Abstract
Purpose
The relationships between sleep quality and sleep hygiene awareness in the Chinese population were unclear. We aimed to investigate the associations and related factors between sleep quality and sleep hygiene awareness in adults and to identify the most central domain for sleep quality using network analysis.
Methods
A cross-sectional survey was conducted from April 22 to May 5, 2020. Adults (18 years old or above) who had access to smartphones were invited to participate in this survey. The Pittsburg Sleep Quality Index (PSQI) and the Sleep Hygiene Awareness and Practice Scale (SHAPS) were used to evaluate the sleep quality and sleep hygiene awareness of the participants. Propensity score matching (PSM) was used as sensitivity analysis to reduce the confounding effects. Multiple logistic regression was performed to evaluate the associations. The R packages “bootnet” and “qgraph” were used to estimate the connection and calculate the network centrality indices between good and poor sleepers.
Results
In total, 939 respondents were included in the analysis. Of them, 48.8% (95% CI: 45.6–52.0%) were identified as poor sleepers. Participants with nervous system diseases, psychiatric diseases, and psychological problems were more likely to have poor sleep quality. The notion that using sleep medication regularly was beneficial to sleep was associated with poor sleep quality. Similarly, the notion that waking up at the same time each day disrupted sleep was also associated with poor sleep quality. The findings were consistent before and after PSM. Subjective sleep quality was the most central domain for sleep quality in good and poor sleepers.
Conclusion
Poor sleep quality was positively associated with certain sleep hygiene notions in Chinese adults. Effective measures such as self-relief, sleep hygiene education, and cognitive behavioral treatment may have been needed to improve sleep quality, especially during the COVID-19 outbreak.
Similar content being viewed by others
Introduction
Sleep disorder has been ranked as the second most common mental health problem worldwide. In China, the prevalence of insomnia is estimated at 38.9% [1], higher than the 27.3% in the USA [2]. Difficulties with sleep initiation and maintenance as well as early awakening may lead to deficits in daytime function and well-being, increasing the risks of diabetes [3], hypertension [4], and mental health problems [5].
The concept of sleep quality is complex and controversial. Nelson et al. performed a systematic review on the evolution of the concepts and defined sleep quality as an individual’s self-satisfaction with all aspects of the sleep experience, including both subjective and objective aspects [6]. In a social-ecological model, three levels of factors played roles in sleep, namely the individual level, social level, and societal level [7]. Health status, beliefs, behaviors, attitudes, choices, and psychological factors are individual-level factors that could be modified by improving the attitudes and behaviors toward sleep. Behavioral and environmental recommendations to promote sleep, also known as sleep hygiene, are widely used in public sleep education and non-clinical treatments of insomnia [8]. Sleep hygiene awareness is the knowledge or awareness of sleep hygiene people acquire, such as reducing caffeine intake, taking regular exercise, not sleeping too late, and getting up at the same time each day [9]. People with good sleep hygiene awareness are more likely to seek assistance from professionals and manage their sleep problems positively. A few studies were conducted to explore the associations between sleep hygiene and sleep quality; however, the results have been inconsistent. Some studies reported that good sleep hygiene awareness was associated with regular sleep habits, higher sleep quality, and higher sleep sufficiency [10, 11]. On the contrary, other studies found no significant associations between sleep quality and sleep hygiene awareness [12, 13]. This discrepancy may be attributed to the heterogeneity of participants, study design, and assessment instruments. Most current studies were conducted on university students, and the associations were still unclear for the Chinese general population. Additionally, with the effects of COVID-19, sleep quality and sleep hygiene awareness probably changed due to the direct effects of viral infection, social isolation, or other factors [14]. Therefore, the primary aim of this study was to investigate the associations between sleep quality and sleep hygiene awareness among Chinese adults during the COVID-19 pandemic. We hypothesized that sleep quality and sleep hygiene awareness were positively associated after accounting for covariates.
