Abstract
Background
Although outdoor water sport activities are gaining increasing attention for their therapeutic potential in the social and care management of populations with chronic diseases, these practices are currently underutilised. Moreover, the available body of literature on the topic has not been critically and comprehensively assessed yet.
Aims
(1) To appraise the health effects of outdoor water sport activities for chronic disease populations; (2) to preliminarily assess the potential size and scope of the available research literature for this emerging field and identify potential gaps and avenues of development.
Methods
A literature search was performed scanning PubMed (including MEDLINE), Physiotherapy Evidence Database (PEDro) and Scopus from inception to December 2021. A scoping review was carried out by appraising all the available evidence on outdoor water sport interventions specifically designed for therapeutic purposes for individuals with chronic disease. The quality score of each study was calculated with the Tool for the assEssment of Study qualiTy and reporting in Exercise (TESTEX) tool.
Results
Fifteen studies (five RCTs, seven non-RCTs and three CTs with healthy subjects as controls) met the inclusion criteria and were assessed. Among the studies selected, two focused on canoa kayak, one on stand-up paddle, two on surfing, two on sailing activity, and eight on dragon boat padding. The median TESTEX score for study quality and reporting was 6/15, i.e., “very low” (range 5–8). Based on the qualitative analysis, the few individual studies that could be included reported generally positive results, ranging from improvements in antioxidant action and cardiovascular function for dragon boating, to beneficial effects on balance, postural control, and flexibility for on-water paddle board activities. Overall, outdoor water sport interventions were associated to higher rates of adherence than conventional trainings.
Conclusions
Very low to low quality evidence from a limited set of pilot studies seems to suggest beneficial effects of outdoor water sports for chronic disease populations. However, such preliminary findings need to be replicated through large, high-quality RCTs to be conducted in target populations. Avenues of development, scoping directions and translational perspectives for this specific research field are proposed and discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Evidence is accumulating on the potential benefits of outdoor sports in natural environments on physical and mental wellbeing [1,2,3]. Overall, natural environments are associated to multi-domain positive effects, which seem to add to the benefits brought by physical activity. Thompson et al. [2] confirmed such hypothesis in their systematic review comparing the effects of indoor and outdoor activity programmes. The main effects reported by subjects participating in outdoor sport activities ranged from increased perception of health and vitality to reduced tension, anger, and depression [3]. Social benefits [4, 5] including increased participation, sense of community and active citizenship [6, 7] were also demonstrated following this type of activity. In this perspective, outdoor sports in natural environments would provide participants with the opportunity to pursue psychophysical health benefits and, importantly, to connect with nature and peers [4,5,6,7].
A specific research line is, thus, shaping, with a focus on outdoor blue spaces, defined by the European Commission project BlueHealth as “outdoor environments—either natural or manmade—that prominently feature water and are accessible to humans either proximally (being in, on, or near water) or distally/virtually (being able to see, hear or otherwise sense water)” (https://bluehealth2020.eu/) [8]. In this context, the recreational and amateur practice of outdoor water sport activities is increasing in popularity, partly because many of these activities are long part of the Olympic programme, or have been recently included (e.g., surf in Tokyo 2021), or will be added in the next Olympic appointment (e.g., kitesurf in Paris 2024).
Outdoor water sport activities incorporate the abovementioned benefits of exercising in outdoor environments with those inherent to aquatic exercise. Regarding the latter, in their recent systematic review on conventional aquatic exercise for adults with chronic diseases [9], Faíl and colleagues reported improvements ranging from small-moderate to large on several symptomatic and functional outcome measures in patients with bone diseases (pain, balance, flexibility, and strength), coronary artery disease (strength and anthropometry), diabetes (balance and quality of life), fibromyalgia (in balance and cardiorespiratory fitness), hypertension (quality of life), multiple sclerosis (quality of life and balance), Parkinson's disease (pain, gait, cardiorespiratory fitness, and quality of life), and stroke (quality of life). Such benefits, both physiological and psychosocial, are provided by outdoor water sports in a unique manner, providing a sense of group cohesion with others, often teammates with the same competition objective, who share the same visual natural view [4]. Needless to say, outdoor water sports exercise help participants overcome physical limitations, with the water physically embracing them allowing to engage in physical activity when land-based exercise may not be as feasible.
