Abstract
Purpose
The purpose of the study was to assess polysomnographic indicators of increased mortality risk in patients with stroke or a transient ischemic attack (TIA).
Methods
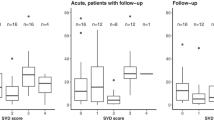
We performed polysomnographies in 63 acute stroke/TIA patients. Mortality data were collected from a national database after a 19–37-month follow-up period.
Results
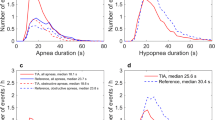
Of the 57 stroke and 6 TIA patients, 9 stroke patients died during follow-up. All nine had moderate or severe sleep-related breathing disorders (SRBDs). Binarily divided, the group with the highest apnea hypopnea index (AHI) had an almost 10-fold higher mortality risk (hazard ratio (HR) 9.71; 95 % confidence interval (CI) 1.20–78.29; p = 0.033) compared to the patients with the lowest AHI. The patients with the longest versus shortest nocturnal wake time had a higher mortality (HR 8.78; 95 % CI 1.1–71.8; p = 0.0428). Lung disease increased mortality (HR 9.92; 95 % CI 2.00–49.23; p = 0.005), and there was a trend toward a higher mortality risk with atrial fibrillation/flutter (HR 3.63; 95 % CI 0.97–13.51; p = 0.055).
Conclusions
In stroke patients, the AHI and nocturnal wake time are indicators of increased mortality risk. SRBDs in stroke patients should receive increased attention.


Similar content being viewed by others
Abbreviations
- AASM:
-
American Academy of Sleep Medicine
- AHI:
-
Apnea hypopnea index
- CSR:
-
Cheyne-Stokes respiration
- EEG:
-
Electroencephalography
- HSAT:
-
Home Sleep Apnea Testing
- mBI:
-
Modified Barthel index
- MRI:
-
Magnetic resonance imaging
- mRS:
-
Modified Rankin Scale
- OSA:
-
Obstructive sleep apnea
- PSG:
-
Polysomnography
- SSS:
-
Scandinavian Stroke Scale
- SRBD:
-
Sleep-related breathing disorder
- TIA:
-
Transient ischemic attack
References
Jennum P, Schultz-Larsen K, Davidsen M, Christensen NJ (1994) Snoring and risk of stroke and ischaemic heart disease in a 70 year old population. A 6-year follow-up study. Int J Epidemiol 23:1159–1164
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041. doi:10.1056/NEJMoa043104
Good DC, Henkle JQ, Gelber D, Welsh J, Verhulst S (1996) Sleep-disordered breathing and poor functional outcome after stroke. Stroke 27:252–259
Johnson KG, Johnson DC (2010) Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin Sleep Med 6:131–137
Ponsaing LB, Iversen HK, Jennum P (2015) Sleep apnea diagnosis varies with the hypopnea criteria applied. Sleep Breath. doi:10.1007/s11325-015-1210-2
Martinez-Garcia MA, Soler-Cataluna JJ, Ejarque-Martinez L, et al. (2009) Continuous positive airway pressure treatment reduces mortality in patients with ischemic stroke and obstructive sleep apnea: a 5-year follow-up study. Am J Respir Crit Care Med 180:36–41. doi:10.1164/rccm.200808-1341OC
Parra O, Arboix A, Montserrat JM, Quinto L, Bechich S, Garcia-Eroles L (2004) Sleep-related breathing disorders: impact on mortality of cerebrovascular disease. Eur Respir J 24:267–272
Martinez-Garcia MA, Galiano-Blancart R, Roman-Sanchez P, Soler-Cataluna JJ, Cabero-Salt L, Salcedo-Maiques E (2005) Continuous positive airway pressure treatment in sleep apnea prevents new vascular events after ischemic stroke. Chest 128:2123–2129. doi:10.1378/chest.128.4.2123
Rowat AM, Dennis MS, Wardlaw JM (2006) Central periodic breathing observed on hospital admission is associated with an adverse prognosis in conscious acute stroke patients. Cerebrovasc Dis 21:340–347. doi:10.1159/000091540
Bonnin-Vilaplana M, Arboix A, Parra O, Garcia-Eroles L, Montserrat JM, Massons J (2012) Cheyne-stokes respiration in patients with first-ever lacunar stroke. Sleep Disord 2012:257890. doi:10.1155/2012/257890
Sahlin C, Sandberg O, Gustafson Y, et al. (2008) Obstructive sleep apnea is a risk factor for death in patients with stroke: a 10-year follow-up. Arch Intern Med 168:297–301. doi:10.1001/archinternmed.2007.70
Bassetti CL, Milanova M, Gugger M (2006) Sleep-disordered breathing and acute ischemic stroke: diagnosis, risk factors, treatment, evolution, and long-term clinical outcome. Stroke 37:967–972. doi:10.1161/01.STR.0000208215.49243.c3
Mansukhani MP, Bellolio MF, Kolla BP, Enduri S, Somers VK, Stead LG (2011) Worse outcome after stroke in patients with obstructive sleep apnea: an observational cohort study. J Stroke Cerebrovasc Dis 20:401–405. doi:10.1016/j.jstrokecerebrovasdis.2010.02.011
Medeiros CA, Bruin VM, Castro-Silva C, Araujo SM, Chaves Junior CM, Bruin PF (2011) Neck circumference, a bedside clinical feature related to mortality of acute ischemic stroke. Rev Assoc Med Bras 57:559–564
Rola R, Jarosz H, Wierzbicka A, et al. (2008) Sleep disorderd breathing and recurrence of cerebrovascular events, case-fatality, and functional outcome in patients with ischemic stroke or transient ischemic attack. J Physiol Pharmacol 59(Suppl 6):615–621
