Abstract
Purpose
Obstructive sleep apnea (OSA) is an important public health problem. Beyond common treatment options, solution-oriented options are needed. Oropharyngeal exercise training may be a research area in this respect. This study aimed to evaluate the effects of oropharyngeal exercise (OPE) in addition to continuous positive airway pressure (CPAP) therapy in patients diagnosed with OSA.
Methods
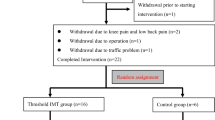
Patients with moderate and severe OSA were screened from the electronic database of our hospital and 41 patients (20: exercise group; 21: control group) were included in the study. Each patient was assessed with CPAP usage time, maximal voluntary ventilation (MVV), maximum inspiratory and expiratory pressure (MIP-MEP), neck circumference, body mass index (BMI), waist-hip ratio, Epworth sleepiness score, Pittsburgh sleep quality index (PSQI), and short-form health survey (SF-36) in the first visit. The OPE was prescribed in addition to CPAP for the exercise group and performed by the patients for 3 months. At the end of the third month, groups were re-assessed with the same parameters.
Results
Most of the patients were men, and the mean age of the study population was 51.9 ± 7.4; the mean apnea–hypopnea index (AHI) in the last polysomnography report was 53.3 ± 27.4. In the exercise group, MVV (p = 0.003), MIP (p = 0.002), MEP (p = 0.024), and SF-36 energy/fatigue (p = 0.020) were observed to increase while the total PSQI score (p = 0.036) decreased. The neck circumference (p = 0.006) and BMI (p = 0.013) were found to be significantly decreased in the exercise group.
Conclusions
We found that OPE training may have improved respiratory muscle strength as well as sleep quality and health-related quality of life in the exercise group. OPE along with CPAP therapy may be recommended in moderate and severe OSA patients who are willing to participate.

Similar content being viewed by others
Availability of data and material
Data is available for data transparency.
Code availability
Not applicable.
References
Lavie P, Lavie L (2008) Cardiovascular morbidity and mortality in obstructive sleep apnea. Curr Pharm Des 14(32):3466–3473. https://doi.org/10.2174/138161208786549317
Kapur VK, Auckley DH, Chowdhuri S et al (2017) Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 13(3):479–504. https://doi.org/10.5664/jcsm.6506
Patil SP, Ayappa IA, Caples SM, John Kimoff R, Patel SR, Harrod CG (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 15(2):335–343. https://doi.org/10.5664/jcsm.7640
Bloch KE (2006) Alternatives to CPAP in the treatment of the obstructive sleep apnea syndrome. Swiss Med Wkly. 136 17–18. 261 267 2006/17/smw-11158
Malhotra A, White DP (2002) Obstructive sleep apnoea. Lancet 360(9328):237–245. https://doi.org/10.1016/S0140-6736(02)09464-3
Schwartz AR, Patil SP, Laffan AM, Polotsky V, Schneider H, Smith PL (2008) Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc Am Thorac Soc 5(2):185–192. https://doi.org/10.1513/pats.200708-137MG
Sforza E, Bacon W, Weiss T, Thibault A, Petiau C, Krieger J (2000) Upper airway collapsibility and cephalometric variables in patients with obstructive sleep apnea. Am J Respir Crit Care Med 161(2):347–352. https://doi.org/10.1164/ajrccm.161.2.9810091
Davidson TM (2003) The great leap forward: the anatomic basis for the acquisition of speech and obstructive sleep apnea. Sleep Med 4(3):185–194. https://doi.org/10.1016/S1389-9457(02)00237-X
Arens R, Marcus CL (2004) Pathophysiology of upper airway obstruction: a developmental perspective. Sleep 27(5):997–1019. https://doi.org/10.1093/sleep/27.5.997
Randerath WJ, Galetke W, Domanski U, Weitkunat R, Ruhle K-H (2004) Tongue-muscle training by intraoral electrical neurostimulation in patients with obstructive sleep apnea. Sleep 27(2):254–259. https://doi.org/10.1093/sleep/27.2.254
Guimarães KC, Drager LF, Genta PR, Marcondes BF, Lorenzi-Filhoy G (2009) Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med 179(10):962–966. https://doi.org/10.1164/rccm.200806-981OC
Engleman HM, Wild MR (2003) Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev 7:81–99
Sateia MJ (2014) International classification of sleep disorders-third edition. Chest 146(5):1387–1394. https://doi.org/10.1378/chest.14-0970
The AASM manual for the scoring of sleep and associated events. Rules, terminology and technical specifications. Version 2, 2012.
