Abstract
Purpose
The present study validated a software-based electrocardiogram (ECG) analysis tool for detection of atrial fibrillation (AF) and risk for AF using polysomnography (PSG)-derived ECG recordings.
Methods
The Stroke Risk Analysis® (SRA®) software was applied to 3-channel ECG tracings from diagnostic PSG performed in enrolled subjects including a subgroup of subjects with previously documented AF. No subjects used positive airway pressure therapy. All ECG recordings were visually analyzed by a blinded cardiologist.
Results
Of subjects enrolled in the study, 93 had previously documented AF and 178 of 186 had an ECG that could be analyzed by either method. In subjects with known history of AF, automated analysis using SRA® classified 47 out of 87 ECG as either manifest AF or showing increased risk for paroxysmal AF (PAF) by SRA® (sensitivity 0.54, specificity 0.86). On visual analysis, 36/87 ECG showed manifest AF and 51/87 showed sinus rhythm. Among the latter subgroup, an increased risk for PAF was ascribed by SRA® in 11 cases (sensitivity 0.22, specificity 0.78) and by expert visual analysis in 5 cases (sensitivity 0.1, specificity 0.90). Among 36/178 ECG with manifest AF on visual analysis, 33 were correctly identified by the SRA® software (sensitivity and specificity 0.92).
Conclusion
Sleep studies provide a valuable source of ECG recordings that can be easily subjected to software-based analysis in order to identify manifest AF and automatically assess the risk of PAF. For optimal evaluability of data, multiple channel ECG tracings are desirable. For assessment of PAF risk, the SRA® analysis probably excels visual analysis, but sensitivity of both methods is low, reflecting that repeated ECG recording remains essential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
About 20% of ischemic strokes are caused by heart disease and atrial fibrillation (AF), in particular [1]. The prevalence of AF has been reported to be 0.51% worldwide and 1–4% in industrialized countries [2, 3]. Stroke etiology cannot be unambigously identified in more than 30% of cases (“cryptogenic stroke”) [4], likely including subjects with paroxysmal AF (PAF) that may often go undetected [5,6,7]. Cardio-embolic stroke is frequently severe due to occlusion of large cerebral vessels [8]. As ischemic stroke due to AF can be effectively prevented by oral anticoagulation, reliable detection of AF is essential for identifying subjects at risk. However, detection of PAF is known to be delayed in many cases [9], and detection rates strongly depend on the applied type of cardiac monitoring. Frequently, PAF is missed by standard 12-channel electrocardiography (ECG) and 24-h Holter ECG recordings. Repeated or extended 24-h Holter ECG recording substantially enhances PAF detection rate [10,11,12]. Insertable or implantable cardiac monitors have been shown to identify even more subjects with PAF [13]. Lastly, several methods for automated ECG analysis have been developed [14,15,16]. Among these, the Stroke Risk Analysis (SRA®) software utilizes a computational algorithm identifying either manifest AF or yielding a graded score that classifies the risk of AF [17].
Among many other conditions, sleep-disordered breathing (SDB) has been identified as an independent risk factor for AF [18, 19]. For diagnostic purposes, cardiorespiratory polygraphy and polysomnography (PSG) are widely used if SDB is suspected, both including ECG recordings. Routine sleep studies are usually conducted over a 6–8-h period, providing an ECG recording of the same duration that can potentially be used for automated ECG analysis and individual risk assessment. However, the SRA® technology has not yet been applied to ECG recordings derived from overnight sleep studies. Therefore, this study investigated whether the SRA® software correctly identifies subjects with manifest AF and accurately classifies subjects with previously documented PAF as being at risk based on a 3-lead polysomnographic ECG.
