Abstract
Since the discovery of ATP as an extracellular signalling molecule in 1972, purinergic signalling, mediated by extracellular purines and pyrimidines has been identified in virtually all mammalian tissues and is implicated in regulating fundamental cellular processes. In recent years, there has been an increasing focus on the pathophysiology and potential therapeutic interventions based on purinergic signalling. A vast range of compounds targeting purine receptors are in clinical development, and many more are in preclinical studies, which highlights the fast growth in this research field. As a tribute to Professor Geoffrey Burnstock’s legacy in purinergic signalling, we present here a brief review of compounds targeting purine receptors that are in different stages of clinical trials. The review highlights the 50-year journey from basic research on purinergic receptors to clinical applications of therapies targeting purine receptors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The concept of purinergic signalling, first proposed in 1972 [1] refers to the role of extracellular nucleosides and nucleotides, most notably adenosine and adenosine 5′-triphosphate (ATP), as signalling molecules. It was initially viewed that these molecules act as neurotransmitters, but subsequent studies extended their roles to the regulation of numerous cellular processes, including cell proliferation, differentiation, migration, and apoptosis [2]. Since 1972, four subtypes of P1 (adenosine) receptors, seven subtypes of ATP-gated ion channels (P2X receptors) and eight subtypes of P2Y G protein-coupled receptors have been cloned and sequenced [3, 4]. An increasing focus on the role of these receptors in disease and their therapeutic potential as pharmacological targets for drug development has been apparent in recent years [4, 5]. Several decades following the early pioneering work of Professor Geoffrey Burnstock, the therapeutic potential of purinergic signalling is widely recognised, and translational studies have enabled therapeutic compounds to reach clinical trials. As a tribute to Professor Geoffrey Burnstock, we have prepared this brief review of compounds now in Phase I to Phase IV clinical trials and presented several case studies to describe the translational journey of therapies targeting purine receptors to clinical practice.
Studies and reports for inclusion in this review were selected according to the criteria outlined below. An overview of therapies targeting purine receptors was provided by 110 articles containing 18 reviews, 86 original research papers, two expert opinion papers, one research abstract, one editorial paper, and two commentary papers. Comparative and randomized controlled trials, including clinical trials from Phase I to Phase IV and prospective studies, were included in this review. Three databases were used in the search: the National Institute of Health (NIH) National Library of Medicine Registry [6], the European Clinical Trials Registry [7] and the MEDLINE database (as of 5 March 2022). Key search words were P2X1, P2X2, P2X3, P2X4, P2X5, P2X6, P2X7 receptors, P2Y1, P2Y2, P2Y4, P2Y6, P2Y11, P2Y12, P2Y13, P2Y14 receptors, adenosine A1 receptor, A2A receptor, A2B receptor, A3 receptor, and the individual drug compound names. A total of 669 clinical studies were identified after the initial search. No restrictions were applied on the date of study commencement, completion, or status. The clinical trial identification number, stage of development (Phase I–IV), target disease/conditions, trial status, availability of results, statistical significance for the indicated primary outcome measure, completion of study dates, and publications associated with the trial were recorded (Tables 1, 2, 3). Where the results were published, only articles reported in English were included as references.
Compounds in clinical trials
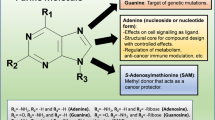
Data from the clinical registries showed that 38 compounds, all agonists and antagonists targeting purine receptors, are currently in clinical development (Tables 1, 2, 3). Four compounds target the P2X3 receptor, and five the P2X7 receptor (Table 1). For P2Y receptors, three compounds target the P2Y2 receptor and different generations of the same compound target the P2Y12 receptor (Table 2). Six compounds target the A1 receptor, ten compounds the A2A receptor, one the A2B receptor, and one the A3 receptor (Table 3, Fig. 1A). These compounds are in different stages of clinical trial. In Phase I, eleven compounds target P2X7, P2Y2, A2A, and A2B receptors. Seventeen compounds targeting P2X3, P2X7, P2Y12, A1, A2A, and A3 receptors are in Phase II. Only three compounds are in Phase III, targeting A1, A2A, and A3 receptors. Six ligands targeting P2Y2, P2Y12 and A2A receptors are in Phase IV under post-approval surveillance evaluation (Fig. 1A). The greater number of compounds targeting the A2A and P2X7 receptors highlights their potential in pharmacotherapy (Table 3). The A2A and P2X7 receptors have gained more attention, likely due to their involvement in inflammatory and immune processes [55]. For example, A2A receptor agonists can suppress peripheral inflammation, and antagonists are used as adjuvant treatments for neuroinflammatory diseases [54]. P2X3, P2X4, P2X7 receptors have been implicated in signalling pathways for pathological pain [65, 66]. In particular, activation of P2X3 subtype expressed in the central terminals of dorsal root ganglia increases nociception by sensitizing nerve fibers associated with the transmission of pain [65]. Blocking P2X3 activities by selective P2X3 antagonists shows promise in reducing pain associated with inflammatory, neuropathic, chronic, and cancer-induced conditions in preclinical studies [65]. P2X7 receptors have also gained attention due to their role in regulating inflammation and the innate and adaptive immune responses [67]. Many studies have focused on manipulating the relation between P2X7 receptor activation and subsequent release of inflammatory cytokines, which can promote cell proliferation or apoptotic cell death [55]. For example, the P2X7 receptor is implicated as a mediator of cancer invasion and metastasis; hence, it has been investigated as a target to inhibit cancer progression [11, 55]. As inflammation and immune processes are involved in most pathologies, sixteen different conditions were identified as targets for purine receptor-based therapies with P1 or P2 receptor ligands under clinical trial (Fig. 1B). Advanced cancer and complications associated with acute coronary syndrome (ACS) and/or cardiovascular disease (CD) appear to be the most targeted, with five different compounds in development for each condition. However, not all compounds were successful in providing significant clinical outcomes. It is not uncommon for compounds to result in less than optimal clinical efficacy when tested in humans despite displaying promising efficacy in preclinical animal studies [66]. For example, P2X7 subtype-specific antagonist AZD9056 showed promising results in an in vivo rat model by suppressing symptoms of rheumatoid arthritis [68, 69]. However, AZD9056 failed to show efficacy for rheumatoid arthritis in a Phase IIa study (NCT00520572). Another unsuccessful example is Rolofylline (KW-3902), an A1 receptor antagonist investigated for preventing renal dysfunction. Although Rolofylline appeared to show potential benefits in improving kidney function in patients with congestive heart failure in a Phase II trial (NCT00159614) [70], it failed to show efficacy in Phase III clinical trials (NCT00354458, NCT00328692) [56] (Table 3). Although there is no definitive explanation for why some trials fail to show clinical efficacy, factors that may influence outcomes include inter-species differences in receptor function or pharmacology, variation in pharmacological profile of compounds for homomeric and heteromeric receptor complexes, and inter-individual variation in receptor function due to single nucleotide polymorphisms [65, 66]. Furthermore, the ubiquitous nature of purinergic receptor expression throughout the body can potentially increase the risk of side effects that may outweigh clinical benefits [71]. However, there are many examples of successful drug development. BIL010t (formerly known as BSCT), a non-functional form of the P2X7 receptor (nf-P2X7) antibody used as topical therapy for basal cell carcinoma [11], and PBF-509, a potent A2A receptor antagonist for the treatment of non-small cell lung cancer [60], were both well-tolerated and safe in Phase I/II trials [11] (Table 3).
Summary of therapeutic compounds in clinical trials targeting purine receptors for specific diseases/conditions. (A) Therapeutic compounds targeting purine receptors in clinical development from Phase I–IV. (B) Purine receptors targeted for specific diseases/conditions in clinical development from Phase I–IV, created with BioRender.com
The development of therapeutics generally follows an exhaustive translational research path from discovery to clinical trial. Approximately 38 compounds targeting purine receptors are at different stages of development, and the most extensively studied are the P2Y12 receptor-based antiplatelet agents clopidogrel, ticagrelor and prasugrel. These are all approved for treating complications associated with the ACS as percutaneous coronary intervention (PCI) [72]. Diquafosol (previously known as INS365), a P2Y2 receptor agonist, is another approved drug that has been commercially successful in treating dry eye syndrome [73]. To illustrate the translational journey from basic science to clinical trials, we present case studies of diquafosol, and a family of P2Y12 receptor antagonists.
