Abstract
The A3 adenosine receptor (AR) is an important inflammatory and immunological target. However, the underlying mechanisms are not fully understood. Here, we report the gene regulation in HL-60 cells treated acutely with highly selective A3AR agonist MRS5698, positive allosteric modulator (PAM) LUF6000, or both. Both pro- and anti-inflammatory genes, such as IL-1a, IL-1β, and NFκBIZ, are significantly upregulated. During our observations, LUF6000 alone produced a lesser effect, while the MRS5698 + LUF6000 group demonstrated generally greater effects than MRS5698 alone, consistent with allosteric enhancement. The number of genes up- and down-regulated are similar. Pathway analysis highlighted the critical involvement of signaling molecules, including IL-6 and IL-17. Important upstream regulators include IL-1a, IL-1β, TNF-α, NF-κB, etc. PPAR, which modulates eicosanoid metabolism, was highly downregulated by the A3AR agonist. Considering previous pharmacological results and mathematical modeling, LUF6000’s small enhancement of genetic upregulation suggested that MRS5698 is a nearly full agonist, which we demonstrated in both cAMP and calcium assays. The smaller effect of LUF6000 on MRS5698 in comparison to its effect on Cl-IB-MECA was shown in both HL-60 cells endogenously expressing the human (h) A3AR and in recombinant hA3AR-expressing CHO cells, consistent with its HL-60 cell genetic regulation patterns. In summary, by using both selective agonists and PAM, we identified genes that are closely relevant to immunity and inflammation to be regulated by A3AR in differentiated HL-60 cells, a cell model of neutrophil function. In addition, we demonstrated the previously uncharacterized allosteric signaling-enhancing effect of LUF6000 in cells endogenously expressing the hA3AR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adenosine is a modulator of numerous functions by acting on the four adenosine receptor (AR) subtypes [1,2,3]. One of the mechanisms of adenosine-promoted tissue protection and repair has been ascribed to its anti-inflammatory effect [4]. In this context, A3AR modulation has been suggested as a promising approach for treating inflammatory and ischemic conditions. Additionally, A3AR agonists have progressed in clinical trials [2, 5,6,7] despite A3AR having both pro- and anti-inflammatory effects in various cell types [8,9,10,11,12]. Furthermore, Cohen et al. [13] have demonstrated that the A3AR positive allosteric modulator (PAM) N-(3,4-dichloro-phenyl)-2-cyclohexyl-1H-imidazo[4,5-c]quinolin-4-amine (LUF6000) also induced anti-inflammatory effects in three experimental rodent models, by a mechanism related to decreased levels of the transcription factor nuclear factor-κ (NF-κB) p65 protein. Moreover, LUF6000 induced a slight stimulatory effect on the number of normal white blood cells and neutrophils.
The A3AR has generated tremendous interest in anti-inflammatory drug development [7]. Many early studies used Cl-IB-MECA and IB-MECA as selective A3AR agonists, currently used in clinical trials for liver conditions and psoriasis [5,6,7, 14]. However, in light of the only moderate A3AR-selectivity of Cl-IB-MECA and IB-MECA [14], a concentration of ≤10 nM is often advisable for A3AR-specific analysis. Alternatively, A1 and A2AAR antagonists can be combined with Cl-IB-MECA to isolate A3AR’s role. For example, Wagner et al. [9] pre-administered A2AAR antagonist ZM241385 (1 mg/kg body weight) before Cl-IB-MECA treatment to reveal potential unspecific effects of Cl-IB-MECA on the A2AAR. With AR subtype selectivity in mind, Lillo et al. [15] performed RNAseq using striatal primary microglial cultures activated and treated with Cl-IB-MECA (200 nM) and/or A2AAR antagonist SCH58261 (200 nM). These results ultimately demonstrated that the chronic (24 h) A3AR agonist treatment regulated more genes negatively than positively. The associated gene ontology enrichment analysis showed the regulation of genes that participate in immune-related events. Analysis of protein-protein interactions showed that Smad3 and Sp1 genes are regulated by Cl-IB-MECA [15]. Under the conditions of cell activation with an agonist treatment regimen, Cl-IB-MECA tended not to favor gene expression related to neuroprotective microglia. Microarray or RNA-Seq has been used to explore anti- or pro-inflammatory functions of AR modulation in several cell types, including macrophages and microglia [15,16,17]. However, to our knowledge, the role of A3AR in neutrophils has not been explored using genetic approaches such as microarray or RNAseq.
Neutrophils are immune cells that are an important part of the host defense system against infection and tissue injury [18]. In response to these challenges, neutrophils migrate from peripheral blood toward the site of infection through the endothelial cell layer and into tissues [19]. Thus, the pharmacological modulation of neutrophil functions could enhance neutrophil capability against infections and protect tissues during inflammation. In the present study, we studied differentiated HL-60 cells, a commonly used cell line to model neutrophil functions such as cytokine release and migration [20,21,22,23].
The human (h) A3AR endogenously expressed in HL-60 cells has been characterized functionally and using radioligand binding [24, 25]. It was suggested that A3AR expression in HL-60 cells is like that in neutrophils, thus providing a practical model for investigating A3AR’s role. It is noted that A2AAR is also expressed in HL-60 cells [25]. Through studying both human neutrophils and HL-60 cells, Chen et al. [22] suggested that A3AR appears as the crucial AR for regulating neutrophil chemotaxis by controlling cell migration. Both A3AR agonists [26] and A3AR PAMs [13] are of interest as anti-inflammatory agents.
