Abstract
Purpose
Obstructive sleep apnea (OSA) is frequently treated with continuous positive airway pressure (CPAP) or mandibular advancement devices (MADs). For various reasons, both treatment options are often affected by low adherence. While factors associated with low CPAP adherence are described in the literature extensively, less is known about adherence to MAD therapy. This scoping review aimed to synthesize the body of literature on the factors associated with adherence to MAD treatment.
Methods
A systematic literature search was conducted using bibliographic databases PubMed, Embase.com, Web of Science, and the Cochrane Library (Wiley) to identify relevant studies that described factors associated with adherence to MAD in the treatment of OSA or snoring combined with OSA in adults.
Results
The literature search yielded a total of 694 references. Forty studies were found eligible for inclusion. The literature showed that factors with a possible negative influence on the adherence to MAD treatment are personality aspects; failing effectiveness of MAD; side effects during MAD therapy; using a thermoplastic MAD; dental treatments during MAD therapy; and a poor first experience with the MAD with inadequate guidance by professionals. Factors that may have a positive effect on MAD adherence include effectiveness of therapy, custom-made MAD, good communication skills of the practitioner, early recognition of side effects, stepwise titration of the MAD, and positive first experience with MAD.
Conclusions
The knowledge of factors associated with MAD adherence can be used to provide further insight into individual adherence to OSA treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a common condition that affects approximately 17% of women and 34% of men in the general adult population [1]. People with untreated OSA are at risk of diabetes type 2 [2], hypertension [3], and cardiovascular disease [4] and have a higher risk of traffic accidents [5]. Due to not only the high prevalence of OSA, but also personal health concerns and socioeconomic healthcare issues associated with OSA, effective treatment is essential.
The severity of OSA is determined by the apnea-hypopnea index (AHI) measured during a polysomnography (PSG). OSA severity is classified into mild (AHI ≥5 to <15), moderate (AHI ≥15 to <30), or severe (AHI ≥30) [6]. While the current standard treatment for patients with severe OSA is continuous positive airway pressure (CPAP) [7], oral appliance therapy is indicated for patients with mild to moderate OSA and for patients with severe OSA who cannot tolerate CPAP [8, 9]. Oral appliances advance the mandible and the tongue during sleep and thereby prevent obstruction of the upper airway. Such oral appliances are known as mandibular advancement devices (MADs). As neither CPAP nor MAD eliminate the underlying causes of upper airway collapsibility, lifelong treatment is necessary.
Although CPAP reduces OSA severity more than MAD therapy in patients with mild to severe OSA [10,11,12], its clinical effect is often compromised by low adherence [13, 14]. Adherence is commonly defined as behaving exactly according to rules or beliefs, which, in healthcare, usually involves conformity to treatment or medication [15, 16]. Another common related term is compliance, which is defined as obeying a particular law or rule or acting according to an agreement [15, 16]. Although the terms “compliance” and “adherence” are used synonymously, they are different in terms of the quality of healthcare, as the first term implies passively following of the instructions of the physician, while the second term implies active participation of the patient in the development of the treatment plan. The World Health Organization (WHO) prefers adherence to treatment over compliance [17]. Adherence to medical therapy is of utmost importance in the management of chronic conditions such as OSA. Studies on MAD therapy show varying results for long-term treatment adherence, which likely relate to many factors. Although numerous factors underlying poor adherence have been identified for CPAP therapy (Appendix 1) [13, 18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43], little is known about MAD adherence. Therefore, the aim of this scoping review was to assess the factors that may be associated with MAD adherence and to compare them with those related to CPAP adherence.
We hypothesized that patient-related factors associated with adherence to CPAP therapy — such as psychological status, perception of side effects, and social support [18, 33,34,35,36, 38] — also have an impact on adherence to MAD therapy. On the other hand, we also expected to find differences between adherence to both therapies regarding factors related to the device itself, such as effectivity and comfort. We expected to find that educational and behavioral interventions, as with CPAP [13, 26, 32], improve adherence to MAD.
Methods
Study design
This scoping review was conducted by the department of Orofacial Pain and Dysfunction of the Academic Centre for Dentistry Amsterdam (ACTA). The protocol was approved by the local ethics committee of ACTA (file number 2022-50457).
Search strategy
On February 21, 2023, a literature search was performed in collaboration with a medical information specialist (RdeV) based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) statement (www.prisma-statement.org). To identify all relevant publications, systematic searches were conducted in the bibliographic databases of PubMed, Embase.com, Web of Science, and the Cochrane Library (Wiley). The following terms were used as index terms or free-text words (including synonyms and closely related words): “Mandibular Advancement” and “Treatment Adherence and Compliance.”
Wherever possible, the choice has been made to use MeSH terms in order to select only those articles that focused on our research aim. Duplicate articles were excluded using Endnote X20.0.1 (Clarivate™), following the Amsterdam Efficient Deduplication (AED)-method and the Bramer-method [44, 45]. For the full search strategies for all databases, see Appendix 2.
Selection process
To establish whether the publications were relevant to our research aim, titles and abstracts were screened by a medical doctor studying for a dental Master’s degree (BR; MD, BSc) and a dental Master student (LH; BSc). The full-text articles were then checked for the eligibility criteria (see below). Differences in judgment were resolved during consensus meetings between BR, LH, and LR (DDS, PhD). To be included, a study had to describe factors that were associated with adherence to MADs in adults. Publications were excluded if they did not describe such factors and/or if the patients were under the age of 18. In addition, only articles that dealt with OSA or snoring combined with OSA were included. Further, all publication types were included, regardless of method. Only articles in English were included. The full texts of the selected articles were obtained for further review, in which positive and negative associations with adherence were examined.
Results
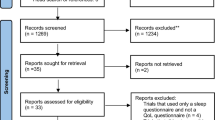
The search resulted in 1202 articles (376, PubMed; 414, Embase.com; 139, Cochrane Library; 273, Web of Science). After removal of duplicate articles and screening of titles and abstracts, 114 articles remained for full-text screening (Fig. 1). Ultimately, we identified 40 primary studies for this scoping review that addressed factors associated with MAD adherence in adults. These studies were published between 2001 and 2022. The types of factors found to be associated with MAD adherence were grouped according to the following categories: physical and psychological status of patients, effectiveness of MAD therapy, type of MAD, professional guidance during MAD treatment, side effects during MAD therapy, dental treatments during MAD therapy, previous treatments of OSA, and quantity of factors of non-adherence. Table 1 gives an overview of all the included papers and which positive and negative adherence factors they have described. The column “categories” indicates under which subheading of the “Results” section the findings from the articles are classified. In the last two columns, we described how the data was obtained (based on scientific research (fact) or by expert opinion) and how the adherence was measured (objective, subjective (self-reported), or not applicable). Side effects during MAD therapy, effectiveness of MAD therapy, and type of MAD are the most frequently described factors related to adherence in the literature (Fig. 2).