The seven components of sleep quality in the Pittsburgh Sleep Quality Index (PSQI) instrument are subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, the use of sleep medication, and daytime dysfunction [15]. Previous studies analyzed the components of sleep quality with a latent disease model, which assumes that the symptoms were independent of each other [16]. However, these domains were intercorrelated, leading to a difficulty in interpreting the correlations among them. Network analysis is an approach to describe the interactions among symptoms through the modeling of dynamic systems and is able to identify the central symptoms visually [17]. It has been widely used in psychological area to elucidate the complex connections among symptoms [18, 19] and has showed good reliability [20]. Using the network analysis may provide us the opportunity to understand the interactions among the domains of sleep quality.
In summary, this study aimed to (1) investigate the association between sleep disorder and sleep hygiene awareness in Chinese adults and (2) interpret the interactions among sleep quality domains in good and poor sleepers using the network analysis.
Participants and methods
Study design and participants
This cross-sectional study was conducted from April 22 to May 5, 2020. Adults (18 years old or above) who had access to smartphones were invited to participate in this survey. Participants were recruited with the “snowball” sampling method. Considering the prevention and control policy of COVID-19, the investigation was performed through “Wenjuanxing” (Changsha Ranxing Science and Technology, Shanghai, China), an online platform widely used in cross-sectional studies during the pandemic [21, 22]. All participants provided informed consent before participating in the study. Ethics approval was obtained from the Institutional Review Board of Beijing Anding Hospital.
Data collection
The questionnaire comprised the following three parts: (1) demographic data including age, gender, nationality, place of residence, education, occupation, marital status, and the history of chronic diseases; (2) sleep quality assessment; (3) sleep hygiene awareness assessment. It took 5–10 min to complete the questionnaire. Chronic diseases such as nervous system diseases (cerebrovascular disease, myotonic dystrophy, etc.), digestive system diseases (peptic ulcer, gastritis, gallstones, cholecystitis, etc.), and psychiatric diseases (major depressive disorder, generalized anxiety disorder, schizophrenia, etc.) and psychological problems were identified by self-report of participants.
Measurements
In this study, the Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality during the past month. This self-administered questionnaire contains 17 items belonging to seven domains and yields a total score ranging from 0 to 21 [15]. The cutoff for “poor sleepers” was a total score of more than 5 [23]. The Chinese version of PSQI showed good reliability and validity in both subjects with primary insomnia and control subjects (Cronbach’s α coefficient of 0.82–0.83) [23] and has been widely used in epidemiology studies [24,25,26]. The Cronbach α coefficient was 0.766 in this study.
Additionally, the sleep hygiene awareness of the participants was assessed using the Sleep Hygiene Awareness and Practice Scale (SHAPS) [27]. SHAPS consisted of two subsections: awareness and practice. The Chinese version of SHAPS showed acceptable test–retest reliability (Cronbach’s α coefficient of 0.71) [28]. In this study, the awareness subsection including 13 items was used to measure the participants’ attitudes toward specific activities about sleep, such as daytime napping, consumption of caffeine, smoking, drinking, or strenuous exercise. The answers scored on a 7-point Likert scale, ranging from “behavior is very beneficial to sleep (1)” to “behavior is very disruptive to sleep (7).” Higher scores represented poorer sleep hygiene awareness [13]. Meanwhile, we categorized the answers reflecting sleep hygiene awareness into three categories when comparing the sleep hygiene awareness of good and poor sleepers: category one was “beneficial to sleep,” category two was “no effects on sleep,” and category three was “disruptive to sleep.” The Cronbach α coefficient was 0.709 in this study.
Data analyses
Association analyses
IBM SPSS statistics version 21.0 (IBM Corp, Armonk, NY, USA) was used for association analyses. Due to the non-normal distribution of the data, the Mann–Whitney U test was used for the comparisons of continuous variables. Chi-square tests were performed to compare the characteristics and sleep hygiene awareness of good sleepers and poor sleepers. Moreover, propensity score matching (PSM) in a 1:1 ratio with calipers of 0.01 was performed to reduce the imbalance of participants in age, gender, education, marital status, nervous system diseases, digestive system diseases, psychiatric diseases, and psychological problems. Multiple logistic regressions were conducted to analyze the associations between sleep hygiene awareness and sleep quality in the full analysis set and post-matching subset. The odds ratio (OR) and 95% confidence intervals (CIs) were calculated after adjusting for covariables. A P value of < 0.05 (two-tailed) was considered statistically significant.