Turkington PM, Allgar V, Bamford J, Wanklyn P, Elliott MW (2004) Effect of upper airway obstruction in acute stroke on functional outcome at 6 months. Thorax 59:367–371
(2008) Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 25:457–507. doi:10.1159/000131083
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus CL, Vaughn BV (2012) The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.0 ed. American Academy of Sleep Medicine, Darien, IL
Iber C, Ancoli-Israel S, Chessonn A (2007) The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. American Academy of Sleep Medicine, Westchester, IL
Berry RB, Budhiraja R, Gottlieb DJ, et al. (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American Academy of sleep medicine. J Clin Sleep Med 8:597–619. doi:10.5664/jcsm.2172
Munoz R, Duran-Cantolla J, Martinez-Vila E, et al. (2012) Central sleep apnea is associated with increased risk of ischemic stroke in the elderly. Acta Neurol Scand 126:183–188. doi:10.1111/j.1600-0404.2011.01625.x
Kuo TB, Li JY, Kuo HK, Chern CM, Yang CC (2016) Differential changes and interactions of autonomic functioning and sleep architecture before and after 50 years of age. Age (Dordr) 38:5. doi:10.1007/s11357-015-9863-0
Scala R, Turkington PM, Wanklyn P, Bamford J, Elliott MW (2009) Acceptance, effectiveness and safety of continuous positive airway pressure in acute stroke: a pilot study. Respir Med 103:59–66. doi:10.1016/j.rmed.2008.08.002
Wessendorf TE, Wang YM, Thilmann AF, Sorgenfrei U, Konietzko N, Teschler H (2001) Treatment of obstructive sleep apnoea with nasal continuous positive airway pressure in stroke. Eur Respir J 18:623–629
Dew MA, Hoch CC, Buysse DJ, et al. (2003) Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med 65:63–73
Bixler EO, Vgontzas AN, Ten HT, Tyson K, Kales A (1998) Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med 157:144–148
Godoy J, Mellado P, Tapia J, Santin J (2009) Obstructive sleep apnea as an independent stroke risk factor: possible mechanisms. Curr Mol Med 9:203–209
Parra O, Arboix A, Bechich S, et al. (2000) Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack. Am J Respir Crit Care Med 161:375–380. doi:10.1164/ajrccm.161.2.9903139
Aaronson JA, Hofman WF, van Bennekom CA, et al. (2016) Effects of continuous positive airway pressure on cognitive and functional outcome of stroke patients with obstructive sleep apnea: a randomized controlled trial. J Clin Sleep Med 12:533–541. doi:10.5664/jcsm.5684
Bravata DM, Concato J, Fried T, et al. (2011) Continuous positive airway pressure: evaluation of a novel therapy for patients with acute ischemic stroke. Sleep 34:1271–1277. doi:10.5665/SLEEP.1254
Acknowledgments
We would like to thank the patients for participating, technologist Mia Dyhr for setting up some of the PSGs, and technologist Helle Leonthin for discussing PSG scoring dilemmas. In addition, we thank Sune Birch, M.Sc., for performing the statistical analyses and Margit Graves Ponsaing, M.A., for proofreading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
We thank the Center for Healthy Aging, Copenhagen University, along with the Danish Center for Sleep Medicine, Department of Clinical Neurophysiology, and the Stroke Unit, Department of Neurology, Rigshospitalet - Glostrup, for the financial support of the study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Comments
The study further substantiates that sleep disordered breathing frequently occurs following an acute stroke. More notably though is the finding that an elevated AHI is associated with an increased risk of short-term mortality. However, their results are provocative as it is unknown if positive airway pressure (PAP) therapy can improve outcomes. Adherence to PAP was low and in many cases this treatment was not accepted. In these highly prevalent disorders, further study is warranted to determine should aggressive treatment algorithms for OSA, to include non-PAP therapies, become part of the treatment plan. Conversely, is there a degree of stroke severity whereby treatment of OSA does not improve morbidity or mortality and treatment of OSA is not indicated.
Vincent Mysliwiec
WA, USA
The work was performed at The Danish Center for Sleep Medicine, Department of Clinical Neurophysiology, Rigshospitalet - Glostrup, Copenhagen University Hospital and The Stroke Unit, Department of Neurology, Rigshospitalet - Glostrup, Copenhagen University Hospital.
Electronic supplementary material
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Ponsaing, L.B., Iversen, H.K. & Jennum, P. Polysomnographic indicators of mortality in stroke patients. Sleep Breath 21, 235–242 (2017). https://doi.org/10.1007/s11325-016-1387-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1387-z