Abstract
Purpose
To compare the short-term treatment effect of a mandibular advancement device (MAD) with and without previous drug-induced sleep endoscopy (DISE) on polysomnography (PSG) and other sleep apnea–related treatment outcomes (Short Form Health Survey [SF-36] and Epworth Sleepiness Scale [ESS]) among adults with mild, moderate, and severe obstructive sleep apnea (OSA). We hypothesized that using DISE would improve the efficacy of MADs on the sleep apnea parameters.
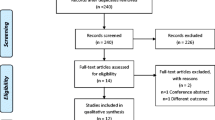
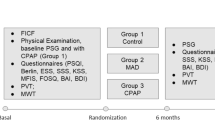
Methods
The study sample consisted of patients with OSA who were unable or unwilling to tolerate a CPAP device, divided into an experimental (with DISE) and a control (without DISE) group.
Results
Of 50 patients with OSA, 40 men (80%), mean age was 48.8 ± 12,3 years. The mean apnea–hypopnea index (AHI) score of both groups decreased significantly between baseline and the 8-week follow-up titration PSG with MAD in situ, from 31.7 ± 17.3 (mean ± SD) apnea–hypopnea episodes/h to 7.0 ± 6.4/h (p < 0.0001) in the experimental group, and from 22.5 ± 16.6 episodes/h to 11.4 ± 8.0/h (p < 0.024) in the control group. Capillary oxygen saturation (SpO2) levels did not change significantly between the two timepoints for either group. The SF-36 (p < 0.023) and ESS (p < 0.036) results of both groups improved significantly between baseline and the 8-week follow-up after starting MAD treatment; however, the improvement in quality of life was significantly more pronounced in the experimental group than in the control group (p < 0.0001).
Conclusion
DISE provides a significant benefit to patients with OSA undergoing MAD treatment. It can be used as a valuable prediction tool in clinical practice for the management of patients with OSA, even those with moderate and severe disease.



Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5(2):136–143
Garvey JF, Pengo MF, Drakatos P, Kent BD (2015) Epidemiological aspects of obstructive sleep apnea. J Thorac Dis 7(5):920–929
Tietjens JR, Claman D, Kezirian EJ, De Marco T, Mirzayan A, Sadroonri B, Goldberg AN, Long C, Gerstenfeld EP, Yeghiazarians Y (2019) Obstructive sleep apnea in cardiovascular disease: a review of the literature and proposed multidisciplinary clinical management strategy. J Am Heart Assoc 8(1):e010440
Xie W, Zheng F, Song X (2014) Obstructive sleep apnea and serious adverse outcomes in patients with cardiovascular or cerebrovascular disease: a PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore) 93(29):e336
Ho ML, Brass SD (2011) Obstructive sleep apnea. Neurol Int 3(3):e15
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504
Rundo JV, Downey R 3rd (2019) Polysomnography. Handb Clin Neurol 160:381–392
Masa JF, Corral J, Pereira R, Duran-Cantolla J, Cabello M, Hernández-Blasco L, Monasterio C, Alonso A, Chiner E, Rubio M, Garcia-Ledesma E, Cacelo L, Carpizo R, Sacristan L, Salord N, Carrera M, Sancho-Chust JN, Embid C, Vázquez-Polo FJ, Negrín MA, Montserrat JM (2011) Effectiveness of home respiratory polygraphy for the diagnosis of sleep apnoea and hypopnoea syndrome. Thorax 66(7):567–573
Cao MT, Sternbach JM, Guilleminault C (2017) Continuous positive airway pressure therapy in obstuctive sleep apnea: benefits and alternatives. Expert Rev Respir Med 11(4):259–272
Rotenberg BW, Murariu D, Pang KP (2016) Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg 45(1):43
Park P, Jeon HW, Han DH, Won TB, Kim DY, Rhee CS, Kim HJ (2016) Therapeutic outcomes of mandibular advancement devices as an initial treatment modality for obstructive sleep apnea. Medicine (Baltimore) 95(46):e5265
Ramar K, Dort LC, Katz SG, Lettieri CJ, Harrod CG, Thomas SM, Chervin RD (2015) Clinical practice guideline for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med 11(7):773–827
Basyuni S, Barabas M, Quinnell T (2018) An update on mandibular advancement devices for the treatment of obstructive sleep apnoea hypopnoea syndrome. J Thorac Dis 10(1):S48–S56
Chan AS, Sutherland K, Schwab RJ, Zeng B, Petocz P, Lee RW, Darendeliler MA, Cistulli PA (2010) The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax 65(8):726–732
Doff MH, Veldhuis SK, Hoekema A, Slater JJ, Wijkstra PJ, de Bont LG, Stegenga B (2012) Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Investig 16(3):689–697
Pliska BT, Nam H, Chen H, Lowe AA, Almeida FR (2014) Obstructive sleep apnea and mandibular advancement splints: occlusal effects and progression of changes associated with a decade of treatment. J Clin Sleep Med 10(12):1285–1291