Methods
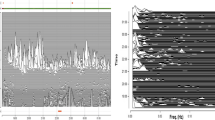
This retrospective study was approved by the local ethics authority (Ethikkommission der Ärztekammer Westfalen-Lippe und der Medizinischen Fakultät der WWU Münster, Az. 2019–238-f-S). PSG recordings were extracted from the sleep laboratory database at Münster University Hospital (10/2009–02/2019). Inclusion criteria comprised age > 18 years, diagnostic PSG (i.e., no use of positive airway pressure therapy) and total sleep time > 6 h. Subjects wearing a cardiac pacemaker were excluded. Patients with known chronic AF or PAF at the time of diagnostic sleep studies were identified based on pre-existing information derived from hospital records (ICD-10 codes I48.0, I48.1, and I48.2). Subjects in whom manifest AF had been identified on visual evaluation of the PSG-derived ECG were also included in this subgroup. Medical records and PSG data of control subjects were extracted from the same clinical database. Control subjects had no known AF, did not use positive airway pressure therapy, and were matched for age (± 3 years) and gender. Diagnostic PSGs were performed for evaluation of sleep-related breathing, insomnia, parasomnia, or hypersomnolence. Cardiorespiratory PSG (Nihon Kohden, Rosbach, Germany) was conducted and validated following standard recommendations. ECG recordings comprised three leads and were extracted from the PSG record in European Data Format (EDF) for SRA® analysis. SRA® technology uses non-linear and linear computational algorithms to evaluate the dynamics of R-R interval variations. Increased or irregular R-R intervals are known to occur more frequently in subjects with PAF even in periods with sinus rhythm. SRA® technology classifies QRS complexes as either normal or ventricular based on morphological features. For further mathematical analysis, an algorithm is applied that was trained in a neural network setup for which a large number of ECG datasets from subjects with and without PAF were used [15]. Finally, the risk for AF is classified according to four categories: 0, no increased risk for paroxysmal AF (normal); 1, increased risk for PAF; 2, manifest AF; x, not evaluable. The results are displayed using a Lorenz plot that depicts successive R-R intervals in an alternating manner on the x-axis and y-axis of a Cartesian coordinate system (Fig. 1). Finally, all ECG recordings were visually and independently analyzed by an expert cardiologist (G. F.) who was blinded for both group affiliation of ECG recordings and results of SRA® analysis. Visually analyzed ECG recordings were also grouped according to the above four categories (i.e., normal, increased risk of AF, manifest AF, not evaluable). Increased risk of AF was thought to be reflected by occurrence of premature supraventricular beats and short atrial runs that have been shown to predict future AF (or PAF, respectively) in patients with cryptogenic stroke [20].
Results
In total, PSG recordings from 186 individuals (56 women, mean age 65, standard deviation 12) were used for data analysis. The patient cohort comprised 93 subjects with documented AF and 93 controls. All ECG tracings could successfully be extracted for both software-based and independent visual analysis. Among the entire cohort, the number of recordings that were considered technically unevaluable by either SRA® or visual analysis was 4 (2.1%) and 7 (3.7%), respectively. Finally, 178 ECG tracings were analyzable by both methods.
SRA® analysis
By SRA® analysis, 35/178 (19.7%) ECGs were classified as manifest AF, 25/178 (14.0%) as “increased risk of AF,” and 118/178 (66.3%) as unremarkable. Among 89 evaluable ECG tracings from patients with documented AF, classification was as follows: 33 manifest AF, 14 increased risk, and 42 no increased risk of AF. Regarding the status “previously documented AF,” sensitivity and specificity of SRA® analysis were 0.54 and 0.86, respectively. Among controls (i.e., without previously documented AF), 11/93 patients were categorized as showing increased risk for PAF, and in 2/93 subjects, manifest AF was detected.
Expert visual analysis
In 179 evaluable ECGs, visual analysis revealed manifest AF in 36 recordings which were all derived from patients with previously documented AF. Supraventricular extrasystoles (SVES), potentially indicating increased risk of AF [20], were observed in 5/88 patients with documented AF, and in 9/91 control subjects. In patients with previously documented AF (n = 88), sensitivity and specificity of visual ECG analysis for detection of either AF or an increased risk was 0.48 and 0.90 respectively.
