Abstract
An increasing number of studies examined the potential effects of PM1 (submicronic particulate matter with an aerodynamic diameter ≤ 1 μm) on the risk of respiratory diseases; however, the results have been inconclusive. This study aimed to determine the overall association between PM1 with total and cause-specific respiratory diseases. A systematic review and meta-analysis was conducted with 68 related articles retrieved, and six articles met the full inclusion criteria for the final analysis. For a 10 μg/m3 increase in PM1, the pooled odds ratio (OR) was 1.05 (95% CI 0.98–1.12) for total respiratory diseases, 1.25 (95% CI 1.00–1.56) for asthma, and 1.07 (95% CI 1.04–1.10) for pneumonia with the I2 value of 87%, 70%, and 0%, respectively. Subgroup analyses showed that long-term exposure to PM1 was associated with increased risk of asthma (OR 1.47, 95% CI 1.33–1.63) with an I2 value of 0%, while short-term exposure to PM1 was not associated with asthma (OR 1.07, 95% CI 0.89–1.27) with the I2 value of 0%. Egger’s test showed that publication bias existed (P = 0.041); however, the funnel plot was symmetrical with the inclusion of the moderator. In conclusion, elevated levels of PM1 may increase morbidity in total and cause-specific respiratory diseases in the population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Respiratory diseases are the leading causes of morbidity and mortality worldwide (GBD 2019 Diseases and Injuries Collaborators 2020). In recent decades, chronic respiratory diseases, such as chronic obstructive pulmonary disease (COPD) and asthma, have attracted increasing attention (Wang et al. 2018; Huang et al. 2019). In 2019, the numbers of people with COPD and asthma were 212 million and 262 million worldwide, respectively (GBD 2019 Diseases and Injuries Collaborators 2020). Therefore, further study on the risk factors is necessary to minimize the morbidity of respiratory diseases and to improve prevention and guidelines for treating respiratory diseases.
Ambient particulate matter pollution has been a severe public health issue worldwide (Kim et al. 2019; Wang et al. 2021a). Although there has been improvement in air quality over recent decades in some countries, more than 90% of the global population lives in areas with air quality exceeding guidelines (Evangelopoulos et al. 2020). In 2019, ambient particulate matter pollution led about 1.4 million deaths in China (GBD 2019 Diseases and Injuries Collaborators 2020). The acute and long-term effects of ambient air pollution on human health are well known. Some epidemiological studies showed that the degree of exposure to ambient particulate matter (PM) is associated with daily mortality, mainly from cardiovascular and respiratory diseases (Liu et al. 2019a; Tian et al. 2020). Previous epidemiological studies have focused on the adverse effects of fine particulate matter (PM2.5, particulate matter with an aerodynamic diameter ≤ 2.5 μm) and inhalable particulate matter (PM10, particulate matter with an aerodynamic diameter ≤ 10 μm) (Doiron et al. 2019; Yang et al. 2020). Exposure to PM2.5 and PM10 has been proven to be associated with respiratory diseases (Yao et al. 2020; Gurung et al. 2017; Pun et al. 2017; Sicard et al. 2019; Cao et al. 2021).
The most recent research indicated that PM1 (submicronic particulate matter with an aerodynamic diameter ≤ 1 μm) contributed 77–86% of the PM2.5 concentration in China (Chen et al. 2018). However, it remains unknown whether PM1 or PM1-2.5 induced the adverse effects of PM2.5. It has been stated that the size of PM has a negative correlation with the level of its toxicity in the lungs, which means that PM1 provide more detrimental effects than PM2.5 (Hamra et al. 2014; Valavanidis et al. 2008). However, limited evidence was found for the association between particulate matter and respiratory diseases, especially on PM1.
According to previous epidemiological studies, the exposure to PM1 contributing to the development of respiratory diseases remains uncertain (Zhang et al. 2021). To assess the effects of exposure to PM1 quantitatively and accurately on the respiratory diseases, we conducted a systematic review and meta-analysis on all relevant studies published thus far.
Methods
Literature search strategy
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines (Moher et al. 2009; Stroup et al. 2000). Three authors systematically searched PubMed (1966 to Apr 2021), Embase (1950 to Apr 2021), and the Cochrane Library (2000 to Apr 2021) for studies on the associations between PM1 and respiratory diseases. The full search strategies are described in the supplementary data (Appendix 1). We also examined the references of the selected papers and reviews for additional pertinent data.