Network analyses
Network analysis was performed to estimate the connection between sleep quality and sleep hygiene awareness. Spearman correlations and Gaussian Markov random field estimation graphical LASSO (EBICglasso) were used to estimate the structure of the network with the R package “bootnet” [20]. The visualization of the network was completed using the R package “qgraph” [29]. In the network, the scores of seven domains of sleep quality were considered as nodes, and the correlations among the nodes were considered as edges [17]. The color and thickness of the edges indicated the directions and strengths of the associations. The network was constructed automatically, and the nodes with stronger connections were placed more centrally in the network. The Network Comparison Test (NCT) was applied to compare the networks of good and poor sleepers.
Then, the network centrality indices, including strength, closeness, and betweenness, were calculated (Z-score) to characterize the importance of the items [30]. Nodes with higher centrality were more central and important in the network. Strength reflects the importance of a node by summing the weights of edges. Betweenness indicates the indirect connections between the nodes in the network by summing the number of times a node is on the shortest path between any two nodes. Closeness is the average length of the inverse shortest path between any nodes in the network.
The stability of the network was evaluated with the correlation stability coefficient (CS-Cs) and a node-dropping sub-setting bootstrap method for the centrality indices of the network. Generally, a CS-C higher than 0.5 indicates a stable network [20]. Meanwhile, the non-parametric bootstrap of resampling by repeating 1000 times was applied to estimate the accuracy of edges (α = 0.05).
Results
Sample characteristics
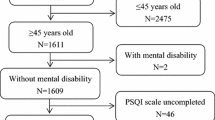
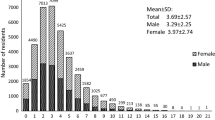
In total, 942 respondents completed the online survey. Subjects who finished the survey in less than 120s were removed and 939 subjects were included in the final analysis. The demographic characteristics of the participants and the comparison between good and poor sleep quality are summarized in Table 1. Most participants were women (67.8%), living in the urban area of Beijing (47.4%), having a bachelor’s degree or above (93.4%), and married (72.2%). The mean age of the participants was 38.7 ± 10.5 years old with a range from 18 to 84. Of them, 458 (48.8%, 95% CI: 45.6–52.0%) had a total PSQI score of more than 5 and were thus categorized as poor sleepers. The mean score of PSQI was 6.2 ± 3.9. The result of the chi-square test showed that compared with the good sleepers, a significantly higher proportion of poor sleepers had nervous system diseases, digestive system diseases, psychiatric diseases, and mood problems (P < 0.05). The power analysis showed a satisfied power of more than 0.9 with a sample size of 939, alpha of 0.05, a null proportion of 0.35 [31], and an alternative proportion of 0.49 in this study.
Associations between sleep quality and sleep hygiene awareness
Table 2 showed the differences between the sleep hygiene awareness of the participants with good or poor sleep quality. The poor sleepers believed that daytime napping, using sleep medication, sleeping for about the same length of time each night, and drinking 3 oz of alcohol in the evening were more beneficial to sleep (P < 0.05). Also, they believed that exercising in the afternoon or early evening and waking up at the same time each day were disruptive to sleep (P < 0.05).
Using multiple logistic regression, we could know that participants with nervous system diseases (OR = 6.41, 95% CI: 3.19–12.90), psychiatric diseases (OR = 5.44, 95% CI: 2.76–10.72), and psychological problems (OR = 3.63, 95% CI: 1.49–8.83) were more likely to have poor sleep quality. Moreover, participants who held the notion that using sleep medication regularly was beneficial to sleep and waking up at the same time each day was disruptive to sleep were positively associated with poor sleep quality (OR = 1.99, 95% CI: 1.36–2.90; OR = 2.39, 95% CI: 1.45–3.92) after adjusting for confounders (Table 3).
