Abstract
Links between environmental chemicals and human health have emerged over the last few decades, but the effects from polyaromatic hydrocarbons were less studied, compared to other commonly known environmental chemicals such as heavy metals, phthalates, arsenic, phenols, pesticides, etc. Therefore, the aim of the study was to examine the relationships of urinary polyaromatic hydrocarbons and adult respiratory health conditions using a large human sample in a national and population-based setting in recent years. Data were retrieved from United States National Health and Nutrition Examination Surveys, 2011–2012 including demographics, self-reported health conditions, and urinary polyaromatic hydrocarbons. Statistical analyses including chi-square test, t test, and survey-weighted logistic regression modeling were performed. Of 5560 American adults aged 20–80, urinary 2-hydroxyfluorene and 3-hydroxyfluorene were positively associated with emphysema (OR, 1.60, 95 % CI 1.26 to 2.03, P = 0.001 and OR, 1.42, 95 % CI 1.15 to 1.77, P = 0.003, respectively) and chronic bronchitis (OR, 1.42, 95 % CI 1.04 to 1.94, P = 0.031 and OR, 1.40, 95 % CI 1.03 to 1.91, P = 0.036, respectively), while 2-hydroxynaphthalene (2-naphthol) was likely to be borderline associated with emphysema and chronic bronchitis. Conversely, urinary 1-hydroxyphenanthrene, 3-hydroxyphenanthrene, 1-hydroxypyrene, and 4-hydroxyphenanthrene were inversely associated with asthma and infections. Urinary polyaromatic hydrocarbons are associated with adult respiratory health conditions, although the causality cannot be established. For future research, studies using large human sample across regions to longitudinally monitor would be suggested. For practice and policy-making, regulation on minimizing polyaromatic hydrocarbons exposure to protect respiratory health might need to be considered in future health and environmental policies and intervention programs.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Evidence before this study
Links between environmental chemicals and human health including self-rated health, hypertension, cardiovascular disease, food allergy, oral health, emotional support, and cognitive function in American adults have emerged in Americans (Shiue 2015a; Shiue 2015b; Shiue 2015c; Shiue 2015d; Shiue 2015e; Shiue 2014; Shiue 2013a; Shiue 2013b; Shiue 2013c), but the effects from polyaromatic hydrocarbons (PAHs) were less studied, compared to other commonly known environmental chemicals such as heavy metals, arsenic, phenols, phthalates, etc. PAHs constitute a group of chemicals that people could be exposed via vehicle exhausts, asphalt, coal tar, wild fires, agricultural burning, soil, charbroiled foods, and tobacco smoke. Approximately, everyone could be exposed to PAHs on a daily basis from multiple sources. PAH pollution may have significant health implications, and the extent of damage to organisms from PAH exposure could be dependent on several factors including degrees and types of PAH exposure (Ball and Truskewycz 2013).
Knowledge gap
Previously, animal models under a laboratory condition using rodents showed that exposure to PAHs adversely affected immunologic health (Luebke et al. 1997). However, research in this topic from human sample has not been well conducted. Providing evidence using human sample might help environmental health promotion in the next few years. Recently, associations of PAHs and cardiovascular, oral, emotional, and self-rated health have been observed (Shiue 2015a; Shiue 2015b; Shiue 2015c; Shiue 2015d; Shiue 2015e), but those on respiratory health have not been documented.
Study aim
Following this context, therefore, the aim of the present study was to examine the relationships of urinary PAHs and adult respiratory conditions using a large human sample in a national and population-based setting in recent years.
Methods
Study sample
As described elsewhere (Centers for Disease Control and Prevention 2012), United States National Health and Nutrition Examination Surveys (NHANES) has been a national, population-based, multi-year, cross-sectional study. Study samples are representative sample of the civilian, non-institutionalized US population. Information on demographics (more details via http://wwwn.cdc.gov/nchs/nhanes/2011-2012/DEMO_G.htm), serum cotinine (more details via http://wwwn.cdc.gov/nchs/nhanes/2011-2012/COTNAL_G.htm), and self-reported respiratory health conditions (more details via http://wwwn.cdc.gov/nchs/nhanes/2011-2012/MCQ_G.htm) was obtained by household interview using questionnaires. In the current analysis, the 2011–2012 study cohort as the most recent wave with data on urinary PAHs was selected. Informed consents were obtained from participating subjects by the NHANES researchers.
Biomonitoring
Urines were only collected in a subsample, being one third of the whole study cohort with representation (more details via http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/homeurine.pdf), to measure environmental chemical concentrations in urines among people aged 6 and above (more details via http://www.cdc.gov/nchs/nhanes/nhanes2011-2012/labdoc_g.htm). Urine specimens from urinary polyaromatic hydrocarbon were processed, stored under appropriate frozen (−20 °C) conditions, and shipped to the Division of Environmental Health Laboratory Sciences, National Center for Environmental Health, Centers for Disease Control and Prevention for analysis. According to the NHANES website (more details via http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/PAH_G_met.pdf), the procedure involved enzymatic hydrolysis of glucuronidated/sulfated OH-polyaromatic hydrocarbon metabolites in urine, extraction, derivatization, and analysis using isotope dilution capillary gas chromatography tandem mass spectrometry (GC-MS/MS). Ion transitions specific to each analyte and carbon-13-labeled internal standards are monitored, and the abundances of each ion are measured. Since urinary hydrocarbon concentrations were highly skewed, they were all log transformed when carrying out the statistical analyses.