P2Y2 receptor agonist: diquafosol
Diquafosol (Tetrasodium ophthalmic solution 3%; INS365, Prolacria, DIQUAS®) is a synthetic dinucleotide derivative of naturally occurring uridine 5′-triphosphate (UTP), acting as a potent P2Y2 receptor agonist [74]. Diquafosol targets P2Y2 receptors expressed in ocular tissues, including palpebral and bulbar conjunctival epithelium, conjunctival goblet cells, corneal epithelial, and meibomian glands [74]. It is used to treat dry eye syndrome by stimulating tear fluid secretion from conjunctival goblet cells, promoting ocular surface hydration and stabilization of the tear film, independent of tear fluid secretion from lacrimal glands [73].
For details on the current use of diquafosol and its tolerance by patients, the reader is directed to a review by Keating et al., 2015 [75]. Here, we will focus on the discovery and translational journey. Basic science discoveries for the target receptor of diquafosol, P2Y2, were published in early 2000–2003. Early work identified P2Y2 receptor mRNA expression to be highly conserved across species, from rhesus monkeys to white rabbits, with expression observed in the conjunctiva, cornea, ciliary body, lens, and pigmented epithelium [76]. Pharmacological and functional evidence of diquafosol action on P2Y2 receptors has stemmed from several cell line and animal models, including non-transformed bovine ciliary epithelial cells [77], human non-pigmented ciliary epithelial cells [78], rabbit ciliary epithelial cells [79], and dry-eye rat model [74]. Earlier in 1999, diquafosol was developed as a P2Y2-specific agonist INS365 (note, the name subsequently changed to diquafosol), effective in airway clearance in sheep [80]. At that time, Inspire Pharmaceuticals had already announced its potential use for dry eye syndrome [81]. The effect of diquafosol on ocular tissues for dry eye treatment was published in 2001 [74]. These preclinical studies were important in demonstrating the mechanism of action of P2Y2 receptor agonists on eye physiology. For example, diquafosol administration in rabbit conjunctiva led to stimulation of Cl− and water transport from the serosal to mucosal conjunctival epithelium [82]. The observed increase in tear fluid secretion was dependent on the dose of diquafosol with no significant change in tear fluid composition [82, 83]. From a clinical viewpoint, a therapeutic effect of diquafosol was demonstrated using the rat dry-eye model, as the application of diquafosol (3.0% or 8.5%) resulted in a 1.5-fold transient increase in tear fluid secretion accompanied by a decline in corneal permeability (51% compared to controls). Both effects resulted in an overall improvement in ocular surface hydration [74]. Additionally, diquafosol improved ocular surface health and mitigated corneal epithelial damage caused by superficial punctate keratopathy. An instillation of diquafosol was associated with an increase in Periodic acid-Schiff (PAS)-stained positive goblet cells in the rat dry-eye model [74] and a significant decrease in corneal fluorescein staining scores compared to controls in a diabetic rat model [84].
Following substantial research and publications between 2000 and 2003, diquafosol was granted priority in the review process by the FDA in 2003 as a diquafosol tetrasodium ophthalmic formulation [85, 86], driving a cascade of clinical trials. The translation of the potential therapeutic effects observed in the preclinical studies can be illustrated by two pivotal Phase IIb and Phase III clinical trials. Both were randomized, double-blind, multi-centre trials, with a primary outcome measure defined as improving corneal and conjunctival epithelial damage after 4 weeks [87, 88]. In the Phase IIb (NCT01189032) study involving 286 participants, a greater dose-dependent reduction in fluorescein corneal staining scores in week 4 was reported in patients receiving either 1% or 3% diquafosol (DQS) [87]. However, when examining the maintenance of fluorescein corneal staining scores at week 6, only the 3% DQS group scores were significantly different from placebo controls (P = 0.005) [87]. Both 1% and 3% DQS groups showed a decrease in fluorescein corneal staining scores (1% DQS, P = 0.037; 3% DQS, P = 0.002) and rose bengal corneal staining scores (1% DQS, P = 0.007; 3% DQS, P = 0.003) compared to placebo at week 4 [87]. This study included subjective dry eye sensation symptom scores as a secondary outcome measure. Patients receiving DQS showed a significant improvement in this secondary outcome measure compared with the placebo (1% DQS, P = 0.003; 3% DQS, P = 0.033) [87]. Concerning dosage, 3% DQS was superior to 1% DQS in efficacy [87]. The efficacy of 3% DQS was also superior to 0.1% sodium hyaluronate ophthalmic solution [89]. Similar to the Phase IIb study, both fluorescein and rose bengal corneal staining scores showed significant improvement in both treatment groups at weeks 2 and 4 (P < 0.05), although the 3% DQS treatment group exhibited greater improvement in mucin coating on the ocular surface at week 4 than 0.1% sodium hyaluronate [89]. Similar improvement in subjective dry-eye-related symptoms and corneal and conjunctival fluorescein staining scores was also observed in a larger Phase III study involving 3196 patients with dry eye disease conducted over two months (P < 0.001) [88]. Adverse reactions to 3% DQS treatment affected 6.3% of patients, including eye discharge, eye irritation, and eye pain [88]. Additional information regarding the effectiveness of 3% DQS as an intervention for dry-eye syndrome was delineated in a Phase IV study involving 580 patients with dry eye disease [90]. It was a prospective, multi-centre, open-label observational study conducted over 12 months [90]. Significant improvements in fluorescein corneal staining scores were observed at 3, 6, 9 and 12 months with DQS treatment (P < 0.001) [388]. Moreover, DQS treatment was associated with a significant reduction in other outcome measures such as Dry Eye-related Duality of Life Scores, ocular symptoms scores, and impact on daily life scores (P < 0.001) [90]. However, it should be noted that the open-label design of this study can be subject to bias in favor of DQS treatment in efficacy measures [90]. The study population included a higher proportion of elderly patients (42.8%, ≥ 70 years), which should also be taken into consideration [90]. DQS 3.0% ophthalmic solution was approved as an intervention for dry eye in 2010 by the Ministry of Health in Japan [91] and is now widely available in other countries, including South Korea, Indonesia, Malaysia, Philippines, Thailand, Vietnam, Cambodia and China [92]. The contributing factors to the success of diquafosol can be attributed to its localized direct delivery in the form of an ‘eye-drop’ and ease of assessment of the target tissue.
P2Y12 receptor antagonist: thienopyridines prasugrel and cangrelor
The discovery of P2Y12 as the drug target for coronary diseases dates back to 1961, when ADP was found to play a functional role in platelet activation and aggregation [93]. The breakthrough came in 2001 when the P2Y12 receptor was cloned and recognized as the molecular identity of the receptor responsible for triggering the potent ADP-induced antithrombotic activity [94]. Strikingly, the expression of P2Y12 was found to be very specific to platelets and showed negligible expression in most other tissues [94]. The strong link between the P2Y12 and ADP-induced platelet aggregation has set a rapid rise in investigations of P2Y12 as a potential therapeutic target for blood clotting conditions and led to the development of thienopyridine prodrugs [95, 96]. Thienopyridines are a family of closely related prodrugs. As prodrugs, thienopyridines need to be metabolized by a hepatic enzyme, Cytochrome P-450 (CYP), into the active metabolite to bind to the P2Y12 receptor irreversibly [97]. This blocks ADP binding, subsequently inhibiting platelet activation and aggregation [97]. The actions of thienopyridines are specific to P2Y12 receptor and selectively interfere with platelet activation and aggregation induced by ADP [98, 99].
Subsequent research has led to the development of at least three thienopyridine compounds in the market; first-generation ticlopidine (Ticlid ®), second-generation clopidogrel bisulfate (Plavix®) and third-generation prasugrel (Effient®) [100, 101].
