Abstract
The P2X7 purinoceptor is unique amongst the P2X receptor family in that its activation is able to stimulate the release of mature, biologically active interleukin-1β (IL-1β), as well as a variety of other proinflammatory cytokines. Coupled with the predominate localisation of this receptor to immunocytes of haemopoetic origin, this receptor is an obvious candidate to play a major and pivotal role in processes of pain and inflammation. Using genetically modified animals that lack the P2X7 receptor, several investigators have shown that these mice do indeed demonstrate a blunted inflammatory response, and fail to develop pain following both inflammatory and neuropathic insult. These animals also show altered cytokine production in response to inflammatory stimulus, which is far broader than merely modulation of IL-1β release. In this short article, we review the role of the P2X7 receptor in modulating the release of cytokines and other mediators, and discuss the findings made from P2X7 receptor-deficient animals. As well as highlighting outstanding questions regarding this intriguing receptor, we also speculate as to the potential therapeutic benefit of P2X7 receptor modulation.
Similar content being viewed by others
Introduction
The P2X7 receptor is an unusual member of the P2X receptor superfamily. Like the other channels, P2X7 is an ATP-gated non-selective cation channel, but this receptor differs from the other members in several important ways. First, the C-terminal domain of the P2X7 receptor is some 200 amino acids longer than the other members, a feature that has been hypothesised to confer some of the unusual functional properties of this receptor. Secondly, the P2X7 receptor can function as a bifunctional receptor, which, depending on receptor expression and duration and intensity of stimulation (Chessell et al. [1]), appears either as a non-selective cation channel, or as a large, non-selective pore with permeability to molecules of molecular mass up to −?00 Da. Uniquely in this receptor family, activation of P2X7 can also activate caspase 1, which causes rapid release of mature, biologically active interleukin-1β (IL-1β (Colomar et al. [2]). Whilst the P2X7 receptor was initially thought to be localised only to cells of the immune system (Collo et al. [3]), more recent studies suggest a more diverse distribution (e.g., Narcisse et al. [4]; Zhang et al. [5]), although some doubts have been raised regarding the specificity of the tools sometimes used to establish this localisation (Sim et al. [6]).
Given the localisation and properties of the P2X7 receptor, it is perhaps not surprising that recent data suggests a pivotal role in initiating or maintaining an inflammatory response. Whether wholly dependent on this or mediated by other P2X7 mediated transductional events, this receptor also appears to play a pivotal role in the induction or maintenance of both neuropathic and inflammatory pain. Here we review these data, and speculate as to the potential therapeutic indications that P2X7 receptor antagonists may address.
The P2X7 receptor as a regulator of inflammatory mediators
As above, P2X7 receptors are found predominantly expressed in cells of hemopoietic lineage, including monocytes, macrophages and lymphocytes. Upon appropriate activation, this receptor is reported to regulate a variety of pro-inflammatory cellular signalling events and has been proposed to serve as a regulator of inflammation based on its ability to initiate post-translational processing of leaderless cytokines such as IL-1β and IL-18 (Hogquist et al. [7]; Sanz et al. [8]). At present it is not completely clear whether these events depend on the ‘large pore’form of the receptor, but there is some data to suggest that very brief activation of the receptor is sufficient to initiate cytokine release (Chessell et al. [9]). Upon inflammatory insult, immune cells generate large quantities of pro-IL-1β but very little mature biologically active cytokine is released from the activated cells. Perregaux and Gabel [10] were the first to demonstrate that ATP potentiates the post-translational processing and release of IL-1β from lipopolysacharide (LPS) primed cells. Since then many studies, both in vitro and in vivo, have demonstrated the requirement of exogenous ATP to produce large quantities of active IL-1β and the subsequent impact of this on the inflammatory response (Griffiths et al. [11]; Solle et al. [12]). However, the absence of suitable selective pharmacological tools has hampered full elucidation of the role P2X7 plays in this process. Thus, we and others have generated P2X7 -deficient mice to demonstrate that absence of the receptor leads to loss of ATP-dependent immune functions (Chessell et al. [1]; Labasi et al. [13]).