Inclusion and exclusion criteria
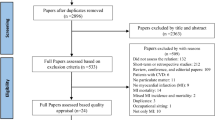
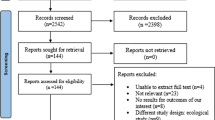
The flowchart of studies through the review process is shown in Fig. 1. Studies included in this meta-analysis met the following criteria: (1) epidemiological studies investigated the association between exposure to PM1 and morbidity of respiratory diseases; (2) the subjects of the study were the general human population, regardless of age, geographical areas, and occupations of the population; (3) studies that quantitatively showed the results of estimation of exposure to ambient outdoor PM1; (4) respiratory diseases in relation to exposure to PM1 were selected according to the 10th Revision of the International Classification of Diseases: total respiratory diseases (ICD-10: J00-J99) and cause-specific diseases including upper respiratory tract infections (URTI, J00-J06), pneumonia (J18), obstructive pulmonary diseases (COPD, J40-J44 and J47), and asthma (J45-J46); (5) provided the effect size of prevalence, hospital admission or emergency visit of respiratory diseases per 10 or interquartile range (IQR) μg/m3 increase in PM1 concentration: regression coefficient, percentage change (PR), excess rate (ER), risk ratio (RR), hazard ratio (HR) and odds ratio (OR), standard error (SE), and/or 95% confidence interval (CI); and (6) were published in English with full text. The exclusion criteria were as follows: (1) did not conform to the inclusion criteria or (2) reviews, commentaries, or communications; or (3) the subjects of the study were patients with comorbid diseases. If studies were published based on overlapping data, the most recent article with comprehensive data was included.
Risk of bias and quality assessment
The methodological quality and risk of bias of individual studies were assessed independently by two authors (Yaoyu Hu and Mengqiu Wu) using the criteria recommended by BioMed Central for study assessment (Luong et al. 2019). This recommendation contains 20 items for several study designs. The details of the score are as follows:
-
1.
Overall, scores higher than 75% are considered high quality, and scores lower than 50% are not included.
-
2.
Single questions: (1) there are only two options (yes or no): 1 is high quality, and 0 is low quality; (2) there is a problem if there are two high-quality studies and one low-quality study; (3) if there are three problems, the highest one is high quality, the middle one is medium quality, and the second one is low quality. In addition, we used RoB (Risk of Bias) for all quality evaluations.
Data extraction
The data extraction process was independently conducted by two researchers. The extracted data included citation information (name of the first author, publication year, and location in which the study was carried out); study setting (study design, time span, sample size, age of population, and percentages of males); exposure (pollutants, exposure type, mean concentration, and method used to estimate air pollutant levels); and outcome (health outcome/diagnosis, day lags of the effect, unit of concentrations of PM1, confounding factors that were adjusted for and study results). The short-term effect was defined as < 7 days. For short-term exposure studies with multiple lag estimates, we used an a priori lag selection protocol devised by Atkinson et al. to select one estimate for preventing the overrepresentation of a single study in this meta-analysis (Atkinson et al. 2014).
Statistical analysis
We used OR with 95% CI in the prevalence/hospital admission/emergency visit of respiratory diseases as a measure of effect size. All estimates were transformed to a 10 μg/m3 increase in PM1 concentration to pool results. We used Q-statistics to conduct heterogeneity tests, where P < 0.10 was considered to be statistically significant. The I2 statistics were calculated to represent the percentage of variation observed in studies caused by heterogeneity. An I2 value < 50% was generally regarded as low moderate heterogeneity between studies, indicating a fixed-effect model to pool the estimates. I2 values > 50%, representing high heterogeneity, indicated a random-effect model. We used forest plots to graphically display results. We assessed publication bias using funnel plots, contour-enhanced meta-analysis funnel plots, Begg’s test, and Egger’s weighted linear regression.
A subgroup analysis based on the exposure type of PM1 (short term and long term) was conducted. All tests were two-sided, and P < 0.05 was considered statistically significant, except in the heterogeneity test (P < 0.10). Transformation of effect size and meta-analysis was performed using MATLAB version 2018 and R version 4.0.5, respectively.