Variables and analysis
Adults aged 20 and above were included in the current statistical analysis since chronic diseases were commonly reported in adults. Associations of urinary PAHs and adult self-reported respiratory health conditions were examined by using t test and survey-weighted logistic regression model, presenting with mean values, odds ratios (OR), and 95 % confidence intervals (CI). Covariates including urinary creatinine, age, sex, ratio of family income to poverty (proxy of socioeconomic status), body mass index, education level, serum cotinine (biomarker of smoking status), alcohol status, and physical activity level were adjusted. Statistical software STATA version 13.0 (STATA, College Station, Texas, USA) was used to perform all the statistical analyses.
Ethics consideration
Since there is only secondary data analyses employed without any participant personal information identified by extracting statistical data from the NHANES website in the present study, no further ethics approval for conducting the present study is required (more details via http://www.ethicsguidebook.ac.uk/Secondary-analysis-106).
Results
Descriptive statistics
Of 5560 American adults aged 20–80 and included in the statistical analysis, their characteristics are shown in Table 1. The presence of different respiratory health conditions in the American adult population varied and is accordingly presented in Table 2.
Analytical statistics
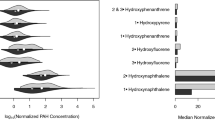
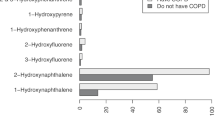
In Tables 3, 4, 5, 6, 7, 8, 9, 10, 11, and 12, associations of 10 urinary PAHs and adult respiratory health conditions are listed separately. In general, urinary PAHs were higher in people with emphysema or chronic bronchitis but lower in people with asthma or infections. No associations were found between urinary PAHs and wheezing, coughing, and hay fever. Specifically, urinary 2-hydroxyfluorene and 3-hydroxyfluorene were positively associated with emphysema (OR, 1.60, 95 % CI 1.26 to 2.03, P = 0.001 and OR, 1.42, 95 % CI 1.15 to 1.77, P = 0.003, respectively) and chronic bronchitis (OR, 1.42, 95 % CI 1.04 to 1.94, P = 0.031 and OR, 1.40, 95 % CI 1.03 to 1.91, P = 0.036, respectively), while 2-hydroxynaphthalene (2-naphthol) was likely to be borderline associated with emphysema (OR, 1.20, 95 % CI 0.82 to 1.75, P = 0.332) and chronic bronchitis (OR, 1.32, 95 % CI 1.02 to 1.72, P = 0.038). Conversely, urinary 1-hydroxyphenanthrene, 3-hydroxyphenanthrene, 1-hydroxypyrene, and 4-hydroxyphenanthrene were inversely associated with asthma and infections.
Discussion
PAHs, emphysema, and chronic bronchitis
In animal studies, bitumen fumes or traffic exposure releasing hydrocarbons were observed to result in emphysema in rats (Gate et al. 2006; Wang et al. 1992). However, evidence from human sample was lacking. Consistent with the findings in the animal studies mentioned above, the present study has provided epidemiological evidence on the relationship of PAHs and emphysema from a large human sample. Moreover, the link between PAHs and adult chronic bronchitis has been continuously documented. Previous evidence was obtained in 598 Brazilian male workers (Mendonça et al. 2007), 211 Swedish loggers (Hagberg et al. 1985), and 138 Polish steel mill workers (Kolarzyk et al. 2000). Again, consistent with these studies, the present study has further provided epidemiological evidence drawn from the general population to report such association.
PAHs, asthma, and infections
The link of PAHs and asthma has not been established and that of PAHs and infections has not been well documented as well. Similar to a previous study in 184 American volunteers showing urinary 1-hydroxypyrene was observed to be less in people with hepatitis virus infection (Johnson et al. 2010), the present study also presented the inverse associations of 1-hydroxyphenanthrene, 3-hydroxyphenanthrene, 1-hydroxypyrene, and 4-hydroxyphenanthrene and infections in the general population. However, the mechanism is unknown and would need longitudinal and/or experimental research to confirm or refute the finding.
Strengths and limitations
The present study has a few strengths. Firstly, this study was conducted in a large and nationally representative human sample with mixed ethnicities and socioeconomic status. Secondly, this is the first time to examine the effects of urinary hydrocarbon concentrations on adult respiratory health conditions by symptoms. However, there are also a few limitations that cannot be ignored. First, there could be still other emerging chemicals from the living environments through different channels/vehicles that we might not yet know and would need future research to further identify and examine. Second, causality cannot be established in the present study due to the cross-sectional study design in nature. Taken together, future studies retaining the strengths and overcoming the limitations with a longitudinal and/or experimental study design to confirm or refute the current findings and, if at all, to understand the persisting effects along the life course from early years to old age would be recommended.