Solle and colleagues were the first to report that in vivo administration of ATP to LPS primed P2X7 receptor −?−?mice failed to generate significant levels of IL-1β release from peritoneal macrophages (Solle et al. [12]). In contrast, wild-type littermates showed a 10-fold increase in biologically active IL-1β levels. The release of IL-1β is thought to initiate a signalling cascade leading to the up-regulation of various other inflammatory mediators such as cyclo-oxygenase-2 (COX-2), IL-6 and tumour necrosis factor α (TNFα). Importantly, this group went on to demonstrate that IL-6 production was also greatly reduced (3-fold reduction) in the P2X7 −?−?mice following exposure to LPS and ATP, suggesting that blockade of IL-1β release could impair cytokine signalling cascades in vivo. This work was further supported by Labasi et al. [13]. Here, blood samples from P2X7 −?−?mouse and wild-type controls underwent challenge with either ATP or the P2X agonist, Bz-ATP, following LPS treatment in vitro. Results similar to those above were obtained with P2X7 −?−?mice showing an absence of IL-1β release compared to wild-type controls.
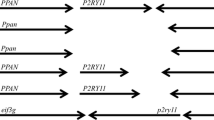
LPS-induced IL-1β release was also examined in thioglycollate-elicited macrophages from both P2X7 −?−?and control animals (Chessell et al. [1]). Six hours following stimulation with LPS, cultures were stimulated with Bz-ATP and 30 min later IL-1β was measured in cell supernatants. No significant release of IL-1β was detected using cells from the P2X7 −?−?animals whilst IL-1β levels peaked at 700 pg/ml in the control cells following LPS and BzATP treatment (Fig. 1).
Mature interleukin-1β (IL-1β) release from thioglycolate-elicited peritoneal macrophages obtained from P2X7 −?−?and control mice. Addition of agonist, Bz-ATP, caused a dose-dependent release of IL-1β from control animals, LPS-primed cells measured 30 min following agonist addition, but not from LPS-primed cells from P2X7 −?−?animals or non-primed cells from control or P2X7 −?−?animals (adapted from Chessell et al. [1])
To further elucidate the effect of P2X7 loss on the global inflammatory response, we profiled local and systemic cytokine levels in P2X7 −?−?and P2X7 +/+ animals 0, 1 and 7 days post intraplantar Freund’s complete adjuvant (FCA) challenge. Profiling of P2X7 +/+ paw samples revealed a sustained increase for all cytokines tested (IL-10, IL-1β, IL-6, MCP-1, TNF-α), with only the increases in IL-1β and IL-10 being significantly attenuated in the P2X7 −?−?animals across the whole timecourse, indicating that the effect of P2X7 receptor ligation on down-regulation of cytokine levels local to insult may be quite selective (Table 1). In contrast, the IL-6 response was enhanced in P2X7 −?−?animals, suggesting potential compensatory changes.
These data indicate that P2X7 −?−?animals demonstrate an attenuated cytokine response to FCA challenge. Although the release of IL-1β from P2X7 −?−?paws is significantly reduced at both 1 and 7 days post-FCA-injection as compared to control animals, there was no deficit in IL-1β mRNA expression in the P2X7 −?−?paws over the time-course studied, indicating normal transcriptional regulation of pro-IL-1β in these animals (Fig. 2). As such, the P2X7 −?−?animals appear to have a normal immune capability at the transcriptional level but they possess a deficiency in their ability to process pro-IL-1β in response to an inflammatory stimulus. This correlates with the observation that the P2X7 −?−?animals possess normal nociceptive processing but lack the ability to develop inflammation induced hypersensitivity. A potential mechanism of action may be proposed whereby deletion of P2X7 in vivo is sufficient to block processing of mature IL-1β and as a consequence block initiation or maintenance of pathological changes in response to inflammatory insults. This proposal is further strengthened by the observation that systemic inflammation following FCA challenge is abolished in P2X7 −?−?animals.