The synergistic combination of aquatic activities carried out in outdoor environments with competitive goals associated is also gaining increasing attention in a translational perspective for its therapeutic potential, especially in the secondary and tertiary prevention of chronic disease-related disability progress.
According to the Medical Subject Headings (MeSH) of the National Library of Medicine (https://www.ncbi.nlm.nih.gov/mesh/?term=chronic+disease), chronic diseases are conditions that have one or more of the following characteristics: they are permanent, leave residual disability, are caused by non-reversible pathological alterations, require special training of the patient for rehabilitation, or may be expected to require a long period of supervision, observation, or care. For epidemiological studies the term ‘chronic disease’ often includes heart diseases, cancer, diabetes (diabetes mellitus, type 2), stroke and other chronic neurological conditions including Parkinson’s disease and multiple sclerosis. For these selected populations, outdoor water sports activities may represent non-conventional and appealing strategies to prevent reinjury or recurrence, potentially contributing to return people to their original health or to regain as much function as possible, and prevent long-term problems, as well. Engaging in team sports activities as is the case of many outdoor water activities like, among others, kayaking and dragon boating, can also facilitate social participation, support from and aggregation with the teammates, who share common challenges and understanding of the main issues of living with chronic conditions. According to the 2007 qualitative study by Sabiston and colleagues in breast cancer survivors [10], experiences as members of dragon boat teams provided “opportunities to (re)gain a sense of personal control, develop new identities as athletes, and overcome physical challenges.” Accordingly, evidence from other survey-based qualitative studies and the only available narrative review on the topic revealed significant benefit on psychological distress and quality of life following water sports such as sailing, kayaking and dragon boat in cancer survivors [10,11,12]. The choice of a natural environment such as a blue/green gym may represent an added value and an enjoyable alternative to the conventional forms of indoor exercise.
Despite the promising effects emerging for outdoor water sport activities as novel approaches to prevent and manage disability secondary to chronic disease, to the best of our knowledge no critical appraisal of the potential size and scope of the extant literature on the topic has been carried out so far. This seems a necessary step in the perspective to provide sports professionals, clinicians, and patients with a detailed and unbiased account of the translational opportunities that might be offered by these relatively novel activities. However, it should also be pointed out that much of the available literature consists of qualitative studies where patients were generally interviewed about their personal experience and subjective feelings towards the activity. While patient’s point of view is undoubtedly the priority, gathering information about the objective effects (i.e., on gait, cardiorespiratory performance, muscle strength, balance, etc.) of outdoor water sports is also a worth endeavour.
Based on the above background and rationale, we planned a critical scoping review of the available evidence. By the present knowledge synthesis, we specifically aimed at (1) appraising the health effects of outdoor water sport activities for chronic disease populations; (2) identifying potential gaps and future avenues of development for this emerging research field.
Methods
Study design and search strategy
The 2018 Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA) extension for scoping reviews was followed [13], and the study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) (May 2021), with the registration number CRD42021246993. A literature search was conducted over the following databases: PubMed (including MEDLINE), Physiotherapy Evidence Database (PEDro) and Scopus. All the search terms and filters were adapted to each database that was searched from the earliest record up to December 31, 2021. A detailed search strategy with the keywords used can be found in the Supplementary file 1. Reference lists from all included studies and any thematic reviews on this field were screened to identify further pertinent articles.
Eligibility criteria
Studies were included if they met the following inclusion criteria based on the PICO model [14] (i) population: persons affected by chronic diseases [15] including heart diseases, cancer, diabetes (diabetes mellitus, type 2), congenital disabilities, mental health, stroke and other chronic neurological conditions such as, but not limited to, Parkinson’s disease and multiple sclerosis; (ii) intervention: studies employing mid- to long-term outdoor water sport continuous programmes (defined as ≥ 4 weeks with a frequency of at least one session/week); (iii) comparisons: presence of at least one comparison/control group of patients with the same condition or, alternatively, at least a control group of healthy subjects; (iv) outcomes: analyses of validated and quantitative outcome measures relating to quality of life, mobility, gait and overall functioning, balance, fitness and cardiorespiratory performance, muscle strength, hematic determinations, and psychosocial functioning; (v) only randomized controlled trials (RCTs), non-randomized controlled trials (non-RCTs) with at least a patient control group, non-randomized controlled trials having healthy participants as control subjects were considered for inclusion. Abstracts, conference papers, case reports, case–control studies, observational trials with only one intervention group, review articles or studies which did not include a comparative/control group were excluded. Studies were also excluded if the full text was in a language other than English.
