Abstract
The main source of cholesterol in the central nervous system (CNS) is represented by glial cells, mainly astrocytes, which also synthesise and secrete apolipoproteins, in particular apolipoprotein E (ApoE), the major apolipoprotein in the brain, thus generating cholesterol-rich high density lipoproteins (HDLs). This cholesterol trafficking, even though still poorly known, is considered to play a key role in different aspects of neuronal plasticity and in the stabilisation of synaptic transmission. Moreover, cell cholesterol depletion has recently been linked to a reduction in amyloid beta formation. Here we demonstrate that guanosine, which we previously reported to exert several neuroprotective effects, was able to increase cholesterol efflux from astrocytes and C6 rat glioma cells in the absence of exogenously added acceptors. In this effect the phosphoinositide 3 kinase/extracellular signal-regulated kinase 1/2 (PI3K/ERK1/2) pathway seems to play a pivotal role. Guanosine was also able to increase the expression of ApoE in astrocytes, whereas it did not modify the levels of ATP-binding cassette protein A1 (ABCA1), considered the main cholesterol transporter in the CNS. Given the emerging role of cholesterol balance in neuronal repair, these effects provide evidence for a role of guanosine as a potential pharmacological tool in the modulation of cholesterol homeostasis in the brain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although cholesterol metabolism in peripheral cells has been studied in detail, much less is known about lipid homeostasis in the central nervous system (CNS). There is increasing evidence that cholesterol plays a key role in the regulation of synaptic physiology and neurotransmission, as well as in those mechanisms underlying synaptic plasticity [1]. Recent data demonstrate that, in purified cultures of retinal ganglion cells, cholesterol is able to induce the development of new synapses [2] and that cholesterol perturbation in neuronal lipid microdomains in presynaptic membranes alters the clustering of calcium channel subtypes with molecules of the exocytotic machinery, thus impairing neurotransmitter release [3]. In addition, lipid efflux and the consequent reduction in intracellular cholesterol levels seem to be an important factor in amyloid precursor protein (APP) processing. Low cellular cholesterol concentrations favour the activity of the proteolytic pathway of α-secretases [4, 5] and reduce that of β-secretases [6], resulting in a decrease of beta-amyloid (Aβ) secretion, thus strengthening the link between cholesterol and Alzheimer’s disease pathophysiology.
Even though most of the cholesterol in the brain is synthesised in situ, rather than imported from the blood, it has been proposed that, at least in adult animals, neurons seem to depend on external cholesterol supply [7]. This cholesterol supplement could reasonably derive from glial cells and mainly from astrocytes, which have been reported to synthesise approximately three-times more cholesterol than do neuronal cells [8]. Besides their presence in the plasma, lipoproteins are also present in the cerebrospinal fluid (CFS), where they resemble in size and density the high-density lipoproteins (HDLs). These lipoproteins contain different combinations of apolipoproteins E, A1, A2, A4 and/or J (ApoE, ApoA1, ApoA2, ApoA4, ApoJ) [9, 10]. ApoA1 is secreted by brain endothelial cells [11] and in only a very small amount is imported, with ApoA2, from the circulation [12]. Both astrocytes and microglia represent the main sources of ApoE, which is the major apolipoprotein present in the CNS. Glial cells have been shown to generate ApoE-containing lipoproteins, which are rich in cholesterol, and ApoJ-containing lipoproteins that, like the ApoA1 ones, are poor in cholesterol. Previous studies have reported that both ApoA1 and ApoE markedly stimulate lipid efflux from different cell types, including astrocytes [13].
The ATP-binding cassette protein A1 (ABCA1) has been shown to act as the major transporter that mediates cholesterol efflux from cells to lipid-free apolipoproteins in peripheral tissues [14]. Moreover, recent evidence has shown that: (1) ABCA1 is involved not only in lipid efflux but also in the secretion of ApoE in human macrophages [15]; (2) ApoE levels are reduced in brain of ABCA1-deficient mice [16]; (3) ABCA1 mediates cholesterol efflux and facilitates ApoE secretion from astrocytes and microglia [16], thus indicating that, in glial cells, ABCA1 may regulate not only lipid efflux but also ApoE synthesis or secretion.
We previously reported that primary cultures of astrocytes and microglia express a wide range of ATP-binding cassette (ABC) proteins, including P-glycoprotein, multi-drug related proteins and cystic fibrosis transmembrane regulator able to mediate the release of adenine-based purines at rest and much more under stimulation [17]. We have also shown that the activation of specific purinergic receptors, namely P2Y1 ATP metabotropic receptors and P2X7 ATP ionotropic receptors, was able to trigger the efflux of cysteinyl leukotrienes (CysLTs) in microglia and astrocytes, respectively [18, 19]. Pre-treatment of glial cells with a suitable cocktail of ABC protein inhibitors reduced the P2Y1 and the P2X7-mediated CysLT production, confirming that, also in astrocytes and microglia, ABC proteins are involved in the release of CysLTs and indicating that extracellular ATP modulates the activity of these membrane transporters.
Astrocytes are involved in several brain functions in physiological conditions participating in neuronal development, synaptic plasticity, activity and control of extracellular environment. They also actively participate in the processes triggered by brain injuries aimed at limiting and repairing brain damage. In these mechanisms extracellular purines, mainly adenosine and ATP, have been reported to play important roles [20]. Astrocytes represent the main sources of extracellular cerebral adenine-based purines [21, 22] and express a wide array of purinergic receptors belonging to either metabotropic adenosine P1 and ATP P2Y sites or ionotropic ATP P2X receptor subtypes [22].
We previously reported that rat brain cultured astrocytes also release guanine-based purines both at rest and under pathological conditions such as hypoxia/hypoglycaemia [23]; moreover, we recently provided evidence for the presence, in both rat brain and astrocyte membranes, of a new specific cell-surface purine binding site which recognises guanosine as its naturally occurring agonist [24, 25]. Challenging astrocytes with this nucleoside causes: (1) release of adenine-based purines [26]; (2) astrocyte proliferation [27]; (3) synthesis and release of trophic factors [22, 28]. Cell pre-treatment with this nucleoside was also able to protect SH-SY5Y human neuroblastoma cells and rat brain cultured astrocytes against apoptosis induced by Aβ and staurosporine, respectively [29, 30].
On the basis of these findings we investigated in C6 rat glioma cells and in rat brain cultured astrocytes the intracellular signalling pathways by which guanosine was able to modulate the efflux of cholesterol. The possible effect of guanosine on the expression of ApoE was also investigated.