Matching of SRA® and visual analysis
From 178 ECG recordings, 163 tracings were classified by the cardiologist and SRA® in consensus. In fifteen cases, ECG interpretation was discordant, including 3 ECG that were categorized as “increased risk of AF” by SRA® but were classified as manifest AF by visual analysis. In two cases, classification was manifest AF by SRA® but sinus rhythm with SVES by visual analysis. In ten ECG showing sinus rhythm, SRA® and visual analysis did not agree on risk assessment. On visual analysis, 36/87 ECG showed manifest AF and 51/87 showed sinus rhythm (Fig. 2). Among the latter subgroup, an increased risk for paroxysmal AF was ascribed by SRA® in 11 cases (sensitivity 0.22, specificity 0.78). The SRA® software correctly identified 33/36 ECGs that were classified as manifest AF by visual evaluation and categorized all remaining three recordings as “increased risk of AF.” Thus, none of these ECG traces were falsely classified as normal by automated analysis. With regard to the cardiologist’s interpretation, sensitivity and specificity of the SRA® analysis were both 0.92.
Intercorrelation of AF and obstructive sleep apnea
Among 186 patients, 82 (44.1%) showed obstructive sleep apnea (OSA) on diagnostic PSG. Prevalence of OSA was 58.1% in patients with and 30.1% in subjects without previously documented AF (p < 0.001). Based on visual ECG classification, OSA was present in 32.0% of patients with sinus rhythm, 57.1% of those with increased risk of AF, and 81.1% of subjects with manifest AF (p < 0.001). Vice versa, manifest AF was present in 30/82 (36.5%) patients with newly diagnosed OSA compared to only 7/102 (6.7%) individuals without sleep-disordered breathing (p < 0.001).
Discussion
The present study is the first to test both suitability and validity of the SRA® analysis software for automated evaluation of ECG recordings derived from overnight sleep studies. While it does not follow a prospective approach (e.g., by focusing on the prediction of future AF), the present work merely investigates whether the SRA® software is applicable to 3-channel PSG-derived ECG recordings. The study rationale is based on the assumption that sleep laboratory ECG data might be a valuable source for cardiovascular risk assessment in patients undergoing sleep studies. Sleep-disordered breathing (SDB) is highly prevalent in the aging population [21] and the most frequent cause for sleep laboratory evaluations. At the same time, it is a known risk factor for AF [18], rendering it reasonable to combine sleep studies with ECG analysis that is focused on either manifest AF or, using and automated approach, predictors of PAF risk. Many patients with SDB undergo repetitive evaluation of sleep once mask-based therapy has been established, increasing the number and cumulative duration of ECG recordings. As many PSG systems include more than one ECG channel, reliable tracings are available that can be used for automated ECG analysis.
This study confirms a substantial overlap (or coincidence) between OSA and AF. Prevalence of OSA was highest in patients with previously documented AF and with manifest AF, in particular. Based on expert visual analysis, OSA prevalence was intermediate in subjects showing sinus rhythm but ECG abnormalities that suggest an increased risk for PAF, indicating that the association between OSA and AF reflects a disease continuum. These findings are not pivotal for the present validation study but support previous work suggesting that SDB promotes AF risk and triggers episodes of manifest AF [22, 23].