Study selection, data extraction, data synthesis and quality assessment
Titles and abstracts of selected articles were independently evaluated by two authors (LC and MM). Duplicates and records outside the scope of the study were removed at the preliminary stage of the screening. Eligible studies were included based on the information reported in their full texts. Any disagreement between the two authors was resolved by mutual discussion to reach consensus. In case of irreconcilable controversy, the opinion of a third author (PB) was sought. A predefined data extraction form was filled by the two authors (LC and MM) independently, containing information on the author/s’ name/s, publication year and country, study design, population characteristics, demographics, description of the specific outdoor water sport activity and program features, main outcomes and findings, dropout/adherence data and quality score of the study. To this regard, the total quality score for each study was calculated by employing the Tool for the assEssment of Study qualiTy and reporting in Exercise (TESTEX) tool [16]. The TESTEX scale uses 12 criteria (e.g., eligibility criteria specified, randomization specified, allocation concealment, etc.), with some criteria having more than one possible point, for a maximum score of 15 points (5 points for study quality and 10 points for reporting), and a total score ranging from one to 15 points (a higher score corresponds to a higher methodological study quality). This instrument is considered a useful and specific checklist for the assessment of study quality and reporting in exercise training trials [16].
If not otherwise specified, values are expressed as mean ± standard deviation (SD).
Results
Search results and qualitative synthesis
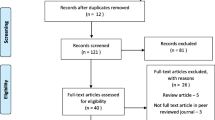
The PRISMA flow chart showing the study selection process is reported in Fig. 1.
Fifteen studies met the inclusion criteria and were included [17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]: five RCTs [18, 19, 21,22,23], seven non-RCTs [20, 25, 26, 28,29,30,31], and three CTs with healthy control groups [17, 24, 27]. The 15 selected studies were published between 2004 and 2021 and enrolled a total of 1045 individuals, comprising 280 men (26.8%) and 645 women (61.7%). In one study (120 subjects, 11.5%), gender composition was not disclosed [25]. Of the 15 studies selected, 2 focused on canoa kayak [17, 18] 1 on stand-up paddle (SUP) [19], 2 on surfing [20, 21], 2 on sailing [22, 23], and 8 on dragon boat padding [24,25,26,27,28,29,30,31]. Three studies were conducted in people affected by mental health disorders [21,22,23], seven in cancer survivors (among these, six studies focused on women with breast cancer, BC) [25,26,27,28,29,30,31], one study in patients with cardiac and non-cardiac transplants [24], one in children with congenital disabilities [20], two studies in persons with neurological diseases, such as spinal cord injury (SCI) [19] and Parkinson’s disease, PD [18], while one enrolled healthy older adults [19]. The median TESTEX score for study quality and reporting was 6/15 (range 5–8), indicating “very low” to “low” methodological quality of the studies. This was predominantly due to the following TESTEX criteria: lack of randomization specified, allocation concealment, ‘intention-to-treat’ analysis, point measures and measures of variability for all reported outcome measures and relative exercise intensity remained constant.
No meta-analyses could be performed because none of the five RCTs retrieved [18, 19, 21,22,23] shared data on at least one similar outcome achieved from comparable populations.
Table 1 summarizes the main characteristics and findings of the included studies.
Kayaking, stand-up paddle and surfing
Two studies, one CT with healthy control group [17] and one RCT [18], examined the effects of kayak training performed in open sea. The study by Grigorenko et al. [17] (TESTEX score 5/15) compared the effects of a kayaking program carried out by persons with SCI and by healthy controls on balance control. Data showed a significant yet slight decrease in sagittal body sway (i.e., reduced median frequency of the acceleration of the center of pressure on the sagittal plane) in persons with SCI [17]. Likewise, the RCT by Shujaat et al. [18] (TESTEX score 8/15), which examined the axial rigidity and bed mobility in people with PD, reported slight but significantly larger improvements in truck rotation (e.g., cervical spine left rotation + 14.3 vs. + 8.42; cervical spine right rotation + 13.58 vs. + 8.46) and axial rigidity (e.g., MPAS III bed mobility + 2.88 vs. + 2.63) following a kayak training program compared with a general exercise training. Balance performance was also the focus of the RCT by Osti et al. [19] (TESTEX score 8/15), who showed the superiority of an eight-week SUP seawater training compared to a group-walking program of the same duration in reducing body sway amplitude, both anteroposterior and mediolateral in a population of older individuals. One non-RCT and one RCT focused on surf therapy in children affected by congenital disabilities [20] and in children and adolescents diagnosed with mental health disorders [21], respectively. Both studies reported beneficial effects of surf therapy. In particular, the non-RCT by Clapham et al. (TESTEX score 6/15) [20], who compared surf therapy to unstructured pool-playgroup, showed moderate to large effects on body strength, cardiorespiratory fitness, and body composition, only in the participants who engaged in the surf program [20]. The RCT by Pereira et al. (TESTEX score 8/15) [21] showed significant reductions in the total emotional and behavioural problems, and a significant increase of youth pro-social behaviour and quality of life only in those children and adolescents with mental health disorders who had participated in surfing activities compared to the waiting list group.