Released IL-1β and IL-1β mRNA expression levels for in paw samples from P2X7−?−?and P2X7+/+ animals. a No deficit in IL-1β mRNA expression seen in the P2X7−?−?paws over the time-course studied. b Release of IL-1β from P2X7−?−?paws is significantly reduced at both 1 and 7 days post-FCA-injection as compared to control animals. Data are expressed as mean values ±SEM. *P–lt;–.05, **P–lt;–.01, ***P–lt;–.001 significantly different from WT values, Student’s unpaired t-test
This study also demonstrated that the levels of cell-free IL-10 are significantly reduced in P2X7 −?−?animals as compared to WT across the time course. The reason for the decrease in an ‘anti-inflammatory–cytokine in the P2X7 −?−?animals is not yet clear. However, studies in macrophages derived from IL-10-deficient animals demonstrate higher levels of TNF-α production upon activation (Gazzinelli et al. [14]) indicating an inverse relationship. This is further supported in the present study, where a transient increase in levels of TNF-α in the paw samples was also observed in the P2X7 −?−?animals (correlating with a transient increase in TNF-α gene expression over the time course), indicative of a synergy between P2X7, IL-1β, IL-10 and TNF-α. It also raises the interesting possibility that P2X7 may act directly upon IL-10, as seen with IL-1β and IL-18 (Mehta et al. [15]). These observations have been extended by Fulgenzi et al. [16] who demonstrated reduced IL-10, MCP-1 and IL-8 levels in inflamed vessels following FCA injection into rat paw following local use of periodate oxidised ATP (oATP). These pro-inflammatory chemokines mediate recruitment of neutrophils, T-cells and monocytes/macrophages into the inflamed tissues and this data once again may link P2X7 activation to the inflammatory process. However, it should be noted that while oATP is considered an effective antagonist of P2X7, it has been reported that currents at P2X1 and P2X2 receptors are also affected (Humphreys et al. [17]). The hypothesis that P2X7 may directly modulate IL-10 and TNF-α as well as IL-1β is supported by studies on human P2X7 receptor polymorphisms. These investigations have revealed a polymorphism-dependent modulation of LPS-induced TNF-α and IL-10 levels in human blood (Denlinger et al. [18]). Blood samples from individuals with a reduced capacity for monocyte P2X7 ‘large pore–formation produced lower levels of TNF-α as compared to the high pore activity group following stimulation of the samples with LPS for 6 or 24 h (cytokine levels assessed by ELISA). This coincided with higher levels of IL-10 in the low ‘pore–group and no difference in IL-1β. Although these changes are different to those observed in P2X7 −?−?animals following FCA injection, it is now important to try and elucidate fully the mechanism whereby P2X7 channel activity and/or large pore formation ability affects LPS-induced IL-10 and TNF-α production, as has been examined for IL-1β. Importantly, regardless of mechanism, these data suggest that in the future, relative levels of specific cytokines in the blood may serve as a surrogate marker to predict predisposition to inflammatory diseases.