The propensity score matching yielded 696 matched participants, with 348 in each sleeper (good or poor) group. The binary logistic regression showed that the notions about using sleep medication regularly and waking up at the same time were still positively associated with poor sleep quality after adjusting for the propensity score in the post-matching subset. Moreover, participants who believed that exercising in the afternoon or early evening was disruptive to sleep were more likely to have poor sleep quality after adjusting for the propensity score in the post-matching subset (OR = 1.82, 95% CI: 1.01–3.25) (Supplementary Table 1).
Sleep quality network estimation, centrality stability tests, and strength comparison
The estimated network of seven sleep quality domains of good sleepers and poor sleepers using the “EBICglasso” model and Spearman correlations is shown in Fig. 1. The results revealed that “use of sleep medication” had no edge with other nodes of good sleepers. Sleep disturbance and daytime dysfunction showed strong negative correlations with subjective sleep quality in good sleepers, while habitual sleep efficiency was positively associated with subjective sleep quality, daytime dysfunction, and sleep disturbance. For poor sleepers, except for habitual sleep efficiency, all other five domains showed negative associations with subjective sleep quality. According to the centrality indices including strength, betweenness, and closeness, subjective sleep quality was the most central domain in both good- and poor-sleep-quality networks (Fig. 2).
The estimated network of poor sleepers showed good stability as the CS-Cs were 0.52, 0.52, and 0.44 for “strength,” “betweenness,” and “closeness,” respectively. However, the stability of the network of good sleepers was relatively low due to the low CS-Cs for “betweenness” and “closeness” (Supplementary Fig. 1). The NCT indicated that the global strength was significantly higher in poor sleepers (NCT sum = 1.67) than in good sleepers (NCT sum = 0.50, test statistic S = 1.17, P < 0.001), which means that the poor-sleeper network was more densely connected.
Discussion
This is the first study to explore the associations between sleep quality and sleep hygiene awareness in Chinese adults. In this study, we found that almost half of the participants (48.8%, 95% CI: 45.6–52.0%) exhibited poor sleep quality (defined as a PSQI score of more than 5). Multivariate logistic regression analysis revealed that having nervous system diseases, psychiatric diseases, and mental health problems were positively associated with poor sleep quality. Also, the notions that using sleep medication regularly was beneficial to sleep and waking up at the same time each day was disruptive to sleep were significantly associated with poor sleep quality. Subjective sleep quality was the most important domain among the seven domains of sleep quality in networks of good sleepers and poor sleepers.
The prevalence of sleep disorders in our study was much higher than the pooled prevalence of sleep disturbances in a meta-analysis for older Chinese (35.9%, 95% CI: 30.6–41.2%) [31], the crude (21.6%) and age-standardized (15.8%) prevalence of poor sleep quality in Henan Province rural adults [32], the prevalence (21.0%, 95% CI: 19.7–22.2%) in older adults in Hebei Province [33], and the prevalence (32.0%) in Chinese governmental employees [34]. The prevalence was similar to the finding of an epidemiology survey conducted in Beijing (52.1%) [35]. The high prevalence could be attributed to the impacts of the COVID-19 pandemic [36], different cutoff values of PSQI, and different population characteristics. In this study, 8.1% of the participants were diagnosed with mental disorders, and mental disorders showed strong associations with sleep alterations in our results and other studies [37]. Additionally, because most participants (70.9%) lived in Beijing, the high societal pressures and economic burdens could also result in insufficient sleep duration and sleep disorders [38]. Considering that this survey was conducted during the COVID-19 pandemic, the social isolation, irregular schedule, and lack of physical exercise may have disturbed the sleep circles and increased the prevalence of insomnia [39].
