution 268:115859
Vantarakis, A., Chatziprodromidou, I., & Apostolou, T. (2020). COVID-19 and environmental factors. A PRISMA-compliant systematic review. MedRxiv.
Yao Y, Pan J, Wang W, Liu Z, Kan H, Qiu Y, Meng X, Wang W (2020) Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Science of the Total Environment 741:140396
Zhu Y, Xie J, Huang F, Cao L (2020) Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Science of The Total Environment 727:138704
Funding
This study was approved and financially supported by Shiraz University of Medical Sciences (Grant number: 99–01-106–19536). The authors would like to thank the vice chancellor for research and technology for financial support.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. AMA and MGG participated in the design of the study. KJ, LM, and AH performed data collection. FR and AJ wrote the manuscript. SSD and ML revised the manuscript. FR and MGG helped with statistical analysis and prepared the illustrations. AHH edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research ethics committee of Shiraz University of Medical Sciences (IR.SUMS.REC.1399.174).
Consent for publication
All the authors agreed this article be published.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mirahmadizadeh, A., Rezaei, F., Jokari, K. et al. Correlation between environmental factors and COVID-19 indices: a global level ecological study. Environ Sci Pollut Res 29, 16667–16677 (2022). https://doi.org/10.1007/s11356-021-16876-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16876-x