More recently, the signalling events involved in post-translational processing and release of IL-1β from cells following P2X7 activation have been investigated. IL-1β and IL-18 are inactive until cleaved by caspase-1. ATP-stimulation of P2X7 results in the rapid activation of caspase-1 in macrophages and the release of mature, biologically active, IL-1β into the culture medium within 15 min (Mackenzie et al. [19]; Kahlenberg et al. [20]). It has now been demonstrated that P2X7 receptor activation of caspase-1 is dependent on the pre-stimulation of macrophages with microbially derived ligands for Toll-like receptors (TLR2/4/9) such as LPS and is dependent on de novo protein synthesis (cyclohexamide blocks the ability of LPS to prime cells for P2X7-dependent caspase-1 activation) via the NF-kB pathway (Kahlenberg et al. [21]). To date the proteins that facilitate efficient coupling of caspase-1 activation to P2X7 stimulation are unclear but their identification may provide interesting alternative therapeutic targets for inflammatory diseases. One molecule that may be involved in controlling P2X7 activity is regeneration and tolerance factor (RTF; Derks and Beaman [22]). RTF is the alpha-2 isoform of the alpha subunit of the vacuolar ATPase proposed to regulate activity of the ATPase complex. RTF is expressed on the surface of activated lymphocytes, constitutively expressed on macrophages and is thought to regulate both IL-10 secretion (Lee et al. [23]) and apoptosis (Boomer et al. [24]). Anti-RTF antibodies enhance ATP-stimulated IL-1β secretion from macrophages, block surface ATPase activity and permeability of the cell to PI. These results suggest that RTF may modulate IL-1β secretion from immune cells by controlling activation of P2X7. Additional studies have demonstrated a role for P2X7 in immune cell apoptosis. Bulanova et al. [25] have shown that addition of extracellular ATP in the millimolar range induced activation of P2X7 expressed on murine mast cells, resulting in the rapid but transient phosphorylation of ERK, Jak2 and STAT6. In addition, ATP stimulation increased expression levels of IL-4, IL-6, IL-13 and TNF-α and these effects could be blocked by pre-treatment of the cells with oATP or KN-62 (a selective blocker of human and mouse P2X7).
Taken together, the data reviewed here indicates that P2X7 plays a critical role in the development of inflammation via modulation of inflammatory mediator production. As such, drugs that block P2X7 directly, or interact with proteins that modulate P2X7 activity, may have the potential to treat a broad range of inflammatory diseases, including pain associated with inflammation.
The role of P2X7 in pain and inflammation in vivo studies
The in vivo investigation of the role of P2X7 in inflammation has been hampered by a lack of selective compounds acting at this receptor (see Baraldi et al. [26]). However, some work has been published reporting effects of oATP in rats treated with FCA (Dell’Antonio et al. [27, 28]). FCA causes a long-lasting hyperalgesia, demonstrated by a reduction in paw withdrawal thresholds. Injection of oATP into the treated paw significantly reversed this hyperalgesia, indicating a putative role for the P2X7 receptor. However, oATP is known to have actions at receptors other than P2X7, so it is not possible to unequivocally link the action of oATP with P2X7 inhibition in these studies. Given the lack of selective compounds, the development of the P2X7 receptor knockout mouse (P2X7 −?−? has allowed for the investigation of the role played by this receptor in inflammation using in vivo animal models. To date, three reports of such work have appeared.
As mentioned previously, the first study (Solle et al. [12]) reported that the administration of ATP to LPS primed P2X7 receptor −?−?mice failed to generate significant levels of mature IL-1β following peritoneal lavage as compared to the wild-type littermates. No further in vivo data was reported, with the exception of the fact that the P2X7 −?−?mice appeared to be healthy and fertile. Labasi et al. [13] also demonstrated that ATP/BzATP stimulation of LPS-primed blood samples from P2X7 −?−?mice in vitro resulted in markedly less IL-1β release as compared to wild-type controls. These authors went on to examine the response of the P2X7 −?−?mouse in a monoclonal antibody (mAb)-induced arthritis model. Here mAbs against collagen were injected into the mice, which were then injected with LPS. Following this, wild-type mice developed a severe arthritic phenotype, which was assessed using a scoring system for arthritis outcome measures. Under this system each limb was graded and given a score of 1–. Mean maximum severity was then calculated. In these studies, mean maximum severity scores of 7 were obtained in wild-type mice. However, the maximum mean score observed in P2X7 −?−?mice was significantly less (<3). Investigations of cartilage structural integrity were also carried out. This showed that whilst in the wild-type mice all joints subjected to mAb-induced arthritis were affected, the P2X7 −?−?mice showed a much lower incidence of pathology.