The associations between sleep hygiene awareness and sleep quality in the general population were barely investigated before. Chung et al. used PSQI and SHAPS to examine the relationships between sleep hygiene practices and sleep quality in nurses, and found that sleep hygiene practices and mood states mediated the effects of morningness-eveningness and menstrual distress on sleep quality [28]. On the contrary, Mazza et al. evaluated the associations between psychometric measures and napping habitude in patients with insomnia, and no significant correlations were found between nap parameters and psychometric results [40]. Our results revealed that poor sleepers held the notions that using sleep medication regularly was beneficial to sleep and waking up at the same time each day was disruptive to sleep. Clinically, sleep medication (also called sedative-hypnotics) such as benzodiazepines and non-benzodiazepines are widely prescribed by clinicians to deal with insomnia. However, adverse effects include tolerance and dependence may lead to overdose or even abuse of sedative-hypnotics, which may be life-threatening [41,42,43]. A survey showed that 53.6% of elderly outpatients had knowledge of the safe use of sedative-hypnotics. But of them, only 24.8% knew that not all sedative-hypnotics would have a better sedative or sleep-inducing effect with increased dosage [44]. Insufficient knowledge of the correct use of sedative-hypnotics indicates that the government and physicians should pay more attention to sleep hygiene education [45]. Additionally, experts recommended taking a multifaceted and personalized approach to balance the efficacy and adverse effects of sedative-hypnotics [46].
The network analysis showed that subjective sleep quality was the most central domain in both good and poor sleepers. Subjective sleep quality had one of the highest component-total correlation coefficients among the seven domains in PSQI [15]. Compared with objective sleep quality, subjective sleep quality is mainly a self-perception. It concerns how one feels at the moment of waking and throughout the day and one’s subjective estimation of sleep parameters such as depths of sleep or awakenings in the night [47]. To some extent, compared with objective sleep parameters like the total sleeping time, sleep efficiency, and times of awakening, subjective sleep quality may better reflect a patient’s perception of his or her sleep condition which is worth more attention in clinical practice [48]. Some studies found discrepancies between self-reported sleep quality and the results of polysomnography and actigraphy measurements in adolescents, patients with insomnia, or patients with psychiatric disorders [49,50,51]. The differences between subjective perception and objective sleep parameters could even result in paradoxical insomnia, which is manifested as a subjective report of insomnia despite normal results of objective measures of sleep [52, 53]. Although the sleep patterns of patients with paradoxical insomnia would be nearly normal, the distress and anxiety induced by the perceived poor sleep quality may also have a negative impact on mental health [54]. Therefore, timely and effective interventions such as cognitive behavioral treatment (CBT) or appropriate medication are needed to address sleep misperception and improve subjective sleep quality.
Our study had the strength of exploring the association between sleep quality and sleep hygiene awareness in adults and investigating the most central domain in the PSQI. However, there were limitations that deserve attention. First, considering the policies for the control of the COVID-19 pandemic, the participants were recruited with a web-based “snowball” sampling method instead of random sampling, so the results may be influenced by selection bias and need to be interpreted with caution. Second, the cross-sectional design limited the exploration of causal relationships among sleep quality, sleep hygiene awareness, and chronic diseases. Longitudinal study design and causal inference methods could be used to further elucidate the risk factors for sleep disorders. Third, the self-report assessment of sleep quality may produce results inconsistent with the objective measurement. Additionally, objective sleep quality was not measured for some logistic reasons. Furthermore, most participants lived in Beijing, which limited the generalizability of the results to the entire country.