Materials and methods
Cell culture
Rat brain cortical astrocytes
Primary cultures of astrocytes were prepared according to the method of Levison and McCarthy [31], with slight modifications. Two-four-day-old postnatal Sprague Dawley rats were used. After they had been decapitated, their neocortices were collected in the usual growth medium, high glucose Dulbecco’s modified Eagle medium (DMEM) supplemented with 10% foetal bovine serum (FBS). Subsequently, the tissue was washed in phosphate-buffered saline (PBS), cut in small fragments, digested with 0.025% trypsin/0.04% ethylenediamine tetra-acetic acid (EDTA) solution in PBS for 20 min at 37°C and then dissociated in 0.01% DNase solution in growth medium for 10 min. The pellet was then re-suspended in growth medium also containing 5 mM l-leucine methyl ester to restrain microglia contamination. Cells were seeded onto poly-d-lysine (10 µg/ml) coated flasks and maintained at 37°C in a humidified incubator under 95% air and 5% CO2. After the first 24 h, the culture medium was renewed with an identical medium without leucine methyl ester, and it was then replaced every 3–4 days. On the 7th and then on the 13th day in vitro (DIV), the cells were shaken for 3 h at 80 r.p.m. on a plate shaker to minimise microglia contamination. For bioassay, confluent primary cultures of astrocytes at the 14th DIV were trypsinised (0.025% trypsin/0.04% EDTA dissolved in PBS, 10–20 min, 37°C) and re-plated at a concentration of approximately 20–25×103 cells/cm2. After seeding, cells were maintained in the usual medium containing 5 mM leucine methyl ester only for the first 24 h.
C6 cells
Rat C6 glioma cells were cultured in low-glucose DMEM supplemented with 5% heat-inactivated FBS.
Cholesterol efflux
Cholesterol efflux was evaluated as described by Demeester et al. [32], with slight modifications. To evaluate cholesterol efflux we seeded astrocytes and C6 cells in 24-well plates at 150,000 cells/well and 100,000 cells/well, respectively. Cells were labelled by incubation for 24 h in fresh growth medium containing 2 µCi/ml of [3H]cholesterol (1.48 TBq/mmol, Amersham Biosciences, Milan, Italy). Following labelling with [3H]cholesterol, cells were washed and incubated for an additional 24 h in serum-free media containing 2 mg/ml bovine serum albumin (BSA) to allow for equilibration of [3H]cholesterol with the intracellular pool. After this incubation, cells were washed and treated in serum-free media as indicated. After treatment, the media were briefly centrifuged to remove non-adherent cells. Cells were lysed in 0.1 N NaOH. Aliquots of medium and cell lysates were assayed by liquid scintillation counting. We calculated the percentage cholesterol efflux by dividing the radioactivity in the medium by the sum of the radioactivity in the medium and cell lysate.
RNA isolation and reverse transcriptase-polymerase chain reaction
Total RNA was isolated from confluent cells using TRIzol reagent (Life Technologies, Milan, Italy) according to the manufacturer’s recommendations. The resulting RNA pellet was washed with 70% ice-cold ethanol, air dried and re-dissolved in 30 µl diethyl-pyrocarbonate (DEPC)-treated water. The quantity and purity of RNA were estimated spectrophotometrically by absorbance at 260 nm, and 5 µg were run on formaldehyde gel to confirm the integrity of the RNA, as indicated by the preservation of the 28 and 18S rRNA.
To remove any genomic DNA contaminants we treated RNA samples (10 µg) with 1 U Dnase-I RNase-free (Roche, Monza, Italy). First strand cDNA was synthesised from 1.5 µg of total RNA using the reverse transcriptase-polymerase chain reaction (RT-PCR) system RETROscript (Ambion, Tex., USA) with random hexamers. The resultant cDNA (2 µg) was amplified in a 100 µl reaction volume containing PCR reaction buffer, 1.5 mM MgCl2, 0.2 mM each deoxy-dNTP, 1 µM oligonucleotide primers (MWG Biotech, Ebersberg, Germany), 2.5 U AmpliTaq Gold DNA polymerase (Applied Biosystems, Calif., USA). The sequences of the oligonucleotide primers for amplification of rat ABCA1 and rat ApoE were the following: ABCA1 (GenBank accession number NM_178095) forward 5′-CT CGAATTATTTGGAAGGCAC-3′ and reverse 5′-TTT GGGGACTGAACATCCTCT-3′; apoE (GenBank accession number BC086581) forward 5′-GGAACTGACGG TACTGATGGA-3′ and reverse 5′- TCGGATGCGG TCACTCAAA-3′. Conditions applied for PCR amplification were: 94 °C for 5 min, 35 cycles of denaturation at 94 °C for 1 min, annealing at 55 °C for 1 min and elongation at 72 °C for 1 min. Reaction was also conducted without the reverse transcriptase step as a control for genomic contamination. Amplification products were resolved by 1.5% agarose gel electrophoresis. The identity of the products was confirmed by cycle sequencing of the amplified cDNA.
Northern blotting analysis
Total RNA was isolated from the cells as reported above. Equal amounts of RNA (15 µg/lane) were fractionated on formaldehyde denaturing 1% agarose gel and blotted overnight onto Hybond N nylon membrane (Amersham Pharmacia Biotech, Buckinghamshire, UK). The filter was then UV cross-linked in UV Stratalinker 1800 (Stratagene). The blots were pre-hybridised for at least 8 h at 42°C in a solution containing 50% formamide, 5× Denhardt’s solution, 0.1% sodium dodecyl sulphate (SDS) and 100 µg/ml salmon sperm DNA. Hybridisation of cDNA probes was performed in a buffer of the same composition containing 106 c.p.m./ml of radiolabelled probe. cDNAs, obtained by extracting PCR products from agarose gel slices (Millipore, Bedford, Mass., USA), were radiolabelled by the method of random priming (Megaprime DNA labelling system, Amersham Pharmacia Biotech) using [alpha 32P]-dCTP (Amersham Pharmacia Biotech). After hybridisation, the membranes were washed in 0.1X SSC, containing 0.1% SDS, at 50 °C and exposed to Kodak Biomax MS autoradiography film at −80 °C with intensifying screen for 1 day. Subsequent to hybridisation with ApoE cDNA probe, Northern blots were hybridised with a probe for 28S to allow correction for the recovery of RNA in each sample. Experiments were performed at least in triplicate. For the purpose of quantification, autoradiograms were scanned using laser densitometry. ApoE mRNA signals were normalised against 28S content by determination of the ratio of the respective optical densities.