Sailing
Two RTCs [22, 23] from the same research group and carried out in the same sample of participants examined the effects of a sailing program for adults with severe mental health disorders. Self-efficacy and social functioning were found significantly improved in the training group compared to the waiting list group. The TESTEX score for these studies was 7/15.
Dragon boat padding
Eight studies (six non-RCTs and two CTs with healthy control groups) examined the effects of dragon boat padding for chronic disease population [24,25,26,27,28,29,30,31]. Among these, six investigations focused on women with BC [26,27,28,29,30,31], and one non-RTC on survivors of different types of cancer [25]. The shared outcomes analysed within these trials included blood variables (e.g., oxidative system parameters, cytokines) [26, 29], hemodynamic and functional cardiovascular parameters (e.g., ejection fraction, echocardiographic variables, aerobic capacity) [27, 30], body composition and quality of life [25, 31]. Based on the data from two non-RCTs [26, 29], dragon boat paddling programs were associated to decreased values of reactive oxygen species and increased values for the antioxidant component of the systemic oxidative status when compared to a non-active control group sampled from the same population [26, 29]. The hemodynamic and functional cardiovascular parameters were monitored in the studies by Stefani et al. [27] and Galanti et al. [30]. In the first study, two groups (BC survivors and healthy controls) of dragon boat paddlers showed significantly improved diastolic parameters after four years of competitive activity. This was particularly evident in BC survivors (atrial peak: from 68.5 ± 15.1 cm/s to 50 ± 14.1 cm/s; ejection velocity: from 9.3 ± 2 cm/s to 11.89 ± 1.7 cm/s). In the non-RCT by Galanti et al. [30], dragon boat competitive training was found as effective as conventional exercise prescriptions on cardiac global longitudinal strain (GLS), which is a newly emerging predictor of cardiovascular outcomes. Regarding quality of life, the non-RCT by Iacorossi et al. [31] compared two groups of women with BC, one involved in a dragon boat program and one in other forms of physical exercise, showed that women who participated in dragon boat racing had more positive clinical and quality of life outcomes than did the women who did not participate in that sporting activity. Additionally, in the non-RCT by Carter et al. [25] carried out among survivors from different types of cancer, compared to walkers, dragon boat paddlers showed greater team cohesion, training adherence/attendance, and increased upper-body strength. Finally, the CT with healthy control group by Warburton et al. [24], compared the effects of a ten-week dragon boat training program on patients with cardiac and non-cardiac transplants and on a group of healthy subjects. The main finding of the study was that patients with transplants, regardless of transplant type, and sedentary control subjects experienced significant increases in aerobic fitness after 10 weeks of dragon boat training. However, the magnitude of improvement in aerobic fitness depended on the transplant type, with patients who underwent cardiac transplant experiencing greater changes in response to the training program than patients with noncardiac transplant (e.g., maximal aerobic power + 18% in cardiac transplants vs. + 8% in non-cardiac transplants). The TESTEX scores for all the studies on dragon boat padding proved “very low” (median 5/15).
Discussion
The main goal of the present scoping review was to preliminarily examine the health-related, translational potential of outdoor water sport activities on outcome measures relating to quality of life, mobility, gait and overall functioning, balance, fitness and cardiorespiratory performance, muscle strength, hematic determinations, and psychosocial functioning in people with chronic diseases. Additionally, by means of a scoping review we aimed at assessing the potential size, scope and quality of the available literature on the topic as well as identifying directions for upcoming research.