Results
Search findings and study characteristics
Sixty-eight studies were identified through the literature search, and 21 studies were eligible for full-text evaluation. Among them, 6 studies (Zhang et al. 2021; Wang et al. 2021b; Zhang et al. 2020; Yu et al. 2020; Luong et al. 2016; Michaud et al. 2004), published between 2004 and 2021, met our full inclusion criteria and were finally analyzed. The flowchart of this review shows the detailed process of selection (Fig. 1). The basic characteristics of the literature in the meta-analysis are summarized in Table 1. The included studies were performed in various regions (China, 4; Vietnam, 1; America, 1), including cross-sectional, time series, and case-crossover studies. In the included studies, PM1 was defined as fine particulate matter with an aerodynamic diameter ≤ 1 μm. The daily mean concentrations of PM1 across the 6 studies were 26.9 μg/m3. The outcomes of respiratory diseases included asthma (Zhang et al. 2021; Zhang et al. 2020; Yu et al. 2020; Michaud et al. 2004), pneumonia (Wang et al. 2021b; Zhang et al. 2020), and total respiratory diseases (Zhang et al. 2020; Luong et al. 2016). Four studies used ICD-10 to define the outcome, one based on incidence data, one based on emergency department visit data, and three based on hospital admission data. The estimated risk of outcome was reported as OR, HR, and PC.
Risk of bias and quality assessment
According to our bias assessment, the six included studies all had a low risk of bias (Fig. 2, Fig. S1). Table S1 shows the detailed assessment process.
Meta-analysis results
The pooled effect sizes of the association between exposure to PM1 and respiratory diseases are presented in Fig. 3. The degree of heterogeneity (I2) in this meta-analysis was large in pooled estimates for total respiratory diseases (87%) and asthma (70%) and low for pneumonia (0%). We revealed that the pooled effect of a 10 μg/m3 increase in PM1 on total respiratory diseases was not statistically significant (OR 1.05, 95% CI 0.98–1.12, Fig. 3a). There was a marginal association between a 10 μg/m3 increase in PM1 and asthma (OR 1.25, 95% CI 1.00–1.56, Fig. 3b). A 10 μg/m3 increase in PM1 was positively associated with pneumonia (OR 1.07, 95% CI 1.04–1.10, Fig. 3c).
The subgroup analysis demonstrated that the pooled acute effect of short-term exposure to PM1 on asthma was not statistically significant (OR 1.07, 95% CI 0.89–1.27, Fig. 4a), and long-term exposure to PM1 was positively associated with increased risk of asthma (OR 1.47, 95% CI 1.33–1.63, Fig. 4b).
Publication bias
The funnel plot was found to be asymmetric (Fig. 5), and publication bias was observed with Egger’s test (P = 0.041). Trim and fill analyses were conducted to investigate the impact of this bias (Fig. 6). With the inclusion of the moderator (study design), the funnel plot was symmetrical.
Discussion
This is the first meta-analysis to evaluate the impact of PM1 on respiratory diseases and provide an estimate of the impact. We found positive associations between PM1 and total and cause-specific respiratory diseases. PM1 is a health-damaging particle because it has chemical components and can penetrate deep inside the lungs to aggravate existing asthma or contribute to chronic bronchitis development (Fuertes et al. 2014; Ostro et al. 2009). Luong et al. found that an increase in PM1 concentration would decrease pulmonary function (Luong et al. 2016). In addition, our meta-analyses showed that asthma was most strongly associated with PM1, which was consistent with the limited literature available on fine particles (Liu et al. 2020; Hassanvand et al. 2015). We found that the funnel graph was asymmetric, and Egger’s test observed publication bias. However, with the addition of a moderator, we found that the funnel diagram is symmetrical. This indicates that most of the heterogeneity comes from different types of research designs.
It is not easy to assess the long-term impact of PM1 on human health because long-term prospective observation and research require many resources and much effort. Special techniques are needed to measure and estimate the exposure level of air pollutants over a wide range of areas. The few available studies identified through our literature search reflect considerable difficulties in designing such a study to investigate the impact of PM1 on respiratory diseases. In addition, the results of insufficient research proved to be inconsistent. Therefore, we believe that systematic review and meta-analysis would be a good choice for a more reliable estimation of the long-term effects of PM1 on respiratory diseases.
Despite growing experimental evidence on the toxicity of PM1, whether they truly contribute to the development of clinically manifested respiratory diseases is another question. A previous analysis showed a significant correlation between PM1 exposure and the incidence of respiratory diseases (Yang et al. 2018). However, regarding respiratory diseases, whether PM1 exposure can lead to the development of the disease has been controversial. Several reports have shown a higher prevalence of acute exacerbation of respiratory diseases, and odds have reported conflicting results. Previous studies on the long-term effects of PM1 on respiratory diseases produced inconsistent results (Zhang et al. 2021). This inconsistency of previous studies may be based on differences in host factors that are difficult to quantify. For example, host susceptibility to air pollutants can vary widely due to genetic factors or other environmental factors, such as tobacco smoking status (Ward-Caviness 2019; Lyall et al. 2017).