The behavioural phenotype of the P2X7 −?−?mouse was investigated further by Chessell et al. [1]. In this latter paper, IL-1β levels were examined following the administration of Bz-ATP to LPS primed plated cell cultures, as discussed above. The effect of P2X7 deletion on the behavioural phenotype of the mice was demonstrated in models of both inflammatory and neuropathic pain. In the first model, P2X7 −?−?mice along with wild-type littermate controls were treated with intraplantar FCA and assessed for changes in mechanical hypersensitivity using a weight-bearing averager. Whilst wild-type mice showed a long lasting hypersensitivity when compared to baseline readings, no difference was observed in P2X7 −?−?mice, indicating a lack of inflammatory response. In the model of neuropathic pain, mice underwent surgery to partially ligate the sciatic nerve (Seltzer et al. [29]). Again a significant level of hyperalgesia was observed in wild-type mice to both a thermal and a mechanical stimulus, whilst no significant changes were seen in the P2X7 −?−?mice. Whilst, in the light of the altered cytokine production in the knockout animals, the lack of development of pain in the inflammatory model is perhaps not surprising, the phenotypic differences in the neuropathic pain model were more unexpected. Whether this phenotype is also resultant on altered cytokine production, or some other alteration in signalling is not known. However, in some neuropathic pain models, the initial development of the pain is driven by an inflammatory neuritis around the injured nerve, so it could be hypothesised that the lack of development of pain in the neuropathy model is again a direct result of an impaired inflammatory response in the knockout animals.
Taken together, these data indicate that the P2X7 receptor does appear to play a pivotal role in the development, or maintenance, of pain associated with both inflammation, and nerve injury. The use of selective antagonist tools, which are now becoming available (Alcarez et al. [30]), will help to elucidate the temporal role of P2X7 in these disease models, as well as answering any issues regarding the potential for compensatory changes in knockout animals.
Discussion
The unique properties of the P2X7 receptor, in terms of its role in mediating the release of biologically active cytokines, and also its localisation to cells of haemopoetic origin, makes this receptor an obvious candidate to play a pivotal role in the inflammatory process. Given that many inflammatory mediators, including the cytokines, IL-1β and TNF-α, are able to directly sensitise, or activate, sensory afferents, it is perhaps no surprise that this receptor also appears to play a key role in the induction or maintenance of pain of both inflammatory and neuropathic origin (Chessell et al. [1]).
Whilst intensive research efforts are beginning to address the mechanisms by which the P2X7 receptor mediates some of its effects, many questions remain unanswered. The exact mechanisms by which the P2X7 receptor undergoes transformation from a conventional ion channel to the large pore form remain elusive, although it is hypothesised that the pore and channel are separate entities (Schilling et al. [31]), or that there exists both an intrinsic and extrinsic large pore that is activated by P2X7 (Jiang et al. [32]). Nonetheless, it is clear that this transition from channel to pore is not necessarily an absolute requirement for the release of mature IL-1β (Chessell et al. [1]), although the events required for the release of TNF-α and IL-10 are less clear. The actions of the increasing number of cytokines whose release is modulated by the P2X7 receptor are better understood; in most cases these cytokines are potent sensitisers or activators of sensory nerve terminals (and thus contribute to the generation of pain signalling), and most also induce expression of further downstream inflammatory mediators, or enzyme capable of producing them (e.g., nitric oxide synthase, cyclooxygenase-2, superoxide products, nerve growth factor; Woolf et al. [33, 34]; Samad et al. [35]; Parvathenani et al. [36]). Interestingly, some studies have also demonstrated that release of the ‘anti-inflammatory–cytokine, IL-10, is impaired in P2X7−?−?animals (Chessell et al. [1]), which may either be resultant in changes in concentrations of TNF-α, or perhaps modulated more directly via the P2X7 receptor.
