Abstract
Purpose
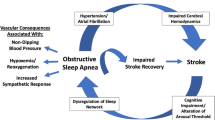
Sleep-disordered breathing (SDB) occurs frequently after stroke and is associated with poor functional outcome and increased mortality. The purpose of this study was to detect changes in SDB over time after acute ischemic stroke and investigate relationships between SDB and stroke etiologies with focus on cerebral small vessel disease.
Methods
From May 2015 to August 2016, we conducted an observational study of 99 patients with mild to moderate stroke (median age: 68 years, range 36–88; 56% men). Polysomnography was performed within 7 days of stroke onset (n = 91) and after 6 months (n = 52). The strokes were classified using the etiological TOAST classification. Total small vessel disease (SVD) scores were calculated based on MRIs.
Results
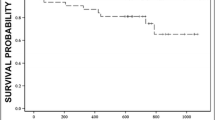
SDB, defined as an apnea–hypopnea index (AHI) ≥ 15, was found in 56% of patients in the acute state and in 44% at follow-up. AHI decreased over time (median change 4.7, 95% confidence interval [95% CI] 0.5–8.9; p = 0.03). Patients with AHI ≥ 15 in both the acute state and at follow-up had higher SVD score at follow-up (p = 0.003). AHI was not associated with ischemic stroke subgroups according to the TOAST classification.
Discussion
In conclusion, 6 months after stroke, AHI decreased, but 44% still had AHI ≥ 15. Persistent SDB in both the acute state and at follow-up was associated with a higher SVD score, but not to the TOAST subgroups. SDB evaluation should be offered to stroke patients, and the effect of SDB on cerebral small vessel disease needs to be further investigated using the well-defined SVD score.
Trial registration
clinicaltrials.gov NCT02111408, April 11, 2014

Similar content being viewed by others
References
Seiler A, Camilo M, Korostovtseva L et al (2019) Prevalence of sleep-disordered breathing after stroke and TIA. American Academy of Neurology. https://doi.org/10.1212/WNL.0000000000006904-7.10.1212/WNL.0000000000006904
Franklin KA, Lindberg E (2015) Obstructive sleep apnea is a common disorder in the population-a review on the epidemiology of sleep apnea. J Thorac Dis 7:1311–1322. https://doi.org/10.3978/j.issn.2072-1439.2015.06.11
Yaggi HK, Concato J, Kernan WN et al (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041. https://doi.org/10.1056/NEJMoa043104
Good DC, Henkle JQ, Gelber D et al (1996) Sleep-disordered breathing and poor functional outcome after stroke. Stroke 27:252–259. https://doi.org/10.1161/001.STR.27.2.252
Jensen MLF, Vestergaard MB, Tønnesen P et al (2018) Cerebral blood flow, oxygen metabolism, and lactate during hypoxia in patients with obstructive sleep apnea. Sleep 41:310. https://doi.org/10.1093/sleep/zsy001
Ponsaing LB, Lindberg U, Rostrup E et al (2018) Impaired cerebrovascular reactivity in obstructive sleep apnea: a case-control study. Sleep Med 43:7–13. https://doi.org/10.1016/j.sleep.2017.10.010
Patel SK, Hanly PJ, Smith EE et al (2015) Nocturnal hypoxemia is associated with white matter hyperintensities in patients with a minor stroke or transient ischemic attack. J Clin Sleep Med 11:1417–1424. https://doi.org/10.5664/jcsm.5278
Lipford MC, Flemming KD, Calvin AD et al (2015) Associations between cardioembolic stroke and obstructive sleep apnea. Sleep 38:1699–1705. https://doi.org/10.5665/sleep.5146
Fisse AL, Kemmling A, Teuber A et al (2017) The association of lesion location and sleep related breathing disorder in patients with acute ischemic stroke. PLoS ONE 12:e0171243. https://doi.org/10.1371/journal.pone.0171243
Šiarnik P, Kollár B, Čarnická Z et al (2015) Characteristics of sleep-disordered breathing in etiologic subtypes of minor-to-moderate acute ischemic stroke. J Stroke Cerebrovasc Dis 24:1087–1093. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.01.023
Brown DL, Mowla A, McDermott M et al (2015) Ischemic stroke subtype and presence of sleep-disordered breathing: the BASIC Sleep Apnea Study. J Stroke Cerebrovasc Dis 24:388–393. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.09.007
Menon D, Sukumaran S, Varma R, Radhakrishnan A (2017) Impact of obstructive sleep apnea on neurological recovery after ischemic stroke: a prospective study. Acta Neurol Scand 136:419–426. https://doi.org/10.1111/ane.12740
Staals J, Makin SDJ, Doubal FN et al (2014) Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology 83:1228–1234. https://doi.org/10.1212/WNL.0000000000000837
Song T-J, Park J-H, Choi KH et al (2017) Moderate-to-severe obstructive sleep apnea is associated with cerebral small vessel disease. Sleep Med 30:36–42. https://doi.org/10.1016/j.sleep.2016.03.006
Adams HP, Bendixen BH, Kappelle LJ et al (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Berry RB, Budhiraja R, Gottlieb DJ et al (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8:597–619. https://doi.org/10.5664/jcsm.2172
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. In: Sleep. pp 667–689
Wardlaw JM, Smith EE, Biessels GJ et al (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12:822–838. https://doi.org/10.1016/S1474-4422(13)70124-8
Devaraj NK (2020) Knowledge, attitude, and practice regarding obstructive sleep apnea among primary care physisians. Sleep and Breathing 24:1581–1590. https://doi.org/10.1007/s11325-020-02040-1
Bradley TD, Floras JS (2009) Obstructive sleep apnoea and its cardiovascular consequences. Lancet 373:82–93. https://doi.org/10.1016/S0140-6736(08)61622-0
Parra O, Arboix A, Bechich S et al (2000) Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack. Am J Respir Crit Care Med 161:375–380
Manconi M, Zavalko I, Cereda C et al (2014) Longitudinal polysomnographic assessment from acute to subacute phase in infratentorial versus supratentorial stroke. Cerebrovasc Dis 37:85–93. https://doi.org/10.1159/000356323
Schwarz EI, Stradling JR, Kohler M (2018) Physiological consequences of CPAP therapy withdrawal in patients with obstructive sleep apnoea—an opportunity for an efficient experimental model. J Thorac Dis 10:S24–S32. https://doi.org/10.21037/jtd.2017.12.142
Funding
This study was funded by the Clinical Stroke Research Unit, Department of Neurology, Rigshospitalet, Glostrup; the Grosser L. F. Foghts Foundation; and the Hoerslev Foundation.
Code availability.
Not applicable.
Author information
Authors and Affiliations
Contributions
SS and HI researched the literature and conceived the study. SS, AW, PJ, and HI were involved in protocol development, data analysis, and data interpretation. AA and FW were involved in patient recruitment and data acquisition. SS wrote the first draft of the manuscript. All the authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study has been approved by the appropriate ethic committee (H-2–2013-091) and the data-protecting agency (GLO-2013–18; IT suite nr. 02385) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate.
All persons gave their written informed consent prior to their inclusion in the study.
Consent for publication.
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simonsen, S.A., Andersen, A.V., West, A.S. et al. Sleep-disordered breathing and cerebral small vessel disease—acute and 6 months after ischemic stroke. Sleep Breath 26, 1107–1113 (2022). https://doi.org/10.1007/s11325-021-02482-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02482-1