Thienopyridine antiplatelet drugs are indicated for managing and preventing complications after ACS and PCI, including ischemic complications, myocardial infarction (MI), and stent thrombosis [102], albeit with slightly different properties. The first generation ticlopidine was replaced by the second generation clopidogrel due to a better tolerability profile but with similar efficacy. Soon dual antiplatelet therapy with aspirin and clopidogrel became the ‘gold standard’ for patients undergoing stenting and acute coronary syndromes [100, 103]. However, reports of inter-individual variability in responsiveness to clopidogrel from in vitro studies sparked concerns, potentially explained by genetic polymorphisms and cytochrome P-450 polymorphisms, which can manifest as differential pharmacodynamic and therapeutic responses [104]. A heightened platelet reactivity (thienopyridine hypersensitivity reaction) or clopidogrel non-responsiveness (also referred to as clopidogrel resistance) was associated with a high risk of adverse ischemic events such as stent thrombosis [100, 105]. This supported the development of the third-generation thienopyridine prasugrel, which exhibited a superior pharmacodynamic profile to clopidogrel with less interpatient variability and a more potent platelet aggregation response [100, 103, 105]. Pharmacological and functional evidence of prasugrel (CS-747, LY640315, Effient®), 5-[2-cyclopropyl-1-pyridin-2yl acetate] and P2Y12 receptors have been attributed to preclinical research across a number of animal models including rats, beagle dogs, and cynomolgus monkeys [95, 106, 107]. One of the first studies to evaluate the therapeutic effect of prasugrel (CS-747) used a rat model, where single oral administration of prasugrel (0.3–3 mg/kg) produced a dose-related inhibition of ex vivo ADP-induced aggregation in washed platelets [95]. The same dose-dependent inhibition of platelet aggregation following oral administration of prasugrel was observed in a rat model where maximum inhibition was achieved 2–4 h after dosing [106]. A similar potent, dose-related inhibition of ADP-induced platelet aggregation was observed in beagle dogs (0.03–3 mg/kg/day), cynomolgus monkeys (0.1–0.3 mg/kg/day), and rats (3 mg/kg/day) across a 14-day treatment period. Inhibition reached a plateau on days 3 and 5, suggesting a cumulative effect [107]. The order of potency (from high to low) in different animal models was: dogs, humans, monkeys, and rats [107]. When comparing the antiplatelet and antithrombotic potency of prasugrel with its predecessors, the potency of prasugrel exceeded that of clopidogrel and ticlopidine in a rat arterio-venous shunt model [95]. In an ex vivo rat model, clopidogrel exhibited a slower onset of action and antiplatelet potency 13 times lower than prasugrel [106]. A dose-dependency study of prasugrel (0.1–1 mg/kg/day, p.o.) in a rat carotid arterial thrombosis model demonstrated dose-related prolongation of the time to arterial occlusion. CS-747 (prasugrel) had approximately tenfold and 100-fold higher potency when compared to clopidogrel (1–20 mg/kg/day, p.o.) and ticlopidine (30–300 mg/kg/day, p.o.), respectively [107].
The progress of prasugrel from the preclinical studies to clinical trials can be followed from the Phase II JUMBO-TIMI 26 study [108], which served as a feasibility study for one of the pivotal Phase III studies, TRITON-TIMI 38 [109]. The JUMBO-TIMI 26 study involved 904 patients and was the first to report on the use of prasugrel in patients undergoing elective or urgent PCI [97]. Patients were randomized into 1 of 3 prasugrel dosing regimens: low dose (40 mg loading dose (LD) and 7.5 mg maintenance dose (MD)), intermediate-dose (60 mg LD and 10 mg MD), and a high-dose (60 mg LD and 10 mg MD). A control group treated with clopidogrel (300 mg LD and 75 mg MD) was also included [108]. Although patients receiving prasugrel had a slightly lower incidence of major adverse cardiac events, including myocardial infarction, stroke, recurrent myocardial ischemia requiring hospitalization, and thrombosis (7.2%) compared to patients receiving clopidogrel (9.4%), the difference was not statistically significant (P = 0.26) [108]. Patients receiving prasugrel had slightly lower rates (0.5%) of major bleeding, significant bleeding and transfusion events compared to the clopidogrel group (0.8%), although it also was not statistically significant (P = 0.590) [108]. TRITON-TIMI 38 (NCT00097591) was a double-blind, double-dummy, parallel-group, multi-centre, multinational Phase III clinical trial [109]. It involved 13,608 subjects with moderate- to high-risk ACS with planned PCI who were randomized to receive either clopidogrel (300 mg LD and 75 mg MD) or prasugrel (60 mg LD and 10 mg MD) daily for 6–15 months [109]. The primary outcome measure was defined as a combination of cardiovascular death, non-fatal MI, or urgent target vessel revascularization at 30 days [109]. Patients receiving prasugrel reported fewer cardiovascular events (primary outcome measure composite) of 9.9% compared to 12.1% reported from patients receiving clopidogrel (Hazard Ratio (HR), 0.81; 95% Confidence Interval (CI), 0.73–0.090; P < 0.001) [109]. This was driven by a significant reduction in ischemic events among patients receiving prasugrel including myocardial infarction (9.7% for clopidogrel vs. 7.4% for prasugrel; P < 0.001), urgent target vessel revascularization (3.7% for clopidogrel vs. 7.4% for prasugrel; P < 0.001), and stent thrombosis (2.4% clopidogrel versus 1.1% prasugrel; P < 0.001), but there was no significant difference in the rate of stroke [109]. However, prasugrel treatment was associated with an increase in the rate of major bleeding (2.4% prasugrel vs. 1.8% clopidogrel; HR, 1.32; 95% CI, 1.03–1.68; P = 0.03) and life-threatening bleeding (1.4% vs. 0.9%; P = 0.01) events, inclusive of nonfatal bleeding (1.1% vs. 0.9%; HR, 1.25; P = 0.23) and fatal bleeding (0.4% vs. 0.1%; P = 0.002) [109]. There was no significant difference in overall mortality between treatment groups [109]. Notably, in a different Phase III study, TRILOGY-ACS trial (NCT00699998), the more serious or life-threatening bleeding events observed with the prasugrel group in the TRITON study were not observed [110]. This particular trial had a long follow-up of up to 2.5 years, and the risk of the major bleeding event was observed to be similarly low in the two treatment groups, prasugrel (10 mg daily) and clopidogrel (75 mg daily) [110, 111]. As for the efficacy, at 30 months, no significant difference was observed in the rate of death from cardiovascular causes, MI or stroke among patients under the age of 75 (13.9% in the prasugrel group and 16% in the clopidogrel group; HR 0.91; 95% CI 0.79–1.05; P = 0.21) [110]. However, a lower risk of multiple recurrent ischemic events was observed among patients under the age of 75 receiving prasugrel (6%) compared to the clopidogrel group (13%) after 12 months of treatment (HR 0.94; 95% CI 0.79–0.86; P = 0.018), consistent with findings from the TRITON study [109, 110]. In July 2009, prasugrel gained FDA approval as an intervention for reducing thrombotic cardiovascular events in patients with ACS managed with PCI, with a warning indicating a higher risk of bleeding events [112]. Several years after prasugrel became available for clinical use, some concerns were raised in subsequent analysis from the TRILOGY-ACS trial regarding the long-term effects of prasugrel and clopidogrel [113]. In 2020, the manufacturer, Eli Lilly and Co., discontinued production of prasugrel as a business decision; hence it is no longer available in Canada [114] and New Zealand [115]. After many years of success, the gap left by the withdrawal of prasugrel further prompted the use and investigation of reversible non-thienopyridine agents ticagrelor and, most recently, cangrelor.
Cangrelor (also known as AR-C69931MX) is a non-thienopyridine ATP analogue that has different actions to thienopyridines, and is a class of selective antagonists of the P2Y12 receptor [116]. Similar to thienopyridine, cangrelor is a direct-acting antagonist of the P2Y12 receptor; however, unlike thienopyridines, the inhibitory action of cangrelor is reversible [116]. It is delivered intravenously and is characterized by a rapid onset of action with a fast offset of effects due to its short plasma half-life of 3 to 6 min [116]. Furthermore, due to the drug’s short half-life, the platelet function returns to normal within 30 to 60 min after intravenous infusion of Cangrelor [116]. This fast termination of action makes Cangrelor an attractive compound by reducing the risk of potential ischemic or thrombotic complications [116,117,118]. In a Phase II BRIDGE trial (Bridging Anti-Platelet Therapy With Intravenous Agent Cangrelor In Patients Undergoing Cardiac Surgery, NCT00767507), a greater proportion of patients with ACS treated with Cangrelor (0.75 μg/kg per minute) had low levels of platelet reactivity during the treatment period compared with placebo (P < 0.001), with a low risk of thrombotic events [117]. However, in a large-scale international Phase III trial, CHAMPION (Cangrelor Versus Standard Therapy to Achieve Optimal Management of Platelet Inhibition) PCI trial (NCT00305162) reported a contradictory outcome that cangrelor (bolus of 30 μg/kg plus an infusion at 4 μg/kg per minute) was not superior to clopidogrel (loading dose of 600 mg) in reducing the primary composite death, myocardial infarction, or ischemia-driven revascularization at 48 h (P = 0.59) in patients with ACS before PCI [118]. This study was terminated due to insufficient evidence of the clinical effectiveness of cangrelor [6]. Another separate Phase III trial, CHAMPION PHOENIX (NCT01156571) reported that cangrelor significantly reduced the rate of myocardial infarction, ischemia-driven revascularization, or stent thrombosis at 48 h (adjusted odds ratio [OR] with Cangrelor, 0.78; 95% CI, 0.66 to 0.93; P = 0.005) with a lower rate of stent thrombosis compared to clopidogrel (OR, 0.62; 95% CI, 0.43 to 0.90; P = 0.01) [119]. Although several ongoing studies will likely provide additional insight into the clinical use of cangrelor (Table 2), further evaluations on the safety and efficacy of cangrelor are needed.