Fransson AM, Tegelberg A, Johansson A, Wenneberg B (2004) Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop 126(6):687–693
Lim J, Lasserson TJ, Fleetham J, Wright J (2004) Oral appliances for obstructive sleep apnoea. Cochrane Database Syst Rev 4:CD004435
Dieltjens M, Vanderveken OM, Hamans E, Verbraecken JA, Wouters K, Willemen M, De Backer WA, Van de Heyning PH, Braem MJ (2013) Treatment of obstructive sleep apnea using a custom-made titratable duobloc oral appliance: a prospective clinical study. Sleep Breath 17(2):565–572
Burlon G, Tepedino M, Laurenziello M, Troiano G, Cassano M, Romano L, Rinaldi R, Ciavarella D (2020) Evaluation of factors that influence the success rate of OSA treatment with a customised adjustable MAD device - a retrospective study. Acta Otorhinolaryngol Ital 40(4):297–303
Vanderveken O, Vroegop A, de Heyning van, Braem M (2011) Drug-induced sleep endoscopy completed with a simulation bite approach for the prediction of the outcome of treatment of obstructive sleep apnea with mandibular repositioning appliances. Oper Tech Otolayngol Head Neck Surg 22(2):175–182
Gillespie MB, Reddy RP, White DR, Discolo CM, Overdyk FJ, Nguyen SA (2013) A trial of drug-induced sleep endoscopy in the surgical management of sleep-disordered breathing. Laryngoscope 123(1):277–282
De Corso E, Bastanza G, Della Marca G, Grippaudo C, Rizzotto G, Marchese MR, Fiorita A, Sergi B, Meucci D, Di Nardo W, Paludetti G, Scarano E (2015) Drug-induced sleep endoscopy as a selection tool for mandibular advancement therapy by oral device in patients with mild to moderate obstructive sleep apnoea. Acta Otorhinolaryngol Ital 35(6):426–432
Johal A, Hector MP, Battagel JM, Kotecha BT (2007) Impact of sleep nasendoscopy on the outcome of mandibular advancement splint therapy in subjects with sleep-related breathing disorders. J Laryngol Otol 121(7):668–675
Huntley C, Cooper J, Stiles M, Grewal R, Boon M (2018) Predicting success of oral appliance therapy in treating obstructive sleep apnea using drug-induced sleep endoscopy. J Clin Sleep Med 14(8):1333–1337
Koutsourelakis I, Safiruddin F, Ravesloot M, Zakynthinos S, de Vries N (2012) Surgery for obstructive sleep apnea: sleep endoscopy determinants of outcome. Laryngoscope 122(11):2587–2591
Gobbi R, Baiardi S, Mondini S, Cerritelli L, Piccin O, Scaramuzzino G, Milano F, Melotti MR, Mordini F, Pirodda A, Cirignotta F, Sorrenti G (2017) Technique and preliminary analysis of drug-induced sleep endoscopy with online polygraphic cardiorespiratory monitoring in patients with obstructive sleep apnea syndrome. JAMA Otolaryngol Head Neck Surg 143(5):459–465
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268(8):1233–1236
Jo S, Lee JB, Jin Y, Jeong T, Yoon J, Park B (2019) Change in peak expiratory flow rate after the head-tilt/chin-lift maneuver among young, healthy, and conscious volunteers. Clin Exp Emerg Med 6(1):36–42
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, Ramar K, Rogers R, Schwab RJ, Weaver EM, Weinstein MD (2009) Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine 2009. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 5(3):263–76
Tsara V, Serasli E, Amfilochiou A, Constantinidis T, Christaki P (2004) Greek version of the Epworth Sleepiness Scale. Sleep Breath 8(2):91–95
Thorarinsdottir EH, Bjornsdottir E, Benediktsdottir B, Janson C, Gislason T, Aspelund T, Arnardottir ES (2019) Definition of excessive daytime sleepiness in the general population: feeling sleepy relates better to sleep-related symptoms and quality of life than the Epworth Sleepiness Scale score. Results from an epidemiological study. J Sleep Res 28(6):e12852
Anagnostopoulos F, Niakas D, Pappa E (2005) Construct validation of the Greek SF-36 Health Survey. Qual Life Res 14(8):1959–1965
Silva GE, Goodwin JL, Vana KD, Quan SF (2016) Obstructive sleep apnea and quality of life: comparison of the SAQLI, FOSQ, and SF-36 questionnaires. Southwest J Pulm Crit Care 13(3):137–149
Lins L, Carvalho FM (2016) SF-36 total score as a single measure of health-related quality of life: scoping review. SAGE Open Med 4:2050312116671725
Mishra P, Pandey CM, Singh U, Gupta A, Sahu C, Keshri A (2019) Descriptive statistics and normality tests for statistical data. Ann Card Anaesth 22(1):67–72