Conclusion
The results showed that poor sleep quality was common in Chinese adults. Sleep quality was positively associated with sleep hygiene awareness about sleep medication usage, waking up at the same time each day, and exercising in the afternoon or early evening. Furthermore, subjective sleep quality was the most central domain of sleep quality for good and poor sleepers, which suggested that sleep hygiene education and CBT were quite important for improving sleep quality in adults, especially during the COVID-19 pandemic.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P (2020) Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 88:901–907. https://doi.org/10.1016/j.bbi.2020.05.026
Olfson M, Wall M, Liu SM, Morin CM, Blanco C (2018) Insomnia and impaired quality of life in the United States. J Clin Psychiatry. 79(5). https://doi.org/10.4088/JCP.17m12020
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W et al (2015) Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care 38(3):529–537. https://doi.org/10.2337/dc14-2073
Meng L, Zheng Y, Hui R (2013) The relationship of sleep duration and insomnia to risk of hypertension incidence: a meta-analysis of prospective cohort studies. Hypertens Res 36(11):985–995. https://doi.org/10.1038/hr.2013.70
Biddle DJ, Hermens DF, Lallukka T, Aji M, Glozier N (2019) Insomnia symptoms and short sleep duration predict trajectory of mental health symptoms. Sleep Med 54:53–61. https://doi.org/10.1016/j.sleep.2018.10.008
Nelson KL, Davis JE, Corbett CF (2022) Sleep quality: an evolutionary concept analysis. Nurs Forum 57(1):144–151. https://doi.org/10.1111/nuf.12659
Grandner MA (2020) Sleep, health, and society. Sleep Med Clin 15(2):319–340. https://doi.org/10.1016/j.jsmc.2020.02.017
Stepanski EJ, Wyatt JK (2003) Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev 7(3):215–225. https://doi.org/10.1053/smrv.2001.0246
Zhu Y, Huang J, Yang M (2022) Association between chronotype and sleep quality among Chinese college students: the role of bedtime procrastination and sleep hygiene awareness. Int J Environ Res Public Health. 20(1). https://doi.org/10.3390/ijerph20010197
Brown FC, Buboltz WC Jr, Soper B (2002) Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behav Med 28(1):33–38. https://doi.org/10.1080/08964280209596396
Suen LK, Tam WW, Hon KL (2010) Association of sleep hygiene-related factors and sleep quality among university students in Hong Kong. Hong Kong Med J 16(3):180–185
Alshahrani M, Al Turki Y (2019) Sleep hygiene awareness: its relation to sleep quality among medical students in King Saud University, Riyadh, Saudi Arabia. J Family Med Prim Care 8(8):2628–2632. https://doi.org/10.4103/jfmpc.jfmpc_359_19
Al-Kandari S, Alsalem A, Al-Mutairi S, Al-Lumai D, Dawoud A, Moussa M (2017) Association between sleep hygiene awareness and practice with sleep quality among Kuwait University students. Sleep Health 3(5):342–347. https://doi.org/10.1016/j.sleh.2017.06.004
Huang C, Huang L, Wang Y, Li X, Ren L, Gu X et al (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 397(10270):220–232. https://doi.org/10.1016/S0140-6736(20)32656-8
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28(2):193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Khosravi A, Emamian MH, Hashemi H, Fotouhi A (2021) Components of Pittsburgh Sleep Quality Index in Iranian adult population: an item response theory model. Sleep Med X 3:100038. https://doi.org/10.1016/j.sleepx.2021.100038
Borsboom D, Cramer AO (2013) Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 9:91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
Barthel AL, Pinaire MA, Curtiss JE, Baker AW, Brown ML, Hoeppner SS et al (2020) Anhedonia is central for the association between quality of life, metacognition, sleep, and affective symptoms in generalized anxiety disorder: a complex network analysis. J Affect Disord 277:1013–1021. https://doi.org/10.1016/j.jad.2020.08.077
Cai H, Zhao YJ, Xing X, Tian T, Qian W, Liang S et al (2022) Network analysis of comorbid anxiety and insomnia among clinicians with depressive symptoms during the late stage of the COVID-19 pandemic: a cross-sectional study. Nat Sci Sleep 14:1351–1362. https://doi.org/10.2147/NSS.S367974