Quality assessment and reliability
This scoping review is intended to provide an overview of all existing evidence, regardless of quality. Therefore, a formal assessment of the methodological quality of the included studies was not performed [46]. Nevertheless, to give an indication of the quality of the included studies, the factors found were assessed for quality by distinguishing between scientifically researched or expert opinion. The distinction between the two categories was made by the way in which the described data was obtained and presented in the included studies. Whereas 2.5% of the factors derived from expert opinion, 77.5% of the factors were on scientific research, and the remaining 20% were based on both. Additionally, the method of measuring adherence was examined. Where possible, a distinction was made between objective or subjective (self-reported). Of the 40 articles included, seven measured adherence objectively, 25 measured it subjectively (self-reported), one article measured adherence both subjectively and objectively, and seven articles did not mention this (not applicable). Also, of all 40 included studies, seven articles are randomized controlled trials (RCT) and two articles are systematic reviews and meta-analysis [47]. The remaining articles are reviews, cohort studies, and expert opinions.
Factors associated with MAD adherence
The results are divided into several categories. For each category, the results are noted.
Physical and psychological status of patients
It is important to look at the patients’ physical characteristics before starting MAD therapy. Among OSA patients, some are arousers, i.e., patients who wake up at night, and others are desaturaters, i.e., patients who have low saturation during the night. There is a significant difference in MAD adherence between arousers (85%) and desaturaters (55%). Women were classified more as arousers than men, and patients with a higher body mass index (BMI) had more oxygen desaturations than those with a lower BMI [48]. Patients of younger age were more adherent than older-aged subjects in the treatment of mild or moderate OSA [49], and patients familiar with bruxism or smoking on a daily basis were less adherent [50].
Looking at anatomic features, Berg et al. concluded that even though tongue size of patients may predict OSA severity, no association was found between Friedman score (i.e., a score developed to describe and classify the morphology of the oropharynx with the tongue in a natural relaxed position [51]) and treatment adherence in patients with mild to moderate OSA receiving MAD treatment [52]. Although Ingman et al. found positive correlations between maxillary and mandible mesio-distal lengths and a trend toward a retrognathic maxilla position in compliant patients [53], Prescinotto et al. found no influence of anatomical features on treatment adherence [54], in contrast, Pahkala et al. found that mandibular retrusion negatively affects adherence [50]. Patients familiar with a temporomandibular dysfunction (TMD) diagnosis prior to MAD treatment and diagnosed with mild to moderate OSA adhered better to MAD therapy when they got exercise support therapy during their MAD therapy in the first 120 days of their treatment [55]. Other studies described no significant association between patient phenotype (e.g., sex, age, education, anthropometric characteristics, and economic status) and adherence rates [54, 56,57,58].
Also, certain personality traits have been linked to poor adherence. In medical psychology, personalities are often divided into 4 types of personalities, from A to D. Type D personality is defined as the simultaneous presence of both negative affectivity and social inhibition. Therefore, the letter D stands for distressed [55]. Type D personality may be related to the fact that these patients experience a higher frequency and extent of side effects, which reduces their confidence in treatment and affects MAD adherence. Research has shown that type D patients reported a significantly lower adherence to MAD treatment and exhibit a higher discontinuation rate when compared to patients without a type D personality [47, 59]. Also, a poor psychological disposition (i.e., perception of their state of health, and their mental state measured by a depression test) had an association with poor MAD adherence [60].
Effectiveness of MAD therapy
Therapy effectiveness is one of the most important reasons for adherence and continuation of therapy. In Attali et al., it was described that a ≥50% reduction in AHI and a complete symptom resolution at short-term evaluation had a positive association with adherence and is a significant predictor for long-term MAD usage [61]. Similarly, an improvement of OSA symptoms was observed with long-term MAD adherence for OSA therapy [62]. This was also described in Dieltjens et al., who found that a reduction in snoring is perceived as a therapeutic effectiveness and therefore promotes the use of the MAD, thereby improving adherence [63]. Noticing snoring and apneas by the bed partner is positively associated with adherence, so information from the bed partner about reduction in breathing cessations can support patients’ MAD adherence [64]. While treatment adherence increased in patients whose snoring and daytime OSA symptoms subjectively improved, patients tended to stop treatment when no change was noticed, either by themselves or by their partner [63, 65]. There is a significant difference in MAD adherence between arousers (85%) and desaturaters (55%) (see paragraph 3.2.1: “Physical and psychological status of patients”) [48]. Patients with mainly arousals at their PSG were more adherent at 12 months of therapy, as opposed to patients with more oxygen desaturations at their PSG. Also, a lower value of AHI and less arousals at baseline are associated with better adherence. This suggests that patients with milder OSA have better adherence to MAD treatment than those with severe OSA [54]. Furthermore, Bachour et al. described that high adherence could be due to a strict MAD indication policy, not starting MAD therapy in simple snorers or as a backup or additional therapy to CPAP [62]. The absence of OSA symptoms at the start of therapy negatively affects MAD adherence [66], while Pahkala et al. found that on baseline, the presence of a more pronounced disturbance of snoring correlates positively with objective adherence [50]. The main reason for discontinuation of the treatment was inefficacy of the treatment [47, 49, 61, 65, 67]. It is described that both a lower objective success rate (e.g., higher residual AHI with the device) and a lower subjective success rate (e.g., more residual sleepiness or relapse of symptoms, still snoring, or the partner noticed no change) are the reasons for discontinuation [47, 57, 65, 67,68,69].
Type of MAD
In general, the MADs currently on the global market can be divided into 2 categories: self-molded and custom-made. A self-molded thermoplastic MAD must usually be warmed up with hot water and then placed in the mouth so that it molds itself to the patient. In contrast, a custom-made MAD is manufactured by professionals. The existing literature shows a great preference and better adherence rates for custom-made MADs, mainly because of their better retention [58, 70,71,72,73,74,75,76,77,78]. Only Bosschieter et al. found similar adherence for both MADs [79]. In addition, custom-made MADs performed more favorable than self-molded thermoplastic MADs in AHI reduction [11, 80]. Overall disadvantages of thermoplastic designs include more side effects, difficulties in tolerating the device, and a lack of retention, resulting in poor adherence rates. However, the possibility of home-based fitting and its lower costs are advantages [80]. Another distinction can be made between mono-bloc or bi-bloc MADs. Mono-bloc MADs consist of one part, while bi-bloc MADs consist of two separate parts. While the efficacy of a mono-bloc MAD is greater because it allows no movement of the jaw, the relatively free movement of the jaw when using bi-bloc MAD may be the explanation for the better adherence of bi-bloc MAD compared to mono-bloc MAD [59, 78, 81]. Another common reason for discontinuing MAD therapy was loss or breakage of the device and possible cost of replacement [57].