Overall, this review revealed that the majority of the relatively few studies that could be here included portray outdoor water sport activities as highly enjoyable and potentially useful to attain health benefits in populations with chronic diseases. According to these reports, positive effects seem to involve not only the functional and physiological domains, but also the social and psychological wellbeing and, consequently, the participants’ quality of life.
That being said, the body of knowledge accumulated so far on the topic is too limited in its width, reach and methodological robustness to draw substantial inference on the utility of outdoor water sports in a translational perspective. Of the initial set of potentially eligible articles (n = 84), most of them were excluded due to the absence of a comparison group and/or the absence of validated and quantitative outcome measures (n = 60 studies). Only one third of the included studies (5 out of 15) had a RCT design, which heavily limits our ability to draw causal inferences on the effectiveness of the interventions tested in the individual studies. While this weakness seems to apply to the range of water-based interventions here reviewed, this may not be the case for dragon boat training, which has been investigated more frequently (8 studies out of 15), particularly in BC survivors. In this specific population, the findings seem to match among the different investigations, generally pointing toward beneficial effect of this activity, even though also for this activity more robust research is warranted.
The potential reasons for the relatively more frequent employment of dragon boat training in a translational perspective for this chronically diseased population may relate to the specific paddling technique, which involves rhythmic and cyclic movements of the shoulder girdle and upper limbs, which have been reported to resemble a natural lymph drainage, favouring the prevention of lymphedema, and making this activity suitable to this population [31]. In conjunction with this mechanical effect, this type of group-based water sport allows several social and emotional interactions, which in turn can contribute to influence quality of life of the participants in a positive manner [32]. This is particularly relevant to women with BC, who must cope with the disease-related distress: participants can find the support they need from one another to face common challenges [32, 33].
Relatedly, a potentially relevant effect of dragon boating for, but not limited to, this population is the long-term improvements in the oxidative status, as shown by the lower reactive oxygen species that could be traced in those individuals participating in this activity [26, 29]. Some authors attributed such effect to the increased formation of superoxide dismutase and glutathione peroxidase and, overall, of antioxidant enzyme activity [34, 35]. In this line, another potentially relevant effect observed following dragon boating was that on cardiac haemodynamic function [24, 27, 30] especially if considering the key-role played by regular exercise in the attenuation of cancer treatment-related side effects as well [36]. Indeed, data from animal models showed specific cardioprotective effects of various aerobic exercise programs prior to, during and after multiple cycles of anthracycline doxorubicin treatment, thus mitigating doxorubicin-induced cardiac injuries and dysfunctions [37, 38].
When analysing the findings of the studies that focused on the effects of paddle board sports, balance and flexibility emerged as the functional variables most positively impacted [17,18,19,20]. In their study, Osti and colleagues [19] concluded that those activities challenging body balance should be considered as useful and appropriate approaches to improve postural stability in older adults. The possible mechanism by which improvements in these functions can be achieved would relate to the modulation of spinal and cortico-spinal circuitry, resulting in improved postural control, and increased strength and neuromuscular properties of the core and lower limb muscles [19]. In this line, on-water paddle board exercise may prove of utility to fragile individuals at an increased risk of falls such as neurological and rheumatological populations as well as obese/overweight people and populations diagnosed with peripheral vascular diseases. As this activity and, in general, most of the outdoor water sport interventions here reviewed were associated to higher rates of adherence than conventional trainings, administering these approaches may prove of relevance for diseased populations who, more than others, need continued participation in training programmes. The significantly higher compliance of outdoor water sports might be at least partially explained by the inherent characteristics of these unconventional forms of exercise, which combine physical activity carried out in an outdoor aquatic environment (also known as blue exercise) with the specific demands, both technical and motivational, of sports competitions. In this regard, it has been pointed out that the competitive engagement offered by these activities can provide participants burdened by living with chronic conditions with new identities as athletes [10]. Such new status along with the role of teammate represent per se strong motivations to stick to the training schedule, which in turn would allow to work on and possibly overcome physical challenges. Overall, these factors would interact and work together making outdoor water sport exercise a promising approach in the prevention of disease-related disability progress, as well as reinjury or recurrence (Table 1).
However, it should be reiterated that the findings generated by the present review cannot be generalized straightaway as the validity of the results is threatened by the number of methodological gaps and weaknesses still suffered by this literature.