Conclusion
The development of therapies targeting purine receptors has been a long journey that began with basic research characterising P1 and P2 receptors in health and disease, and this led to the identification of potential therapeutic targets for different conditions. Through the insights gained from preclinical studies and with the increasing interest from clinical researchers, the development of therapies targeting purine receptors became a reality. With 38 therapeutic compounds currently in clinical trials, we should expect more to emerge over the next few decades. Furthermore, building on our knowledge of purinergic signalling in various tissues and the existence of many drug candidates in the pipeline, repurposing the existing drugs as alternative pathways for drug development should also be considered. Substantial progress made in the last two decades is a true reflection of Professor Geoffrey Burnstock’s legacy that has established the field of purinergic signalling and paved the way for the development of purine receptor targeting therapies for several diseases and clinical conditions.
Data availability
Clinical trial information included in this publication are available in a public repository specified in the manuscript.
References
Burnstock G (1972) Purinergic nerves. Pharmacol Rev 24(3):509–581
Ralevic V, Burnstock G (1998) Receptors for purines and pyrimidines. Pharmacol Rev 50(3):413–492
Burnstock G, Knight GE (2004) Cellular distributions and functions of P2 receptor subtypes in different systems. Int Rev Cytol 240:31–304
Burnstock G (2016) Short- and long-term (trophic) purinergic signaling. Philos Trans R Soc B 371(1700):20150422
Huang Z, Xie N, Illes P, Di Virgilio F, Ulrich H, Semyanov A, Verkhratsky A, Sperlagh B, Yu SG, Huang C, Tang Y (2021) From purines to purinergic signalling: molecular functions and human diseases. Signal Transduct Target Ther 6(1):162
ClinicalTrials.gov. National Library of Medicine (US) Bethesda. https://clinicaltrials.gov/. Accessed 5 March 2022
EU Clinical Trials Register. https://www.clinicaltrialsregister.eu/. Accessed 5 March 2022
Abdulqawi R, Dockry R, Holt K, Layton G, McCarthy BG, Ford AP, Smith JA (2015) P2X3 receptor antagonist (AF-219) in refractory chronic cough: a randomized, double-blind, placebo-controlled phase 2 study. Lancet 385(9974):1198–1205
Martinez FJ, Afzal AS, Smith JA, Ford AP, Li JJ, Li Y, Kitt MM, Chronic cough in IPF Study Group (2021) Treatment of persistent cough in subjects with idiopathic pulmonary fibrosis (IPF) with Gfapixant, a P2X3 antagonist, in a randomized, placebo-controlled clinical trial. Pulm Ther 7(2):471–486
Fletcher MC (2022) Selectivity of the P2X3 receptor antagonist Eliapixant, and its potential use in the treatment of endometriosis. Purinergic Signal 18(1):1–3
Gilbert SM, Baird AG, Glazer S, Barden JA, Glazer A, Teh LC, King J (2017) A phase I clinical trial demonstrates that nfP2X7-targeted antibodies provide a novel, safe and tolerable topical therapy for basal cell carcinoma. Br J Dermatol 177:12–13
Stock TC, Bloom BJ, Wei N, Ishaq S, Park W, Wang X, Gupta P, Mebus CA (2012) Efficacy and safety of CE-224.535, an antagonist of P2X7 receptor, in treatment of patients with rheumatoid arthritis inadequately controlled by methotrexate. J Rheumatol 39(4):720–727
Diaz VAJ, Tello-Montoliu A, Moreno R, Gonzalez IG, Alonso JAB, Romaguera R, Navarro EM, Salvadores PJ, Galan EP, De Miguel CA, Fernandez GB, Saez AO, Barbeira SF, Roubin SR, Miguez JO, Penaranda AS, Chavarri MV, Fillat AC, Iglesias FC, Romo AI (2019) Assessment of platelet REACtivity after transcatheter aortic valve replacement: the REACTAVI Trial. JACC Cardiovasc Interv 12(1):22–32
Park JB, Koo BW, Choi WG, Kim SY, Park J, Kwan J, Park CG, Kim HS (2013) Comparison of antiplatelet efficacy and tolerability of clopidogrel napadisilate with clopidogrel bisulfate in coronary artery disease patients after percutaneous coronary intervention: a prospective, multicentre, randomized, open-label, phase IV, noninferiority trial. Clin Ther 35(1):28–37
Kim CJ, Park MW, Kim MC, Choo EH, Hwang BH, Lee KY, Choi YS, Kim HY, Yoo KD, Jeon DS, Shin ES, Jeong YH, Seung KB, Jeong MH, Yim HW, Ahn Y, Chang K, TALOS-AMI investigators (2021) Unguided de-escalation from ticagrelor to clopidogrel in stabilized patients with acute myocardial infarction undergoing percutaneous coronary intervention (TALOS-AMI_: an investigator-initiated, open-label, multicentre, non-inferiority, randomized trial. Lancet 398(10308):1305–1316
Lee S, Lee H, Park KW, Kang HJ, Koo BK, Kim HS, Choi D, Kim M, Oh BH (2013) Comparison of antiplatelet effect and safety of clopidogrel napadisilate with clopidogrel bisulfate in coronary artery disease patients: multi-centre, randomized, double-blind, phase IV, non-inferiority clinical trial. Am J Cardiovasc Drugs 13(6):413–424
Tam CC, Kwok J, Wong A, Yung A, Shea C, Kong SH, Tang WH, Siu D, Chan R, Lee S (2017) Genotyping-guided approach versus the conventional approach in selection of oral P2Y12 receptor blockers in Chinese patients suffering from acute coronary syndrome. J Int Med Res 45(1):134–146
Steblovnik K, Blinc A, Mijovski MB, Fister M, Mikuz U, Noc M (2016) Ticagrelor versus Clopidogrel in comatose survivors of out-of-hospital cardiac arrest undergoing percutaneous coronary intervention and hypothermia. Circulation 134(25):2128–2130
Seo K, Tahk S, Yang H, Yoon M, Shin J, Choi S, Lim H, Hwang G, Choi B, Park J, Shin J, Lee Y, Choi Y, Park S, Jin X (2014) Point-of-care measurements of platelet inhibition after clopidogrel loading in patients with acute coronary syndrome: comparison of generic and branded clopidogrel bisulfate. Clin Ther 36(11):1588–1594
Li H, Guo J, Carlson GF, Teng R (2016) Pharmacodynamics, pharmacokinetics, and safety of ticagrelor in Chinese patients with stable coronary artery disease. Br J Clin Pharmacol 82(2):352–361
Natale P, Palmer SC, Saglimbene VM, Ruospo M, Razavian M, Craig JC, Jardine MJ, Webster AC, Strippoli GF (2022) Antiplatelet agents for chronic kidney disease. Cochrane Database Syst Rev 2(2):CD008834
Liu PY, Su CH, Kuo FY, Lee WL, Wang YC, Lin WS, Chu PH, Lu TM, Lo PH, Lee CH, Lan WR, Huang CL, Tsukiyama S, Yang WC, Cheng LC, Rafael V, Nikolajsen C, Yin WH (2022) Prasugrel switching from clopidogrel after percutaneous coronary intervention for acute coronary syndrome in Taiwanese patients: an analysis of safety and efficacy. Cardiovasc Interv Ther 37(2):269–278
Sweeny JM, Angiolillo DJ, Franchi F, Rollini F, Waksman R, Raveendran G, Dangas G, Khan ND, Carlson GF, Zhao Y, Teng R, Mehran R (2017) Impact of diabetes mellitus on the pharmacodynamic effects of ticagrelor versus clopidogrel in troponin-negative acute coronary syndrome patients undergoing ad hoc percutaneous coronary intervention. J Am Heart Assoc 6(4):e005650
Price MJ, Walder JS, Baker BA, Heiselman DE, Jakubowski JA, Logan DK, Winters KJ, Li W, Angiolillo DJ (2012) Recovery of platelet function after discontinuation of prasugrel or clopidogrel maintenance dosing in aspirin-treated patients with stable coronary disease: the recovery trial. J Am Coll Cardiol 59(25):2338–2343