In the present study, we investigated gene regulation following the acute treatment of HL-60 cells with the recently available and highly selective A3AR agonist MRS5698, which we reported to be > 3000-fold receptor subtype selective at both human and rat A3AR [27], and the heterocyclic A3AR-selective PAM LUF6000. In addition to genetic modulation by the exogenous agonist, we also studied the allosteric enhancement by LUF6000 of the endogenously expressed HL-60 cell A3AR, which lacks previous exploration. It remains to be seen if chronic administration of MRS5698 and LUF6000 will be similar to or different than the chronic effects of Cl-IB-MECA, as reported by Lillo et al. [15].
Materials and methods
Materials
The MicroArray chips were purchased from Affymax (New York, NY, USA). Nonselective AR agonist adenosine-5′-N-ethyluronamide (NECA) and other reagents were from Sigma (St. Louis, MO, USA). (1S,2R,3S,4R,5S)-4-(6-((3-Chlorobenzyl)amino)-2-((3,4-difluorophenyl)ethynyl)-9H-purin-9-yl)-2,3-dihydroxy-N-methylbicyclo[3.1.0]hexane-1-carboxamide (MRS5698) was prepared as reported [27]. Our HL-60 cells were from ATCC (Manassas, VA, USA). An AlphaScreen cAMP kit was purchased from PerkinElmer (Waltham, MA). Other CHO cell lines stably expressing the hA3AR were made at the Laboratory of Bioorganic Chemistry, NIDDK (Bethesda, MD, USA). All other reagents were from standard commercial sources and of analytical grade. N-(3,4-Dichloro-phenyl)-2-cyclohexyl-1 H-imidazo[4,5-c]quinolin-4-amine (LUF6000) was synthesized at Leiden/Amsterdam Center for Drug Research (Leiden, The Netherlands) as reported [28]. Calcium assay kits were from Molecular Devices (Sunnyvale, CA, USA).
Cell culture, drug treatment, and cell differentiation
CHO-A3 cells were grown in DMEM/F12 medium with 10% fetal bovine serum and 1% penicillin-streptomycin. HL-60 cells were cultured in RPMI-1640 medium (ATCC, Manassas, VA, USA) supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin. Differentiation of HL-60 cells was accomplished by incubating cells with 1.3% DMSO for seven days before experiments. Our microarray analysis utilized four experimental groups, including a control group, MRS5698 group (1 µM, 20 min treatment), LUF6000 group (3 µM, 20 min treatment), MRS5698 + LUF6000 group (LUF6000 treatment for 20 min, followed by MRS5698 for 20 min). DMSO (5 mM) was used to dissolve the drugs before dilution in aqueous medium.
RNA extraction and real-time PCR
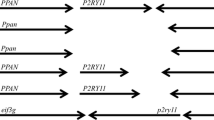
Total RNA was extracted from 107 differentiated HL-60 cells using a RNeasy kit (Qiagen, Redwood City, CA, USA) and was reversed-transcribed with the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA) according to the manufacturer’s protocol. The cDNA was then amplified with gene-specific primers for each of the four AR subtypes, two cytokines IL-1± and IL-1², and GAPDH on a 7900HT Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) according to the manufacturer’s protocol. The TaqMan gene expression assays were from Applied Biosystems (Foster City, CA, USA). Values were normalized to GAPDH and then expressed as relative expression levels. The ΔΔCt method was used to conduct quantitative analysis of data.
Intracellular calcium mobilization
The measurement of calcium mobilization was essentially described previously [29, 30]. Briefly, CHO cells expressing the recombinant hA3AR were grown in a set of 96-well black-wall, clear-bottom plates overnight before the day of the experiment and maintained at 37 °C/5% CO2. Then, we added 100 µl of dye (Calcium 6) to each well. Afterward, the plates were subsequently maintained at room temperature for 60 min. Finally, 50 µl of each compound or a control agonist was added into the respective assay plate wells during the determination of intracellular Ca2+ using a FLIPR (Molecular Devices, San Jose, CA, USA). We utilized a calcium assay kit as directed without washing cells and with probenecid added to the loading dye at a final concentration of 2.5 mM to increase dye retention. The compound plate was prepared using dilutions of various compounds in Hank’s Buffer (pH 7.4). Samples were run in duplicate at room temperature. Cell fluorescence (excitation = 485 nm; emission = 525 nm) was monitored following compound exposure. Increases in intracellular Ca2+ are reported as the maximum fluorescence value after exposure minus the basal fluorescence value before exposure.
Measurement of cyclic AMP levels
CHO-A3 cells were cultured in DMEM/F12 (1:1) medium containing 10% fetal bovine serum, 100 units/ml penicillin, 100 µg/ml streptomycin, and 2 µmol/ml glutamine. For the assay of 3′,5′-cyclic adenosine monophosphate (cAMP), cells were plated in 96-well plates in 100 µl of medium overnight. An AlphaScreen cAMP kit was used for the measurement of cAMP levels as described previously [29, 30]. HL-60 cells 4 × 104 cells/well were suspended in 80 µl Hank’s buffer containing 20 mM HEPES. Where applicable, the A3AR allosteric enhancer LUF6000 (3 µM) was added, and the incubation was continued for 20 min in the presence of phosphodiesterase inhibitor rolipram (10 µM), followed by the addition of A3AR agonist MRS5698 plus 10 µM forskolin to the mixture and incubation for 10 min. The reaction was terminated by centrifugation at 250 g for 5 min at 4°C upon the addition of 100 µL cold 0.3% Tween-20 to each well. Cells were then shaken at room temperature for 10 min. Finally, the reaction was terminated by supernatant removal, and the cells were lysed with the addition of 50 µl of lysis buffer (0.3% Tween-20). For the determination of cAMP production, an AlphaScreen cAMP kit was used according to the manufacturer’s instructions (PerkinElmer, Waltham, MA).