Western blotting analysis
ABCA1
ABCA1 protein expression was evaluated as described by Wagner et al. [33]. C6 cells and astrocytes in 100 mm dishes were incubated for 24 h in serum-free medium to equilibrate the cells and then treated as indicated. At the end of the incubation times, cells were lysed at 4 °C in a buffer consisting of 10 mM Tris-HCl pH 7.5, 150 mM NaCl, 1.0 mM EDTA, 1% Triton X-100, 1 mM PMSF, 5 µg/ml leupeptin, 5 µg/ml aprotinin. The cells were lysed by subjecting them to three cycles of freezing and thawing, followed by 5 min of microcentrifugation to remove nuclei. An aliquot of the supernatants was processed for the assessment of protein concentration by the Bradford method [34]. Extracts were incubated in sodium dodecyl sulfate gel loading buffer containing 5% β-mercaptoethanol at room temperature for 10 min before being loaded on the gel. Electrophoresis was performed in 12% SDS-polyacrylamide gel using 50 µg of total protein per lane. After separation, proteins were transferred onto a PVDF membrane (Bio-Rad Laboratories, Milan, Italy) using a mini-trans-blot transfer cell (Bio-Rad Laboratories). After blocking, membranes were incubated with specific anti-ABCA1 antibody (Novus Biologicals, Littleton, Colo., USA) overnight at 4 °C and then washed and exposed to donkey anti-rabbit HPR-conjugated secondary antibody for 1 h at room temperature (Amersham Pharmacia Biotech). Immunocomplexes were visualised using the enhancing chemiluminescence (ECL) detection system (Amersham Pharmacia Biotech). To determine the equal loading of samples per lane, at the end of each experiment we stripped the blots and re-probed with a rabbit anti-β actin polyclonal antibody (Santa Cruz Biotechnology), according to the manufacturer’s instructions.
Extracellular signal-regulated kinase 1/2
Western blot analysis was used to evaluate mitogen-activated protein kinase (MAPK) activation in C6 cells. Cells in 100 mm dishes were incubated for 24 h in serum-free medium to equilibrate the cells and then treated as indicated. At the end of the indicated incubation times, cells were harvested at 4 °C in buffers specific to the assays (25 mM Tris buffer, pH 7.4, containing 150 mM NaCl, 100 µM sodium orthovanadate, 1.5 mM MgCl2, 1.0 mM EDTA, 1% NP40, 10% glycerol, 1 mM PMSF, 5 µg/ml leupeptin, 5 µg/ml aprotinin). After sonication, samples were centrifuged at 14,000 r.p.m. for 5 min, and an aliquot of the supernatants was processed for the assessment of protein concentration by the Bradford method. Samples were diluted in SDS-bromophenol blue buffer and boiled for 5 min before loading. Electrophoresis was performed in 12% SDS-polyacrylamide gel using 10 µg of total protein per lane. After separation, proteins were transferred onto a PVDF membrane (Bio-Rad Laboratories) using a minitrans-blot transfer cell (Bio-Rad Laboratories). After blocking, membranes were incubated with polyclonal primary antibody (rabbit phospho-extracellular signal-regulated kinase (ERK) 1/2 antibody, New England Biolabs, Celbio, Milan, Italy; final dilution 1:1000) for 1 h at room temperature and then repeatedly washed and exposed to donkey anti-rabbit HPR-conjugated secondary antibody for 1 h at room temperature (Amersham Pharmacia Biotech; final dilution 1:5000). Immunocomplexes were visualised using the ECL detection system (Amersham Pharmacia Biotech). To determine the equal loading of samples per lane, at the end of each experiment we stripped the blots and re-probed with a goat polyclonal antibody against total ERK1/2, followed by a secondary antibody anti-goat IgGHRP (both antibodies from Santa Cruz Biotechnology), according to the manufacturer’s instructions.
ApoE
ApoE expression was evaluated as described by Mori et al. [35]. Cells were scraped, lysed in a buffer containing 20 mM Tris-HCl, pH 7.4, 5 mM MgCl2, 100 mM NaCl, 1% NP40, 1 mM PMSF, 5 µg/ml leupeptin, 5 µg/ml aprotinin (all protease inhibitors were from Sigma) and centrifuged at 14,000 r.p.m. for 10 min to remove nuclei. Cell lysate samples were analysed for apoE expression by Western blot. Electrophoresis was performed in 12% SDS-polyacrylamide gel using 50 µg of total protein per lane. After separation, proteins were transferred onto a PVDF membrane (Bio-Rad Laboratories) using a mini-trans-blot transfer cell (Bio-Rad Laboratories). After blocking, membranes were incubated with specific monoclonal anti-ApoE antibody (BD Biosciences) overnight at 4 °C and then washed and exposed to sheep anti-mouse HPR-conjugated secondary antibody for 1 h at room temperature (Amersham Pharmacia Biotech). Immunocomplexes were visualised using the ECL detection system (Amersham Pharmacia Biotech). To determine the equal loading of samples per lane, at the end of each experiment we stripped the blots and re-probed with a rabbit anti-β actin polyclonal antibody (Santa Cruz Biotechnology), according to the manufacturer’s instructions.
Statistical analysis
The statistical significance was established by the analysis of data by Student’s two-tailed t-test, using the Prism (version 3.03) program (GraphPad Software, San Diego, Calif., USA) with P < 0.05 considered to be significant.
Results
ATP-binding cassette protein A1 expression in primary astrocytes of rat brain and C6 rat glioma cells
It was reported that astrocytes express ABCA1 [36], whereas no data have been published on the expression of this cholesterol transporter in C6 rat glioma cells. As shown in Figure 1, RT-PCR performed by using total RNA from cultures of rat brain astrocytes confirmed the presence of ABCA1 in these cells. Like astrocytes (Figure 1a), C6 cells also expressed ABCA1 mRNA. The PCR product was separated on a 1.5% agarose gel, and a single band of 331 bp, corresponding to ABCA1 mRNA, was revealed.
