Abstract
Purpose
The clinical significance of the comorbidity of periodic limb movements during sleep (PLMS) in sleep-disordered breathing remains unclear. This study aimed to determine whether or not the presence of PLMS is related to depressed mood and poor quality of life in subjects with obstructive sleep apnea (OSA).
Methods
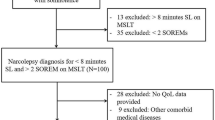
We defined PLMS as a periodic leg movement index of > 15/h. Scores for the Medical Outcomes Study Short Form Health Survey and Beck Depression Inventory were assessed with multiple logistic or linear regression analyses.
Results
Of 1370 subjects with OSA, a prevalence of PLMS was 14.1%. Older age, men, and obesity were positively associated with PLMS. PLMS occurred in 17%, 15%, and 12% of mild, moderate, and severe subjects with OSA, respectively. Severe OSA was less likely to be associated with PLMS than mild OSA. PLMS negatively correlated with physical and mental component summary scores of the health survey but not with Beck Depression Inventory scores after controlling for confounding variables. PLMS were significantly associated with poor sleep architecture on polysomnography. However, the relationship between PLMS and disturbed sleep was no longer significant after adjusting for age.
Conclusions
Health-related quality of life, including physical and mental health but not depressive symptoms, was worse in subjects with OSA and PLMS than in those without PLMS.

Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
American Academy of Sleep Medicine (2014) International classification of sleep disorders, 3rd ed. American Academy of Sleep Medicine, Darien
Scofield H, Roth T, Drake C (2008) Periodic limb movements during sleep: population prevalence, clinical correlates, and racial differences. Sleep 31:1221–1227
Haba-Rubio J, Marti-Soler H, Tobback N et al (2018) Clinical significance of periodic limb movements during sleep: the HypnoLaus study. Sleep Med 41:45–50
Huang TC, Tseng PT, Wu MN, et al (2019) Periodic limb movements during sleep are associated with cardiovascular diseases: a systematic review and meta-analysis. J Sleep Res 28:e12720
Mirza M, Shen WK, Sofi A, Jahangir A, Mori N, Tajik AJ, Jahangir A (2013) Frequent periodic leg movement during sleep is associated with left ventricular hypertrophy and adverse cardiovascular outcomes. J Am Soc Echocardiogr 26:783–790
Giannaki CD, Zigoulis P, Karatzaferi C et al (2013) Periodic limb movements in sleep contribute to further cardiac structure abnormalities in hemodialysis patients with restless legs syndrome. J Clin Sleep Med 9:147–153
Karatas M (2007) Restless legs syndrome and periodic limb movements during sleep: diagnosis and treatment. Neurologist 13:294–301
Budhiraja R, Javaheri S, Pavlova MK, Epstein LJ, Omobomi O, Quan SF (2020) Prevalence and correlates of periodic limb movements in OSA and the effect of CPAP therapy. Neurology 94:e1820–e1827
Kim HJ, Lee SA (2020) Periodic limb movements during sleep may reduce excessive daytime sleepiness in men with obstructive sleep apnea. Sleep Breath 24:1523–1529
Al-Alawi A, Mulgrew A, Tench E, Ryan CF (2006) Prevalence, risk factors and impact on daytime sleepiness and hypertension of periodic leg movements with arousals in patients with obstructive sleep apnea. J Clin Sleep Med 2:281–287
Haba-Rubio J, Staner L, Krieger J, Macher JP (2005) Periodic limb movements and sleepiness in obstructive sleep apnea patients. Sleep Med 6:225–229
Chervin RD (2001) Periodic leg movements and sleepiness in patients evaluated for sleep-disordered breathing. Am J Respir Crit Care Med 164(8 Pt 1):1454–1458
Lee TH, Yen TT, Chiu NY, Chang CC, Hsu WY, Chang YJ, Chang TG (2019) Depression is differently associated with sleep measurement in obstructive sleep apnea, restless leg syndrome and periodic limb movement disorder. Psychiatry Res 273:37–41
Warnes H, Dinner DS, Kotagal P, Burgess RC (1993) Periodic limb movements and sleep apnoea. J Sleep Res 2:38–44
Allen RP, Picchietti DL, Garcia-Borreguero D, Ondo WG, Walters AS, Winkelman JW, Zucconi M, Ferri R, Trenkwalder C, Lee HB; International Restless Legs Syndrome Study Group (2014) Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria--history, rationale, description, and significance. Sleep Med 15:860–73