Statistical and data analyses
The microarray RNA normalized data sets were loaded into the commercial bioinformatics software Partek Flow and were aligned with human genome Hg38 alongside the aligner BWA. The gene ANOVA result lists three treatment groups (Group 1, MRS5698, final concentration (1 µM); Group 2 LUF6000, final concentration (3 µM); Group 3, MRS5698 + LUF6000) in comparison to a corresponding control group, which were filtered by both P value of ≤0.05 and an absolute value of fold change ≥1.8. These filtered gene lists were then both used to create a Heat map using Partek Genomic Suite (Chesterfield, MO, USA) and a gene pathway analysis using the commercial software IPA (Qiagen, Redwood City, CA, USA). Functional parameters were calculated using Prism 10.0.0 software (GraphPAD, San Diego, CA, USA). Data was expressed as mean ± standard error. A Student’s t-test (between two conditions) or a One-Way Analysis of Variance (ANOVA) followed by Bonferroni’s multiple comparison tests (between multiple conditions) was used to compare statistically significant differences. Differences yielding P values < 0.05 are considered statistically significant.
Results
Genetic modulation by A3AR selective agonist MRS5698 and allosteric enhancer LUF6000
Table 1 shows the top ten genes upregulated (the complete list of genes is listed in Table S1). Following the treatment of MRS5698 (1 µM) for 20 min, many inflammation-associated genes were found upregulated 3-fold or more. For example, IL1A and IL1B, which are known for their inflammatory functions, are among the most highly upregulated genes. Interestingly, the anti-inflammatory IL-1RN, which reduces the inflammatory effects of cytokines IL-1α and IL-1β and aids the preservation of cell functions, was also highly upregulated. Both NFKBIA and NFKBIZ were also upregulated. NFKBIZ is a regulator of NFKB that inhibits NF-κB activity without affecting its nuclear translocation upon stimulation [31]. NFκB1A is an NF-κB response suppressor that attenuates inflammation, aging, and cancer [32]. TNFAIP3, the tumor necrosis factor α-induced protein 3, has been reported as a key molecule controlling NF-κB activation and has been linked to the development of multiple inflammation-related conditions in humans [33]. CCL4 has been shown to enhance preosteoclast migration alongside its receptor [34]. Additionally, CCR5 downregulation by RANKL promotes osteoclastogenesis [34]. Neutrophil-produced CCL4L2 was negatively related to inhaled corticosteroid (ICS) responsiveness in asthmatics and has been suggested as a potential therapeutic target for ICS-refractory asthma [35]. CCL3L3 has been suggested to be involved in susceptibility to systemic lupus erythematosus, an autoimmune disease [36]. Of the two most upregulated genes IL1A and IL1B, we confirmed the result using quantitative real-time PCR analysis. MRS5698 upregulated IL-1α and IL-1β mRNA expression by 19.1- and 16.4-fold, respectively, which is consistent with the data from microarray analysis.
The changes in the LUF6000 (3 µM, 20 min) group were modest in comparison to the MRS5698 group (Table 1). The MRS5698 + LUF6000 group (LUF6000 was added 20 min before MRS5698 and incubated for an additional 20 min) showed overall larger upregulation compared with the MRS5698 group. This pattern of gene expression by LUF6000 is consistent with its functional enhancement [30]. The complete list of genes with significant upregulation or downregulation is listed in Table S1 (Supporting Information).
Notably, a similar number of genes were upregulated and downregulated upon MRS5698 treatment (20 min) (Fig. 1). These results contrast with a recent report by Lillo et al. [15], reporting that chronic treatment (24 h) of activated mouse microglia with another A3AR agonist Cl-IB-MECA resulted in mostly downregulated genes. The upregulation by LUF6000 and MRS5698 + LUF6000 is generally consistent with that in the MRS5698 alone group.
It is also interesting to note that the heatmap shows that LUF6000 enhanced both the down- and upregulation of genes regulated by the selective A3AR agonist MRS5698 (Fig. 1). Furthermore, even in the absence of an exogenous agonist, the allosteric enhancer LUF6000 alone shows an effect in the regulation of many genes in the same direction as the agonist MRS5698, which is consistent with an early report that another A3AR PAM, LUF6096, induced anti-ischemic cardioprotective effect in the absence of an exogenous agonist [37].
Pathway analysis (Fig. 2) highlighted the critical involvement of important signaling pathways downstream of the A3AR, including IL-6, IL-17, and P38 MAPK signaling, as evidenced by all treatment groups: MRS5698 (G1-S-1-ipa), LUF6000 (G2-S-ipa), MRS5698 + LUF6000 (G3-S-ipa). The complete list of pathways from IPA analysis is included in the Supplementary Information (Figure S1). Canonical peroxisome proliferator-activated receptor (PPAR) and adrenergic receptor signaling pathways are strongly downregulated in both agonist groups and somewhat downregulated even in the LUF6000 group. Retinoic acid receptor (RAR) activation and liver X receptor-retinoid X receptor (LXR/RXR) gene expression is also downregulated in both agonist groups.
Upstream (UPS) analysis of regulators from all three groups MRS5698 (G1-S-1-ipa), LUF6000 (G2-S-ipa), and MRS5698 + LUF6000 (G3-S-ipa) identified important regulatory molecules including IL-1α, IL-1β, TNF-α, NFκB, JNK and ERK (Fig. 3). The complete list of upstream regulators from IPA analysis is included in the Supplementary Information (Figure S2). Analysis of known network interactions and regulated genes reveals IL-1β, IL-17, and TNF as important elements connecting A3AR signaling and function in vivo.
The IPA analysis summary of the MRS5698 + LUF6000 group is shown in Fig. 4. Two partially overlapping pathway nodes are evident: downstream of PPAR, which is highly downregulated by an A3AR agonist, and an anti-inflammatory node. The modulation of eicosanoid/arachidonic acid pathways downstream of PPAR would demonstrate mixed effects on inflammation and metabolism.