The main finding of our study was a significant association between the incidence of respiratory diseases and exposure to PM1. However, the explanation for this result is limited because the funnel diagram is asymmetric. This is not only because of the small research influence but also because more than 10,000 participants were involved in the research, which showed relatively wide confidence intervals (Zhang et al. 2021; Wang et al. 2021b). Furthermore, the asymmetry in the funnel plot may be due to the type of study design. Although the trim-and-fill analysis showed that the pooled OR was not significantly influenced by this funnel plot asymmetry, further well-designed observational studies are still needed to better clarify the association between PM1 and respiratory disease development.
The issue of heterogeneity between the studies must be addressed to appreciate our results more precisely. First, these studies have different follow-up times and durations according to different study designs. Second, different studies focus on different regions, which may lead to more significant. In addition, although there is a lack of knowledge regarding how long it takes for respiratory diseases to develop from exposure to PM1, it is assumed that more prolonged exposure may be more harmful (Yu et al. 2020; Guan et al. 2016). This is in line with a study showing that the duration of tobacco smoking has a more substantial effect than the daily amount of cigarette consumption on the development of COPD (Bhatt et al. 2018). The lengths of the follow-up period of each study may influence the evaluation of the effect. In addition, there are differences in the methods used to estimate air pollutant levels, including ground-based monitoring stations or the space-time extremely randomized trees model. A recently adopted method uses satellite data to estimate air quality to improve the spatial and temporary resolution of air quality modeling (Wang et al. 2019). With satellite-based data, future research is expected to make it easier and more accurate to evaluate the health impact of PM1.
Even though the exact biological mechanism for the association between PM1 and respiratory diseases are not entirely clear, several studies suggested that inhalation of PM may result in inflammation and oxidative stress (Zou et al. 2020; Wang et al. 2020; Valavanidis et al. 2008). Small particles, especially PM1, can more easily enter and deposit in the deeper respiratory tract. After internalized by respiratory epithelial cells, PM1 can trigger oxidative stress and inflammatory responses (Valavanidis et al. 2008; Yang et al. 2017). Existing research indicates that the pro-inflammatory response may play important roles in the effect of PM1 on lung function (Mazzarella et al. 2012).
One of our study’s strengths is the efforts made throughout the design and the systematic review to ensure its validity, including the incorporating risk of bias assessment. Another strength is to search all relevant literature and to make an in-depth, transparent, and repeatable evaluation of the evidence from studies focused on PM1 exposures as a potential cause of respiratory diseases. It is a timely contribution to a rapidly evolving field that could inform future research's focus and design to improve its utility. However, the present study has limitations. First, the number of included studies was small, and they did not cover all countries in the world. This limitation requires further research worldwide to assess the impact of PM1 on respiratory diseases, which would contribute to an updated systematic review and meta-analysis. Second, most of the studies included in the meta-analysis were conducted in China, with fewer studies in high-income developed countries and low-income developing countries. Studies have shown that countries with different incomes have different air pollutant levels (Quansah et al. 2017; Liu et al. 2019b; Baumgartner et al. 2020; Naidja et al. 2018). Therefore, we need more national data to understand the health effects of PM1 more clearly. Finally, our meta-analysis is based on different observational research designs, including cross-sectional, case-crossover, and time series. Therefore, individual studies may be affected by uncontrolled time-varying deviations, which we could not test.
Conclusion
The present systematic review and meta-analysis demonstrated that the pooled effect of a 10 μg/m3 increase in PM1 on total respiratory diseases was not statistically significant (OR 1.05, 95% CI 0.98–1.12). There was a marginal association between a 10 μg/m3 increase in PM1 and asthma (OR 1.25, 95% CI 1.00–1.56). A 10 μg/m3 increase in PM1 was positively associated with pneumonia (OR 1.07, 95% CI 1.04–1.10). Our research helps evaluate the current literature to understand the public health impact better worldwide. However, the amount of research conducted globally is still minimal, so more research needs to be carried out in different regions.