Iber C, Iber C (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, vol 1. American Academy of Sleep Medicine Westchester, IL, American Academy of Sleep Medicine
Berry RB, Brooks R, Gamaldo CE, Harding SM, Marcus C, Vaughn BV (2012) The AASM manual for the scoring of sleep and associated events. Rules, Terminology and Technical Specifications, Version 2.0. Darien, Illinois, American Academy of Sleep Medicine
Han CW, Lee EJ, Iwaya T et al (2004) Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med 203:189–194
Lee YH, Song JY (1991) A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. J Korean Neuropsychiatry Assoc 10:93–113
Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW (2011) The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 15:377–384
Leary EB, Moore HE IV, Schneider LD, Finn LA, Peppard PE, Mignot E (2018) Periodic limb movements in sleep: prevalence and associated sleepiness in the Wisconsin Sleep Cohort. Clin Neurophysiol 129:2306–2314
Szentkirályi A, Stefani A, Hackner H, et al (2019) Prevalence and associated risk factors of periodic limb movement in sleep in two German population-based studies. Sleep 42:zsy237
Scharf SM, Tubman A, Smale P (2005) Prevalence of concomitant sleep disorders in patients with obstructive sleep apnea. Sleep Breath 9:50–56
Aritake-Okada S, Namba K, Hidano N et al (2012) Change in frequency of periodic limb movements during sleep with usage of continuous positive airway pressure in obstructive sleep apnea syndrome. J Neurol Sci 317:13–16
Leng Y, Blackwell T, Stone KL, Hoang TD, Redline S, Yaffe K (2016) Periodic limb movements in sleep are associated with greater cognitive decline in older men without dementia. Sleep 39:1807–1810
Covassin N, Neikrug AB, Liu L et al (2012) Clinical correlates of periodic limb movements in sleep in Parkinson’s disease. J Neurol Sci 316:131–136
Van Herzeele C, Dhondt K, Roels SP, Raes A, Groen LA, Hoebeke P, Vande WJ (2015) Periodic limb movements during sleep are associated with a lower quality of life in children with monosymptomatic nocturnal enuresis. Eur J Pediatr 174:897–902
Hardy De Buisseret FX, Mairesse O, Newell J, Verbanck P, Neu D (2017) While isolated periodic limb movement disorder significantly impacts sleep depth and efficiency, co-morbid restless leg syndrome mainly exacerbates perceived sleep quality. Eur Neurol 77:272–80
Iriarte J, Murie-Fernandez M, Toledo E et al (2009) Sleep structure in patients with periodic limb movements and obstructive sleep apnea syndrome. J Clin Neurophysiol 26:267–271
Fry JM, DiPhillipo MA, Pressman MR (1989) Periodic leg movements in sleep following treatment of obstructive sleep apnea with nasal continuous positive airway pressure. Chest 96:89–91
Baran AS, Richert AC, Douglass AB, May W, Ansarin K (2003) Change in periodic limb movement index during treatment of obstructive sleep apnea with continuous positive airway pressure. Sleep 26:717–720
Hedli LC, Christos P, Krieger AC (2012) Unmasking of periodic limb movements with the resolution of obstructive sleep apnea during continuous positive airway pressure application. J Clin Neurophysiol 29:339
Chervin RD, Chung S, O’Brien LM et al (2014) Periodic leg movements during sleep in children scheduled for adenotonsillectomy: frequency, persistence, and impact. Sleep Med 15:1362–1369
Yang EH, Hla KM, McHorney CA, Havighurst T, Badr MS, Weber S (2000) Sleep apnea and quality of life. Sleep 23:535–541
Author information
Authors and Affiliations
Contributions
Conceptualization: Sang-Ahm Lee; methodology: Sang-Ahm Lee; writing— original draft preparation: Sang-Ahm Lee; reviewing and editing, supervision: Sang-Ahm Lee; data curation: Hyo Jae Kim, Soo Jeong Kim, So Young Lee; formal analysis: Hyo Jae Kim.
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Asan medical center approved this study.
Consent to participate
This was a retrospective study based on records, and formal consent was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, SA., Kim, S.J., Lee, S.Y. et al. Periodic limb movements during sleep are associated with poor health-related quality of life in patients with obstructive sleep apnea. Sleep Breath 26, 1045–1052 (2022). https://doi.org/10.1007/s11325-021-02469-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02469-y