Pourdjabbar A, Hibbert B, Chong AY, Le May MR, Labinaz M, Simard T, Ramirez FD, Lugomirski P, Maze R, Froeschl M, Glover C, Dick A, Marquis JF, Bernick J, Wells G, So DYF, CAPITAL Investigators (2017) A randomized study for optimizing crossover from ticagrelor to clopidogrel in patients with acute coronary syndrome The CAPITAL OPTI-CROSS Study. Thromb Haemost 117(2):393–310
Franchi F, Rollini F, Rivas J, Rivas A, Agarwal M, Briceno M, Wali M, Nawaz A, Silva G, Shaikh Z, Maailiki N, Been L, Pineda AM, Suryadevara S, Soffer D, Zenni MM, Bass TA, Angiolillo DJ (2020) Prasugrel versus ticagrelor in patients with CYP2C19 loss-of-function genotypes: results of a randomized pharmacodynamic study in feasibility investigation of rapid genetic testing. JACC Basic Transl Sci 5(5):419–428
Jeong YH, Oh JH, Yoon HJ, Park Y, Suh J, Lee SW, Lee K, Kim JS, Chun WJ, Park YH, Nam CW, Kim JH, Ahn JH, Hwang SJ, Hwang JY, Tantry US, Gurbel PA, Shin ES (2021) Pharmacodynamic profile and prevalence of bleeding episode in East Asian patients with acute coronary syndromes treated with prasugrel standard-dose versus de-escalation strategy: a randomized A-MATCH trial. Thromb Haemost 121(1):1376–1386
Waksman R, Maya J, Angiolillo DJ, Carlson GF, Teng R, Caplan RJ, Ferdinand KC (2015) Ticagrelor versus clopidogrel in Black patients with stable coronary artery disease: prospective, randomized, open-label, multiple-dose, crossover pilot study. Circ Cardiovasc Interv 8(7):e002232
Reisman AM, Robbins BT, Chou DE, Yugrakh MS, Gross GJ, Privitera L, Nazif T, Sommer RJ (2018) Ticagrelor for refractory migraine/ patent foramen ovale (TRACTOR): an open-label pilot study. Neurology 91(22):1010–1017
Sibbing D, Aradi D, Jacobshagen C, Gross L, Trenk D, Geisler T, Orban M, Hadamitzky M, Merkely B, Kiss RG, Komocsi A, Dezsi CA, Holdt L, Felix SB, Parma R, Klopotowski M, Schwinger RHG, Rieber J, Huber K, Neumann FJ, Koltowski L, Mehilli J, Huczek Z, Massberg S (2017) Guided de-escalation of antiplatelet treatment in patients with acute coronary syndrome undergoing percutaneous coronary intervention (TROPICAL-ACS): a randomized, open-label, multicentre trial. Lancet 390(10104):P1747-1757
Gasecka A, Nieuwland R, van der Pol E, Hajji N, Cwiek A, Pluta K, Konwerski M, Filipiak KJ (2019) P2Y12 antagonist ticagrelor inhibits the release of procoagulant extracellular vesicles from activated platelets. Cardiol J 26(6):782–789
Zafar MU, Baber U, Smith DA, Sartori S, Contreras J, Rey-Mendoza J, Linares-Koloffon CA, Escolar G, Mehran R, Fuster V, Badimon JJ (2017) Antithrombotic potency of ticagrelor versus clopidogrel in type-2 diabetic patients with cardiovascular disease. Thromb Haemost 117(10):1981–1988
Lozano I, Rumoroso JR, Perez de Prado A, Moreno R, Hernandez F (2021) Antiplatelet therapy after stenting at the crossroads: easiest or personalized therapy? JACC Cardiovasc Interv 14(8):929–930
Lhermusier T, Lipinski MJ, Drenning D, Marso S, Chen F, Torguson R, Waksman R (2014) Switching patients from clopidogrel to prasugrel in acute coronary syndrome: impact of the clopidogrel loading dose on platelet reactivity. J Interv Cardiol 27(4):365–372
Franchi F, Rollini F, Rios JR, Rivas A, Agarwal M, Kureti M, Nagaraju D, Wali M, Shaikh Z, Briceno M, Nawaz A, Moon JY, Been L, Suryadevara S, Soffer D, Zenni MM, Bass TA, Angiolillo DJ (2018) Pharmacodynamic effects of switching from ticagrelor to clopidogrel in patients with coronary artery disease: results of the SWAP-4 Study. Circulation 137(23):2450–2462
Ariotti S, Ortega-Paz L, van Leeuwen M, Brugaletta S, Leonardi S, Akkerhuis KM, Rimoldi SF, Janssens G, Gianni U, van den Berge JC, Karagiannis A, Windecker S, Valgimigli M, HI-TECH Investigators (2018) Effects of ticagrelor, prasugrel, or clopidogrel in endothelial function and other vascular biomarkers: a randomized crossover study. JACC Cardiovasc Interv 11(16):1576–1586
Park SD, Baek YS, Woo SI, Kim SH, Shin SH, Kim DH, Kwan J, Park KS (2014) Comparing the effect of clopidogrel versus ticagrelor on coronary microvascular dysfunction in acute coronary syndrome patients (TIME trial): study protocol for a randomized controlled trial. Trials 15:151
Alexopoulos D, Xanthopoulou I, Gkizas V, Kassimis G, Theodoropoulos KC, Makris G, Koutsogiannis N, Damelou A, Tsigkas G, Davlouros P, Hahalis G (2012) Randomized assessment of ticagrelor versus prasugrel antiplatelet effects in patients with ST-segment-elevation myocardial infarction. Circ Cardiovasc Interv 5(6):797–804
Lattuca B, Cayla G, Silvain J, Cuisset T, Leclercq F, Mazo-Silberman S, Saint-Etienne C, Delarche N, El Mahmoud R, Carrié D, Souteyrand G, Kerneis M, Hauguel-Moreau M, Zeitouni M, Guedeney P, Diallo A, Collet JP, Vicaut E, Motalescot G, ACTION Study Group (2021) Bleeding in the elderly: risk factors and impact on clinical outcomes after acute coronary syndrome, a sub-study of the randomized ANTARCTIC trial. Am J Cardiovasc Drugs 21(6):681–691
Xanthopoulou I, Bei I, Bampouri T, Barampoutis N, Moulias A, Davlouros P, Alexopoulos D (2018) Absence of differential effect of ticagrelor versus prasugrel maintenance dose on endothelial function in patients with stable coronary artery disease. Hellenic J Cardiol 59(6):338–343
Watanabe H, Morimoto T, Natsuaki M, Yamamoto K, Obayashi Y, Ogita M, Suwa S, Isawa T, Domei T, Yamaji K, Tatsushima S, Watanabe H, Ohya M, Tokuyama H, Tada T, Sakamoto H, Mori H, Suzuki H, Nishikura T, Wakabayashi K, Hibi K, Abe M, Kawai K, Nakao K, Ando K, Tanabe K, Ikari Y, Morino Y, Kadota K, Furukawa Y, Nakagawa Y, Kimura T, STOPDAPT-2 ACS Investigators (2022) Comparison of clopidogrel monotherapy after 1 to 2 months of dual antiplatletlet therapy with 12 months of dual antiplatelet therapy in patients with acute coronary syndrome: the STOPDAPT-2 ACS randomized clinical trial. JAMA Cardiol:e215244
Yang H, Zhang F, Yang J, Zheng M, Cao R, Dai Y, Li C, Yao K, Qian J, Ge J, TARGET DAPT trial investigators (2019) Prospective multicentre open-label randomized controlled trial of 3-month versus 12-months dual antiplatelet therapy after implantation of the new generation biodegradable polymer sirolimus TARGET-eluting coronary stent: protocol of the TARGET DAPT trial. BMJ Open 9(12):e033774
Kim CH, Han JK, Yang HM, Park KW, Lee HY, Kang HJ, Koo BK, Lee N, Cha TJ, Yang TH, Jeong MH, Yoon MH, Lee SU, Lee SJ, Kim JW, Cho JM, Han KR, Pyun WB, Kim HS (2017) Study protocol for a randomised controlled trial: harmonising optimal strategy for treatment of coronary artery stenosis - coronary intervention with next-generation drug-eluting stent platforms and abbreviated dual antiplatelet therapy (HOST-IDEA) trial. BMJ Open 7(10):e016617
Piccolo R, Avvedimento M, Canonico ME, Gargiulo P, Paolillo R, Conti V, Piaz FD, Filippelli A, Morisco C, Simonetti F, Leone A, Marenna A, Bruzzese D, Gargiulo G, Stabile E, Serafino LD, Franzone A, Cirillo P, Esposito G (2022) Platelet inhibition with ticagrelor 60 mg versus 90 mg twice daily in elderly patients with acute coronary syndrome: rationale and design of the PLINY THE ELDER trial. Cardiovasc Drugs The. https://doi.org/10.1007/s10557-021-07302-y