Guimarães KCC PH. The phonoaudiological work at obstructive sleep apnea [abstract]. Sleep. 2003;26(A209.)
Graham BL, Steenbruggen I, Miller MR, et al (2019) Standardization of spirometry 2019 update. An official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med;200(8):e70-e88 https://doi.org/10.1164/rccm.201908-1590ST
ATS/ERS statement on respiratory muscle testing (2002) Am J Respir Crit Care Med 166(4):518–624. https://doi.org/10.1164/rccm.166.4.518
Miller MR (2005) Standardisation of spirometry. Eur Respir J 26(2):319–338. https://doi.org/10.1183/09031936.05.00034805
Kevin Norton. Standards for anthropometry assessment. In: Kinanthropometry and exercise physiology. 4th ed. Routledge, London; :68–137.
Gordon CC, Chumlea WC RA. Stature, recumbent length and weight. In: Lohman TG, Roche AF MR, ed. Anthropometric standardization reference manual. Champaign, IL : Human Kinetics Books, ©1988.
Khosla T, Lowe CR (1967) Indices of obesity derived from body weight and height. J Epidemiol Community Heal 21(3):122–128. https://doi.org/10.1136/jech.21.3.122
Johns MW (1992) Reliability and factor analysis of the Epworth sleepiness scale. Sleep 15(4):376–381. https://doi.org/10.1093/sleep/15.4.376
Ağargün MY, Kara HAÖ (1996) The validity and reliability of the Pittsburgh sleep quality index. Published online, Turkish J Psychiatry
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care;30(6):473–483 http://www.ncbi.nlm.nih.gov/pubmed/1593914
Koçyiğit H, Aydemir Ö, Fişek G, Ölmez N MA. Reliability and validity of the Turkish version of short form-36 (SF-36). İlaç ve Tedavi Derg. 12:102–106.
Aydemir Ö KE (2007) Psikiyatride Kullanılan Klinik Ölçekler. In: Psikiyatride Kullanılan Klinik Ölçekler. 3rd ed. Hekimler Yayın Birliği Basım Yayın:346–353. https://doi.org/10.18506/anemon.325977
Ware JE (2000) SF-36 health survey update. Spine (Phila Pa 1976);25(24):3130–3139. doi:https://doi.org/10.1097/00007632-200012150-00008
Camacho M, Certal V, Abdullatif J et al (2015) Myofunctional therapy to treat obstructive sleep apnea: a systematic review and meta-analysis. Sleep 38(5):669–675. https://doi.org/10.5665/sleep.4652
Atilgan E, Kunter E, Algun ZC (2020) Are oropharyngeal exercises effective in obstructive sleep apnea syndrome? J Back Musculoskelet Rehabil 33(2):209–216. https://doi.org/10.3233/BMR-171101
Ieto V, Kayamori F, Montes MI et al (2015) Effects of oropharyngeal exercises on snoring. Chest 148(3):683–691. https://doi.org/10.1378/chest.14-2953
Younis A. Hemmat Baz AAEM. Upper airway exercises in patients with obstructive sleep apnea. http://www2.mans.edu.eg/hospitals/muh/depts/sdbu/Research/Papers/ Upper.pdf
Clark HM (2003) Neuromuscular treatments for speech and swallowing. Am J Speech-Language Pathol 12(4):400–415. https://doi.org/10.1044/1058-0360(2003/086)
Acknowledgements
We would like to thank Ahmet Naci Emecen, MD, who is working in the Department of Public Health, Epidemiology, for helping us with the analysis of data.
Author information
Authors and Affiliations
Contributions
S.Ç. and O.İ. contributed to the concept and design of this study. İ.Ö. contributed to the interpretation of polysomnography data. A.Ö.A. and S.Ö. both equally contributed to the respiratory physiotherapy design. S.Ç. contributed to the data interpretation, writing the manuscript, and preparing figures. O.İ. supervised the project and reviewed the manuscript. All authors approved the final version.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were following the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The local university ethics committee provided ethical approval, with the ethical protocol number 3980-GOA. All eligible patients were informed about the study and those who were willing to participate signed the consent form for participation and publication of data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 55439 KB)
Supplementary file2 (MP4 40538 KB)
Supplementary file3 (MP4 43669 KB)
Rights and permissions
About this article
Cite this article
Çakmakcı, S., Özgen Alpaydın, A., Özalevli, S. et al. The effect of oropharyngeal exercise in patients with moderate and severe obstructive sleep apnea using CPAP: a randomized controlled study. Sleep Breath 26, 567–574 (2022). https://doi.org/10.1007/s11325-021-02423-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02423-y