Selective A3AR agonist MS5698: functional characterization at four AR subtypes
The moderately selective A3AR agonists IB-MECA and Cl-IB-MECA have been used in many previous pharmacological studies. As mentioned above, at higher concentrations both agonists may activate other AR subtypes. Thus, we chose a more highly selective A3AR agonist in the present study. MRS5698 has been shown in radioligand binding assays to be a selective agonist for both human and mouse A3AR compared to A1AR and A2AAR [27]. However, its activation profile at four ARs has not been compared. To ensure that the effect of MRS5698 used in the genetic regulation is solely via the A3AR, we determined the effect of MRS5698 on cAMP accumulation in CHO cells expressing the recombinant human A3AR. Figure 5 shows that MRS5698 is potent in inhibiting forskolin-stimulated cAMP accumulation (EC50 = 2.52 nM) in hA3AR-expressing cells, and the nucleoside was largely inactive as an agonist at hA1, A2A, and A2BARs at concentrations up to 1 µM (Fig. 5). Thus, we selected a concentration of 1 µM to treat HL-60 cells.
Enhancement of A3AR function in HL-60 cells by LUF6000
LUF6000 at a concentration of 3 µM has demonstrated a substantial enhancement of the A3AR agonist Emax without affecting agonist potency [30]. It has also been shown that LUF6000 is more efficacious in enhancing the Emax of partial agonists than full agonists [30]. At a concentration of 3 µM, LUF6000 enhanced the Emax of Cl-IB-MECA by 41% in an assay of cAMP accumulation [30], while it enhanced the Emax of the full agonist NECA by less than 20%. Here we show that it enhanced the Emax of MRS5698 by 19%, which suggests that MRS5698 is probably a nearly full agonist (Fig. 6).
We further tested the function of MRS5698 and its enhancement by LUF6000 in differentiated HL-60 cells. Similar to CHO cells expressing the recombinant hA3AR, HL-60 cells endogenously expressing the hA3AR LUF6000 also enhanced the agonist efficacy of MRS5698 by ~ 20% (Fig. 7).
MRS5698-induced intracellular calcium mobilization
It has not been previously characterized whether MRS5698 is a full agonist or a partial agonist. The relatively small enhancement by LUF6000 on MRS5698-induced gene upregulation alongside the smaller effect of LUF6000 on the Emax of MRS5698 in the cAMP assay in comparison to the relatively larger effect of LUF6000 on another known partial agonist Cl-IB-MECA [30] suggests that MRS5698 is likely a nearly full A3AR agonist. Thus, in the present study, we compared MRS5698 with a known full A3AR agonist NECA [30] in a calcium mobilization assay in CHO-A3 cells. Figure 8 shows that MRS5698 is as efficacious as NECA as an A3AR agonist but 4.0-fold more potent.
Gene expression comparison of the four AR subtypes in differentiated HL-60 cells
Figure 9 shows that the A3AR is the highest expressed of the four AR subtypes in differentiated HL-60 cells. The A2AAR is also at a relatively high level but is only about 40% of the A3AR. The A1AR and A2BAR are less than 10% of the A3AR expression level. Thus, both the A3AR selectivity of MRS5698 and high A3AR expression in differentiated HL-60 cells guaranteed that the genetic and functional regulation by A3AR agonist occurs via the A3AR. The effects of the A3AR PAM showing changes in parallel to those of the A3AR agonist further supported this nature of regulation. Also, a study of off-target activities of a congeneric series of nucleoside/nucleobase derivatives, including MRS5698, indicated only weak µM affinity at a few other receptors [38].
Discussion
The A3AR is known to play an essential role in various physiological processes, and its activation can influence gene regulation and various cellular responses [1,3,6,7). The present study showed that A3AR activation can lead to the upregulation of genes associated with both pro-inflammation and anti-inflammation, e.g. NFKB1Z and NFKB1A. The NF-κB response suppressor that also attenuates inflammation, aging, and cancer [32], may at least partially explain the anti-inflammatory effect of A3AR agonists. The upregulation of IL-1a and IL-1b could be related to the proinflammatory role of the A3AR.
The A3AR has been reported both pro- and anti-inflammatory depending on cell types [6, 7, 9, 10, 39]. For example, A3AR agonist Cl-IB-MECA (0.1 mg/kg, s.c.) has been found to induce an antiinflammatory and protective effect on the rat liver [39]. Wagner et al. [9] characterized the role of A3AR in a murine model of lung inflammation and found elevated pulmonary A3AR expression levels following lipopolysaccharide (LPS) exposure in vivo. LPS inhalation increased the accumulation of polymorphonuclear leukocytes (PMN) in wild-type and whole-body A3AR(−/−) mice in all lung compartments. Pretreatment with the selective A3AR agonist Cl-IB-MECA significantly decreased the migration of PMNs into the lung interstitium and alveolar air space of wild-type but not A3(−/−) mice. Ren et al. [10] showed that treatment of colonic mucosa from patients with ulcerative colitis (UC) with 100 nM Cl-IB-MECA for 24 h downregulated A3AR expression and upregulated TNF-α, NF-κB, and IL-1β production. A3AR activation by Cl-IB-MECA significantly decreased TNF-α and IL-1β production and attenuated the NF-κB p65 activation in colonic tissues from patients with colonic mucosal inflammation in UC. Hasko et al. [11] reported that in RAW 264.7 macrophages, A3AR agonist IB-MECA, at 0.2 and 0.5 mg/kg, potentiated LPS-stimulated IL-10 production and inhibited LPS-induced TNF-a production, thus suggesting anti-inflammatory action. Sajjadi et al. [12] reported that A3AR stimulation caused a marked decrease in TNF-α mRNA, but not IL-1b, IL-6, or IL-8 mRNA. Thus, the pro- and anti-inflammatory effects of adenosine and the A3AR are dependent on cell types.