The main result of this study is that SRA® analysis can technically be applied to ECG recordings that derive from overnight PSG. The proportion of tracings that cannot be automatically analysed is acceptably small, and with regard to detection of manifest AF, automated ECG analysis is not inferior to visual validation. Regarding prediction of PAF or PAF risk in patients with previously documented AF, test accuracy of the SRA® software is similar to visual ECG analysis. However, sensitivity of both methods is obviously limited and might be considered insufficient. This finding can be ascribed to several reasons. Firstly, duration of PSG-derived ECG recordings is still limited which likely causes a decrease in sensitivity as compared to multiple-day inpatient monitoring, repeated Holter ECG recordings, or long-term ECG tracing by means of implantable devices. Secondly, stratification of patients as “having documented AF” is possibly based on unreliable information that is derived from written medical records only that often cannot be verified. Thirdly, sensitivity of both automated and visual ECG analysis for detection of AF risk has also been shown to be limited in patients with cryptogenic stroke [20], indicating that a subset of patients with PAF cannot be identified by either method. As PSG-derived ECG recordings are technically suitable for automated analysis, longitudinal studies are desirable to investigate whether routine application of this method may help to prospectively identify patients at risk for PAF.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lin H-J, Wolf PA, Benjamin EJ, Belanger AJ, D’Agostino RB (1995) Newly diagnosed atrial fibrillation and acute stroke: the Framingham study. Stroke 26:1527–1530. https://doi.org/10.1161/01.STR.26.9.1527
Lippi G, Sanchis-Gomar F, Cervellin G (2021) Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. Int J Stroke 16:217–221. https://doi.org/10.1177/1747493019897870
Zulkifly H, Lip GYH, Lane DA (2018) Epidemiology of atrial fibrillation. Int J Clin Pract 72:e13070. https://doi.org/10.1111/ijcp.13070
Hu H, Zhang X, Zhao J, Li Y, Zhao Y (2019) Transient ischemic attack and carotid web. Am J Neuroradiol 40:313–318. https://doi.org/10.3174/ajnr.A5946
Humphries KH, Kerr CR, Connolly SJ, Klein G, Boone JA, Green M, Sheldon R, Talajic M, Dorian P, Newman D (2001) New-onset atrial fibrillation: sex differences in presentation, treatment, and outcome. Circulation 103:2365–2370. https://doi.org/10.1161/01.CIR.103.19.2365
Hylek EM, Henault LE (2003) Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med 349(11):1019–26. https://doi.org/10.1056/NEJMoa022913
Roche F, Gaspoz J-M, Da Costa A, Isaaz K, Duverney D, Pichot V, Costes F, Lacour J-R, Barthelemy J-C (2002) Frequent and prolonged asymptomatic episodes of paroxysmal atrial fibrillation revealed by automatic long-term event recorders in patients with a negative 24-hour Holter. Pacing Clin Electrophysiol 25:1587–1593. https://doi.org/10.1046/j.1460-9592.2002.01587.x
Kimura K, Minematsu K, Yamaguchi T, Japan Multicenter Stroke Investigators’ Collaboration (J-MUSIC) (2005) Atrial fibrillation as a predictive factor for severe stroke and early death in 15,831 patients with acute ischaemic stroke. J Neurol Neurosurg Psychiatry 76:679–683. https://doi.org/10.1136/jnnp.2004.048827
Kamel H, Lees KR, Lyden PD, Teal PA, Shuaib A, Ali M, Johnston SC, Virtual International Stroke Trials Archive Investigators (2009) Delayed detection of atrial fibrillation after ischemic stroke. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 18:453–457. https://doi.org/10.1016/j.jstrokecerebrovasdis.2009.01.012
Douen AG, Pageau N, Medic S (2008) Serial electrocardiographic assessments significantly improve detection of atrial fibrillation 2.6-fold in patients with acute stroke. Stroke 39:480–482. https://doi.org/10.1161/STROKEAHA.107.492595
Jabaudon D, Sztajzel J, Sievert K, Landis T, Sztajzel R (2004) Usefulness of ambulatory 7-day ECG monitoring for the detection of atrial fibrillation and flutter after acute stroke and transient ischemic attack. Stroke 35:1647–1651. https://doi.org/10.1161/01.STR.0000131269.69502.d9
