Abstract
Purpose
Obstructive sleep apnea (OSA) can impair cognition. Continuous positive airway pressure (CPAP) is a recommended treatment for OSA but its effectiveness on cognitive improvement is uncertain, a finding which may be biased by various durations and adherence to treatment with CPAP. In a meta-analysis assessing high-quality randomized controlled trials (RCTs), we estimated whether or not CPAP benefits cognition in patients with OSA.
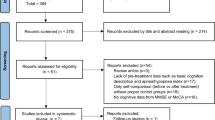
Methods
PRISMA criteria were followed in the performance of this meta-analysis. The weighted mean difference (WMD) and 95% confidence interval (CI) of six neuropsychological scores covering eight cognitive domains were used to evaluate the benefit between CPAP and non-CPAP interventions. Subgroups of different therapeutic durations and adherence, which were divided into short-term (< 8 weeks) and long-term (≥ 12 weeks) durations, and poor (nighttime < 4 h/night) and good (nighttime ≥ 4 h/night) adherence were also analyzed.
Results
Among 16 RCTs, 1529 participants with OSA were included. Comparing the CPAP group and the control group for all treatment durations and adherence, a mild improvement for digit span forward which reflected short-term memory was observed (WMD[95%CI] = 0.67[0.03,1.31], p = 0.04). Trail making test-part B, which reflected executive function was improved for participants with OSA who had good adherence to CPAP (WMD[95%CI] = − 6.24[− 12.60,0.12], p = 0.05). Patients with OSA who received short-term CPAP treatment (WMD[95%CI] = − 7.20[− 12.57, − 1.82], p = 0.009) had a significant improvement in executive function when compared with controls. There was no statistical difference for all scales between long-term (≥ 12 weeks) CPAP treatment group and control group.
Conclusion
The effectiveness of CPAP on cognitive improvement in patients with OSA is limited, although good adherence to CPAP can mildly benefit executive function with short-term effectiveness.

Similar content being viewed by others
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its Supplementary materials.
References
Benjafield AV, Ayas NT, Eastwood PR et al (2019) Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med 7(8):687–698
Ganguli M, Albanese E, Seshadri S et al (2018) Population neuroscience: dementia epidemiology serving precision medicine and population health. Alzheimer Dis Assoc Disord 32(1):1–9
Alzheimer’s disease facts and figures (2021) Alzheimers Dement 17(3):327–406
Jennum P, Rejkjaer-Knudsen M, Ibsen R et al (2020) Long-term health and socioeconomic outcome of obstructive sleep apnea in children and adolescents. Sleep Med 75:441–447
Shieu MM, Dunietz GL, Paulson HL et al (2022) The association between obstructive sleep apnea risk and cognitive disorders: a population-based study. J Clin Sleep Med 18(4):1177–1185
Yaffe K, Laffan AM, Harrison SL et al (2011) Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 306(6):613–619
Ferini-Strambi L, Baietto C, Di Gioia MR et al (2003) Cognitive dysfunction in patients with obstructive sleep apnea (OSA): partial reversibility after continuous positive airway pressure (CPAP). Brain Res Bull 61(1):87–92
Bédard MA, Montplaisir J, Richer F et al (1991) Nocturnal hypoxemia as a determinant of vigilance impairment in sleep apnea syndrome. Chest 100(2):367–370
Mathieu A, Mazza S, Décary A et al (2008) Effects of obstructive sleep apnea on cognitive function: a comparison between younger and older OSAS patients. Sleep Med 9(2):112–120
Bucks RS, Olaithe M, Rosenzweig I et al (2017) Reviewing the relationship between OSA and cognition: where do we go from here? Respirology 22(7):1253–1261
Patil SP, Ayappa IA, Caples SM et al (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American academy of sleep medicine clinical practice guideline. J Clin Sleep Med 15(2):335–343
Gottlieb DJ, Punjabi NM (2020) Diagnosis and management of obstructive sleep apnea: a review. JAMA 323(14):1389–1400
Labarca G, Saavedra D, Dreyse J et al (2020) Efficacy of CPAP for improvements in sleepiness, cognition, mood, and quality of life in elderly patients with OSA: systematic review and meta-analysis of randomized controlled trials. Chest 158(2):751–764
Martinez-Ceron E, Barquiel B, Bezos AM et al (2016) Effect of continuous positive airway pressure on glycemic control in patients with obstructive sleep apnea and type 2 diabetes. A randomized clinical trial. Am J Respir Crit Care Med 194(4):476–85