Laine M, Lemesle G, Burtey S, Cayla G, Range G, Quaino G, Canault M, Pankert M, Paganelli F, Puymirat E, Bonello L (2020) TicagRelor Or Clopidogrel in severe or terminal chronic kidney patients Undergoing PERcutaneous coronary intervention for acute coronary syndrome: The TROUPER trial. Am Heart J 225:19–26. https://doi.org/10.1016/j.ahj.2020.04.013
Kubica J, Adamski P, Ostrowska M, Sikora J, Kubica JM, Sroka WD, Stankowska K, Buszko K, Navarese EP, Jilma B, Siller-Matula JM, Marszałł MP, Rość D, Koziński M (2016) Morphine delays and attenuates ticagrelor exposure and action in patients with myocardial infarction: the randomized, double-blind, placebo-controlled IMPRESSION trial. Eur Heart J 37(3):245–252. https://doi.org/10.1093/eurheartj/ehv547
Franchi F, Rollini F, Faz G, Rivas JR, Rivas A, Agarwal M, Briceno M, Wali M, Nawaz A, Silva G, Shaikh Z, Maaliki N, Fahmi K, Been L, Pineda AM, Suryadevara S, Soffer D, Zenni MM, Baber U, Mehran R, …, Angiolillo DJ (2020) Pharmacodynamic effects of vorapaxar in prior myocardial infarction patients treated with potent oral P2Y12 receptor inhibitors with and without aspirin: results of the VORA-PRATIC study. J Am Heart Assoc 9(8):e015865. https://doi.org/10.1161/JAHA.120.015865
Ferreiro JL, Ueno M, Tomasello SD, Capodanno D, Desai B, Dharmashankar K, Seecheran N, Kodali MK, Darlington A, Pham JP, Tello-Montoliu A, Charlton RK, Bass TA, Angiolillo DJ (2011) Pharmacodynamic evaluation of pantoprazole therapy on clopidogrel effects: results of a prospective, randomized, crossover study. Circ Cardiovasc Interv 4(3):273–279. https://doi.org/10.1161/CIRCINTERVENTIONS.110.960997
Franchi F, Rollini F, Rivas A, Wali M, Briceno M, Agarwal M, Shaikh Z, Nawaz A, Silva G, Been L, Smairat R, Kaufman M, Pineda AM, Suryadevara S, Soffer D, Zenni MM, Bass TA, Angiolillo DJ (2019) Platelet inhibition with cangrelor and crushed ticagrelor in patients with ST-segment-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Circulation 139(14):1661–1670. https://doi.org/10.1161/CIRCULATIONAHA.118.038317
Ubaid S, Ford TJ, Berry C, Murray HM, Wrigley B, Khan N, Thomas MR, Armesilla AL, Townend JN, Khogali SS, Munir S, Martins J, Hothi SS, McAlindon EJ, Cotton JM (2019) Cangrelor versus ticagrelor in patients treated with primary percutaneous coronary intervention: impact on platelet activity, myocardial microvascular function and infarct size: a randomized controlled trial. Thromb Haemost 119(7):1171–1181. https://doi.org/10.1055/s-0039-1688789
Gargiulo G, Esposito G, Avvedimento M, Nagler M, Minuz P, Campo G, Gragnano F, Manavifar N, Piccolo R, Tebaldi M, Cirillo P, Hunziker L, Vranckx P, Leonardi S, Heg D, Windecker S, Valgimigli M (2020) Cangrelor, tirofiban, and chewed or standard prasugrel regimens in patients with ST-segment-elevation myocardial infarction: primary results of the FABOLUS-FASTER trial. Circulation 142(5):441–454
Sinnaeve P, Fahrni G, Schelfaut D, Spirito A, Mueller C, Frenoux JM, Hmissi A, Bernaud C, Ufer M, Moccetti T, Atar S, Valgimigli M (2020) Subcutaneous selatogrel inhibits platelet aggregation in patients with acute myocardial infarction. J Am Coll Cardiol 75(20):2588–2597. https://doi.org/10.1016/j.jacc.2020.03.059
Storey RF, Gurbel PA, Ten Berg J, Bernaud C, Dangas GD, Frenoux JM, Gorog DA, Hmissi A, Kunadian V, James SK, Tanguay JF, Tran H, Trenk D, Ufer M, Van der Harst P, Van’t Hof A, Angiolillo DJ (2020) Pharmacodynamics, pharmacokinetics, and safety of single-dose subcutaneous administration of selatogrel, a novel P2Y12 receptor antagonist, in patients with chronic coronary syndromes. Eur Heart J 41(33):3132–3140. https://doi.org/10.1093/eurheartj/ehz807
Jamwal S, Mittal A, Kumar P, Alhayani DM, Al-Aboudi A (2019) Therapeutic potential of agonists and antagonists of A1, A2a, A2b and A3 adenosine. Curr Pharm Des 25:2892–2905
Burnstock G, Knight GE (2018) The potential of P2X7 receptors as a therapeutic target, including inflammation and tumour progression. Purinergic Signal 14(1):1–18
Voors AA, Dittrich HC, Massie BM, DeLucca P, Mansoor GA, Metra M, Cotter G, Weatherley BD, Ponikowski P, Teerlink JR, Cleland JG, O’Connor CM, Givertz MM (2011) Effects of the adenosine A1 receptor antagonist rolofylline on renal function in patients with acute heart failure and renal dysfunction: results from PROTECT (Placebo-Controlled Randomized Study of the Selective Adenosine A1 Receptor Antagonist Rolofylline for Patients Hospitalized with Acute Decompensated Heart Failure and Volume Overload to Assess Treatment Effect on Congestion and Renal Function). J Am Coll Cardiol 57(19):1899–1907. https://doi.org/10.1016/j.jacc.2010.11.057
Lau CL, Beller JP, Boys JA, Zhao Y, Phillips J, Cosner M, Conaway MR, Petroni G, Charles EJ, Mehaffey JH, Mannem HC, Kron IL, Krupnick AS, Linden J (2020) Adenosine A2A receptor agonist (regadenoson) in human lung transplantation. J Heart Lung Transplant 39(6):563–570. https://doi.org/10.1016/j.healun.2020.02.003
Iskandrian AE, Bateman TM, Belardinelli L, Blackburn B, Cerqueira MD, Hendel RC, Lieu H, Mahmarian JJ, Olmsted A, Underwood SR, Vitola J, Wang W, ADVANCE MPI Investigators (2007) Adenosine versus regadenoson comparative evaluation in myocardial perfusion imaging: results of the ADVANCE phase 3 multicenter international trial. J Nucl Cardiol 14(5):645–658. https://doi.org/10.1016/j.nuclcard.2007.06.114
Field JJ, Majerus E, Gordeuk VR, Gowhari M, Hoppe C, Heeney MM, Achebe M, George A, Chu H, Sheehan B, Puligandla M, Neuberg D, Lin G, Linden J, Nathan DG (2017) Randomized phase 2 trial of regadenoson for treatment of acute vaso-occlusive crises in sickle cell disease. Blood Adv 1(20):1645–1649. https://doi.org/10.1182/bloodadvances.2017009613
Chiappori A, Williams CC, Creelan BC, Tanvetyanon T, Gray JE, Haura EB, Thapa R, Chen DT, Beg AA, Boyle TA, Bendiske J, Morris E, Tao A, Hurtado FK, Manenti L, Castro J, Antonia SJ (2018) Phase I/II study of the A2AR antagonist NIR178 (PBF-509), an oral immunotherapy, in patients (pts) with advanced NSCLC. J Clin Oncol 36(15_suppl):9089–9089
Moeller FG, Steinberg JL, Lane SD, Kjome KL, Ma L, Ferre S, Schmitz JM, Green CE, Bandak SI, Renshaw PF, Kramer LA, Narayana PA (2012) Increased orbitofrontal brain activation after administration of a selective adenosine A(2A) antagonist in cocaine dependent subjects. Front Psych 3:44. https://doi.org/10.3389/fpsyt.2012.00044
Barret O, Hannestad J, Vala C, Alagille D, Tavares A, Laruelle M, Jennings D, Marek K, Russell D, Seibyl J, Tamagnan G (2015) Characterization in humans of 18F-MNI-444, a PET radiotracer for brain adenosine 2A receptors. J Nucl Med 56(4):586–591. https://doi.org/10.2967/jnumed.114.152546
Tavares AA, Batis JC, Papin C, Jennings D, Alagille D, Russell DS, Vala C, Lee H, Baldwin RM, Zubal IG, Marek KL, Seibyl JP, Barret O, Tamagnan GD (2013) Kinetic modeling, test-retest, and dosimetry of 123I-MNI-420 in humans. J Nucl Med 54(10):1760–1767. https://doi.org/10.2967/jnumed.113.119933