Haeusler KG, Kirchhof P, Kunze C, Tütüncü S, Fiessler C, Malsch C, Olma MC, Jawad-Ul-Qamar M, Krämer M, Wachter R, Michalski D, Kraft A, Rizos T, Gröschel K, Thomalla G, Nabavi DG, Röther J, Laufs U, Veltkamp R, Heuschmann PU, Endres M, Investigators MonDAFIS (2021) Systematic monitoring for detection of atrial fibrillation in patients with acute ischaemic stroke (MonDAFIS): a randomised, open-label, multicentre study. Lancet Neurol 20:426–436. https://doi.org/10.1016/S1474-4422(21)00067-3
Bernstein RA, Kamel H, Granger CB, Piccini JP, Sethi PP, Katz JM, Vives CA, Ziegler PD, Franco NC, Schwamm LH, Investigators STROKE-AF (2021) Effect of long-term continuous cardiac monitoring vs usual care on detection of atrial fibrillation in patients with stroke attributed to large- or small-vessel disease: the STROKE-AF randomized clinical trial. JAMA 325:2169–2177. https://doi.org/10.1001/jama.2021.6470
Hoshino T, Nagao T, Shiga T, Maruyama K, Toi S, Mizuno S, Ishizuka K, Shimizu S, Uchiyama S, Kitagawa K (2015) Prolonged QTc interval predicts poststroke paroxysmal atrial fibrillation. Stroke 46:71–76. https://doi.org/10.1161/STROKEAHA.114.006612
Schaefer JR, Leussler D, Rosin L, Pittrow D, Hepp T (2014) Improved detection of paroxysmal atrial fibrillation utilizing a software-assisted electrocardiogram approach. PloS One 9:e89328. https://doi.org/10.1371/journal.pone.0089328
Rizos T, Güntner J, Jenetzky E, Marquardt L, Reichardt C, Becker R, Reinhardt R, Hepp T, Kirchhof P, Aleynichenko E, Ringleb P, Hacke W, Veltkamp R (2012) Continuous stroke unit electrocardiographic monitoring versus 24-hour Holter electrocardiography for detection of paroxysmal atrial fibrillation after stroke. Stroke 43:2689–2694. https://doi.org/10.1161/STROKEAHA.112.654954
Reinke F, Bettin M, Ross LS, Kochhäuser S, Kleffner I, Ritter M, Minnerup J, Dechering D, Eckardt L, Dittrich R (2018) Refinement of detecting atrial fibrillation in stroke patients: results from the TRACK-AF study. Eur J Neurol 25(4):631–636. https://doi.org/10.1111/ene.13538
Hendrikx T, Sundqvist M, Sandström H, Sahlin C, Rohani M, Al-Khalili F, Hörnsten R, Blomberg A, Wester P, Rosenqvist M, Franklin KA (2017) Atrial fibrillation among patients under investigation for suspected obstructive sleep apnea. PLOS ONE 12:e0171575. https://doi.org/10.1371/journal.pone.0171575
Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE, Somers VK, on behalf of the American Heart Association Council on Clinical Cardiology; Council on Peripheral Vascular Disease; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Stroke Council; and Council on Cardiovascular Surgery and Anesthesia (2021) Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American Heart Association. Circulation 144. https://doi.org/10.1161/CIR.0000000000000988
Kochhäuser S, Dechering DG, Dittrich R, Reinke F, Ritter MA, Ramtin S, Duning T, Frommeyer G, Eckardt L (2014) Supraventricular premature beats and short atrial runs predict atrial fibrillation in continuously monitored patients with cryptogenic stroke. Stroke 45:884–886. https://doi.org/10.1161/STROKEAHA.113.003788
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5:136–143. https://doi.org/10.1513/pats.200709-155MG
Zhang D, Ma Y, Xu J, Yi F (2022) Association between obstructive sleep apnea (OSA) and atrial fibrillation (AF): a dose-response meta-analysis. Medicine (Baltimore) 101:e29443. https://doi.org/10.1097/MD.0000000000029443
Linz D, McEvoy RD, Cowie MR, Somers VK, Nattel S, Lévy P, Kalman JM, Sanders P (2018) Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol 3:532. https://doi.org/10.1001/jamacardio.2018.0095
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This retrospective study was approved by the local ethics authority (Ethikkommission der Ärztekammer Westfalen-Lippe und der Medizinischen Fakultät der WWU Münster, Az. 2019–238-f-S).
Conflict of interest
The authors declare no cometing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Kempen, J., Glatz, C., Wolfes, J. et al. Detecting atrial fibrillation in the polysomnography-derived electrocardiogram: a software validation study. Sleep Breath 27, 1753–1757 (2023). https://doi.org/10.1007/s11325-023-02779-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02779-3