Okuno K, Sasao Y, Nohara K, Sakai T, Pliska BT, Lowe AA, Ryan CF, Almeida FR (2016) Endoscopy evaluation to predict oral appliance outcomes in obstructive sleep apnoea. Eur Respir J 47(5):1410–1419
Koutsourelakis I, Kontovazainitis G, Lamprou K, Gogou E, Samartzi E, Tzakis M (2021) The role of sleep endoscopy in oral appliance therapy for obstructive sleep apnea. Auris Nasus Larynx 48(2):255–260
Dieleman E, Veugen CCAFM, Hardeman JA, Copper MP (2021) Drug-induced sleep endoscopy while administering CPAP therapy in patients with CPAP failure. Sleep Breath 25(1):391–398
Johal A, Battagel JM, Kotecha BT (2005) Sleep nasendoscopy: a diagnostic tool for predicting treatment success with mandibular advancement splints in obstructive sleep apnoea. Eur J Orthod 27(6):607–614
Vroegop AV, Vanderveken OM, Dieltjens M, Wouters K, Saldien V, Braem MJ, Van de Heyning PH (2013) Sleep endoscopy with simulation bite for prediction of oral appliance treatment outcome. J Sleep Res 22(3):348–355
Aarab G, Lobbezoo F, Wicks DJ, Hamburger HL, Naeije M (2005) Short-term effects of a mandibular advancement device on obstructive sleep apnoea: an open-label pilot trial. J Oral Rehabil 32(8):564–570
Hoekema A, Stegenga B, Wijkstra PJ, van der Hoeven JH, Meinesz AF, de Bont LG (2008) Obstructive sleep apnea therapy. J Dent Res 87(9):882–887
Ezmek B, Piskin B, Sipahi C (2021) Therapeutic efficiency analyses of mandibular advancement devices using polysomnography, smartphone sleep applications, and simple pulse oximetry. Gulhane Med J 63:52–58
Gagnadoux F, Fleury B, Vielle B, Petelle B, Meslier N, N’Guyen XL, Racineux JL (2009) Titrated mandibular advancement versus positive airway pressure for sleep apnoea. Eur Respir J 34(4):914–920
Sharples LD, Clutterbuck-James AL, Glover MJ, Bennett MS, Chadwick R, Pittman MA, Quinnell TG (2016) Meta-analysis of randomised controlled trials of oral mandibular advancement devices and continuous positive airway pressure for obstructive sleep apnoea-hypopnoea. Sleep Med Rev 27:108–124
Phillips CL, Grunstein RR, Darendeliler MA, Mihailidou AS, Srinivasan VK, Yee BJ, Marks GB, Cistulli PA (2013) Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 187(8):879–887
Francis CE, Quinnell T (2021) Mandibular advancement devices for OSA: an alternative to CPAP? Pulm Ther 7(1):25–36
Aarab G, Lobbezoo F, Heymans MW, Hamburger HL, Naeije M (2011) Long-term follow-up of a randomized controlled trial of oral appliance therapy in obstructive sleep apnea. Respiration 82(2):162–168
Vanderveken OM, Dieltjens M, Wouters K, De Backer WA, Van de Heyning PH, Braem MJ (2013) Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax 68(1):91–96
Sutherland K, Vanderveken OM, Tsuda H, Marklund M, Gagnadoux F, Kushida CA, Cistulli PA (2014) Oral appliance treatment for obstructive sleep apnea: an update. J Clin Sleep Med 10(2):215–227
Author information
Authors and Affiliations
Contributions
Evgenia Gogou was involved in the study design and was responsible for the clinical work and data collection and interpretation; Vasilios Psarras was involved in the study design and manuscript preparation; Ioannis Koutsourelakis was involved in the drug-induced sleep endoscopy procedure and interpretation; Demetrios Halazonetis contributed to data acquisition and interpretation; Nikolaos Nikitas Giannakopoulos was involved in data analysis, interpretation of the results, and manuscript preparation; Michail Tzakis was involved in the supervision of the project, the study design, the fabrication details of the mandibular advancement device, data analysis, and manuscript preparation. All authors critically revised the manuscript and gave final approval.
Corresponding author
Ethics declarations
Ethical approval
This study was conducted in accordance with the tenets of the 1964 Declaration of Helsinki and its later amendments, and all procedures involving human participants were approved by the Ethics Committee of the Dental School of Athens University (approval number: 291). Written informed consent was obtained from all study participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oral Appliance Therapy
Rights and permissions
About this article
Cite this article
Gogou, E.S., Psarras, V., Giannakopoulos, N.N. et al. Drug-induced sleep endoscopy improves intervention efficacy among patients treated for obstructive sleep apnea with a mandibular advancement device. Sleep Breath 26, 1747–1758 (2022). https://doi.org/10.1007/s11325-021-02561-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02561-3