The phenotypic effects of knockout of the P2X7 receptor seem to be clear animals do not develop behaviourally measurable pain following either inflammatory or neuropathic insult (Chessell et al. [1]), and the incidence and severity of disease in a model of rheumatoid arthritis is significantly attenuated (Labasi et al. [13]). Both of these findings are startling and unusual; there are very few studies describing the abolition of pain in any other receptor knockout animals, and such reduction of incidence and severity of arthritis without general immunocompromisation is also unusual. However, in both of these studies, it could not be established, for obvious reasons, whether the pivotal role of the P2X7 receptor was in the induction or the maintenance of the pathophysiology associated with these experimental insults, or perhaps both. It is also important to bear in mind possible compensatory mechanisms in continuous knockout animals, which may have a bearing on the resultant phenotype. The temporal relationship between activation/inhibition of the P2X7 receptor, and development or maintenance of inflammation and pain could be addressed using inducible knockout systems, or perhaps more readily with selective antagonist molecules. It is anticipated that these questions will be addressed over the next few years using either of these approaches.
The lack of development of neuropathic hypersensitivity in the P2X7 −?−?animals was perhaps a little more surprising, as neuropathic pain is not dogmatically associated with overt tissue inflammation, and the role of inflammatory mediators in this pain state is less well established. However, several studies hypothesise or demonstrate the role of proinflammatory cytokines in the induction and maintenance of neuropathic pain (see Lindenlaub and Sommer [37]). Thus, axonal injury does result in proliferation of inflammatory mediators (see Holden and Pizzi [38]), which include those associated with P2X7 receptor activation. Taken together with the demonstration that the P2X7 receptor has also been shown to be upregulated in tissues from chronic neuropathic pain sufferers, the role of this receptor in this disease state does become more tenable.
The data reviewed in this manuscript suggest that the P2X7 receptor could be an important upstream regulator of the inflammatory and pain cascades. Identification and modulation of such upstream processes for therapeutic intervention has proved to be challenging; in some cases discovery of suitable molecular tools has proved to be intractable (e.g., small molecule IL-1β antagonists), and in others the pleiotropic effects of modulating the upstream regulatory machinery has limited the therapeutic benefits in the clinic (e.g., p38 MAP kinase inhibitors). The ability to truly modulate both inflammatory and neuropathic pain, as well as inflammation itself, with small molecule P2X7 antagonists remains to be proven, but data so far suggest a promising future for this receptor in the treatment of diseases as diverse as Alzheimer’s disease and inflammatory bowel disease.
References
Chessell IP, Hatcher JP, Bountra C, Michel AD, Hughes JP, Green P, Egerton J, Murfin M, Richardson J, Peck WL, Grahames CBA, Casula MA, Yiangou Y, Birch R, Anand P, Buell GN (2005) Disruption of P2X7 purinoceptor gene abolishes chronic inflammatory and neuropathic pain. Pain 114:386–96
Colomar A, Marty V, Médina C, Combe C, Parnet P, Amédée T (2003) Maturation and release of interleukin-1b by lipopolysaccharide-primed mouse Schwann cells require the stimulation of P2X7 receptors. J Biol Chem 278:30732–0740