Professional guidance during MAD treatment
Regular follow-up of patients by a sleep physician and a dental practitioner is required to monitor the treatment response, side effects, and adherence. In order to increase adherence, communication skills of the practitioner and early recognition and attention to symptoms of side effects are important [60, 69, 70, 82]. Attali et al. suggested that, as with other chronic diseases, early follow-up of OSA patients (e.g., repeating PSG) is very important because short-term efficacy is strongly predictive for continuation of MAD therapy [61]. Additionally, patients are more likely to be adherent to a device when they have participated in the decision-making process [83]. Kwon et al. revealed that an increase of objective adherence with MAD was seen when using feedback services by information and communication technology (ICT) [84]. A multifactorial intervention (e.g., additional information for the patient’s partner) in addition to standard MAD care improved patient adherence to treatment as well [85].
De Ruiter et al. found that stepwise titration and more protrusion of the mandible result in good adherence [86]. A possible explanation for this could be that patients are motivated to receive optimal treatment but want to experience as few side effects as possible. Patients who declined more protrusion of the mandible were less adherent to treatment. Even though there is a relationship between increased advancement of the mandible and better therapeutic efficacy, increased advancement may increase TMD risk, thereby affecting adherence negatively [47, 87].
Side effects during MAD therapy
Common side effects with MAD treatment include excessive salivation, xerostomia, occlusal problems, dental discomfort, jaw discomfort, and gingival discomfort. The occurrence of these side effects is often associated with low adherence [50, 55, 58, 59, 61, 64,65,66, 68, 69, 75, 78, 83]. Nevertheless, the side effects of MADs are usually mild by intensity and are not an obstacle to long-term regular use [84]. Also, TMD pain is a prevalent reason for low adherence [50, 56]. TMD pain could already have been present before starting the MAD therapy or have arisen in relation to the use of the MAD. Mandibular exercises were found to be effective in reducing pain and increasing MAD adherence [56]. Adherence to MAD depends, among other things, on the balance between perceptions of benefit and side effects [63, 68]. Although persistent side effects are rare [85], initial side effects may prevent early acceptance of the MAD and contribute to non-adherence [48, 57].
Positive initial experiences with MAD treatment predict increased long-term adherence [62, 82]. Sutherland et al. suggest that the first 20 days of the initial treatment period is important to perform interventions in patients with an expectation of poor treatment adherence [66]. The long-term adherence rate was high in patients who were still wearing their MAD after one month of starting their MAD therapy [62]. There could be a correlation between the initial effects of the therapy and the additional side effects. The presence of side effects such as dry mouth and discomfort were reasons for stopping treatment within 6 months. Patients who discontinued after longer use of the MAD mainly reported that it was due to occlusal changes [88]. Therefore, initial side effects could be a reason for early treatment failure, and it could prevent adherence to therapy [56].
Dental treatments during MAD therapy
Dental treatments in patients during MAD treatment was a major reason for discontinuation of MAD therapy, mainly because of an inaccurate fit of the MAD after adding supplementary occlusal units (i.e., dental implants, dental bridges) or making changes to the shape of the teeth and/or molars. In addition, patients became worried that more dental problems would arise in the future or that new dental restorations could be damaged due to the use of the MAD [67].
Previous treatments of OSA
Sometimes, patients with OSA start with another treatment modality before being referred for MAD therapy. When patients are previously treated with another treatment modality, they come from a situation of treatment failure, so Amoric et al. stated that there is a likelihood this category of patients will be more inclined to abandon this new treatment as well, because of their poor psychological acceptance ability [60]. Friedman et al. found that adherence to a custom (50.9%) or a self-molded (32.5%) MAD was poor after 6 months, but explained that this adherence rate was acceptable because all patients in this study had previously failed OSA therapy (e.g., CPAP and/or upper airway surgery) [74]. MAD-therapy as a first-line therapy was one of the predictors of long-term use of MAD [61]. In contrast to this conclusion, Vuorjoki-Ranta et al. found that many of their patients were still using their MAD after receiving CPAP therapy or surgery 5 years earlier [69].
Quantity of factors of non-adherence
Non-adherence to MAD therapy is influenced by many of the factors described above. The amount of these factors associated with non-adherence affects patient adherence. The more possible factors for non-adherence are present, the higher the likelihood of actual non-adherence [54, 57, 67].
Discussion
This scoping review aimed to identify the various factors associated with MAD adherence and compare them to the factors associated with CPAP adherence. The available literature described that several factors may have an association with adherence to MAD treatment. Factors that may have a positive impact on MAD adherence include good effectiveness of therapy, custom-made MAD, good communication skills of the practitioner, early recognition of side effects, stepwise titration of the MAD, and positive first experience with MAD. Main factors with a possible negative influence on the adherence to MAD treatment are personality aspects like a type D personality; failing effectiveness of MAD; occurrence of side effects during MAD therapy, such as patient discomfort or dental pain; usage of a thermoplastic MAD instead of a custom-made one; dental treatments during MAD therapy; and a poor first experience with the MAD with inadequate guidance by professionals. Side effects during MAD therapy, effectiveness of MAD therapy, and type of MAD are the most frequently described factors related to adherence in the literature (Fig. 2). This does not imply that these factors in fact have the greatest influence on adherence. Therefore, in this scoping review, all potential factors were examined.
A distinction can be made between MAD-specific factors and general factors of OSA therapy adherence. MAD-specific factors include occurrence of side effects during MAD therapy; the type of MAD; and dental treatments during MAD therapy. General factors include personality aspects of patients; failing effectiveness of treatment; poor experience of initial treatment with inadequate guidance by professionals; and poor experience with previous treatment modalities. The distinction between both factors is relevant for the purpose of achieving patient’s adherence.