Epskamp S, Borsboom D, Fried EI (2018) Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods 50(1):195–212. https://doi.org/10.3758/s13428-017-0862-1
Li M, Liu L, Yang Y, Wang Y, Yang X, Wu H (2020) Psychological impact of health risk communication and social media on college students during the COVID-19 pandemic: cross-sectional study. J Med Internet Res 22(11):e20656. https://doi.org/10.2196/20656
Chen X, Qi H, Liu R, Feng Y, Li W, Xiang M et al (2021) Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: a comparison of two cross-sectional studies. Transl Psychiatry 11(1):148. https://doi.org/10.1038/s41398-021-01271-4
Tsai PS, Wang SY, Wang MY, Su CT, Yang TT, Huang CJ et al (2005) Psychometric evaluation of the Chinese version of the Pittsburgh Sleep Quality Index (CPSQI) in primary insomnia and control subjects. Qual Life Res 14(8):1943–1952. https://doi.org/10.1007/s11136-005-4346-x
Luo J, Zhu G, Zhao Q, Guo Q, Meng H, Hong Z et al (2013) Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: results from the Shanghai aging study. PLoS One 8(11):e81261. https://doi.org/10.1371/journal.pone.0081261
Sun W, Yu Y, Yuan J, Li C, Liu T, Lin D et al (2015) Sleep duration and quality among different occupations–China national study. PLoS One 10(3):e0117700. https://doi.org/10.1371/journal.pone.0117700
Zhou SJ, Wang LL, Yang R, Yang XJ, Zhang LG, Guo ZC et al (2020) Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med 74:39–47. https://doi.org/10.1016/j.sleep.2020.06.001
Lacks P, Rotert M (1986) Knowledge and practice of sleep hygiene techniques in insomniacs and good sleepers. Behav Res Ther 24(3):365–368. https://doi.org/10.1016/0005-7967(86)90197-x
Chung MH, Liu WI, Lee HL, Hsu N (2013) Selected neurophysiological, psychological, and behavioral influences on subjective sleep quality in nurses: a structure equation model. PLoS One 8(11):e79529. https://doi.org/10.1371/journal.pone.0079529
Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D (2012) qgraph: network visualizations of relationships in psychometric data. J Stat Softw 48(4):367–371
Opsahl T, Agneessens F, Skvoretz J (2010) Node centrality in weighted networks: generalizing degree and shortest paths. Soc Networks 32(3):245–251. https://doi.org/10.1016/j.socnet.2010.03.006
Lu L, Wang SB, Rao W, Zhang Q, Ungvari GS, Ng CH et al (2019) The prevalence of sleep disturbances and sleep quality in older Chinese adults: a comprehensive meta-analysis. Behav Sleep Med 17(6):683–697. https://doi.org/10.1080/15402002.2018.1469492
Wang Y, Li Y, Liu X, Liu R, Mao Z, Tu R et al (2019) Gender-specific prevalence of poor sleep quality and related factors in a Chinese rural population: the Henan Rural Cohort Study. Sleep Med 54:134–141. https://doi.org/10.1016/j.sleep.2018.10.031
Zhang YS, Jin Y, Rao WW, Jiang YY, Cui LJ, Li JF et al (2020) Prevalence and socio-demographic correlates of poor sleep quality among older adults in Hebei province. China Sci Rep 10(1):12266. https://doi.org/10.1038/s41598-020-68997-x
Li YL, Qiu D, Hu C, Ouyang FY, He J, Zang DF et al (2021) Stressful life events and poor sleep quality: a cross-sectional survey in the Chinese governmental employees. Sleep Med 85:123–130. https://doi.org/10.1016/j.sleep.2021.06.030
Ma AJ, Fang K, Wei YQ, Jiang B, Dong J, Xie C et al (2020) Study on the relationship between sleep-related problems and dyslipidemia among adults in Beijing (in Chinese). Chin J Epidemiol 41(08):1250–1255
Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z et al (2020) Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry 11:306. https://doi.org/10.3389/fpsyt.2020.00306
Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C et al (2016) Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull 142(9):969–990. https://doi.org/10.1037/bul0000053
Grandner MA (2017) Sleep, health, and society. Sleep Med Clin 12(1):1–22. https://doi.org/10.1016/j.jsmc.2016.10.012
Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV (2021) Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med 17(2):299–313. https://doi.org/10.5664/jcsm.8930