Limitations
Despite a comprehensive search strategy, the findings of the present scoping review are weakened by the paucity of available data on outdoor water sports in chronic diseases, preventing data aggregation and pooling into quantitative estimates. More research consisting of adequately powered RCTs with common quantitative outcomes is needed to fill the gaps in this literature and enhance our understanding of the translational potential of outdoor water sports.
Another limitation of the review relates to the high heterogeneity of the outdoor water sports that have been here considered. Indeed, the reviewed activities differ largely from a biomechanical and metabolic point of view, and would have deserved separate analyses, which were prevented by the limited data available. Moreover, future studies will have to test the effects of outdoor water sports in specific and homogeneous populations living with chronic diseases (e.g., cancer survivors or people with chronic neurological or muscular or rheumatic conditions, etc.), which could not be accomplished by the present review.
Finally, due to the overall low studies quality and reporting (median TESTEX score 6), cautious interpretation of the studies’ findings is recommended, particularly for those studies showing a high risk of bias (TESTEX score: 5/15) [17, 20, 24,25,26,27,28,29,30,31].
Conclusions and scoping directions for future research
Based on preliminary evidence of generally low quality from small-sized, exploratory pilot studies, outdoor water sports may hold some relevance to mitigate symptoms in frail, chronically diseased populations. However, the generally positive effects of these non-conventional activities on the clinical, functional, and psychosocial domains are worthy of further scrutiny through upcoming RCTs also looking into the cost-effectiveness issue of these interventions. In the perspective of providing scoping directions and future avenues of development for this emerging research field, upcoming studies will need to consider a) increasing the number of subjects studied for each specific disease; b) sparing no efforts in the planning of more robust trials that take important methodological steps, such as randomization, allocation concealment and ‘intention-to-treat’ analysis, into proper account; c) extending the range of outdoor water sports proposed to chronically diseased populations; d) identifying further diseased population who may benefit from outdoor water sports; e) converging on a shared set of health outcomes and endpoints of treatment when assessing the acute and chronic effects as well as the potential contraindications of outdoor water sport interventions in natural environments.
The prospective accumulation of trials that look deeper into causality and dose–response of the administered interventions will likely enhance the translational usability and practical relevance of outdoor water sports.
References
Maller C, Townsend M, Pryor A, Brown P, St LL (2006) Healthy nature healthy people: ‘contact with nature’ as an upstream health promotion intervention for populations. Health Promot Int 21:45–54
Thompson Coon J, Boddy K, Stein K, Whear R, Barton J, Depledge MH (2011) Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol 45(5):1761–1772. https://doi.org/10.1021/es102947t
Eigenschenk B, Thomann A, McClure M, Davies L, Gregory M, Dettweiler U, Inglés E (2019) A systematic literature review and reflections on evidence. Int J Environ Res Public Health 16(6):937. https://doi.org/10.3390/ijerph16060937
Thompson N, Wilkie S (2021) ‘I’m just lost in the world’: the impact of blue exercise on participant well-being. Qualitative Research in Sport, Exercise and Health 13(4):624–638
Foley R, Kistemann T (2015) Blue space geographies: enabling health in place. Health Place 35:157–165. https://doi.org/10.1016/j.healthplace.2015.07.003
Britton E, Kindermann G, Domegan C, Carlin C (2020) Blue care: a systematic review of blue space interventions for health and wellbeing. Health Promot Int 35(1):50–69. https://doi.org/10.1093/heapro/day103