As to enable the comparison between factors influencing adherence to MAD and to CPAP, a search was performed in PubMed with the aim to retrieve factors known to influence adherence to CPAP from systematic reviews (see Appendix 1). Patients with mild OSA are less likely to be compliant with CPAP therapy than patients with moderate to severe OSA[31]. Also, Holley et al. found that there was no significant difference in mild OSA patients between CPAP and MAD treatment in achieving their target AHI [89]. The factors listed above associated with MAD adherence in the treatment of OSA indicate that there are both similarities and differences in physical and psychological status of patients, type of device, and professional guidance during treatment between MAD and CPAP. Both treatments cause different side effects, but for each device, a high frequency or severity of side effects negatively affects adherence [18, 60]. Unlike CPAP, in the case of MAD treatment, TMD is also a reason for poor adherence [55], although a case report has described TMD-related side effects in association with CPAP as well [90]. It is noteworthy that patients with mild OSA are likely to have better adherence with MAD, and patients with severe OSA with CPAP [31, 54]. Lack of support from a partner or family, when no change is noticed by them, has a negative impact on adherence with both MAD and CPAP [18, 36]. Factors related to psychological status also affect both treatments. For example, in both CPAP and MAD treatment, type D personality and a poor perception of their general and mental state of health are of influence [38, 47, 59, 60]. However, for CPAP only, a psychological comorbidity, such as PTSD, influences adherence [33,34,35, 91, 92]. To our knowledge, however, this has not yet been researched for MAD in the current literature. When looking at device-related factors in MAD and CPAP therapy, for both treatments, the design of the device is a topic that has been extensively studied and can affect adherence. For example, for CPAP, the type of mask is of influence, while for MAD, there is a difference between custom-made or thermoplastic devices [11, 20, 21, 64, 80, 93]. For both CPAP and MAD, adherence is improved when using feedback services by ICT [21,22,23,24,25, 43, 84]. It is important to improve and enhance these technologies in the future. Also, MAD and CPAP adherence are both affected by the practitioner in terms of their communication skills or the use of behavioral interventions [13, 18, 26, 32, 60, 64, 69].
Although many interventions have been described in the literature on improving CPAP adherence, such as behavioral interventions like motivational interviewing, few interventions have been described for improving MAD adherence [18]. However, Dioguardi et al. described that patients who are included in the decision-making process of choosing a therapy have better treatment adherence [83]. Also, De Ruiter et al. described that stepwise titration of protrusion of the mandible improves MAD adherence [86].
Only 40 articles were included in this study, despite including all publication types being accepted. Therefore, our findings for this scoping review indicate a scarcity of literature specifically addressing MAD adherence in OSA therapy. Clearly, more research is needed to adequately reveal the associated factors with MAD adherence.
When looking at the type of MAD, it is noteworthy that Uniken Venema et al. described that mono-bloc appliances, compared to bi-bloc appliances, performed more favorable when examining AHI reduction. However, there were no clinically relevant differences in reduction of the Epworth Sleepiness Scale (ESS), preference, side effects, and cost-effectiveness, and in contrast to Dieltjens et al. and Lee et al., in the study by Uniken Venema et al., there were no differences between mono-bloc or bi-bloc MADs in adherence [59, 80, 81].
When comparing our scoping review to the systematic review and meta-analysis of Tallamraju et al., both studies found no significant correlation between adherence and patient or disease characteristics. Patients who did not adhere to the therapy reported experiencing more side effects and were more likely to discontinue the treatment within the first three months. Additionally, custom-made oral appliances were found to be preferred and associated with higher adherence compared to self-molded appliances. However, further research is needed to investigate the relationship between psychosocial factors and adherence to oral appliance therapy [58].
Strengths and limitations
To summarize the existing literature on factors associated with MAD adherence, 4 different databases were searched (PubMed, Embase.com, Web of Science, and the Cochrane Library) with guidance of a medical information specialist. The selection of suitable articles took place in a structured manner by two independent researchers with the help of another researcher to settle differences in judgment. This selection procedure ensures high reproducibility and thus low bias. Only articles in English were included in this scoping review leaving out 5 potentially eligible articles. As a result, additional data may have been missed. To compare the identified factors associated with MAD adherence with those associated with CPAP adherence, a limited search was performed in one database, viz., PubMed, in which only systematic reviews were included. This was done mainly because compared with MAD, there are a substantial number of studies on CPAP adherence. Although only one database was searched, it may be assumed that no important factors were missed because systematic reviews were included, in which the factors have already been mapped. Also, among the identified factors associated with MAD adherence in this scoping review, not all have been scientifically studied. Of these factors, 2.5% were derived from expert opinion, 77.5% from scientific research, and the remaining 20% from both. Thus, some of the factors are not based on scientific research which may cause a biased outcome. Considering that most studies relied on subjective adherence assessments, this scoping review observed a lack of objective measurement of adherence. Although there is a high correlation between subjective and objective data, subjectively measured adherence can cause a biased outcome because it tends to overestimate the actual MAD use [94, 95]. This suggests that more studies that objectively assess adherence are necessary.
Clinical implications
The various factors associated with professional guidance in MAD therapy emphasize the importance of regular follow-up consultations, early follow-up, including the patient in the decision-making process, and performing stepwise titration [60, 61, 69, 70, 82, 83, 86]. These results highlight the importance of integrated, interdisciplinary care between sleep physicians and dental practitioners with regular follow-up to ensure the long-term adherence to MAD treatment [96].
A clinician should develop a clear path of care for OSA patients treated with MADs. Patients should be informed at intake with a clear introduction about the MAD regarding a habituation phase and side effects in the short- and long-term of their MAD treatment. Regular appointments ensure proper monitoring of MAD treatment and for patients to report side effects or other discomforts.
MAD as a first-line treatment facilitates better long-term use [62]. Patients with previous treatment failure might be extra motivated, properly followed up, and instructed at the start of their therapy to make the new treatment a success [70]. Because patients with previous treatment failure may have poor psychological acceptability, these patients will likely stop with this new treatment as well [61, 75].
In addition, when starting MAD treatment, it is important to check the dental situation by a dental specialist, because short-term dental treatments are a common problem with the fit of the MAD [67]. In these situations, MAD therapy should be postponed until a stable and healthy dental situation is reached. Also, the patient should always bring their MAD with them to the dental practitioner. Should any adjustments be made to the dentition, the MAD may then be adjusted by the dental professional as needed.
Also, improved patient adherence was noticed with custom-made MADs compared to thermoplastic self-molded MADs; therefore, custom-made MADs are recommended [80]. Future research could be done to optimize the thermoplastic MAD design by improving retention and, consequently, realizing better therapy adherence.
Conclusion
This scoping review described several factors that may have an association with adherence to MAD therapy, such as physical and psychological status of patients, effectiveness of MAD therapy, type of MAD, side effects during MAD therapy, professional guidance during MAD treatment, dental treatments during MAD therapy, previous treatments of OSA, and quantity of factors of non-adherence. When comparing the factors associated with MAD adherence to those associated with CPAP adherence, there are both similarities and differences in the categories physical and psychological status of patients, type of device, and professional guidance during treatment. These results show that MAD adherence does not depend on the same factors as CPAP adherence, but there is some overlap.
The knowledge of the factors found in this study associated with MAD adherence can be used for further research to make recommendations to improve adherence. Ultimately, further studies would be useful to detect non-adherent patients before starting treatment and to provide proper guidance in the early stages of treatment. Matching patients to treatments in a personalized manner may contribute to the efficacy of OSA management. To facilitate clinical decision-making, more prospective randomized studies are needed.