The A3AR agonist modulates gene expression and is known to occur through various intracellular signaling pathways. The present study further analyzed pathways potentially involved in the A3AR function. Pathway analysis highlighted several important signaling pathways downstream of the A3AR, including IL-6, IL-17, and P38 MAPK signaling. UPS analysis of regulators from all three groups MRS5698 (G1-S-1-ipa), LUF6000 (G2-S-ipa), and MRS5698 + LUF6000 (G3-S-ipa) identified important regulatory molecules including IL-1, NFkB, JNK, and ERK. Analysis of known network interactions and regulated genes reveals interactions among many important signaling molecules upon A3AR activation, e.g. IL-1b, IL-17, TNF-α, and inflammation response.
IB-MECA and Cl-IB-MECA, which are moderately selective A3AR agonists, have been used in many earlier studies [11, 12, 40]. However, at a higher concentration, both agonists may activate other AR subtypes. For example. Kreckler et al. [41] reported that adenosine inhibits tumor necrosis factor-α release from mouse peritoneal macrophages via A2A and A2B but not the A3AR. Thus, the anti-inflammatory effect of adenosine is dependent on both AR subtypes in addition to cell types. Thus, to elucidate the role of the A3AR (not to activate other AR subtypes), we chose a more selective A3AR agonist MRS5698, and an A3AR allosteric enhancer LUF6000 in the present study.
A critical role of the A3AR in neutrophil behavior has been suggested [22, 42]. The A3AR is also highly expressed in monocyte/macrophage, dendritic cells, cytotoxic and helper T cells, and mast cells [6]. It has also been suggested that chronic treatment with an agonist-induced A3AR downregulation. This is possibly responsible for the suppression of its basal inhibitory effect on cytokine production. However, few if any studies have reported the impact of acute A3AR agonist treatment on genetic regulation.
Ochaion et al. [40] reported that A3AR agonist (1′S,2′R,3′S,4′R,5′S)-4-(2-chloro-6-(3-chlorobenzylamino)-9H-purin-9-yl)-2,3-dihydroxy-N-methylbicyclo[3.1.0]hexane-1-carboxamide (CF502, MRS3558), via de-regulation of the NF-kB signaling pathway, inhibits fibroblast-like synoviocyte (FLS) growth and the inflammatory manifestations of arthritis, supporting the development of A3AR agonists for the treatment of rheumatoid arthritis. The A3AR expression level was downregulated shortly after CF502 treatment. Subsequently, the expression levels of protein kinase B/Akt (PKB/Akt), NF-kB, and TNF-α decreased. However, by studying A3AR knockout mice, Inoue et al. [42] suggested that A3AR antagonists could improve the efficacy of hypertonic saline resuscitation by reducing side effects in patients whose polymorphonuclear neutrophils are activated before hypertonic saline treatment.
Németh et al. [16] hypothesized that adenosine may exert some of its anti-inflammatory effects by decreasing NF-kB activation because gene expression of most of the proinflammatory cytokines inhibited by adenosine is dependent on NF-kB activation. Microarray analyses revealed that mRNA levels of neither TNF-α nor other cytokines were altered by adenosine (100 µM) in either lipopolysaccharide (LPS)-stimulated, or non-stimulated RAW 264.7 macrophages. Although LPS induced expression of several other, noncytokine genes, such as A2BAR, adenosine did not affect the expression of these genes. Furthermore, adenosine (100 µM) as well as NECA and other agonists (10 µM) failed to decrease LPS-induced NF-κB DNA binding, NF-κB promoter activity, p65 nuclear translocation, and inhibitory κB degradation. Thus, the authors suggest that the anti-inflammatory effects of adenosine are independent of NF-κB [16]. Streitova et al. [43] showed mRNA expression for all four AR subtypes in normal and LPS-activated murine RAW 264.7 macrophages. LPS upregulated A2A and A2B mRNA expression, but downregulated A3AR. Ehrchen et al. [44] performed microarray analysis on glucocorticoid-treated monocytes and macrophages and identified glucocorticoid-dependent regulation of 133 genes, including anti-inflammatory A3AR, CD1d, and IL-1 receptor II. Barczyk et al. [45] reported that glucocorticoids promote the survival of anti-inflammatory macrophages via A3AR stimulation. Baram et al. [46] showed that by coupling to Gi3, the A3AR stimulates multiple signaling pathways in human mast cells, leading to upregulation of cytokines, chemokines, and growth factors, although it remains to be shown in neutrophils.
It is known that acute and chronic administration of A3AR agonists produced different functional or behavioral effects [47]. Considering that the A3AR-related gene downregulation based on chronic administration of Cl-IB-MECA has been recently reported [15], we observed that the total genes are almost equally up and downregulated in HL-60 cells treated with MRS5698 for 20 min. However, it is to be noted that the effects of Cl-IB-MECA were determined in mouse cells, and there are significant species-dependent differences in the pharmacology and role of the A3AR [14].
In summary, the present study identified genes and pathways that are regulated by the A3AR activation in a neutrophil model HL-60 cells, by using both a recently available and selective A3AR agonist, MRS5698, and the allosteric enhancer LUF6000. Based on the selectivity profile of both MRS5698 and LUF6000 together with the AR receptor expression profile of HL-60 cells, we are confident that the regulated genes and pathways are solely via the A3ARs. The MRS5698 + LUF6000 group had overall effects larger than MRS5698 alone, consistent with allosteric enhancement. We also observed the allosteric enhancement of the native A3AR function by LUF6000 in HL-60 cells. The patterns of transcriptional enhancement by LUF6000 are consistent with those of the functional enhancement. The findings from the present study support the role of A3AR in inflammation and cancer [6, 7, 48,49,50] and may shed light on the further development of A3AR agonists and allosteric enhancers for various conditions.