Gascon M, Zijlema W, Vert C, White MP, Nieuwenhuijsen MJ (2017) Outdoor blue spaces, human health and well-being: a systematic review of quantitative studies. Int J Hyg Environ Health 220(8):1207–1221. https://doi.org/10.1016/j.ijheh.2017.08.004
Grellier J, White MP, Albin M, Bell S, Elliott LR, Gascón M, Gualdi S, Mancini L, Nieuwenhuijsen MJ, Sarigiannis DA, van den Bosch M, Wolf T, Wuijts S, Fleming LE (2017) BlueHealth: a study programme protocol for mapping and quantifying the potential benefits to public health and well-being from Europe’s blue spaces. BMJ Open 7(6):e016188. https://doi.org/10.1136/bmjopen-2017-016188
Faíl LB, Marinho DA, Marques EA et al (2022) Benefits of aquatic exercise in adults with and without chronic disease-a systematic review with meta-analysis. Scand J Med Sci Sports 32(3):465–486. https://doi.org/10.1111/sms.14112
Sabiston CM, McDonough MH, Crocker PR (2007) Psychosocial experiences of breast cancer survivors involved in a dragon boat program: exploring links to positive psychological growth. J Sport Exerc Psychol 29(4):419–438. https://doi.org/10.1123/jsep.29.4.419
Mirandola D, Franchi G, Maruelli A, Vinci M, Muraca MG, Miccinesi G, Manetti M, Marini M (2020) Tailored sailing experience to reduce psychological distress and improve the quality of life of breast cancer survivors: a survey-based pilot study. Int J Environ Res Public Health 17(12):4406. https://doi.org/10.3390/ijerph17124406
Ray H, Jakubec SL (2014) Nature-based experiences and health of cancer survivors. Complement Ther Clin Pract 20(4):188–192. https://doi.org/10.1016/j.ctcp.2014.07.005
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S et al (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850
Heneghan C, Badenoch D (2002) Evidence-based medicine toolkit. BMJ Books, London
Schmidt H (2016) Chronic disease prevention and health promotion. In: Barrett H, Ortmann W, Dawson A et al (eds) Public health ethics: cases spanning the globe. Springer, Cham
Smart NA, Waldron M, Ismail H et al (2015) Validation of a new tool for the assessment of study quality and reporting in exercise training studies: TESTEX. Int J Evid Based Healthc 13:9–18
Grigorenko A, Bjerkefors A, Rosdahl H, Hultling C, Alm M, Thorstensson A (2004) Sitting balance and effects of kayak training in paraplegics. J Rehabil Med 36(3):110–116. https://doi.org/10.1080/16501970310020401
Shujaat F, Soomro N, Khan M (2014) The effectiveness of Kayaking exercises as compared to general mobility exercises in reducing axial rigidity and improve bed mobility in early to mid stage of Parkinson’s disease. Pak J Med Sci 30(5):1094–1098. https://doi.org/10.12669/pjms.305.5231
Osti FR, de Souza CR, Teixeira LA (2018) Improvement of balance stability in older individuals by on-water training. J Aging Phys Act 26(2):222–226. https://doi.org/10.1123/japa.2017-0041
Clapham ED, Lamont LS, Shim M, Lateef S, Armitano CN (2020) Effectiveness of surf therapy for children with disabilities. Disabil Health J 13(1):100828. https://doi.org/10.1016/j.dhjo.2019.100828
Pereira AI, Ferreira C, Oliveira M, Evangelista ES, Ferreira J, Roberto MS, Tereso S, Pereira AM, Neves S, Crespo C (2020) Effectiveness of a combined surf and psychological preventive intervention with children and adolescents in residential childcare: a randomized controlled trial. Revista de Psicología Clínica con Niños y Adolescentes 7(2):22–31. https://doi.org/10.21134/rpcna.2020.07.2.3
Sancassiani F, Cocco A, Cossu G, Lorrai S, Trincas G, Floris F, Mellino G, Machado S, Nardi AE, Fabrici EP, Preti A, Carta MG (2017) “VelaMente?!”—sailin in a crew to improve self-efficacy in people with psychosocial disabilities: a randomized controlled trial. Clin Pract Epidemiol Ment Health 13:200–212. https://doi.org/10.2174/1745017901713010200
Sancassiani F, Lorrai S, Cossu G, Cocco A, Trincas G, Floris F, Mellino G, Machado S, Nardi AE, Fabrici EP, Preti A, Carta MG (2017) The effects of “velamente?!” Project on social functioning of people with severe psychosocial disabilities. Clin Pract Epidemiol Ment Health 13:220–232. https://doi.org/10.2174/1745017901713010220
Warburton DE, Sheel AW, Hodges AN, Stewart IB, Yoshida EM, Levy RD, McKenzie DC (2004) Effects of upper extremity exercise training on peak aerobic and anaerobic fitness in patients after transplantation. Am J Cardiol 93(7):939–943. https://doi.org/10.1016/j.amjcard.2003.12.030