Stemmer SM, Manojlovic NS, Marinca MV, Petrov P, Cherciu N, Ganea D, Ciuleanu TE, Puscas IA, Beg MS, Purcell WT, Croitoru AE, Ilieva RN, Natošević S, Nita AL, Kalev DN, Harpaz Z, Farbstein M, Silverman MH, Fishman P, Llovet JM (2019) A phase I, randomized, double-blind, placebo-controlled trial evaluating efficacy and safety of namodenoson (CF102), an A3 adenosine receptor agonist (A3AR), as a second-line treatment in patients with Child-Pugh B (CPB) advanced hepatocellular carcinoma (HCC). J Clin Oncol (15_suppl):2503–2503
Bernier LP, Ase AR, Séguéla P (2018) P2X receptor channels in chronic pain pathways. Br J Pharmacol 174:2219–2230
Antonioli L, Blandizzi C, Pacher P, Haskó G (2019) The purinergic system as a pharmacological target for the treatment of immune-mediated inflammatory diseases. Pharmacol Rev 71:345–382
Lara R, Adinolfi E, Harwood CA, Philpott M, Barden JA, Di Virgilio F, McNulty S (2020) P2X7 in cancer: from molecular mechanisms to therapeutics. Front Pharmacol 11:793. https://doi.org/10.3389/fphar.2020.00793
McInnes IB, Cruwys S, Bowers K, Braddock M (2014) Targeting the P2X7 receptor in rheumatoid arthritis: biological rationale for P2X7 antagonism. Clin Exp Rheumatol 32(6):878–882
Keystone EC, Wang MM, Layton M, Hollis S, McInnes IB, D1520C00001 Study Team (2012) Clinical evaluation of the efficacy of the P2X7 purinergic receptor antagonist AZD9056 on the signs and symptoms of rheumatoid arthritis in patients with active disease despite treatment with methotrexate or sulphasalazine. Ann Rheum Dis 71(10):1630–1635
Dittrich HC, Gupta DK, Hack TC, Dowling T, Callahan J, Thomson S (2007) The effect of KW-3902, an adenosine A1 receptor antagonist, on renal function and renal plasma flow in ambulatory patients with heart failure and renal impairment. J Cardiac Fail 13(8):609–617
Ciruela F, Jacobson KA (2019) Editorial: Purinergic pharmacology. Front Pharmacol 10:21
Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G, Gibson CM, Antman EM, TRITON-TIMI 38 Investigators (2007) Prasugrel versus clopidogrel in patients with acute cornary syndromes. N Engl J Med 357(2):2001–2015
Murakami T, Fujihara T, Horibe Y, Nakamura M (2004) Diquafosol elicits increases in net Cl- transport through P2Y2 receptor stimulation in rabbit conjunctiva. Ophthalmic Res 36(2):89–93. https://doi.org/10.1159/000076887
Fujihara T, Murakami T, Fujita H, Nakamura M, Nakata K (2001) Improvement of corneal barrier function by the P2Y2 agonist INS365 in a rat dry eye model. Invest Ophthalmol Vis Sci 42(1):96–100
Keating GM (2015) Diquafosol ophthalmic solution 3 %: a review of its use in dry eye. Drugs 75(8):911–922. https://doi.org/10.1007/s40265-015-0409-7
Cowlen MS, Zhang VZ, Warnock L, Moyer CF, Peterson WM, Yerxa BR (2003) Localization of ocular P2Y2 receptor gene expression by in situ hybridization. Exp Eye Res 77(1):77–84
Shahidullah M, Wilson WS (1997) Mobilization of intracellular calcium by P2Y2 receptors in cultured, non-transformed bovine ciliary epithelial cells. Curr Eye Res 16(10):1006–1016
Cullinane AB, Coca-Prados M, Harvey BJ (2001) Extracellular ATP effects on calcium signaling in cultured human non-pigmented ciliary body epithelium. Curr Eye Res 23(6):448–454
Farahbakhsh NA, Cilluffo MC (2002) P2 purinergic receptor-coupled signaling in the rabbit ciliary body epithelium. Invest Ophthalmol Vis Sci 43(7):2317–2325
Sabater JR, Mao YM, Shaffer C, James MK, O’Riordan TG, Abraham WM (1999) Aerosolization of P2Y(2)-receptor agonists enhances mucociliary clearance in sheep. J Appl Physiol 87(6):2191–2196. https://doi.org/10.1152/jappl.1999.87.6.2191
(2003) Diquafosol: DE 089, diquafosoltetrasodium, INS 365, INS 365 Ophthalmic, INS 365 Respiratory, KPY 998. Drugs R D 4(6):359–362. https://doi.org/10.2165/00126839-200304060-00005
Murakami T, Fujihara T, Nakamura M, Nakata K (2000) P2Y(2) receptor stimulation increases tear fluid secretion in rabbits. Curr Eye Res 21(4):782–787. https://doi.org/10.1076/ceyr.21.4.782.5550
Li Y, Kuang K, Yerxa B, Wen Q, Rosskothen H, Fischbarg J (2001) Rabbit conjunctival epithelium transports fluid, and P2Y2(2) receptor agonists stimulate Cl(-) and fluid secretion. Am J Physiol Cell Physiol 281(2):C595–C602. https://doi.org/10.1152/ajpcell.2001.281.2.C595
Dota A, Sakamoto A, Takashi N, Tadahiro M, Takeshi M (2020) Effect of diquafosol ophthalmic solution on airflow-induced coular surface disorder in diabetic rats. Clin Ophthalmol 14:1019–1024
Inspire Pharmaceuticals. Inspire Pharmaceuticals announces FDA acceptance of diquafosol NDA for filing. Media Release: 9 Sep 2003. http://www.inspirepharm.com. Accessed 04 August 2021
Inspire Pharmaceuticals Inc (2003) Inspire Pharmaceuticals’ diquafosol NDA granted priority review by the FDA media release. http://www.nrpeuro.com. Accessed 21 November 2021
Matsumoto Y, Ohashi Y, Watanabe H, Tsubota K, Diquafosol Ophthalmic Solution Phase 2 Study Group (2012) Efficacy and safety of diquafosol ophthalmic solution in patients with dry eye syndrome: a Japanese phase 2 clinical trial. Ophthalmology 119(10):1954–1960
Yamaguchi M, Nishijima T, Shimazaki J, Takamura E, Yokoi N, Watanabe H, Ohashi Y (2014) Clinical usefulness of diquafosol for real-world dry eye patients: a prospective, open-label, non-interventional, observational study. Adv Ther 31(11):1169–1181
Takamura E, Tsubota K, Watanabe H, Ohashi Y (2012) A randomized, double-masked comparison study of diquafosol versus sodium hyaluronate ophthalmic solutions in dry eye patients. Br J Ophthalmol 96(10):1310–1315
Ohashi Y, Munesue M, Shimazaki J, Takamura E, Yokoi N, Watanabe H, Nomura A, Shimada F (2020) Long-term safety and effectiveness of diquafosol for the treatment of dry eye in a real-world setting: a prospective observational study. Adv Ther 37(2):707–717
Santen (2010) Santen announces approval of DIQUASTM for dry eye treatment in Japan media release. https://www.santen.com/en/news/20100416_2.pdf. Accessed 21 November 2021
Eom Y, Kim HM (2021) Clinical effectiveness of diquafosol ophthalmic solution 3% in Korean patients with dry eye disease: a multicenter prospective observational study. Int J Ophthalmol 14(10):1518. https://doi.org/10.18240/ijo.2021.10.07
Gaarder A, Jonsen J, Laland S, Hellem A, Owren PA (1961) Adenosine diphosphate in red cells as a factor in the adhesiveness of human blood platelets. Nature 192:531–532. https://doi.org/10.1038/192531a0
Hollopeter G, Jantzen HM, Vincent D, Li G, England L, Ramakrishnan V, Yang RB, Nurden P, Nurden A, Julius D, Conley PB (2001) Identification of the platelet ADP receptor targeted by antithrombotic drugs. Nature 409(6817):202–207. https://doi.org/10.1038/35051599
Sugidachi A, Asai F, Ogawa T, Inoue T, Koike H (2000) The in vivo pharmacological profile of CS-747, a novel antiplatelet agent with platelet ADP receptor antagonist properties. Br J Pharmacol 129(7):1439–1446. https://doi.org/10.1038/sj.bjp.0703237
Sugidachi A, Asai F, Yoneda K, Iwamura R, Ogawa T, Otsuguro K, Koike H (2001) Antiplatelet action of R-99224, an active metabolite of a novel thienopyridine-type G(i)-linked P2T antagonist, CS-747. Br J Pharmacol 132(1):47–54. https://doi.org/10.1038/sj.bjp.0703761