Expression of ABCA1 in rat brain cultured astrocytes and C6 rat glioma cells was investigated by RT-PCR and by Western blot. (a) Total RNA was isolated from the cells, and 2.5 µg was used for reverse transcription and then subjected to PCR amplification using primer pairs specific for this transporter. Amplification products of the expected size (331 bp) were resolved by agarose (1.5%) gel electrophoresis. M represents the size markers as indicated; lane 1 astrocytes, lane 2 C6 cells. (b) Total proteins were isolated from the cells, and equal amounts (50 µg) were separated on 12% SDS-polyacrylamide gel. ABCA1 protein was detected using a rabbit polyclonal anti-ABCA1 antibody. The immunoblot was also stripped, and western blotting with β actin antibody was used as a loading control. Lane 1 astrocytes; lane 2 C6 cells. Results are representative of experiments carried out with RNA and protein isolated from at least three independent cell culture seedings
The ABCA1 expression was also detected at protein level by Western blotting in both glial cell types (Figure 1b).
Effect of apolipoprotein A1, 22R-hydroxycholesterol and 9-cis-retinoic acid on cholesterol efflux from primary astrocytes of rat brain and C6 rat glioma cells
Recent studies have shown that ApoA1 is able to facilitate cholesterol efflux from astrocytes [16, 36]. The increase of cholesterol efflux was greater in the presence of 22R-hydroxycholesterol (22R) and 9-cis-retinoic acid (RA), which are ligands for the nuclear hormone liver X receptors (LXRs) and retinoic receptors (RXRs), respectively [36]. Thus, we next examined cholesterol efflux in both astrocytes and C6 cells either in basal conditions or under cell treatment with the above-mentioned pharmacological agents. To induce cholesterol efflux we added 15 µg/ml ApoA1 to the cell medium alone or in combination with 10 µM 22R plus 10 µM RA. At the chosen times cholesterol efflux was determined as described in Materials and methods. As shown in Figure 2a, in astrocytes, as expected, cholesterol efflux to ApoA1 was significantly increased after 12 h of treatment up to 24 h. Interestingly, the same trend was found in C6 cells (Figure 2b). In both cell types the lipid efflux to extracellular ApoA1 was stimulated by treatment with the combination of the oxysterol plus the RXR ligand (Figure 2). Thus, as a first step, we chose to use C6 cells to test the effect of guanosine on cholesterol efflux.
Time course of apolipoprotein-dependent cholesterol efflux in rat brain cultured astrocytes (a) and C6 cells (b) treated with LXR/RXR ligands. Cells were loaded for 24 h with [3H]cholesterol (2 µCi/ml), allowed to equilibrate for 24 h with 2 mg/ml BSA, and treated with ApoA1 (15 µg/ml) in the presence or absence of 22R+RA (10 µM each). Media and cell lysates were subjected to liquid scintillation counting. Cholesterol efflux, expressed as a percentage, was calculated as reported in Materials and methods. Data points were measured in triplicate and represent the mean ± SEM of three independent experiments. * P < 0.05, ** P < 0.005 versus control (Student’s t-test)
Effect of guanosine on cholesterol efflux from C6 rat glioma cells and primary astrocytes of rat brain
When added to the culture medium in the absence of ApoA1, guanosine (300 µM), used at a concentration reported to stimulate astrocyte proliferation to the maximum [27] and protect astrocytes against Aβ or staurosporine-induced apoptosis [29, 30], was able to increase significantly the cholesterol efflux from C6 cells. Interestingly, the effect of this nucleoside became evident much earlier than that obtained by treating the cells with ApoA1 in the presence or in the absence of 22R plus RA. Indeed, as shown in Figure 3, guanosine had already markedly increased cholesterol efflux after 1 h of treatment (approximately 4.5-times the control value). The effect was still evident after 6 h (about 1.5-times the control values), whereas, after 18 h, guanosine-induced cholesterol efflux was only slightly greater than the control values.
Time course of cholesterol efflux from C6 rat glioma cells in both basal conditions and after treatment with 300 µM guanosine. Cells were loaded for 24 h with [3H]cholesterol (2 µCi/ml), incubated for 24 h with 2 mg/ml BSA and treated with guanosine (300 µM) for the indicated periods. Radioactivity was evaluated in both media and cell lysates. Cholesterol efflux, expressed as a percentage, was calculated as reported in Materials and methods. Data points were measured in triplicate and represent the mean ± SEM of four independent experiments. * P < 0.05, ** P < 0.005, *** P < 0.0005 versus untreated cells (Student’s t-test)
Thus, the 1 h treatment was chosen to test different guanosine concentrations on cholesterol efflux, not only from C6 but also from cultured astrocytes. The addition of guanosine, up to 300 µM for 1 h, to the cell medium caused a concentration-dependent increase in cholesterol efflux (Figure 4) in both astrocytes and C6 cells. The calculated EC50 for guanosine in these experiments was 38 µM and 35 µM for C6 cells and astrocytes, respectively. A concentration of 150 µM guanosine was then chosen for the further experiments.
Dose-dependent increase of cholesterol efflux induced by guanosine in rat brain cultured astrocytes and C6 rat glioma cells. Following labelling and equilibration, cells were incubated with the indicated concentrations of guanosine. After 1 h, radioactivity in the media and in the cell lysates was measured and cholesterol efflux calculated, as reported in Materials and methods. Data points were measured in triplicate and represent the mean ± SEM of four independent experiments
Extracellular signal-regulated kinase signalling involvement in guanosine-mediated increase of cholesterol efflux
We recently reported that guanosine induces a rapid and time-dependent increase in ERK1/2 phosphorylation in both microglia and astrocytes [37]. The same effect was also described in PC12 cells [38]. Thus, we investigated whether treatment of C6 cells with guanosine could affect this intracellular target. As shown in Figure 5a, the exposure of C6 cells to 150 µM guanosine caused an increase in ERK1/2 phosphorylation as early as 5 min after treatment, being maximal by 10 min following the nucleoside addition and declining towards the basal values after 20 min of treatment. Again, the effect of this nucleoside was very similar to that obtained using cultured astrocytes (Figure 5b). To test whether this pathway was involved in the guanosine-mediated increase in cholesterol efflux, we pre-treated C6 cells and astrocytes for 30 min with the extracellular signal-regulated kinase kinase 1/2 (MEK1/2) inhibitor PD98059 (30 µM). The concentration used was that reported to reduce: (1) the anti-apoptotic effect of guanosine in cultured astrocytes [30]; (2) the guanosine-induced P2Y2 up-regulation (P. Ballerini, personal communication). This drug reduced the guanosine-mediated cholesterol efflux by approximately 60% in both C6 cells and astrocytes (Figure 6), suggesting that the activation of the MAPK pathway was involved in this mechanism.