Abuzaid AS, Al Ashry HS, Elbadawi A et al (2017) Meta-analysis of cardiovascular outcomes with continuous positive airway pressure therapy in patients with obstructive sleep apnea. Am J Cardiol 120(4):693–699
Lin R, Yi M, Yan W et al (2022) Positive airway pressure therapy in heart failure patients comorbid with obstructive sleep apnea: cardiovascular outcomes and nighttime-duration effect. Eur J Clin Invest 31:e13821
Kylstra WA, Aaronson JA, Hofman WF et al (2013) Neuropsychological functioning after CPAP treatment in obstructive sleep apnea: a meta-analysis. Sleep Med Rev 17(5):341–347
Jiang X, Wang Z, Hu N et al (2021) Cognition effectiveness of continuous positive airway pressure treatment in obstructive sleep apnea syndrome patients with cognitive impairment: a meta-analysis. Exp Brain Res 239(12):3537–3552
Wang G, Goebel JR, Li C et al (2020) Therapeutic effects of CPAP on cognitive impairments associated with OSA. J Neurol 267(10):2823–2828
Wang Y, Lin YN, Zhang LY et al (2022) Changes of circulating biomarkers of inflammation and glycolipid metabolism by CPAP in OSA patients: a meta-analysis of time-dependent profiles. Ther Adv Chronic Dis 13:20406223211070920
Sanchez-de-la-Torre M, Gracia-Lavedan E, Benitez ID et al (2022) Long-term Effect of OSA and CPAP Treatment on Blood Pressure in Patients with Acute Coronary Syndrome. Ann Am Thorac Soc. https://doi.org/10.1513/AnnalsATS.202203-260OC
Dalmases M, Sole-Padulles C, Torres M et al (2015) Effect of CPAP on cognition, brain function, and structure among elderly patients with OSA: a randomized pilot study. Chest 148(5):1214–1223
Joyeux-Faure M, Naegele B, Pepin JL et al (2016) Continuous positive airway pressure treatment impact on memory processes in obstructive sleep apnea patients: a randomized sham-controlled trial. Sleep Med 24:44–50
Harvey PD (2019) Domains of cognition and their assessment. Dialogues Clin Neurosci 21(3):227–237
Clark HD, Wells GA, Huët C et al (1999) Assessing the quality of randomized trials: reliability of the Jadad scale. Control Clin Trials 20(5):448–452
Ponce S, Pastor E, Orosa B et al (2019) The role of CPAP treatment in elderly patients with moderate obstructive sleep apnoea: a multicentre randomised controlled trial. Eur Respir J 54(2):1900518. https://doi.org/10.1183/13993003.00518-2019
Wan Y, Zhao F, Liu L et al (2018) Influence of continuous positive airway pressure on sleep status, neuropsychological characteristics in patients with stroke combined with obstructive sleep apnea syndrome [Article]. Chin J Neurol 51(4):256–262
Rosenzweig I, Glasser M, Crum WR et al (2016) Changes in neurocognitive architecture in patients with obstructive sleep apnea treated with continuous positive airway pressure. EBioMedicine 7:221–229
Martinez-Garcia MA, Chiner E, Hernandez L et al (2015) Obstructive sleep apnoea in the elderly: role of continuous positive airway pressure treatment. Eur Respir J 46(1):142–151
McMillan A, Bratton DJ, Faria R et al (2014) Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Respir Med 2(10):804–812
Barnes M, McEvoy RD, Banks S et al (2004) Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med 170(6):656–664
Engleman HM, McDonald JP, Graham D et al (2002) Randomized crossover trial of two treatments for sleep apnea/hypopnea syndrome: continuous positive airway pressure and mandibular repositioning splint. Am J Respir Crit Care Med 166(6):855–859
Montserrat JM, Ferrer M, Hernandez L et al (2001) Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: a randomized controlled study with an optimized placebo. Am J Respir Crit Care Med 164(4):608–613
Monasterio C, Vidal S, Duran J et al (2001) Effectiveness of continuous positive airway pressure in mild sleep apnea-hypopnea syndrome. Am J Respir Crit Care Med 164(6):939–943
Bardwell WA, Ancoli-Israel S, Berry CC et al (2001) Neuropsychological effects of one-week continuous positive airway pressure treatment in patients with obstructive sleep apnea: a placebo-controlled study. Psychosom Med 63(4):579–584
Barbe F, Mayoralas LR, Duran J et al (2001) Treatment with continuous positive airway pressure is not effective in patients with sleep apnea but no daytime sleepiness: a randomized, controlled trial. Ann Intern Med 134(11):1015–23
Engleman HM, Kingshott RN, Wraith PK et al (1999) Randomized placebo-controlled crossover trial of continuous positive airway pressure for mild sleep Apnea/Hypopnea syndrome. Am J Respir Crit Care Med 159(2):461–467