Data availability
Not applicable
References
Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA (2014) Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax 69:660–665. https://doi.org/10.1136/thoraxjnl-2013-204492
Baumgartner J, Brauer M, Ezzati M (2020) The role of cities in reducing the cardiovascular impacts of environmental pollution in low- and middle-income countries. BMC Med 18:39–39. https://doi.org/10.1186/s12916-020-1499-y
Bhatt SP, Kim YI, Harrington KF, Hokanson JE, Lutz SM, Cho MH, DeMeo DL, Wells JM, Make BJ, Rennard SI, Washko GR, Foreman MG, Tashkin DP, Wise RA, Dransfield MT, Bailey WC (2018) Smoking duration alone provides stronger risk estimates of chronic obstructive pulmonary disease than pack-years. Thorax 73:414–421. https://doi.org/10.1136/thoraxjnl-2017-210722
Cao D, Li D, Wu Y, Qian ZM, Liu Y, Liu Q, Sun J, Guo Y, Zhang S, Jiao G, Yang X, Wang C, McMillin SE, Zhang X, Lin H (2021) Ambient PM(2.5) exposure and hospital cost and length of hospital stay for respiratory diseases in 11 cities in Shanxi Province, China. Thorax 76:815–820. https://doi.org/10.1136/thoraxjnl-2020-215838
Chen G, Knibbs LD, Zhang W, Li S, Cao W, Guo J, Ren H, Wang B, Wang H, Williams G, Hamm NAS, Guo Y (2018) Estimating spatiotemporal distribution of PM(1) concentrations in China with satellite remote sensing, meteorology, and land use information. Environ Pollut 233:1086–1094. https://doi.org/10.1016/j.envpol.2017.10.011
Doiron D, de Hoogh K, Probst-Hensch N, Fortier I, Cai Y, De Matteis S, Hansell AL (2019) Air pollution, lung function and COPD: results from the population-based UK Biobank study. Eur Respir J 54:1802140. https://doi.org/10.1183/13993003.02140-2018
Evangelopoulos D, Perez-Velasco R, Walton H, Gumy S, Williams M, Kelly FJ, Künzli N (2020) The role of burden of disease assessment in tracking progress towards achieving WHO global air quality guidelines. Int J Public Health 65:1455–1465. https://doi.org/10.1007/s00038-020-01479-z
Fuertes E, MacIntyre E, Agius R, Beelen R, Brunekreef B, Bucci S, Cesaroni G, Cirach M, Cyrys J, Forastiere F, Gehring U, Gruzieva O, Hoffmann B, Jedynska A, Keuken M, Klümper C, Kooter I, Korek M, Krämer U, Mölter A, Nieuwenhuijsen M, Pershagen G, Porta D, Postma DS, Simpson A, Smit HA, Sugiri D, Sunyer J, Wang M, Heinrich J (2014) Associations between particulate matter elements and early-life pneumonia in seven birth cohorts: results from the ESCAPE and TRANSPHORM projects. Int J Hyg Environ Health 217:819–829. https://doi.org/10.1016/j.ijheh.2014.05.004
GBD 2019 Diseases and Injuries Collaborators (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396:1204–1222. https://doi.org/10.1016/s0140-6736(20)30925-9
Guan WJ, Zheng XY, Chung KF, Zhong NS (2016) Impact of air pollution on the burden of chronic respiratory diseases in China: time for urgent action. Lancet 388:1939–1951. https://doi.org/10.1016/s0140-6736(16)31597-5
Gurung A, Son JY, Bell ML (2017) Particulate matter and risk of hospital admission in the Kathmandu valley, Nepal: a case-crossover study. Am J Epidemiol 186:573–580. https://doi.org/10.1093/aje/kwx135
Hamra GB, Guha N, Cohen A, Laden F, Raaschou-Nielsen O, Samet JM, Vineis P, Forastiere F, Saldiva P, Yorifuji T, Loomis D (2014) Outdoor particulate matter exposure and lung cancer: a systematic review and meta-analysis. Environ Health Perspect 122:906–911. https://doi.org/10.1289/ehp/1408092
Hassanvand MS, Naddafi K, Faridi S, Nabizadeh R, Sowlat MH, Momeniha F, Gholampour A, Arhami M, Kashani H, Zare A, Niazi S, Rastkari N, Nazmara S, Ghani M, Yunesian M (2015) Characterization of PAHs and metals in indoor/outdoor PM10/PM2.5/PM1 in a retirement home and a school dormitory. Sci Total Environ 527-528:100–110. https://doi.org/10.1016/j.scitotenv.2015.05.001