Time-dependent increase of ERK1/2 phosphorylation induced by guanosine in rat brain cultured C6 rat glioma cells (a) and astrocytes (b). Cells were serum deprived for 24 h and then treated for the indicated periods with 150 µM guanosine. Cell lysates were prepared as described in Materials and methods and immunoblotted with phospho-ERK specific antibodies. After development, the membranes were stripped and re-probed with regular antibody against ERK1/2. The blots are representative of at least three independent experiments with similar results. Immunoblots were quantified by densitometric analysis, and the ERK1/2 values, normalised to the corresponding β actin values, are expressed as number of times of increase versus basal values (untreated cells) in the histograms under the blots. Data are mean ± SEM of three independent experiments. * P < 0.05, ** P < 0.005, *** P < 0.0005 versus basal values (Student’s t-test)
Effect of the MEK1/2 inhibitor PD98059 on cholesterol efflux induced by guanosine. Following labelling and equilibration, cells were pre-incubated for 30 min with PD98059 (30 µM) and then treated with 150 µM guanosine. After 1 h radioactivity in media and in cell lysates was measured and cholesterol efflux calculated, as reported in Materials and methods. Data points were measured in triplicate and represent the mean ± SEM of three independent experiments. # P < 0.0001 guanosine-treated cells versus untreated cells, * P < 0.005 PD98059-treated cells versus guanosine-treated cells (Student’s t-test)
Protein kinase C and protein kinase A involvement in guanosine-mediated increase of cholesterol efflux
It has been recently reported that, in other cell types, protein kinase C (PKC) signalling can cause phosphorylation/activation of ERK [39, 40]. Cell pre-treatment with calphostin C (100 nM), at a concentration known to specifically inhibit PKCs, reduced, by approximately 35%, the guanosine-mediated increase of cholesterol efflux in both C6 cells and cultured astrocytes, as shown in Figure 7.
Effect of inhibitors of PKC and PKA on the cholesterol efflux induced by guanosine. Following labelling and equilibration, cells were pre-incubated for 30 min with calphostin C (100 nM), to inhibit PKCs, or for 3 h with KT5720 (1 µM), to inhibit PKA, and then treated with 150 µM guanosine. After 1 h the radioactivity in media and cell lysates was measured and cholesterol efflux calculated, as reported in Materials and methods. Data points were measured in triplicate and represent the mean ± SEM of three independent experiments. # P < 0.0001 guanosine-treated cells versus untreated cells, * P < 0.05 calphostin C-treated or KT5720-treated cells versus guanosine-treated cells (Student’s t-test)
Previously, we had shown that guanosine induced a dose-dependent increase in intracellular cyclic AMP levels (cAMP) in slices from rat brain [25] and in rat brain cultured astrocytes (P. Patricelli, oral communication). As seen in Figure 7, cell pre-treatment with the specific protein kinase A (PKA) inhibitor KT5020 for 3 h reduced only by approximately 30% the guanosine effect on cholesterol efflux from C6 cells and astrocytes.
Phosphoinositide 3 kinase involvement in guanosine-mediated increase of cholesterol efflux
We have recently shown that another intracellular pathway activated by guanosine is represented by phosphoinositide 3 kinase (PI3K) [30]. Thus, we investigated whether this transduction signalling was involved in guanosine-mediated increase of cholesterol efflux. To this aim, we used the cell-permeable selective PI3K inhibitor, LY294002. When C6 cells and astrocytes were pre-treated for 30 min with LY294002 (30 µM), the increase in cholesterol efflux induced by guanosine proved to be significantly reduced by approximately 50%, as shown in Figure 8. When the drug was used in combination with the MEK1/2 inhibitor PD98059, the effect was similar to that obtained by LY294002 (Figure 8) and PD98059 (Figure 6) given alone.
Effect of the PI3K inhibitor LY294002 alone or in combination with the MEK1/2 inhibitor PD98059 on cholesterol efflux induced by guanosine. Following labelling and equilibration, cells were pre-incubated for 30 min with LY294002 (30 µM) or with LY294002 (30 µM) plus PD98059 (30 µM) and then treated with 150 µM guanosine. After 1 h the radioactivity in media and cell lysates was measured and cholesterol efflux calculated as reported in Materials and methods. Data points were measured in triplicate and represent the mean ± SEM of three independent experiments. ## P < 0.0001 guanosine-treated cells versus untreated C6 cells, # P < 0.0005 guanosine-treated astrocytes versus untreated astrocytes, ** P < 0.005 LY294002-treated or LY294002+ PD98059-treated cells versus guanosine-treated C6 cells, * P < 0.05 LY294002-treated or LY294002+ PD98059-treated astrocytes versus guanosine-treated astrocytes (Student’s t-test)
Effect of apolipoprotein A1, 22R-hydroxycholesterol, 9-cis-retinoic acid and guanosine on ATP-binding cassette A1 expression in C6 rat glioma cells and primary astrocytes of rat brain
Very little is known of the pharmacological regulation of cholesterol efflux mechanisms, not only in the CNS but also in peripheral tissues. Evidence has been provided on the capability of ApoA1, oxysterols and RA in causing an increase of ABCA1 expression, both at message level and protein level in different cell types, including neuronal cells [36, 41]. To determine whether the induction of ABCA1 might be involved in the enhanced efflux of cholesterol induced by the guanine-based nucleoside, we exposed the cells to 150 µM guanosine for 1 h, 3 h and 6 h (Figure 9).
Time course of ABCA1 expression induced by 150 µM guanosine in (a) C6 rat glioma cells and (b) rat brain cultured astrocytes. Cells were serum deprived for 24 h and were treated for the indicated periods with 150 µM guanosine or with ApoA1 (15 µg/ml) plus 22R (10 µg/ml) and RA (10 µg/ml). Fifty microgrammes of total protein were loaded per lane and immunoblotted with rabbit polyclonal antibody to ABCA1. Western blotting with β actin antibody was used as a loading control. The blots are representative of three independent experiments with similar results. Immunoblots were quantified by densitometric analysis, and the ABCA1 values, normalised to the corresponding β actin values, are expressed as number of times of increase versus basal values (untreated cells) in the histograms under the blots. Data are mean ± SEM of three independent experiments. * P < 0.05 versus basal values (Student’s t-test)
As shown by the representative Western blot reported in Figure 9, guanosine was unable to modify ABCA1 expression either in C6 glioma cells or in rat brain astrocytes at the chosen times. On the other hand, the combination of ApoA1, 22R and RA, considered as positive control, significantly increased the protein levels in both types of glial cells after 12 h of treatment, a time when, in our experimental conditions, a stimulated cholesterol efflux could be pointed out.