Collo G, Neidhart S, Kawashima E, Kosco-Vilbois M, North RA, Buell G (1997) Tissue distribution of the P2X7 receptor. Neuropharmacology 36:1277–283
Narcisse L, Scemes E, Zhao Y, Lee SC, Brosnan CF (2005) The cytokine IL-1b transiently enhances P2X7 receptor expression and function in human astrocytes. Glia 49:245–58
Zhang X, Han P, Faltynek CR, Jarvis MF, Shieh C (2005) Functional expression of P2X7 receptors in non-neuronal cells of rat dorsal root ganglia. Brain Res 1052:63–0
Sim JA, Young MT, Sung H-Y, North RA, Surprenant A (2004) Reanalysis of P2X7 receptor expression in rodent brain. J Neurosci 24:6307–314
Hogquist KA, Nett MA, Unanue ER, Chaplin DD (1991) Interleukin 1 is processed and released during apoptosis. Proc Natl Acad Sci USA 88:8485–489
Sanz JM, Di Virgilio F (2000) Kinetics and mechanism of ATP-dependent Il-1beta release form microglial cells. J Immunol 164:4893–898
Chessell IP, Grahames CBA, Michel AD, Humphrey PPA (2001) Dynamics of P2X7 receptor pore dilation: pharmacological and functional consequences. Drug Dev Res 53:60–5
Perregaux D, Gabel CA (1994) Interleukin 1beta maturation and release in response to ATP and nigericin: evidence that potassium depletion mediated by these agents is a necessary and common feature of their activity. J Biol Chem 269:15195–5203
Griffiths RJ, Stam EJ, Downes JT, Otterness IG (1995) ATP induces the release of IL-1 from LPS-primed cells in vivo. J Immunol 154:2821–828
Solle M, Labasi J, Perregaux DG, Stam E, Petrushova N, Koller BH, Griffiths RJ, Gabel CA (2001) Altered cytokine production in mice lacking P2X7 receptors. J Biol Chem 276:125–32
Labasi JM, Petrushova N, Donovan C, McCurdy S, Lira P, Payette MM, Brissette W, Wicks JR, Audoly L, Gabel CA (2002) Absence of the P2X7 receptor alters leukocyte function and attenuates an inflammatory response. J Immunol 168:6436–445
Gazinelli RT, Wysocka M, Hieny S, Scharton-Kersten T, Cheever A, Kuhn R, Muller W, Trinchieri G, Sher A (1996) In the absence of endogenous IL-10, mice acutely infected with Toxoplasma gondii succumb to a lethal immune response dependent on CD4+ T cells and accompanied by overproduction of IL-12, IFN-gamma and TNF-alpha. J Immunol 157:798–05
Mehta VB, Hart J, Wewers MD (2001) ATP-stimulated release of interleukin-1 beta and IL-18 requires priming by lipopolysaccharide and is independent of caspase-1 cleavage. J Biol Chem 276:3820–826
Fulgenzi A, Dell’Antonio G, Foglieni C, Cin ED, Ticozzi P, Franzone JS, Ferrero ME (2005) Inhibition of chemokine expression in rat inflamed paws by systemic use of the antihyperalgesic oxidized ATP. BMC Immunology 6:18
Humphreys BD, Rice J, Kertsey SB, Dubyak GR (2000) Stress-activated protein kinase/JNK activation and apoptopic induction by the macrophage P2X7 nucleotide receptor. J Biol Chem 275:26792–6798
Denlinger LC, Angelini G, Schell K, Green DN, Guadarrama AG, Prabhu U, Coursin DB, Berties PJ, Hogan K (2005) Detection of human P2X7 nucleotide receptor polymorphisms by a novel monocyte pore assay predictive of alterations in lipopolysaccharide-induced cytokine content. J Immunol 174:4424–431
MacKenzie A, Wilson HL, Kiss-Toth E, Dower SK, North RA, Surprenant A (2001) Rapid secretion of IL-1beta by microvesicle shedding. Immunity 15:825–35
Kahlenberg JM, Dubyak GR (2004) Mechanisms of caspase-1 activation by P2X7receptor-mediated K+ release. Am J Physiol 286:C1100–108
Kahlenberg JM, Lundberg KC, Kertesy SB, Qu Y, Dubyak GR (2005) Potentiation of caspase-1 activation by the P2X7 receptor is dependent on TLR signals and requires NF-kB-driven protein synthesis. J Immunol 175:7611–622