Huang K, Yang T, Xu J, Yang L, Zhao J, Zhang X, Bai C, Kang J, Ran P, Shen H, Wen F, Chen Y, Sun T, Shan G, Lin Y, Xu G, Wu S, Wang C, Wang R, Shi Z, Xu Y, Ye X, Song Y, Wang Q, Zhou Y, Li W, Ding L, Wan C, Yao W, Guo Y, Xiao F, Lu Y, Peng X, Zhang B, Xiao D, Wang Z, Chen Z, Bu X, Zhang H, Zhang X, An L, Zhang S, Zhu J, Cao Z, Zhan Q, Yang Y, Liang L, Tong X, Dai H, Cao B, Wu T, Chung KF, He J, Wang C (2019) Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet 394:407–418. https://doi.org/10.1016/s0140-6736(19)31147-x
Kim JJ, Hann T, Lee SJ (2019) Effect of flow and humidity on indoor deposition of particulate matter. Environ Pollut 255:113263. https://doi.org/10.1016/j.envpol.2019.113263
Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, Coelho M, Saldiva PHN, Lavigne E, Matus P, Valdes Ortega N, Osorio Garcia S, Pascal M, Stafoggia M, Scortichini M, Hashizume M, Honda Y, Hurtado-Díaz M, Cruz J, Nunes B, Teixeira JP, Kim H, Tobias A, Íñiguez C, Forsberg B, Åström C, Ragettli MS, Guo YL, Chen BY, Bell ML, Wright CY, Scovronick N, Garland RM, Milojevic A, Kyselý J, Urban A, Orru H, Indermitte E, Jaakkola JJK, Ryti NRI, Katsouyanni K, Analitis A, Zanobetti A, Schwartz J, Chen J, Wu T, Cohen A, Gasparrini A, Kan H (2019a) Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med 381:705–715. https://doi.org/10.1056/NEJMoa1817364
Liu F, Chen G, Huo W, Wang C, Liu S, Li N, Mao S, Hou Y, Lu Y, Xiang H (2019b) Associations between long-term exposure to ambient air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Environ Pollut 252:1235–1245. https://doi.org/10.1016/j.envpol.2019.06.033
Liu K, Li S, Qian Z, Dharmage SC, Bloom MS, Heinrich J, Jalaludin B, Markevych I, Morawska L, Knibbs LD, Hinyard L, Xian H, Liu S, Lin S, Leskinen A, Komppula M, Jalava P, Roponen M, Hu L-W, Zeng X-W, Hu W, Chen G, Yang B-Y, Guo Y, Dong G-H (2020) Benefits of influenza vaccination on the associations between ambient air pollution and allergic respiratory diseases in children and adolescents: new insights from the seven northeastern cities study in China. Environ Pollut 256:113434. https://doi.org/10.1016/j.envpol.2019.113434
Luong LM, Phung D, Sly PD, Morawska L, Thai PK (2016) The association between particulate air pollution and respiratory admissions among young children in Hanoi, Vietnam. Sci Total Environ 578:249–255. https://doi.org/10.1016/j.scitotenv.2016.08.012
Luong LMT, Sly PD, Thai PK, Phung D (2019) Impact of ambient air pollution and wheeze-associated disorders in children in Southeast Asia: a systematic review and meta-analysis. Rev Environ Health 34:125–139. https://doi.org/10.1515/reveh-2018-0079
Lyall K, Croen L, Daniels J, Fallin MD, Ladd-Acosta C, Lee BK, Park BY, Snyder NW, Schendel D, Volk H, Windham GC, Newschaffer C (2017) The changing epidemiology of autism spectrum disorders. Annu Rev Public Health 38:81–102. https://doi.org/10.1146/annurev-publhealth-031816-044318
Mazzarella G, Esposito V, Bianco A, Ferraraccio F, Prati MV, Lucariello A, Manente L, Mezzogiorno A, De Luca A (2012) Inflammatory effects on human lung epithelial cells after exposure to diesel exhaust micron sub particles (PM1.0) and pollen allergens. Environ Pollut 161:64–69. https://doi.org/10.1016/j.envpol.2011.09.046
Michaud JP, Grove JS, Krupitsky D (2004) Emergency department visits and "vog"-related air quality in Hilo, Hawai'i. Environ Res 95:11–19. https://doi.org/10.1016/s0013-9351(03)00122-1
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj 339:b2535. https://doi.org/10.1136/bmj.b2535
Naidja L, Ali-Khodja H, Khardi S (2018) Sources and levels of particulate matter in North African and sub-Saharan cities: a literature review. Environ Sci Pollut Res Int 25:12303–12328. https://doi.org/10.1007/s11356-018-1715-x