Mega JL, Close SL, Wiviott SD, Shen L, Walker JR, Simon T, Antman EM, Braunwald E, Sabatine MS (2010) Genetic variants in ABCB1 and CYP2C19 and cardiovascular outcomes after treatment with clopidogrel and prasugrel in the TRITON-TIMI 38 trial: a pharmacogenetic analysis. Lancet 376(9749):1312–1319. https://doi.org/10.1016/S0140-6736(10)61273-1
Jakubowski JA, Winters KJ, Naganuma H, Wallentin L (2007) Prasugrel: a novel thienopyridine antiplatelet agent. A review of preclinical and clinical studies and the mechanistic basis for its distinct antiplatelet profile. Cardiovasc Drug Rev 25(4):357–374
Shan J, Sun H (2013) The discovery and development of prasugrel. Expert Opin Drug Discov 8(7):897–905. https://doi.org/10.1517/17460441.2013.793668
Calogiuri GF, Al-Sowaidi S, Nettis E, Cortellini G, Macchia L, Vacca A, Kounis NG (2016) A joint allergist/cardiologist classification for thienopyridines hypersensitivity reactions based on their symptomatic patterns and its impact on the management strategies. Int J Cardiol 222:509–514
Schilling U, Dingemanse J, Ufer M (2020) Pharmacokinetics and pharmacodynamics of approved and investigational P2Y12 receptor antagonists. Clin Pharmacokinet 59(5):545–566. https://doi.org/10.1007/s40262-020-00864-4
Goodwin MM, Desilets AR, Willett KC (2011) Thienopyridines in acute coronary syndrome. Ann Pharmacother 45(2):207–217. https://doi.org/10.1345/aph.1P319
Angiolillo DJ, Fernandez-Ortiz A, Bernardo E, Alfonso F, Macaya C, Bass TA, Costa MA (2007) Variability in individual responsiveness to clopidogrel: clinical implications, management, and future perspectives. J Am Coll Cardiol 49(14):1505–1516
Mega JL, Close SL, Wiviott SD, Shen L, Hockett RD, Brandt JT, Walker JR, Antman EM, Macias W, Braunwald E, Sabatine MS (2009) Cytochrome p-450 polymorphisms and response to clopidogrel. N Engl J Med 360(4):354–362. https://doi.org/10.1056/NEJMoa0809171
Gurbel PA, Tantry US (2007) Clopidogrel resistance? Thromb Res 120(3):311–321
Sugidachi A, Ogawa T, Kurihara A, Hagihara K, Jakubowski JA, Hashimoto M, Niitsu Y, Asai F (2007) The greater in vivo antiplatelet effects of prasugrel as compared to clopidogrel reflect more efficient generation of its active metabolite with similar antiplatelet activity to that of clopidogrel’s active metabolite. J Thromb Haemost 5(7):1545–1551. https://doi.org/10.1111/j.1538-7836.2007.02598.x
Niitsu Y, Sugidachi A, Ogawa T, Jakubowski JA, Hashimoto M, Isobe T, Otsuguro K, Asai F (2008) Repeat oral dosing of prasugrel, a novel P2Y12 receptor inhibitor, results in cumulative and potent antiplatelet and antithrombotic activity in several animal species. Eur J Pharmacol 579(1–3):276–282. https://doi.org/10.1016/j.ejphar.2007.10.005
Wiviott SD, Antman EM, Winters KJ, Weerakkody G, Murphy SA, Behounek BD, Carney RJ, Lazzam C, McKay RG, McCabe CH, Braunwald E, JUMBO-TIMI 26 Investigators (2005) Randomized comparison of prasugrel (CS-747, LY640315), a novel thienopyridine P2Y12 antagonist, with clopidogrel in percutaneous coronary intervention. Circulation 111(25):3366–3373
Wiviott SD, Braunwald E, McCabe CH, Motalescot G, Ruzyllo W, Gottlieb S, Neumann FJ, Ardissino D, De Servi S, Murphy SA, Riesmeyer J, Weerakkody G et al (2007) Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 357:2001–2015
FDA U.S. Food & Drug Administration (2022) Drugs@FDA: FDA-Approved Drugs. https://Accessdata.fda.gov. Accessed 21 November 2021
Roe MT, Armstrong PW, Fox KA, White HD, Prabhakaran D, Goodman SG, Cornel JH, Bhatt DL, Clemmensen P, Martinez F, Ardissino D, Nicolau JC, Boden WE, Gurbel PA, Ruzyllo W, Dalby AJ, McGuire DK, Leiva-Pons JL, Parkhomenko A, Gottlieb S et al (2012) Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med 367(14):1297–1309
FDA US Food & Drug Administration (2022) Effient (prasugrel) tablets label. https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022307s002lbl.pdf. Accessed 22 November 2021
Yan AT, Roe MT, Neely M, Cyr DD, White H, Fox K, Prabhakaran D, Armstrong PW, Ohman EM, Goodman SG (2018) Early discontinuation of prasugrel or clopidogrel in acute coronary syndromes: insights from the TRILOGY ACS trial. Coron Artery Dis 29(6):469–476. https://doi.org/10.1097/MCA.0000000000000623
Lordkipanidzé M, Marquis-Gravel G, Tanguay JF, Mehta SR, So D (2020) Implications of the antiplatelet therapy gap left with discontinuation of prasugrel in Canada. CJC Open 3(6):814–821. https://doi.org/10.1016/j.cjco.2020.11.021
Pharmac Te Pataka whaioranga (2021) Prasugrel: discontinued media release. https://pharmac.govt.nz/medicine-funding-and-supply/medicine-notices/prasugrel/#:~:text=About%20this%20discontinuation&text=Prasugrel%20is%20an%20antiplatelet%20medicine,delisted%20on%2031%20January%202021. Accessed 09 January 2022
De Luca L, Steg PG, Bhatt DL, Capodanno D, Angiolillo DJ (2021) Cangrelor: clinical data, contemporary use, and future perspectives. J Am Heart Assoc 10(13):e022125. https://doi.org/10.1161/JAHA.121.022125
Angiolillo DJ, Firstenberg MS, Price MJ, Tummala PE, Hutyra M, Welsby IJ, Voeltz MD, Chandna H, Ramaiah C, Brtko M, Cannon L, Dyke C, Liu T, Montalescot G, Manoukian SV, Prats J, Topol EJ, BRIDGE Investigators (2012) Bridging antiplatelet therapy with cangrelor in patients undergoing cardiac surgery: a randomized controlled trial. JAMA 307(3):265–274
Harrington RA, Stone GW, McNulty S, White HD, Lincoff AM, Gibson CM, Pollack CV Jr, Montalescot G, Mahaffey KW, Kleiman NS, Goodman S, Amine M, Angiolillo DJ, Becker RC, Chew DP, French WJ, Leisch F, Parikh KH, Skerjanec S, Bhatt DL (2009) Platelet inhibition with cangrelor in patients undergoing PCI. N Engl J Med 361(24):2318–2329
Bhatt DL, Stone GW, Mahaffey KW, Gibson CM, Steg PG, Hamm CW, Price MJ, Leonardi S, Gallup D, Bramucci E, Radke PW, Widimský P, Tousek F, Tauth J, Spriggs D, McLaurin BT, Angiolillo DJ, Généreux P, Liu T, Prats J et al (2013) Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med 368(14):1303–1313
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions S Han has been supported by the University of Auckland doctoral scholarship, Auckland, New Zealand and a Ph.D. scholarship grant from the Eisdell Moore Centre, University of Auckland, Auckland, New Zealand. H Suzuki-Kerr has been supported by project grants (Project number: 3726420) from the Auckland Medical Research Foundation, Auckland, New Zealand and the Eisdell Moore Centre.
Author information
Authors and Affiliations
Contributions
All authors contributed to this review and idea development. Seunga Han performed the literature search, data analysis and drafted the work. Haruna Suzuki-Kerr, Srdjan M Vlajkovic and Peter R Thorne critically revised this review.
Corresponding author
Ethics declarations
Conflicts of interest
S. Han declares that she has no conflict of interest.
H. Suzuki-Kerr declares that he/she has no conflict of interest.
S. M. Vlajkovic declares that he/she has no conflict of interest.
P. R. Thorne declares that he/she has no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Han, S., Suzuki-Kerr, H., Vlajkovic, S.M. et al. The developmental journey of therapies targeting purine receptors: from basic science to clinical trials. Purinergic Signalling 18, 435–450 (2022). https://doi.org/10.1007/s11302-022-09896-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-022-09896-w