Data availability
The authors declare that the data supporting the findings of this study are available within the article.
References
Peppard PE et al (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. https://doi.org/10.1093/aje/kws342
Seetho IW, Wilding JP (2014) Sleep-disordered breathing, type 2 diabetes and the metabolic syndrome. Chron Respir Dis 11(4):257–275. https://doi.org/10.1177/1479972314552806
Nieto FJ et al (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study Sleep Heart Health Study. Jama 283(14):1829–1836. https://doi.org/10.1001/jama.283.14.1829
Marin JM et al (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365(9464):1046–1053. https://doi.org/10.1016/s0140-6736(05)71141-7
Tregear S et al (2009) Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clin Sleep Med 5(6):573–581
Darien IL (2014) The International Classification of Sleep Disorders - Third Edition (ICSD-3). Amarican Academy of Sleep Medicine
Sullivan CE et al (1981) Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1(8225):862–865. https://doi.org/10.1016/s0140-6736(81)92140-1
Kushida CA et al (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380. https://doi.org/10.1093/sleep/29.3.375
Ramar K et al (2015) Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med 11(7):773–827. https://doi.org/10.5664/jcsm.4858
Phillips CL et al (2013) Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 187(8):879–887. https://doi.org/10.1164/rccm.201212-2223OC
Gagnadoux F et al (2009) Titrated mandibular advancement versus positive airway pressure for sleep apnoea. Eur Respir J 34(4):914–920. https://doi.org/10.1183/09031936.00148208
Engleman HM et al (2002) Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 166(6):855–859. https://doi.org/10.1164/rccm.2109023
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg 45(1):43. https://doi.org/10.1186/s40463-016-0156-0
Vanderveken OM et al (2013) Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax 68(1):91–96. https://doi.org/10.1136/thoraxjnl-2012-201900
Aronson JK (2007) Compliance, concordance, adherence. Br J Clin Pharmacol 63(4):383–384. https://doi.org/10.1111/j.1365-2125.2007.02893.x
Tilson HH (2004) Adherence or compliance? Changes in terminology. Ann Pharmacother 38(1):161–162. https://doi.org/10.1345/aph.1D207
Burkhart PV, Sabaté E (2003) Adherence to long-term therapies: evidence for action. J Nurs Scholarsh 35(3):207
Sawyer AM et al (2011) A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 15(6):343–356. https://doi.org/10.1016/j.smrv.2011.01.003
Andrade RGS et al (2018) Nasal vs oronasal CPAP for OSA treatment: a meta-analysis. Chest 153(3):665–674. https://doi.org/10.1016/j.chest.2017.10.044
Chai CL, Pathinathan A, Smith B (2006) Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev 4:Cd005308. https://doi.org/10.1002/14651858.CD005308.pub2
Patil SP et al (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med 15(2):301–334. https://doi.org/10.5664/jcsm.7638
Chen C et al (2020) Telemonitor care helps CPAP compliance in patients with obstructive sleep apnea: a systemic review and meta-analysis of randomized controlled trials. Ther Adv Chronic Dis 11:2040622320901625. https://doi.org/10.1177/2040622320901625
Murphie P et al (2019) Remote consulting with telemonitoring of continuous positive airway pressure usage data for the routine review of people with obstructive sleep apnoea hypopnoea syndrome: a systematic review. J Telemed Telecare 25(1):17–25. https://doi.org/10.1177/1357633x17735618
Aardoom JJ et al (2020) Effectiveness of ehealth interventions in improving treatment adherence for adults with obstructive sleep apnea: meta-analytic review. J Med Internet Res 22(2):e16972. https://doi.org/10.2196/16972
Hu Y et al (2021) Effects of telemedicine interventions in improving continuous positive airway pressure adherence in patients with obstructive sleep apnoea: a meta-analysis of randomised controlled trials. Sleep Breath 25(4):1761–1771. https://doi.org/10.1007/s11325-021-02292-5
Haniffa M, Lasserson TJ, Smith I (2004) Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev 4:Cd003531. https://doi.org/10.1002/14651858.CD003531.pub2
Gao W et al (2012) Is automatic CPAP titration as effective as manual CPAP titration in OSAHS patients? A meta-analysis. Sleep Breath 16(2):329–340. https://doi.org/10.1007/s11325-011-0495-z
Ayas NT et al (2004) Auto-titrating versus standard continuous positive airway pressure for the treatment of obstructive sleep apnea: results of a meta-analysis. Sleep 27(2):249–253. https://doi.org/10.1093/sleep/27.2.249
Ip S et al (2012) Auto-titrating versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: a systematic review with meta-analyses. Syst Rev 1:20. https://doi.org/10.1186/2046-4053-1-20
Zhu D et al (2018) Heated humidification did not improve compliance of positive airway pressure and subjective daytime sleepiness in obstructive sleep apnea syndrome: a meta-analysis. PLoS One 13(12):e0207994. https://doi.org/10.1371/journal.pone.0207994
Madbouly EM et al (2014) The role of severity of obstructive sleep apnea measured by apnea-hypopnea index in predicting compliance with pressure therapy, a meta-analysis. Am J Ther 21(4):260–264. https://doi.org/10.1097/MJT.0b013e318249a09d
Smith I, Nadig V, Lasserson TJ (2009) Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2:Cd007736. https://doi.org/10.1002/14651858.Cd007736
Zhang Y et al (2019) The effect of treating obstructive sleep apnea with continuous positive airway pressure on posttraumatic stress disorder: a systematic review and meta-analysis with hypothetical model. Neurosci Biobehav Rev 102:172–183. https://doi.org/10.1016/j.neubiorev.2019.03.019
Zhang Y et al (2017) Prevalence of obstructive sleep apnea in patients with posttraumatic stress disorder and its impact on adherence to continuous positive airway pressure therapy: a meta-analysis. Sleep Med 36:125–132. https://doi.org/10.1016/j.sleep.2017.04.020
Gupta MA, Simpson FC (2015) Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med 11(2):165–175. https://doi.org/10.5664/jcsm.4466
Ward K, Hoare KJ, Gott M (2014) What is known about the experiences of using CPAP for OSA from the users’ perspective? A systematic integrative literature review. Sleep Med Rev 18(4):357–366. https://doi.org/10.1016/j.smrv.2014.01.001
Ayers CM et al (2016) The effect of upper airway surgery on continuous positive airway pressure levels and adherence: a systematic review and meta-analysis. ORL J Otorhinolaryngol Relat Spec 78(3):119–125. https://doi.org/10.1159/000442023