Derks R, Beaman K (2004) Regeneration and tolerance factor modulates the effect of adenosine triphosphate-induced interleukin 1beta secretion in human macrophages. Human Immunol 65:676–82
Lee GW, Boomer JS, Gilman-Sachs A, Chedid A, Gudelj L, Rukavina D, Beaman KD (2001) Regeneration and tolerance factor of the human placenta induces IL-10 production. Eur J Immunol 31:687–91
Boomer JS, Derks RA, Lee GW, DuChateau BK, Gilman-Sachs A, Beaman KD (2001) Regeneration and tolerance factor is expressed during T-lymphocyte activation and plays a role in apoptosis. Hum Immunol 62:577–88
Bulanova E, Budagian V, Orinska Z, Hein M, Petersen F, Thon L, Adam D, Bulfone-Paus S (2005) Extracellular ATP induces cytokine expression and apoptosis through P2X7 receptor in murine mast cells. J Immunol 174:3880–890
Baraldi PG, Di Virgilio F, Romagnoli R (2004) Agonists and antagonists acting at P2X7 receptor. Curr Top Med Chem 4:1707–717
Dell’Antonio G, Quattrini A, Dal Cin E, Fulgenzi A, Ferrero ME (2002a) Antinociceptive effects of a new P2Z/ P2X7 antagonist, oxidised ATP, in arthritic rats. Neurosci Lett 327:87–0
Dell’Antonio G, Quattrini A, Dal Cin E, Fulgenzi A, Ferrero ME (2002b) Relief of inflammatory pain in rats by local use ofthe selective P2X7 ATP receptor inhibitor, oxidised ATP. Arthritis Rheum 46:3378–385
Seltzer Z, Dubner R, Shir Y (2000) A novel behavioural model of neuropathic pain disorders produced in rats by partial sciatic nerve injury. Pain 43:205–18
Alcarez L, Baxter A, Bent J, Bowers K, Braddock M, Cladingboel D, Donald D, Fagura M, Furber M, Laurent C, Lawson M, Martimore M, McCormick M, Roberts N, Robertson M (2004) Novel P2X7 receptor antagonists. Bioorg Med Chem Lett 13:4043–046
Schilling WP, Waylyna T, Dubyak GR, Humphreys BD, Sinkins WG (1999) Maitotoxin and P2Z/P2X7 puringeric receptor stimulation activate a common cytolytic pore. Am J Physiol 277:C766–C776
Jiang LH, Rassendren F, MacKenzie A, Zhang Y-H, Surprenant A, North RA (2005) N-methyl-d-glucamine and propridium dyes utilize different permeation pathways at rat P2X7 receptors. Am J Physiol 2005:C1295–C1302
Woolf CJ, Allchorne A, Safieh-Garabedian B, Poole S (1997) Cytokines, nerve growth factor and inflammatory hyperlagesia: the contribution of tumour necrosis factor α. Br J Pharmacol 121:417–24
Woolf CJ, Ma Q, Allchorne A, Poole S (1996) Peripheral cell types contributing to the hyperalgesic action of nerve growth factor in inflammation. J Neurosci 16:2716–723
Samad TA, Moore KA, Sapirstein A, Billet S, Allchorne A, Poole S, Bonventre JV, Woolf CJ (2001) Interleukin-1b-mediated induction of Cox-2 in the CNS contributes to inflammatory pain hypersensitivity. Nature 410:471–75
Parvathenani LK, Tertyshnikova S, Greco CR, Roberts SB, Robertson B, Posmantur R (2003) P2X7 mediates superoxide production in primary microglia and is up-regulated in a transgenic mouse model of Alzheimer’s disease. J Biol Chem 278:13309–3317
Lindenlaub T, Sommer C (2000) Partial nerve transection as a model of neuropathic pain: a qualitative and quantitative neuropathological study. Pain 89:97–06
Holden JE, Pizzi JA (2003) The challenge of chronic pain. Adv Drug Del Rev 55:935–48
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Hughes, J.P., Hatcher, J.P. & Chessell, I.P. The role of P2X7 in pain and inflammation. Purinergic Signalling 3, 163–169 (2007). https://doi.org/10.1007/s11302-006-9031-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-006-9031-1