Data availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
Abbreviations
- ANOVA:
-
Analysis of Variance
- AR:
-
adenosine receptor
- BWA:
-
Burrows-Wheeler Aligner
- GPCR:
-
G protein-coupled receptor
- HEPES:
-
4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid
- LPS:
-
lipopolysaccharide
- NF-κB:
-
nuclear factor kappa-light-chain-enhancer of activated B cells
- PAM:
-
positive allosteric modulator
- PMN:
-
polymorphonuclear leukocytes
- PPAR:
-
peroxisome proliferator-activated receptor
- RMA:
-
Robust Multichip Average
- UC:
-
ulcerative colitis
- WT:
-
wild-type
References
IJzerman AP, Jacobson KA, Müller CE, Cronstein BN, Cunha RA (2022) International Union of Basic and Clinical Pharmacology. CXII: Adenosine receptors: a further update. Pharmacol Rev 74(2):340–372. https://doi.org/10.1124/pharmrev.121.000445
Chen JF, Eltzschig HK, Fredholm BB (2013) Adenosine receptors as drug targets–what are the challenges? Nat Rev Drug Discov 12(4):265–286. https://doi.org/10.1038/nrd3955
Jacobson KA, Gao ZG (2006) Adenosine receptors as therapeutic targets. Nat Rev Drug Discov 5(3):247–264. https://doi.org/10.1038/nrd1983
Linden J (2005) Adenosine in tissue protection and tissue regeneration. Mol Pharmacol 67(5):1385–1387. https://doi.org/10.1124/mol.105.011783
Jacobson KA, Tosh DK, Jain S, Gao ZG (2019) Historical and current adenosine receptor agonists in preclinical and clinical development. Front Cell Neurosci 13:124. https://doi.org/10.3389/fncel.2019.00124
Jacobson KA, Merighi S, Varani K, Borea PA, Baraldi S, Aghazadeh Tabrizi M, Romagnoli R, Baraldi PG, Ciancetta A, Tosh DK, Gao ZG, Gessi S (2018) A3 adenosine receptors as modulators of inflammation: from medicinal chemistry to therapy. Med Res Rev 38(4):1031–1072. https://doi.org/10.1002/med.21456
Borea PA, Varani K, Vincenzi F, Baraldi PG, Tabrizi MA, Merighi S, Gessi (2015) The A3 adenosine receptor: history and perspectives. Pharmacol Rev 67(1):74–102
Gessi S, Merighi S, Varani K, Leung E, Mac Lennan S, Borea PA (2008) The A3 adenosine receptor: an enigmatic player in cell biology. Pharmacol Ther 117(1):123–140. https://doi.org/10.1016/j.pharmthera.2007.09.002
Wagner R, Ngamsri KC, Stark S, Vollmer I, Reutershan J (2010) Adenosine receptor A3 is a critical mediator in LPS-induced pulmonary inflammation. Am J Physiol Lung Cell Mol Physiol 299(4):L502–512. https://doi.org/10.1152/ajplung.00083.2010
Ren TH, Lv MM, An XM, Leung WK, Seto WK (2020) Activation of adenosine A3 receptor inhibits inflammatory cytokine production in colonic mucosa of patients with ulcerative colitis by downregulating the nuclear factor-kappa B signaling. J Dig Dis 21(1):38–45. https://doi.org/10.1111/1751-2980.12831
Haskó G, Szabó C, Németh ZH, Kvetan V, Pastores SM, Vizi ES (1996) Adenosine receptor agonists differentially regulate IL-10, TNF-alpha, and nitric oxide production in RAW 264.7 macrophages and in endotoxemic mice. J Immunol 157(10):4634–4640
Sajjadi FG, Takabayashi K, Foster AC, Domingo RC, Firestein GS (1996) Inhibition of TNF-alpha expression by adenosine: role of A3 adenosine receptors. J Immunol 156(9):3435–34342
Cohen S, Barer F, Bar-Yehuda S, IJzerman AP, Jacobson KA, Fishman P (2014) A3 adenosine receptor allosteric modulator induces an anti-inflammatory effect: in vivo studies and molecular mechanism of action. Mediators Inflamm 2014:708746. https://doi.org/10.1155/2014/708746
Gao ZG, Auchampach JA, Jacobson KA (2023) Species dependence of A3 adenosine receptor pharmacology and function. Purinergic Signal 19(3):523–550. https://doi.org/10.1007/s11302-022-09910-1
Lillo A, Serrano-Marín J, Lillo J, Raïch I, Navarro G, Franco R (2023) Gene regulation in activated microglia by adenosine A3 receptor agonists: a transcriptomics study. Purinergic Signal. Jan 27. https://doi.org/10.1007/s11302-022-09916-9
Németh ZH, Leibovich SJ, Deitch EA, Vizi ES, Szabó C, Hasko G (2003) cDNA microarray analysis reveals a nuclear factor-kappab-independent regulation of macrophage function by adenosine. J Pharmacol Exp Ther 306(3):1042–1049. https://doi.org/10.1124/jpet.103.052944
Lillo A, Serrano-Marín J, Lillo J, Raïch I, Navarro G, Franco R (2023) Differential gene expression in activated microglia treated with adenosine A2A receptor antagonists highlights olfactory receptor 56 and T-cell activation GTPase-activating protein 1 as potential biomarkers of the polarization of activated microglia. Cells 12:2213. https://doi.org/10.3390/cells12182213
Kolaczkowska E, Kubes P (2013) Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol 13:159–175. https://doi.org/10.1038/nri3399
Van Haastert PJ, Devreotes PN (2004) Chemotaxis: signalling the way forward. Nat Rev Mol Cell Biol 5:626–634. https://doi.org/10.1038/nrm1435