Ostro B, Roth L, Malig B, Marty M (2009) The effects of fine particle components on respiratory hospital admissions in children. Environ Health Perspect 117:475–480. https://doi.org/10.1289/ehp.11848
Pun VC, Kazemiparkouhi F, Manjourides J, Suh HH (2017) Long-term PM2.5 exposure and respiratory, cancer, and cardiovascular mortality in older US adults. Am J Epidemiol 186:961–969. https://doi.org/10.1093/aje/kwx166
Quansah R, Semple S, Ochieng CA, Juvekar S, Armah FA, Luginaah I, Emina J (2017) Effectiveness of interventions to reduce household air pollution and/or improve health in homes using solid fuel in low-and-middle income countries: a systematic review and meta-analysis. Environ Int 103:73–90. https://doi.org/10.1016/j.envint.2017.03.010
Sicard P, Khaniabadi YO, Perez S, Gualtieri M, De Marco A (2019) Effect of O(3), PM(10) and PM(2.5) on cardiovascular and respiratory diseases in cities of France, Iran and Italy. Environ Sci Pollut Res Int 26:32645–32665. https://doi.org/10.1007/s11356-019-06445-8
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (MOOSE) group. Jama 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Tian F, Qi J, Wang L, Yin P, Qian ZM, Ruan Z, Liu J, Liu Y, McMillin SE, Wang C, Lin H, Zhou M (2020) Differentiating the effects of ambient fine and coarse particles on mortality from cardiopulmonary diseases: a nationwide multicity study. Environ Int 145:106096. https://doi.org/10.1016/j.envint.2020.106096
Valavanidis A, Fiotakis K, Vlachogianni T (2008) Airborne particulate matter and human health: toxicological assessment and importance of size and composition of particles for oxidative damage and carcinogenic mechanisms. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev 26:339–362. https://doi.org/10.1080/10590500802494538
Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, Kang J, Ran P, Shen H, Wen F, Huang K, Yao W, Sun T, Shan G, Yang T, Lin Y, Wu S, Zhu J, Wang R, Shi Z, Zhao J, Ye X, Song Y, Wang Q, Zhou Y, Ding L, Yang T, Chen Y, Guo Y, Xiao F, Lu Y, Peng X, Zhang B, Xiao D, Chen CS, Wang Z, Zhang H, Bu X, Zhang X, An L, Zhang S, Cao Z, Zhan Q, Yang Y, Cao B, Dai H, Liang L, He J (2018) Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China pulmonary health [CPH] study): a national cross-sectional study. Lancet 391:1706–1717. https://doi.org/10.1016/s0140-6736(18)30841-9
Wang W, Mao F, Zou B, Guo J, Wu L, Pan Z, Zang L (2019) Two-stage model for estimating the spatiotemporal distribution of hourly PM1.0 concentrations over central and east China. Sci Total Environ 675:658–666. https://doi.org/10.1016/j.scitotenv.2019.04.134
Wang J, Li Y, Zhao P, Tian Y, Liu X, He H, Jia R, Oliver BG, Li J (2020) Exposure to air pollution exacerbates inflammation in rats with preexisting COPD. Mediat Inflamm 2020:4260204. https://doi.org/10.1155/2020/4260204
Wang HL, Sun J, Qian ZM, Gong YQ, Zhong JB, Yang RD, Wan CL, Zhang SQ, Ning DF, Xian H, Chang JJ, Wang CJ, Shacham E, Wang JQ, Lin HL (2021a) Association between air pollution and atopic dermatitis in Guangzhou, China: modification by age and season. Br J Dermatol 184:1068–1076. https://doi.org/10.1111/bjd.19645
Wang X, Xu Z, Su H, Ho HC, Song Y, Zheng H, Hossain MZ, Khan MA, Bogale D, Zhang H, Wei J, Cheng J (2021b) Ambient particulate matter (PM1, PM2.5, PM10) and childhood pneumonia: the smaller particle, the greater short-term impact? Sci Total Environ 772:145509. https://doi.org/10.1016/j.scitotenv.2021.145509
Ward-Caviness CK (2019) A review of gene-by-air pollution interactions for cardiovascular disease, risk factors, and biomarkers. Hum Genet 138:547–561. https://doi.org/10.1007/s00439-019-02004-w