Effect of guanosine on apolipoprotein E expression in primary astrocytes of rat brain
Recent studies in other cell types, such as human macrophages, have indicated that the removal of secreted ApoE from the medium by the addition of specific antibodies significantly reduced cholesterol efflux from these cells [41]. We then tested whether guanosine would be able to increase ApoE expression in glial cells after 1 h of incubation, a time at which the nucleoside was able to increase cholesterol efflux to the maximum.
As shown by the representative Northern blot reported in Figure 10a, 150 µM guanosine induced ApoE expression in astrocytes. This increase was paralleled by a rise in ApoE content in these cells, measured by Western blot analysis as reported in Figure 10b.
Modulation of ApoE expression by ApoA1 plus LXR/RXR ligands and guanosine in rat brain cultured astrocytes by Northern blot (a) and Western blot (b). Cells were treated for 12 h with a combination of 15 µg/ml ApoA1, 10 µM 22R and 10 µM RA or for 1 h with 150 µM guanosine. At the end of the periods of treatment (a) total RNA was isolated as described in Materials and methods and equal amounts were electrophoresed through formaldehyde-containing gel, transferred to Nylon membrane and hybridised with 32P-labelled cDNA probes. 28S probe was used as control for loading and integrity of the RNAs. The blot is representative of at least three independent experiments. Values from densitometric analysis were normalised to those of 28S and expressed as number of times of increase versus basal values (untreated cells) in the histograms under the blot. Data are mean ± SEM of three independent experiments. * P < 0.05, ** P < 0.005 versus basal values (Student’s t-test). (b) ApoE levels in whole cell lysates were determined using a monoclonal anti-ApoE antibody. β actin was used as loading control. Immunoblots were quantified by densitometric analysis and the ApoE values, normalised to the corresponding β actin values, are expressed as number of times of increase versus basal values (untreated cells) in the histograms under the blots. Data are mean ± SEM of three independent experiments. * P < 0.05, ** P < 0.005 versus basal values (Student’s t-test)
Discussion
There is increasing evidence indicating that cholesterol trafficking can have important implications in CNS function, both in physiological and even more in pathological conditions; however, the mechanisms underlying the synthesis, release, redistribution and uptake of cholesterol among the cells in the CNS are still poorly known.
It has been reported that the efflux of cholesterol complexed to lipoproteins containing ApoE from glial cells promotes synapse development in cultured neurons [42]. These data are in agreement with results showing that most synapses in the CNS develop after the differentiation of astrocytes [43].
The role of cholesterol homeostasis has also been pointed out by data demonstrating that ABCA1 and ApoE are markedly up-regulated at sites of brain damage, thus strongly suggesting a role in neuronal repair for molecules that participate in cholesterol efflux and redistribution [44]. Additionally, ABCA1, recognised as an essential protein for cholesterol secretion and subsequent HDL formation, facilitates cholesterol efflux to exogenous apolipoproteins in primary cultures of glial cells, including astrocytes [16].
The results reported in the present paper confirm that treatment of astrocytes with the lipid acceptor ApoA1 increases cholesterol efflux in a time-dependent manner. The increase of cholesterol efflux was greater when the combination of the natural and synthetic LXR/RXR ligands was added to the medium of astrocytes pre-treated with ApoA1. In agreement with data already reported in the literature, our results show that the combination of ApoA1, 22R and RA was able to cause, in these cells, an increase in ABCA1 expression [36, 44]. Similar results were obtained using C6 cells, indicating that these rat glioma cells can represent a good model to study cholesterol efflux and its possible modulation in glia.
Besides being the main source of cholesterol, astrocytes are also recognised as the major source of extracellular purines, both adenine and guanine-based ones, in the CNS [21, 23]. Interestingly, it has also been shown that the extracellular concentration of guanine-based purines is dramatically enhanced, following insults, more than that of the adenine-based counterparts [23]. Even though the role exerted by adenosine and ATP in the CNS is known much better than that played by guanosine, a great body of evidence is accumulating on the neuroprotective effects mediated by this nucleoside.
In this view, we previously reported that, in astrocytes, guanosine was able to: (1) promote cell proliferation [27, 45]; (2) induce the synthesis and release of neurotrophic and pleiotrophic factors [23, 37, 46, 47]; (3) protect the cells against Aβ- or staurosporine-induced apoptosis [29, 30]. Guanosine is also able to modulate neurotransmission by stimulating glutamate uptake in astrocytes [48].
Moreover, this nucleoside has been shown to be effective in vivo, being able to produce anti-convulsant action against seizures caused by glutamatergic agents [49], inhibit locomotor stimulation induced by dizocilpine [50] and promote remyelination and functional recovery in rats submitted to spinal cord injury [51].
Recently, we reported evidence for the presence of a high-affinity binding site for guanosine in membranes from whole rat brain and from astrocytes [24, 25]. Thus, at least some of the effects mediated by extracellular guanosine may be exerted by its binding to these specific cell membrane sites. Our laboratories are currently investigating the structure and signal transduction pathways of this potential new purinergic receptor.
In the present study we show that guanosine enhances cholesterol efflux from both C6 cells and rat brain cultured astrocytes 1 h after treatment in a dose-dependent manner. The increase in cholesterol efflux was still evident 6 h after treatment, though to a lesser extent. The decrease of the guanosine effect could fit well with our previous observations showing that guanosine, added to the astrocyte culture medium, was metabolised by 75% within 2–3 h [26].
Several kinases, including MAPK have been implicated in the modulation of cholesterol efflux in different cell types.
We have already reported that ERK1/2 phosphorylation is an important event involved in several guanosine-mediated effects in astrocytes, including the synthesis of trophic factors and the protection against staurosporine-induced apoptosis [30, 47]. Recently, this intracellular pathway has also been shown to be involved in the guanosine-mediated protection of neuronal cells from chemical hypoxia [38].
In the present study we report that, as expected, guanosine also significantly and rapidly triggered ERK1/2 phosphorylation in C6 rat glioma cells. Moreover, this pathway also seems to play an important role in mediating the effect of guanosine on cholesterol efflux from glial cells, as shown by the inhibitory action exerted by the MEK1/2 inhibitor PD98059.