Hauert AB, Martinelli S, Marone C, Niggli V, Differentiated (2002) HL-60 cells are a valid model system for the analysis of human neutrophil migration and chemotaxis. Int J Biochem Cell Biol 34:838–854. https://doi.org/10.1016/s1357-2725(02)00010-9
Woo CH, Yoo MH, You HJ, Cho SH, Mun YC, Seong CM, Kim JH (2003) Transepithelial migration of neutrophils in response to leukotriene B4 is mediated by a reactive oxygen species-extracellular signal-regulated kinase-linked cascade. J Immunol 170:6273–6279. https://doi.org/10.4049/jimmunol.170.12.6273
Chen Y, Corriden R, Inoue Y, Yip L, Hashiguchi N, Zinkernagel A, Nizet V, Insel PA, Junger WG (2006) ATP release guides neutrophil chemotaxis via P2Y2 and A3 receptors. Science 314(5806):1792–1795. https://doi.org/10.1126/science.1132559
Carrigan SO, Pink DB, Stadnyk AW (2007) Neutrophil transepithelial migration in response to the chemoattractant fMLP but not C5a is phospholipase D-dependent and related to the use of CD11b/CD18. J Leukoc Biol 82:1575–1584. https://doi.org/10.1189/jlb.0806528
Kohno Y, Sei Y, Koshiba M, Kim HO, Jacobson KA (1996) Induction of apoptosis in HL-60 human promyelocytic leukemia cells by selective adenosine A3 receptor agonists. Biochem Biophys Res Comm. ;219:904–910. Correction: 1996;221:849
Gessi S, Varani K, Merighi S, Cattabriga E, Iannotta V, Leung E, Baraldi PG, Borea PA (2002) A3 adenosine receptors in human neutrophils and promyelocytic HL60 cells: a pharmacological and biochemical study. Mol Pharmacol 61(2):415–424. https://doi.org/10.1124/mol.61.2.415
Koscsó B, Csóka B, Pacher P, Haskó G (2011) Investigational A3 adenosine receptor targeting agents. Expert Opin Investig Drugs 20(6):757–768. https://doi.org/10.1517/13543784.2011.573785
Tosh DK, Padia J, Salvemini D, Jacobson KA (2015) Efficient, large-scale synthesis and preclinical studies of MRS5698, a highly selective A3 adenosine receptor agonist that protects against chronic neuropathic pain. Purinergic Signal 11:371–387
Göblyös A, Gao ZG, Brussee J, Connestari R, Neves Santiago S, Ye K, IJzerman AP, Jacobson KA (2006) Structure activity relationships of 1H-imidazo[4,5-c]quinolin-4-amine derivatives new as allosteric enhancers of the A3 adenosine receptor. J Med Chem 49:3354–3361
Gao ZG, Levitan IM, Inoue A, Wei Q, Jacobson KA (2023) A2B adenosine receptor activation and modulation by protein kinase C. iScience 26(7):107178. https://doi.org/10.1016/j.isci.2023.107178
Gao ZG, Verzijl D, Zweemer A, Ye K, Göblyös A, Ijzerman AP, Jacobson KA (2011) Functionally biased modulation of A3 adenosine receptor agonist efficacy and potency by imidazoquinolinamine allosteric enhancers. Biochem Pharmacol 82(6):658–668. https://doi.org/10.1016/j.bcp.2011.06.017
Totzke G, Essmann F, Pohlmann S, Lindenblatt C, Jänicke RU, Schulze-Osthoff K (2006) A novel member of the IkappaB family, human IkappaB-zeta, inhibits transactivation of p65 and its DNA binding. J Biol Chem 281(18):12645–12654. https://doi.org/10.1074/jbc.M511956200
Cartwright T, Perkins ND, Wilson L (2016) NFKB1: a suppressor of inflammation, ageing and cancer. FEBS J 283(10):1812–1822. https://doi.org/10.1111/febs.13627
Giordano M, Roncagalli R, Bourdely P, Chasson L, Buferne M, Yamasaki S, Beyaert R, van Loo G, Auphan-Anezin N, Schmitt-Verhulst AM, Verdeil G (2014) The tumor necrosis factor alpha-induced protein 3 (TNFAIP3, A20) imposes a brake on antitumor activity of CD8 T cells. Proc Natl Acad Sci USA 111(30):11115–11120. https://doi.org/10.1073/pnas.1406259111
Lee D, Shin KJ, Kim DW, Yoon KA, Choi YJ, Lee BNR, Cho JY (2018) CCL4 enhances preosteoclast migration and its receptor CCR5 downregulation by RANKL promotes osteoclastogenesis. Cell Death Dis 9(5):495. https://doi.org/10.1038/s41419-018-0562-5
Tsai CH, Lai AC, Lin YC, Chi PY, Chen YC, Yang YH, Chen CH, Shen SY, Hwang TL, Su MW, Hsu IL, Huang YC, Maitland-van der Zee AH, McGeachie MJ, Tantisira KG, Chang YJ, Lee YL (2023) Neutrophil extracellular trap production and CCL4L2 expression influence corticosteroid response in asthma. Sci Transl Med 15(699):eadf3843. https://doi.org/10.1126/scitranslmed.adf3843
Kim YH, Lee EE, Sim HW, Kang EK, Won YH, Lee DE, Hong KM, Song YW (2021) CCL3L3-null status is associated with susceptibility to systemic lupus erythematosus. Sci Rep 11(1):19172. https://doi.org/10.1038/s41598-021-98531-6
Du L, Gao ZG, Nithipatikom K, IJzerman AP, Veldhoven JP, Jacobson KA, Gross GJ, Auchampach JA (2012) Protection from myocardial ischemia/reperfusion injury by a positive allosteric modulator of the A3 adenosine receptor. J Pharmacol Exp Ther 340(1):210–217. https://doi.org/10.1124/jpet.111.187559