Yang D, Yang X, Deng F, Guo X (2017) Ambient air pollution and biomarkers of health effect. In: Dong G-H (ed) Ambient Air pollution and health impact in China. Springer Singapore, Singapore, pp 59–102
Yang M, Chu C, Bloom MS, Li S, Chen G, Heinrich J, Markevych I, Knibbs LD, Bowatte G, Dharmage SC, Komppula M, Leskinen A, Hirvonen MR, Roponen M, Jalava P, Wang SQ, Lin S, Zeng XW, Hu LW, Liu KK, Yang BY, Chen W, Guo Y, Dong GH (2018) Is smaller worse? New insights about associations of PM(1) and respiratory health in children and adolescents. Environ Int 120:516–524. https://doi.org/10.1016/j.envint.2018.08.027
Yang Y, Qi J, Ruan Z, Yin P, Zhang S, Liu J, Liu Y, Li R, Wang L, Lin H (2020) Changes in life expectancy of respiratory diseases from attaining daily PM2.5 Standard in China: a nationwide observational study. Innovation 1:100064. https://doi.org/10.1016/j.xinn.2020.100064
Yao C, Wang Y, Williams C, Xu C, Kartsonaki C, Lin Y, Zhang P, Yin P, Lam KBH (2020) The association between high particulate matter pollution and daily cause-specific hospital admissions: a time-series study in Yichang, China. Environ Sci Pollut Res Int 27:5240–5250. https://doi.org/10.1007/s11356-019-06734-2
Yu H, Guo Y, Zeng X, Gao M, Yang BY, Hu LW, Yu Y, Dong GH (2020) Modification of caesarean section on the associations between air pollution and childhood asthma in seven Chinese cities. Environ Pollut 267:115443. https://doi.org/10.1016/j.envpol.2020.115443
Zhang Y, Ding Z, Xiang Q, Wang W, Huang L, Mao F (2020) Short-term effects of ambient PM(1) and PM(2.5) air pollution on hospital admission for respiratory diseases: case-crossover evidence from Shenzhen, China. Int J Hyg Environ Health 224:113418. https://doi.org/10.1016/j.ijheh.2019.11.001
Zhang Y, Wei J, Shi Y, Quan C, Ho HC, Song Y, Zhang L (2021) Early-life exposure to submicron particulate air pollution in relation to asthma development in Chinese preschool children. J Allergy Clin Immunol S0091-6749:00359–00356. https://doi.org/10.1016/j.jaci.2021.02.030
Zou W, Wang X, Hong W, He F, Hu J, Sheng Q, Zhu T, Ran P (2020) PM2.5 Induces the expression of inflammatory cytokines via the Wnt5a/Ror2 pathway in human bronchial epithelial cells. Int J Chron Obstruct Pulmon Dis 15:2653–2662. https://doi.org/10.2147/copd.S270762
Funding
This study was supported by National Natural Science Foundation of China (No. 82003559), Nature Science Foundation of Capital Medical University (No. PYZ2018046), and Beijing Municipal Training Project of Excellent Talents. The funding was neither used for the study design nor data collection but to cover for the publication fees.
Author information
Authors and Affiliations
Contributions
Conceptualization: Mengqiu Wu. Methodology: Yaoyu Hu. Literature search: Yaoyu Hu; Mengqiu Wu; Yutong Li. Formal data analysis and investigation: Yaoyu Hu; Mengqiu Wu. Writing — original draft preparation: Yaoyu Hu; Mengqiu Wu. Writing — critically revised the work: Yaoyu Hu; Mengqiu Wu; Yutong Li; Xiangtong Liu. Funding acquisition: Xiangtong Liu. Resources: Xiangtong Liu. Supervision: Xiangtong Liu
Corresponding author
Ethics declarations
Ethics approval
Not applicable
Consent to participate
Not applicable
Consent for publication
All listed authors have approved the manuscript before submission, including the names and order of authors.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 65.7 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hu, Y., Wu, M., Li, Y. et al. Influence of PM1 exposure on total and cause-specific respiratory diseases: a systematic review and meta-analysis. Environ Sci Pollut Res 29, 15117–15126 (2022). https://doi.org/10.1007/s11356-021-16536-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16536-0