Directions for future research, practice, and policy
In conclusion, urinary PAHs were positively associated with emphysema and chronic but inversely associated with asthma and infections. There were no associations between urinary PAHs and wheezing, coughing, and hay fever found. For future research, studies using large human sample across regions to longitudinally monitor would be suggested. For practice and policy-making, regulation on minimizing polyaromatic hydrocarbons exposure to protect respiratory health might need to be considered in future health and environmental policies and intervention programs.
References
Ball A, Truskewycz A (2013) Polyaromatic hydrocarbon exposure: an ecological impact ambiguity. Environ Sci Pollut Res Int 20:4311–4326
Centers for Disease Control and Prevention (CDC) (2012) National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, http://www.cdc.gov/nchs/nhanes.htm
Gate L, Langlais C, Micillino JC, Nunge H, Bottin MC, Wrobel R, Binet S (2006) Bitumen fume-induced gene expression profile in rat lung. Toxicol Appl Pharmacol 215:83–92
Hagberg M, Kolmodin-Hedman B, Lindahl R, Nilsson CA, Norström A (1985) Irritative complaints, carboxyhemoglobin increase and minor ventilatory function changes due to exposure to chain-saw exhaust. Eur J Respir Dis 66:240–247
Johnson NM, Qian G, Xu L, Tietze D, Marroquin-Cardona A, Robinson A, Rodriguez M, Kaufman L, Cunningham K, Wittmer J, Guerra F, Donnelly KC, Williams JH, Wang JS, Phillips TD (2010) Aflatoxin and PAH exposure biomarkers in a U.S. population with a high incidence of hepatocellular carcinoma. Sci Total Environ 408:6027–6031
Kolarzyk E, Stepniewski M, Zapolska I (2000) Occurrence of pulmonary diseases in steel mill workers. Int J Occup Med Environ Health 13:103–112
Luebke RW, Hodson PV, Faisal M, Ross PS, Grasman KA, Zelikoff J (1997) Aquatic pollution-induced immunotoxicity in wildlife species. Fundam Appl Toxicol 37:1–15
Mendonça EM, Silva RC, Bussacos MA, Algranti E (2007) Respiratory impairment in Brazilian foundry workers exposed to sand. Am J Ind Med 50:83–91
Shiue I (2013a) Urine phthalate concentrations are higher in people with stroke: United States National Health and Nutrition Examination Surveys (NHANES), 2001-2004. Eur J Neurol 20:728–731
Shiue I (2013b) Association of urinary arsenic, heavy metal, and phthalate concentrations with food allergy in adults: National Health and Nutrition Examination Survey, 2005-2006. Ann Allergy Asthma Immunol 111:421–423
Shiue I (2013c) Urinary environmental chemical concentrations and vitamin D are associated with vision, hearing, and balance disorders in the elderly. Environ Int 53:41–46
Shiue I (2014) Higher urinary heavy metal, phthalate, and arsenic but not parabens concentrations in people with high blood pressure, U.S. NHANES, 2011-2012. Int J Environ Res Public Health 11:5989–5899
Shiue I (2015a) Urinary arsenic, heavy metals, phthalates, pesticides, polyaromatic hydrocarbons but not parabens, polyfluorinated compounds are associated with self-rated health: USA NHANES, 2011-2012. Environ Sci Pollut Res Int 22(12):9570–9574
Shiue I (2015b) Are urinary polyaromatic hydrocarbons associated with adult hypertension, heart attack, and cancer? USA NHANES, 2011-2012. Environ Sci Pollut Res Int. doi:10.1007/s11356-015-4922-8
Shiue I (2015c) Urinary heavy metals, phthalates, phenols, thiocyanate, parabens, pesticides, polyaromatic hydrocarbons but not arsenic or polyfluorinated compounds are associated with adult oral health: USA NHANES, 2011-2012. Environ Sci Pollut Res Int. doi:10.1007/s11356-015-4749-3
Shiue I (2015d) Arsenic, heavy metals, phthalates, pesticides, hydrocarbons and polyfluorinated compounds but not parabens or phenols are associated with adult remembering condition: US NHANES, 2011-2012. Environ Sci Pollut Res Int 22(8):6381–6386
Shiue I (2015e) Urinary parabens and polyaromatic hydrocarbons independent of health conditions are associated with adult emotional support needs: USA NHANES, 2005-2008. Environ Sci Pollut Res Int. doi:10.1007/s11356-015-4561-0
Wang JM, Ueng TH, Lin JK (1992) Biochemical and morphological alterations in the lungs and livers of mice following exposure to polluted air in a traffic tunnel. Proc Natl Sci Counc Repub China B 16:77–83
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she has no competing interests.
Additional information
Responsible editor: Philippe Garrigues
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shiue, I. Urinary polyaromatic hydrocarbons are associated with adult emphysema, chronic bronchitis, asthma, and infections: US NHANES, 2011–2012. Environ Sci Pollut Res 23, 25494–25500 (2016). https://doi.org/10.1007/s11356-016-7867-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-016-7867-7