Broström A et al (2007) Association of type D personality to perceived side effects and adherence in CPAP-treated patients with OSAS. J Sleep Res 16(4):439–447. https://doi.org/10.1111/j.1365-2869.2007.00620.x
Wang D et al (2021) The effect of non-benzodiazepine sedative hypnotics on CPAP adherence in patients with OSA: a systematic review and meta-analysis. Sleep 44(8). https://doi.org/10.1093/sleep/zsab077
Charakorn N et al (2017) The effects of topical nasal steroids on continuous positive airway pressure compliance in patients with obstructive sleep apnea: a systematic review and meta-analysis. Sleep Breath 21(1):3–8. https://doi.org/10.1007/s11325-016-1375-3
Killick R, Marshall NS (2021) The impact of device modifications and pressure delivery on adherence. Sleep Med Clin 16(1):75–84. https://doi.org/10.1016/j.jsmc.2020.10.008
Xu T et al (2012) Effect of automatic versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: an up-to-date meta-analysis. Sleep Breath 16(4):1017–1026. https://doi.org/10.1007/s11325-011-0626-6
Shaughnessy GF, Morgenthaler TI (2019) The effect of patient-facing applications on positive airway pressure therapy adherence: a systematic review. J Clin Sleep Med 15(5):769–777. https://doi.org/10.5664/jcsm.7772
Bramer WM et al (2016) De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 104(3):240–243. https://doi.org/10.3163/1536-5050.104.3.014
René Otten RDV, Schoonmade L (2019) Amsterdam efficient deduplication (AED) method. Zenodo. https://doi.org/10.5281/zenodo.4544315
Peters MD et al (2015) Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 13(3):141–146. https://doi.org/10.1097/xeb.0000000000000050
Sutherland K, Dalci O, Cistulli PA (2021) What do we know about adherence to oral appliances? Sleep Med Clin 16(1):145–154. https://doi.org/10.1016/j.jsmc.2020.10.004
Nerfeldt P, Friberg D (2016) Effectiveness of oral appliances in obstructive sleep apnea with respiratory arousals. J Clin Sleep Med 12(8):1159–1165. https://doi.org/10.5664/jcsm.6058
Saglam-Aydinatay B, Taner T (2018) Oral appliance therapy in obstructive sleep apnea: Long-term adherence and patients experiences. Med Oral Patol Oral Cir Bucal 23(1):e72–e77. https://doi.org/10.4317/medoral.22158
Pahkala R, Suominen AL (2021) Adherence to oral appliance treatment and its determinants in obstructive sleep apnoea patients. Eur J Orthod 43(4):408–414. https://doi.org/10.1093/ejo/cjaa084
Friedman M et al (1999) Clinical predictors of obstructive sleep apnea. Laryngoscope 109(12):1901–1907. https://doi.org/10.1097/00005537-199912000-00002
Berg LM et al (2020) Friedman score in relation to compliance and treatment response in nonsevere obstructive sleep apnea. Int J Otolaryngol 2020:6459276. https://doi.org/10.1155/2020/6459276
Ingman T et al (2013) Predicting compliance for mandible advancement splint therapy in 96 obstructive sleep apnea patients. Eur J Orthod 35(6):752–757. https://doi.org/10.1093/ejo/cjs092
Prescinotto R et al (2015) Impact of upper airway abnormalities on the success and adherence to mandibular advancement device treatment in patients with obstructive sleep apnea syndrome. Braz J Otorhinolaryngol 81(6):663–670. https://doi.org/10.1016/j.bjorl.2015.08.005
Cunali PA et al (2011) Mandibular exercises improve mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath 15(4):717–727. https://doi.org/10.1007/s11325-010-0428-2
Bates CJ, McDonald JP (2006) Patients’ and sleeping partners’ experience of treatment for sleep-related breathing disorders with a mandibular repositioning splint. Br Dent J 200(2):95–101; discussion 92. https://doi.org/10.1038/sj.bdj.4813149
Brette C et al (2012) A mandibular advancement device for the treatment of obstructive sleep apnea: long-term use and tolerance. Int Orthod 10(4):363–376. https://doi.org/10.1016/j.ortho.2012.09.001
Tallamraju H et al (2021) Factors influencing adherence to oral appliance therapy in adults with obstructive sleep apnea: a systematic review and meta-analysis. J Clin Sleep Med 17(7):1485–1498. https://doi.org/10.5664/jcsm.9184
Dieltjens M et al (2013) Impact of type D personality on adherence to oral appliance therapy for sleep-disordered breathing. Sleep Breath 17(3):985–991. https://doi.org/10.1007/s11325-012-0788-x
Amoric M (2013) Efficacy and compliance in treatment of sleep apnea with Herbst mandibular advancement splints (OHA version). Int Orthod 11(2):193–209. https://doi.org/10.1016/j.ortho.2013.02.008
Attali V et al (2016) Predictors of long-term effectiveness to mandibular repositioning device treatment in obstructive sleep apnea patients after 1000 days. Sleep Med 27-28:107–114. https://doi.org/10.1016/j.sleep.2016.10.004
Bachour P et al (2016) Oral appliance in sleep apnea treatment: respiratory and clinical effects and long-term adherence. Sleep Breath 20(2):805–812. https://doi.org/10.1007/s11325-015-1301-0
Dieltjens M et al (2015) Determinants of objective compliance during oral appliance therapy in patients with sleep-disordered breathing: a prospective clinical trial. JAMA Otolaryngol Head Neck Surg 141(10):894–900. https://doi.org/10.1001/jamaoto.2015.1756
Gjerde K et al (2022) Partner perceptions are associated with objective sensor-measured adherence to oral appliance therapy in obstructive sleep apnea. J Sleep Res 31(2):e13462. https://doi.org/10.1111/jsr.13462
McGown AD et al (2001) Long-term use of mandibular advancement splints for snoring and obstructive sleep apnoea: a questionnaire survey. Eur Respir J 17(3):462–466. https://doi.org/10.1183/09031936.01.17304620
Sutherland K et al (2021) Treatment usage patterns of oral appliances for obstructive sleep apnea over the first 60 days: a cluster analysis. J Clin Sleep Med 17(9):1785–1792. https://doi.org/10.5664/jcsm.9288
Haviv Y et al (2017) Assessment of interfering factors in non-adherence to oral appliance therapy in severe sleep apnea. Oral Dis 23(5):629–635. https://doi.org/10.1111/odi.12633
Hoffstein V (2007) Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath 11(1):1–22. https://doi.org/10.1007/s11325-006-0084-8
Vuorjoki-Ranta TR et al (2020) Mandibular advancement device therapy for obstructive sleep apnea: a longitudinal study among patients treated in community dental care in Finland - Potential for the precision medicine approach. Cranio:1–6. https://doi.org/10.1080/08869634.2020.1752431