Engleman HM, Martin SE, Kingshott RN et al (1998) Randomised placebo controlled trial of daytime function after continuous positive airway pressure (CPAP) therapy for the sleep apnoea/hypopnoea syndrome. Thorax 53(5):341–345
Engleman HM, Martin SE, Deary IJ et al (1997) Effect of CPAP therapy on daytime function in patients with mild sleep apnoea/hypopnoea syndrome. Thorax 52(2):114–119
Engleman HM, Martin SE, Deary IJ et al (1994) Effect of continuous positive airway pressure treatment on daytime function in sleep apnoea/hypopnoea syndrome. Lancet 343(8897):572–575
Olaithe M, Bucks RS (2013) Executive dysfunction in OSA before and after treatment: a meta-analysis. Sleep 36(9):1297–1305
Kylstra WA, Aaronson JA, Hofman WF et al (2013) Neuropsychological functioning after CPAP treatment in obstructive sleep apnea: a meta-analysis [Review]. Sleep Med Rev 17(5):341–347
Kushida CA, Nichols DA, Holmes TH et al (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep 35(12):1593–1602
Filipovic B, Duric V, Filipovic N et al (2021) Anatomical brain changes and cognitive abilities in patients with obstructive sleep apnea syndrome and nonalcoholic fatty liver disease. Can J Gastroenterol Hepatol 2021:8873652
Feng J, Wu Q, Zhang D et al (2012) Hippocampal impairments are associated with intermittent hypoxia of obstructive sleep apnea. Chin Med J (Engl) 125(4):696–701
Calvo-Flores Guzman B, Elizabeth Chaffey T, Hansika Palpagama T et al (2020) The interplay between beta-amyloid 1–42 (Abeta1-42)-induced hippocampal inflammatory response, p-tau, vascular pathology, and their synergistic contributions to neuronal death and behavioral deficits. Front Mol Neurosci 13:522073
Bucks RS, Olaithe M, Eastwood P (2013) Neurocognitive function in obstructive sleep apnoea: a meta-review. Respirology 18(1):61–70
Pun M, Beaudin AE, Raneri JK et al (2021) Impact of nocturnal oxygen and CPAP on the ventilatory response to hypoxia in OSA patients free of overt cardiovascular disease. Exp Neurol 346:113852
Li M, Sun H, Shen T et al (2022) Increased serum levels of cyclophilin a and matrix metalloproteinase-9 are associated with cognitive impairment in patients with obstructive sleep apnea. Sleep Med 93:75–83
Fernandes M, Placidi F, Mercuri NB et al (2021) The importance of diagnosing and the clinical potential of treating obstructive sleep apnea to delay mild cognitive impairment and Alzheimer’s disease: a special focus on cognitive performance. J Alzheimers Dis Rep 5(1):515–533
Yi M, Zhao W, Tan Y et al (2022) The causal relationships between obstructive sleep apnea and elevated CRP and TNF-alpha protein levels. Ann Med 54(1):1578–1589
Yi M, Tan Y, Pi Y et al (2022) Variants of candidate genes associated with the risk of obstructive sleep apnea. Eur J Clin Invest 52(1):e13673
Custodero C, Ciavarella A, Panza F et al (2022) Role of inflammatory markers in the diagnosis of vascular contributions to cognitive impairment and dementia: a systematic review and meta-analysis. Geroscience 44(3):1373–1392
Ward DD, Wallace LMK, Rockwood K (2021) Cumulative health deficits, APOE genotype, and risk for later-life mild cognitive impairment and dementia. J Neurol Neurosurg Psychiatry 92(2):136–142
Funding
This research was supported by the National Natural Science Foundation of China (No. 82001357), the Hunan Provincial Natural Science Foundation of China (No. 2021JJ80079), the Youth Science Foundation of Xiangya Hospital (No. 2019Q17), the Degree & Postgraduate Education Reform Project of Central South University (No. 2021YJSKSA10), the Undergraduate Education Reform Project of Central South University (No. 2021CG065, No. 2021CG068), and the Research Project of Laboratory Construction and Management of Central South University (No. 202120).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
Not applicable. No human participants included. For this type of study formal consent is not required.
Consent to participate
This article does not contain any studies with human participants performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, J., Yan, W., Yi, M. et al. Efficacy of CPAP duration and adherence for cognitive improvement in patients with obstructive sleep apnea: a meta-analysis of randomized controlled trials. Sleep Breath 27, 973–982 (2023). https://doi.org/10.1007/s11325-022-02687-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-022-02687-y