Another intracellular pathway activated by guanosine, when added to the astrocyte culture medium, is represented by PI3K. We have shown that the staurosporine-mediated pro-apoptotic effect was markedly and dose-dependently reduced in cells pre-treated with guanosine [30]. The protective effect of the nucleoside was abolished when astrocytes were pre-incubated with LY294002 (30 µM), a selective inhibitor of PI3K [30]. Consistent with these findings, our results obtained using the same inhibitor suggest that the PI3K pathway could represent a key mediator that links the activation of a potential guanosine purinoceptor to the modulation of mechanisms underlying cholesterol efflux in glial cells. Since the cell treatment with the combination of LY294002 and PD98059 caused a reduction in guanosine-induced cholesterol efflux, which was similar to that obtained by each drug added alone to culture medium, it is tempting to speculate that the two pathways converge. Thus, the PI3K/ERK1/2 pathway may represent a signalling event involved in the guanosine-mediated regulation of cholesterol efflux in glial cells.
A number of protein kinases have been reported to modulate the activity of ABCA1, thus influencing cholesterol efflux in different cell types [14]. In kidney cells, RAW mouse macrophages and in a Flip-in 293 cell line, it has been shown that PKA-mediated phosphorylation of ABCA1 is required for its lipid transport activity [52].
It has also been reported that PKC activators stimulate cholesterol efflux and PKC inhibitors substantially reduce cholesterol efflux induced by ApoA1 in macrophages and human THP-1 cells [53].
Previously, we observed that, in slices of rat cerebral cortex, guanosine caused an increase in intracellular cAMP accumulation [25]. Guanosine-induced rise in cAMP levels could also be detected in rat brain cultured astrocytes, though to a lesser extent (P. Patricelli, personal communication). Our results show that the PKA inhibitor reduced, by approximately 30%, guanosine-mediated cholesterol efflux in both C6 rat glioma cells and cultured astrocytes. Similar results were obtained by pre-treating glial cells with the PKC inhibitor, thus suggesting that these kinases can participate in the guanosine-mediated modulation of cholesterol efflux in these cells.
Data regarding the possible pharmacological modulation of ABCA1 in the CNS are still limited. It has been reported that the increased cholesterol efflux induced by ApoA1 plus 22R and RA in astrocytes correlates with an induced ABCA1 mRNA expression in these cells [36]. Accordingly, our results show that the LXR/RXR ligands in combination with ApoA1, considered as reference drugs, increased the levels of ABCA1 protein in both C6 cells and rat brain cultured astrocytes.
On the other hand, guanosine, used at the same concentration and times that were able to trigger an increased cholesterol efflux from the cells, was unable to induce an up-regulation of the lipid membrane transporter, suggesting that this mechanism seems not to be involved in the nucleoside-mediated effect.
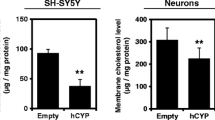
Interestingly, we observed that guanosine was able to enhance cholesterol efflux without the addition of apolipoproteins to the culture medium. It has been reported that ABCA1 is a peculiar ABC protein in that it is necessary that apolipoproteins bind either directly to the transporter or indirectly, possibly through the stimulation of other receptors present on the plasma membrane, to activate ABCA1-mediated lipid efflux [54]. Apolipoproteins could also stimulate ABCA1-mediated lipid efflux by favouring the intracellular recycling of this ABC protein. However, since astrocytes are considered to be, together with microglial cells, the main source of ApoE in the CNS, it could be speculated that guanosine was able to enhance the expression of this apolipoprotein. This event could make the addition of exogenous apolipoproteins less critical to trigger an ABCA1-dependent cholesterol efflux. This hypothesis seems to be likely; indeed, we found that guanosine had already increased the expression of ApoE in rat brain cultured astrocytes both at mRNA level and at protein level after 1 h treatment when the nucleoside stimulated the lipid efflux.
Further experiments are needed to evaluate better the functional role of ABCA1 and that of other elements, such as the enzymes responsible for cholesterol metabolism, in guanosine-mediated efflux of cholesterol.
However, on the whole, the results presented here strongly suggest that guanosine could have a role in ameliorating the delivery of cholesterol from glial cells, thus potentially favouring neuronal repair and regeneration. This event could be considered a further mechanism by which this guanine-based nucleoside, regulating astrocyte activity, may exert its neuroprotective effects.
Abbreviations
- ABCA1:
-
ATP-binding cassette protein A1
- ApoA1:
-
Apolipoprotein A1
- APP:
-
amyloid precursor protein
- Aβ:
-
beta amyloid
- CNS:
-
central nervous system
- CSF:
-
cerebral spinal fluid
- CysLTs:
-
cysteinyl leukotrienes
- ERK1/2:
-
extracellular signal regulated kinase 1/2
- HDL:
-
high density lipoproteins
- LY294002:
-
[2-(4-morpholinyl)-8-phenyl-4H-1benzopyran-4-one]
- LXR:
-
liver X receptor
- MAPK:
-
mitogen-activated protein kinase
- MEK1/2:
-
extracellular signal-regulated kinase kinase 1/2
- PD98059:
-
2-(2-amino-3-methoxy phenyl)-4H-1-benzopyran-4-one
- PI3K:
-
phosphoinositide 3 kinase
- PKA:
-
protein kinase A
- PKC:
-
protein kinase C
- RA:
-
9-cis-retinoic acid
- RT-PCR:
-
reverse transcription followed by PCR
- RXR:
-
retinoic X receptor
- 22R:
-
22R-hydroxycholesterol
References
Koudinov AR, Koudinova NV (2001) Essential role for cholesterol in synaptic plasticity and neuronal degeneration. FASEB J 15:1858′860
Goritz C, Mauch DH, Pfrieger FW (2005) Multiple mechanisms mediate cholesterol-induced synaptogenesis in a CNS neuron. Mol Cell Neurosci 29:190′01