Chan AS, Cistulli PA (2009) Oral appliance treatment of obstructive sleep apnea: an update. Curr Opin Pulm Med 15(6):591–596. https://doi.org/10.1097/MCP.0b013e3283319b12
Vanderveken OM et al (2008) Comparison of a custom-made and a thermoplastic oral appliance for the treatment of mild sleep apnea. Am J Respir Crit Care Med 178(2):197–202. https://doi.org/10.1164/rccm.200701-114OC
Quinnell TG et al (2014) A crossover randomised controlled trial of oral mandibular advancement devices for obstructive sleep apnoea-hypopnoea (TOMADO). Thorax 69(10):938–945. https://doi.org/10.1136/thoraxjnl-2014-205464
Pépin JL et al (2019) Heat-moulded versus custom-made mandibular advancement devices for obstructive sleep apnoea: a randomised non-inferiority trial. Thorax 74(7):667–674. https://doi.org/10.1136/thoraxjnl-2018-212726
Friedman M et al (2012) Compliance and efficacy of titratable thermoplastic versus custom mandibular advancement devices. Otolaryngol Head Neck Surg 147(2):379–386. https://doi.org/10.1177/0194599812439683
Johal A, Agha B (2018) Ready-made versus custom-made mandibular advancement appliances in obstructive sleep apnea: a systematic review and meta-analysis. J Sleep Res 27(6):e12660. https://doi.org/10.1111/jsr.12660
Johal A et al (2017) Ready-made versus custom-made mandibular repositioning devices in sleep apnea: a randomized clinical trial. J Clin Sleep Med 13(2):175–182. https://doi.org/10.5664/jcsm.6440
Gagnadoux F et al (2017) Comparison of titrable thermoplastic versus custom-made mandibular advancement device for the treatment of obstructive sleep apnoea. Respir Med 131:35–42. https://doi.org/10.1016/j.rmed.2017.08.004
Bortolotti F et al (2022) Dropout and adherence of obstructive sleep apnoea patients to mandibular advancement device therapy: a systematic review of randomised controlled trials with meta-analysis and meta-regression. J Oral Rehabil 49(5):553–572. https://doi.org/10.1111/joor.13290
Bosschieter PFN et al (2022) Equal effect of a noncustom vs a custom mandibular advancement device in treatment of obstructive sleep apnea. J Clin Sleep Med 18(9):2155–2165. https://doi.org/10.5664/jcsm.10058
Venema J et al (2021) Mandibular advancement device design: a systematic review on outcomes in obstructive sleep apnea treatment. Sleep Med Rev 60:101557. https://doi.org/10.1016/j.smrv.2021.101557
Lee WH et al (2013) Comparison between mono-bloc and bi-bloc mandibular advancement devices for obstructive sleep apnea. Eur Arch Otorhinolaryngol 270(11):2909–2913. https://doi.org/10.1007/s00405-013-2417-0
Deacon NL et al (2016) Treatment of obstructive sleep apnea. prospects for personalized combined modality therapy. Ann Am Thorac Soc 13(1):101–108. https://doi.org/10.1513/AnnalsATS.201508-537FR
Dioguardi A, Al-Halawani M (2016) Oral appliances in obstructive sleep apnea. Otolaryngol Clin North Am 49(6):1343–1357. https://doi.org/10.1016/j.otc.2016.07.005
Kwon JS et al (2022) Effectiveness of remote monitoring and feedback on objective compliance with a mandibular advancement device for treatment of obstructive sleep apnea. J Sleep Res 31(3):e13508. https://doi.org/10.1111/jsr.13508
Liu J et al (2022) A multifactorial intervention to increase adherence to oral appliance therapy with a titratable mandibular advancement device for obstructive sleep apnea: a randomized controlled trial. Sleep Breath 26(4):1739–1745. https://doi.org/10.1007/s11325-021-02548-0
de Ruiter MHT et al (2020) A stepwise titration protocol for oral appliance therapy in positional obstructive sleep apnea patients: proof of concept. Sleep Breath 24(3):1229–1236. https://doi.org/10.1007/s11325-020-02045-w
Bamagoos AA et al (2019) Dose-dependent effects of mandibular advancement on upper airway collapsibility and muscle function in obstructive sleep apnea. Sleep 42(6). https://doi.org/10.1093/sleep/zsz049
de Almeida FR et al (2005) Long-term compliance and side effects of oral appliances used for the treatment of snoring and obstructive sleep apnea syndrome. J Clin Sleep Med 1(2):143–152
Holley AB, Lettieri CJ, Shah AA (2011) Efficacy of an adjustable oral appliance and comparison with continuous positive airway pressure for the treatment of obstructive sleep apnea syndrome. Chest 140(6):1511–1516. https://doi.org/10.1378/chest.10-2851
Lobbezoo F et al (2020) Nasal CPAP therapy associated with masticatory muscle myalgia. J Clin Sleep Med 16(3):455–457. https://doi.org/10.5664/jcsm.8230
López-López L et al (2020) Nursing interventions improve continuous positive airway pressure adherence in obstructive sleep apnea with excessive daytime sleepiness: a systematic review. Rehabil Nurs 45(3):140–146. https://doi.org/10.1097/rnj.0000000000000190
Richter K et al (2020) Sleep disorders in migrants and refugees: a systematic review with implications for personalized medical approach. Epma J 11(2):251–260. https://doi.org/10.1007/s13167-020-00205-2
Hensley M, Ray C (2009) Sleep apnoea. BMJ Clin Evid 2009
Dieltjens M et al (2013) Objectively measured vs self-reported compliance during oral appliance therapy for sleep-disordered breathing. Chest 144(5):1495–1502. https://doi.org/10.1378/chest.13-0613
Smith YK, Verrett RG (2014) Evaluation of a novel device for measuring patient compliance with oral appliances in the treatment of obstructive sleep apnea. J Prosthodont 23(1):31–38. https://doi.org/10.1111/jopr.12076
Cistulli PA et al (2004) Treatment of snoring and obstructive sleep apnea with mandibular repositioning appliances. Sleep Med Rev 8(6):443–457. https://doi.org/10.1016/j.smrv.2004.04.002
Smith I, Lasserson TJ (2009) Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 4:Cd003531. https://doi.org/10.1002/14651858.CD003531.pub3
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Data collection and analysis were performed by L.H. van der Hoek and B.R.A.M. Rosenmöller. The first draft of the manuscript was written by L.H. van der Hoek and B.R.A.M. Rosenmöller, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This manuscript does not contain clinical studies or patient data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Literature review
To ultimately compare the factors associated with MAD adherence with those associated with CPAP adherence, it was first necessary to identify them. To that end, a literature search on systematic reviews on factors associated with CPAP adherence was conducted in the bibliographic database of PubMed on May 9, 2021.