Carter CL, Onicescu G, Cartmell KB, Sterba KR, Tomsic J, Alberg AJ (2012) The comparative effectiveness of a team-based versus group-based physical activity intervention for cancer survivors. Support Care Cancer 20(8):1699–1707. https://doi.org/10.1007/s00520-011-1263-0
Tresoldi I, Foti C, Masuelli L, Frajese GV, Rossi P, Modesti A, Bei R, Giganti MG (2014) Effects of dragon boat training on cytokine production and oxidative stress in breast cancer patients: a pilot study. Open J Immunol 4:22–29
Stefani L, Galanti G, Di Tante V, Klika RJ, Maffulli N (2015) Dragon Boat training exerts a positive effect on myocardial function in breast cancer survivors. Phys Sportsmed 43(3):307–311. https://doi.org/10.1080/00913847.2015.1037711
Giganti MG, Tresoldi I, Sorge R, Melchiorri G, Triossi T, Masuelli L, Lido P, Albonici L, Foti C, Modesti A, Bei R (2016) Physical exercise modulates the level of serum MMP-2 and MMP-9 in patients with breast cancer. Oncol Lett 12(3):2119–2126. https://doi.org/10.3892/ol.2016.4887
Tomasello B, Malfa GA, Strazzanti A, Gangi S, Di Giacomo C, Basile F, Renis M (2017) Effects of physical activity on systemic oxidative/DNA status in breast cancer survivors. Oncol Lett 13(1):441–448. https://doi.org/10.3892/ol.2016.5449
Galanti G, Pedrizzetti G, Pedri S, Stefani L (2017) 2D longitudinal LV speckle tracking strain pattern in breast cancer survivors: sports activity vs exercise as prescription model. Intern Emerg Med 12(8):1149–1157. https://doi.org/10.1007/s11739-017-1741-6
Iacorossi L, Gambalunga F, Molinaro S, De Domenico R, Giannarelli D, Fabi A (2019) The effectiveness of the sport “dragon boat racing” in reducing the risk of lymphedema incidence: an observational study. Cancer Nurs 42(4):323–331
Ray HA, Verhoef MJ (2013) Dragon boat racing and health-related quality of life of breast cancer survivors: a mixed methods evaluation. BMC Complement Altern Med 13:205. https://doi.org/10.1186/1472-6882-13-205
McDonough MH, Sabiston CM, Ullrich-French S (2011) The development of social relationships, social support, and posttraumatic growth in a dragon boating team for breast cancer survivors. J Sport Exerc Psychol 33(5):627Y648
Radak Z, Chung HY, Goto S (2008) Systemic adaptation to oxidative challenge induced by regular exercise. Free Radical Biol Med 44:153–159. https://doi.org/10.1016/j.freeradbiomed.2007.01.029
Nakatani K, Komatsu M, Kato T, Yamanaka T, Takekura H, Wagatsuma A, Aoyama K, Xu B, Hirano T, Kasai H, Ando S, Takeuchi T (2005) Habitual exercise induced resistance to oxidative stress. Free Radical Res 39:905–911. https://doi.org/10.1080/10715760500183300
Cadeddu Dessalvi C, Deidda M, Noto A, Madeddu C, Cugusi L, Santoro C, López-Fernández T, Galderisi M, Mercuro G (2021) Antioxidant Approach as a Cardioprotective Strategy in Chemotherapy-Induced Cardiotoxicity. Antioxid Redox Signal 34(7):572–588. https://doi.org/10.1089/ars.2020.8055
Hayward R, Lien CY, Jensen BT, Hydock DS, Schneider CM (2012) Exercise training mitigates anthracycline-induced chronic cardiotoxicity in a juvenile rat model. Pediatr Blood Cancer 59(1):149–154
Lee Y, Kwon I, Jang Y, Cosio-Lima L, Barrington P (2020) Endurance Exercise Attenuates Doxorubicin-induced Cardiotoxicity. Med Sci Sports Exerc 52(1):25–36. https://doi.org/10.1249/MSS.0000000000002094
Acknowledgements
We are indebted to Dr. Andrea Manca, PhD, for his critical read of the manuscript.
Funding
Open access funding provided by Università degli Studi di Sassari within the CRUI-CARE Agreement. This work was supported by Bando Fondazione di Sardegna – Progetti di ricerca di base dipartimentali (FdS 2022 and 2023).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and Informed consent
For this type of study informed consent and ethical approval are not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cugusi, L., Meloni, M., Bergamin, M. et al. Health effects of outdoor water sports in chronic disease: a scoping review. Sport Sci Health 19, 1–15 (2023). https://doi.org/10.1007/s11332-022-00989-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11332-022-00989-y