Paoletta S, Tosh DK, Salvemini D, Jacobson KA (2014) Structural probing of off-target G protein-coupled receptor activities within a series of adenosine/adenine congeners. PLoS ONE 9:e97858. https://doi.org/10.1371/journal.pone.0097858
Ohana G, Cohen S, Rath-Wolfson L, Fishman P (2016) A3 adenosine receptor agonist, CF102, protects against hepatic ischemia/reperfusion injury following partial hepatectomy. Mol Med Rep 14(5):4335–4341. https://doi.org/10.3892/mmr.2016.5746
Ochaion A, Bar-Yehuda S, Cohen S, Amital H, Jacobson KA, Joshi BV, Gao ZG, Barer F, Patoka R, Del Valle L, Perez-Liz G, Fishman P (2008) The A3 adenosine receptor agonist CF502 inhibits the PI3K, PKB/Akt and NF-kappaB signaling pathway in synoviocytes from rheumatoid arthritis patients and in adjuvant-induced arthritis rats. Biochem Pharmacol 76(4):482–494. https://doi.org/10.1016/j.bcp.2008.05.032
Kreckler LM, Wan TC, Ge ZD, Auchampach JA (2006) Adenosine inhibits tumor necrosis factor-alpha release from mouse peritoneal macrophages via A2A and A2B but not the A3 adenosine receptor. J Pharmacol Exp Ther 317(1):172–180. https://doi.org/10.1124/jpet.105.096016
Inoue Y, Chen Y, Hirsh MI, Yip L, Junger WG (2008) A3 and P2Y2 receptors control the recruitment of neutrophils to the lungs in a mouse model of sepsis. Shock 30:173–177
Štreitová D, Hofer M, Holá J, Vacek A, Pospíšil M (2010) Adenosine A1, A2a, A2b, and A3 receptors in hematopoiesis. 2. Expression of receptor mRNA in resting and lipopolysaccharide-activated mouse RAW 264.7 macrophages. Physiol Res 59(1):139–144. https://doi.org/10.33549/physiolres.931724
Ehrchen J, Steinmüller L, Barczyk K, Tenbrock K, Nacken W, Eisenacher M, Nordhues U, Sorg C, Sunderkötter C, Roth J (2007) Glucocorticoids induce differentiation of a specifically activated, anti-inflammatory subtype of human monocytes. Blood 109(3):1265–1274. https://doi.org/10.1182/blood-2006-02-001115
Barczyk K, Ehrchen J, Tenbrock K, Ahlmann M, Kneidl J, Viemann D, Roth J (2010) Glucocorticoids promote survival of anti-inflammatory macrophages via stimulation of adenosine receptor A3. Blood 116(3):446–455. https://doi.org/10.1182/blood-2009-10-247106
Baram D, Dekel O, Mekori YA, Sagi-Eisenberg R (2010) Activation of mast cells by trimeric G protein Gi3; coupling to the A3 adenosine receptor directly and upon T cell contact. J Immunol 184(7):3677–3688. https://doi.org/10.4049/jimmunol.0901333Epub 2010 Feb 26
Jacobson KA (1998) Adenosine A3 receptors: novel ligands and paradoxical effects. Trends Pharmacol Sci 19(5):184–191. https://doi.org/10.1016/s0165-6147(98)01203-6
Ledderose C, Hefti MM, Chen Y, Bao Y, Seier T, Li L, Woehrle T, Zhang J, Junger WG (2016) Adenosine arrests breast cancer cell motility by A3 receptor stimulation. Purinergic Signal 12:673–685
Notarbartolo M, Lo Cicero S, Meli M, Poma P, Labbozzetta M, Cervello M, D’Alessandro N (2005) Induction of apoptosis by the adenosine derivative IB-MECA in parental or multidrug-resistant HL-60 leukemia cells: possible relationship to the effects on inhibitor of apoptosis protein levels. Chemotherapy 51(5):272–279. https://doi.org/10.1159/000087255
Li S, Huang S, Peng SB (2005) Overexpression of G protein-coupled receptors in cancer cells: involvement in tumor progression. Int J Oncol 27(5):1329–1339
Acknowledgements
Support from the NIDDK Intramural Research Program (ZIADK031117) is acknowledged.
Author information
Authors and Affiliations
Contributions
Zhan-Guo Gao, Kenneth A. Jacobson conceptualized the initial experiments. Zhan-Guo Gao, Weiping Chen, Ray R. Gao performed the experiments. Dilip K. Tosh provided chemical. Zhan-Guo Gao, Weiping Chen, Ray R. Gao, Jonathan Li, John A. Hanover, and Kenneth A. Jacobson contributed to data analysis or interpretation, manuscript writing and revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval
Not applicable, does not involve any human or animal studies.
Funding
Funding support from the NIDDK Intramural Research Program (ZIADK031117) to K.A.J. This work was supported by the Intramural Research Program of the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases for support [ZIADK031117 to K.A.J] and the Genomics Core (J.A.H).
Inclusion and diversity
We support inclusive, diverse and equitable conduct of research.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gao, ZG., Chen, W., Gao, R.R. et al. Genetic and functional modulation by agonist MRS5698 and allosteric enhancer LUF6000 at the native A3 adenosine receptor in HL-60 cells. Purinergic Signalling (2024). https://doi.org/10.1007/s11302-024-09992-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11302-024-09992-z