Search strategy
To identify all relevant publications, the following MeSH terms were used: “Treatment Adherence and Compliance,” “Continuous Positive Airway Pressure,” and “Systematic Review.” Systematic reviews that described factors related to CPAP adherence in the treatment of OSA in adult patients were included. The search resulted in 118 articles. After screening for title and abstract, 24 articles remained. Several factors related to CPAP adherence emerged after reading the full text articles.
Selection process
To determine if the publications were relevant to our research aim, titles and abstracts were screened by a medical doctor studying for a dental master’s degree (BR; MD, BSc) and a dental master’s student (LH; BSc). The full-text articles were then checked for eligibility criteria, and differences in assessment were resolved during consensus meetings between BR and LH. To be included, a systematic review had to describe factors associated with adherence to CPAP in adult OSA patients. Publications that did not describe such factors and in which the patients were younger than 18 years were excluded. Only systematic reviews were included.
Results
The search resulted in 118 articles. After screening of the titles and abstracts, 24 articles remained for full-text screening (Fig. 3). All factors associated with CPAP adherence were noted. The types of factors found to be associated with CPAP adherence were grouped according to the following categories: physical and psychological status of patients, type of CPAP, professional guidance during CPAP treatment, and medication use during CPAP treatment.
Physical and psychological status of patients
Patient-related factors that influence adherence to CPAP include disease and patient characteristics, psychological factors, and social factors [18]. Patients with mild OSA are less likely to be compliant with CPAP therapy than patients with moderate to severe OSA [31]. Patients who had upper airway surgery showed improved CPAP adherence [37], and nasal anatomy may be of influence on CPAP adherence [18]. When looking at psychological factors, it was found that patients with post-traumatic stress disorder (PTSD) showed low adherence to CPAP and that improvements in PTSD symptoms were associated with better CPAP adherence [33,34,35]. Adults with type D personality (i.e., negative affectivity and social inhibition) perceived more side effects and showed lower CPAP adherence than patients without type D personality [38]. Proper family and social support are an important factor in experiencing CPAP treatment; this requires further study to determine the impact it has on CPAP adherence [36].
Type of CPAP
It was notable that many factors associated with CPAP adherence are device related. For example, CPAP adherence is influenced by the type of mask, being higher with nasal masks than with oronasal masks [19,20,21]. Looking at pressure delivery, some studies reported no significant difference between auto-CPAP and conventional CPAP in adherence [27, 28, 41], while others showed better results for auto-CPAP [26, 29, 42, 97]. Although no significant difference in adherence is observed when the humidification of the device is adjusted, heated humidification reduces some CPAP-related side effects more than no humidification [30].
Professional guidance during CPAP treatment
Improvement of CPAP adherence is shown with educational and behavioral interventions [13, 26, 32] as well as with telemonitor interventions [21,22,23, 25]. Also, the use of patient-facing applications (i.e., web-based applications that interact directly with the patient) improved adherence [43], and eHealth interventions increase adherence during the initial phase of treatment [24].
Medication use during CPAP treatment
When examining CPAP adherence and the use of non-benzodiazepine sedative hypnotics, it shows that such hypnotics may improve CPAP adherence [39]. The same observation applies to the use of nasal steroids [40].
Appendix 2
PubMed session results (21 Feb 2023)
Search | Query | Items found |
#3 | #1 AND #2 | 376 |
#2 | “Treatment Adherence and Compliance”[Mesh] OR complian*[tiab] OR adheren*[tiab] OR noncomplian*[tiab] OR nonadheren*[tiab] OR dropout*[tiab] OR “drop-out*”[tiab] | 575,979 |
#1 | “Mandibular Advancement”[Mesh] OR ((“mandibular advancement”[tiab] OR “maxillomandibular advancement”[tiab] OR “mandibular reposition”[tiab]) AND (device*[tiab] OR appliance*[tiab])) OR “protrusive device*”[tiab] OR “protrusion device*”[tiab] OR “protrusive appliance*”[tiab] OR “protrusion appliance*”[tiab] | 2,561 |
Embase.comsession results (21 Feb 2023)
Search | Query | Items found |
#4 | #3 NOT (‘conference abstract’/it OR ‘conference review’/it) | 414 |
#3 | #1 AND #2 | 542 |
#2 | ‘patient attitude’/exp OR complian*:ab,ti,kw OR adheren*:ab,ti,kw OR noncomplian*:ab,ti,kw OR nonadheren*:ab,ti,kw OR dropout*:ab,ti,kw OR ‘drop-out*’:ab,ti,kw | 914,644 |
#1 | ‘mandibular advancement’/exp OR ‘maxillomandibular advancement’/exp OR ‘sleep apnea device’/exp OR ((‘mandibular advancement’:ab,ti,kw OR ‘maxillomandibular advancement’:ab,ti,kw OR ‘mandibular reposition’:ab,ti,kw) AND (device*:ab,ti,kw OR appliance*:ab,ti,kw)) OR ‘protrusive device*’:ab,ti,kw OR 'protrusion device*':ab,ti,kw OR ‘protrusive appliance*’:ab,ti,kw OR ‘protrusion appliance*’:ab,ti,kw | 2579 |
Wiley/Cochrane Library session results (21 Feb 2023)
Search | Query | Items found |
#3 | #1 AND #2 | 139 |
#2 | (complian* OR adheren* OR noncomplian* OR nonadheren* OR dropout* OR (drop NEXT out*)):ab,ti,kw | 99,299 |
#1 | ((((mandibular NEXT advancement) OR (maxillomandibular NEXT advancement) OR (mandibular NEXT reposition)) AND (device* OR appliance*)) OR (protrusive NEXT device*) OR (protrusion NEXT device*) OR (protrusive NEXT appliance*) OR (protrusion NEXT appliance*)):ab,ti,kw | 392 |
Web of Science (core collection) session results (21 Feb 2023)
Search | Query | Items found |
#3 | #1 AND #2 | 273 |
#2 | TS=(“complian*” OR “adheren*” OR “noncomplian*” OR “nonadheren*” OR “dropout*” OR “drop-out*”) | 509,091 |
#1 | TS=(((“mandibular advancement” OR “maxillomandibular advancement” OR “mandibular reposition”) AND (“device*” OR “appliance*”)) OR “protrusive device*” OR “protrusion device*” OR “protrusive appliance*” OR “protrusion appliance*”) | 1476 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Hoek, L.H., Rosenmöller, B.R., van de Rijt, L.J. et al. Factors associated with treatment adherence to mandibular advancement devices: a scoping review. Sleep Breath 27, 2527–2544 (2023). https://doi.org/10.1007/s11325-023-02862-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02862-9