Mazza M, Lapenta L, Losurdo A, Marano G, Testani E, Janiri L et al (2020) Polysomnographic and psychometric correlates of napping in primary insomnia patients. Nord J Psychiatry 74(4):244–250. https://doi.org/10.1080/08039488.2019.1695285
Lou BX, Oks M (2021) Insomnia: pharmacologic treatment. Clin Geriatr Med 37(3):401–415. https://doi.org/10.1016/j.cger.2021.04.003
Bateson AN (2002) Basic pharmacologic mechanisms involved in benzodiazepine tolerance and withdrawal. Curr Pharm Des 8(1):5–21. https://doi.org/10.2174/1381612023396681
Azevedo K, Johnson M, Wassermann M, Evans-Wall J (2021) Drugs of abuse-opioids, sedatives, hypnotics. Crit Care Clin 37(3):501–516. https://doi.org/10.1016/j.ccc.2021.03.003
Liu J, Feng RJ, Cui XY, Li H, Liu Y, Chen P (2016) Investigation on knowledge and behavior related to safe use of sedative-hypnotic drugs in outpatient elderly patients (in Chinese). J Nursing (China) 23(18):56–8. https://doi.org/10.16460/j.issn1008-9969.2016.18.056
Chung KF, Lee CT, Yeung WF, Chan MS, Chung EW, Lin WL (2018) Sleep hygiene education as a treatment of insomnia: a systematic review and meta-analysis. Fam Pract 35(4):365–375. https://doi.org/10.1093/fampra/cmx122
Jiang HF, Zhao M, Liu TQ, Hao W (2021) Expert opinion on rational use of sedative and hypnotics (in Chinese). Chin J Drug Abuse Prev Treat 27(02):103–6. https://doi.org/10.15900/j.cnki.zylf1995.2021.02.034
Harvey AG, Stinson K, Whitaker KL, Moskovitz D, Virk H (2008) The subjective meaning of sleep quality: a comparison of individuals with and without insomnia. Sleep 31(3):383–393. https://doi.org/10.1093/sleep/31.3.383
Sella E, Borella E (2021) Strategies for controlling sleep-related intrusive thoughts, and subjective and objective sleep quality: how self-reported poor and good sleepers differ. Aging Ment Health 25(10):1959–1966. https://doi.org/10.1080/13607863.2020.1783513
Ma Y, Goldstein MR, Davis RB, Yeh GY (2021) Profile of subjective-objective sleep discrepancy in patients with insomnia and sleep apnea. J Clin Sleep Med 17(11):2155–2163. https://doi.org/10.5664/jcsm.9348
Klumpp H, Roberts J, Kapella MC, Kennedy AE, Kumar A, Phan KL (2017) Subjective and objective sleep quality modulate emotion regulatory brain function in anxiety and depression. Depress Anxiety 34(7):651–660. https://doi.org/10.1002/da.22622
Carter JR, Gervais BM, Adomeit JL, Greenlund IM (2020) Subjective and objective sleep differ in male and female collegiate athletes. Sleep Health 6(5):623–628. https://doi.org/10.1016/j.sleh.2020.01.016
Manconi M, Ferri R, Sagrada C, Punjabi NM, Tettamanzi E, Zucconi M et al (2010) Measuring the error in sleep estimation in normal subjects and in patients with insomnia. J Sleep Res 19(3):478–486. https://doi.org/10.1111/j.1365-2869.2009.00801.x
Rezaie L, Fobian AD, McCall WV, Khazaie H (2018) Paradoxical insomnia and subjective-objective sleep discrepancy: a review. Sleep Med Rev 40:196–202. https://doi.org/10.1016/j.smrv.2018.01.002
Fernandez-Mendoza J, Vgontzas AN (2013) Insomnia and its impact on physical and mental health. Curr Psychiatry Rep 15(12):418. https://doi.org/10.1007/s11920-013-0418-8
Funding
This work was supported by the Beijing Health Technologies Promotion Program (grant number BHTPP202016) and the Beijing High level Public Health Technical Talents Training Plan (grant number xuekedaitouren-01–30).
Author information
Authors and Affiliations
Contributions
Study design: Fang Yan, Han Qi
Data collection, analysis, and interpretation: Han Qi, Rui Liu, Jia Zhou, Yuan Feng, Lei Feng, Zizhao Feng
Drafting of the manuscript: Han Qi
Critical revision of the manuscript: Zizhao Feng, Fang Yan
Approval of the final version for publication: all co-authors
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution (Beijing Anding Hospital) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qi, H., Liu, R., Zhou, J. et al. Investigating sleep quality and sleep hygiene awareness among Chinese adults: an association and network analysis study. Sleep Breath 27, 2049–2058 (2023). https://doi.org/10.1007/s11325-023-02798-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02798-0