Taverna E, Saba E, Rowe J et al (2004) Role of lipid microdomains in P/Q-type calcium channel (Cav2.1) clustering and function in presynaptic membranes. J Biol Chem 279:5127′134
Simons M, Keller P, Dichgans J et al (2001) Cholesterol and Alzheimer’s disease: is there a link? Neurology 57:1089′093
Simons M, Keller P, De Strooper B et al (1998) Cholesterol depletion inhibits the generation of beta-amyloid in hippocampal neurons. Proc Natl Acad Sci USA 95:6460′464
Kalvodova L, Kahya N, Schwille P et al (2005) Lipids as modulators of proteolytic activity of BACE: involvement of cholesterol, glycosphingolipids, and anionic phospholipids in vitro. J Biol Chem 280:36815′6823
Pfrieger FW (2003) Outsourcing in the brain: do neurons depend on cholesterol delivery by astrocytes? Bioessays 25:736′37
Saito M, Benson EP, Saito M et al (1987) Metabolism of cholesterol and triacylglycerol in cultured chick neuronal cells, glial cells, and fibroblasts: accumulation of esterified cholesterol in serum-free culture. J Neurosci Res 18:319′25
Borghini I, Barja F, Pometta D et al (1995) Characterization of subpopulations of lipoprotein particles isolated from human cerebrospinal fluid. Biochim Biophys Acta 1255:192′00
Koch S, Donarski N, Goetze K et al (2001) Characterization of four lipoprotein classes in human cerebrospinal fluid. J Lipid Res 42:1143′151
Weiler-Guttler H, Sommerfeldt M, Papandrikopoulou A et al (1990) Synthesis of apolipoprotein A-1 in pig brain microvascular endothelial cells. J Neurochem 54:444′50
Panzenboeck U, Balazs Z, Sovic A et al (2002) ABCA1 and scavenger receptor class B, type I, are modulators of reverse sterol transport at an in vitro blood-brain barrier constituted of porcine brain capillary endothelial cells. J Biol Chem 277:42781′2789
Michikawa M, Fan Q, Isobe I et al (2000) Apolipoprotein E exhibits isoform-specific promotion of lipid efflux from astrocytes and neurons in culture. J Neurochem 74:1008′016
Oram JF (2000) Tangier disease and ABCA1. Biochim Biophys Acta 1529:321′30
Von Eckardstein A, Langer C, Engel T et al (2001) ATP binding cassette transporter ABCA1 modulates the secretion of apolipoprotein E from human monocyte-derived macrophages. FASEB J 15:1555′561
Hirsch-Reinshagen V, Zhou S, Burgess BL et al (2004) Deficiency of ABCA1 impairs apolipoprotein E metabolism in brain. J Biol Chem 279:41197′1207
Ballerini P, Di Iorio P, Ciccarelli R et al (2002) Glial cells express multiple ATP binding cassette proteins which are involved in ATP release. Neuroreport 13:1789′792
Ballerini P, Di Iorio P, Ciccarelli R et al (2005) P2Y1 and cysteinyl leukotriene receptors mediate purine and cysteinyl leukotriene co-release in primary cultures of rat microglia. Int J Immunopathol Pharmacol 18:255′68
Ballerini P, Ciccarelli R, Caciagli F et al (2005) P2X7 receptor activation in rat brain cultured astrocytes increases the biosynthetic release of cysteinyl leukotrienes. Int J Immunopathol Pharmacol 18:417′30
Varma MR, Dixon CE, Jackson EK et al (2002) Administration of adenosine receptor agonists or antagonists after controlled cortical impact in mice: effects on function and histopathology. Brain Res 951:191′01
Meghji P, Tuttle JB, Rubio R (1989) Adenosine formation and release by embryonic chick neurons and glia in cell culture. J Neurochem 53:1852′860
Ciccarelli R, Ballerini P, Sabatino G et al (2001) Involvement of astrocytes in purine-mediated reparative processes in the brain. Int J Dev Neurosci 19:395′14
Ciccarelli R, Di Iorio P, Giuliani P et al (1999) Rat cultured astrocytes release guanine-based purines in basal conditions and after hypoxia/hypoglycemia. Glia 25:93′8
Traversa U, Bombi G, Di Iorio P et al (2002) Specific 3[H]-guanosine binding sites in rat brain membranes. Br J Pharmacol 135:969
Traversa U, Bombi G, Camaioni E et al (2003) Rat brain guanosine binding site. Biological studies and pseudo-receptor construction. Bioorg Med Chem 11:5417
Di Iorio P, Kleywegt S, Ciccarelli R et al (2002) Mechanisms of apoptosis induced by purine nucleosides in astrocytes. Glia 38:179
Ciccarelli R, Di Iorio P, D’Alimonte I et al (2000) Cultured astrocytes proliferation induced by extracellular guanosine involves endogenous adenosine and is raised by the co-presence of microglia. Glia 29:202
Rathbone MP, Middlemiss PJ, Gysberg IW et al (1999) Trophic effects of purines in neurons and glial cells. Prog Neurobiol 59:663
Pettifer KM, Kleywegt S, Bau CJ et al (2004) Guanosine protects SH-SY5Y cells against beta-amyloid-induced apoptosis. Neuroreport 15:833′36
Di Iorio P, Ballerini P, Traversa U et al (2004) The antiapoptotic effect of guanosine is mediated by the activation of the PI 3-kinase/AKT/PKB pathway in cultured rat astrocytes. Glia 46:356
Levison SW, McCarthy KD (1991) Characterization and partial purification of AIM: a plasma protein that induces rat cerebral type 2 astroglia from bipotential glial progenitors. J Neurochem 57:782′94
Demeester N, Castro G, Desrumaux C et al (2000) Characterization and functional studies of lipoproteins, lipid transfer proteins, and lecithin: cholesterol acyltransferase in CSF of normal individuals and patients with Alzheimer’s disease. J Lipid Res 41:963′74
Wagner BL, Valledor AF, Shao G et al (2003) Promoter-specific roles for liver X receptor/corepressor complexes in the regulation of ABCA1 and SREBP1 gene expression. Mol Cell Biol 23:5780′789
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248′54
Mori K, Yokoyama A, Yang L et al (2004) L-serine-mediated release of apolipoprotein E and lipids from microglial cells. Exp Neurol 185:220′31
Koldamova RP, Lefterov IM, Ikonomovic MD et al (2003) 22R-hydroxycholesterol and 9-cis-retinoic acid induce ATP-binding cassette transporter A1 expression and cholesterol efflux in brain cells and decrease amyloid beta secretion. J Biol Chem 278:13244′3256
Di Iorio P, Caciagli F, Giuliani P et al (2001) Purine nucleosides protect injured neurons and stimulate neuronal regeneration by intracellular and membrane receptor-mediated mechanisms. Drug Dev Res 52:303
Tomaselli B, Podhraski V, Heftberger V (2005) Purine nucleoside-mediated protection of chemical hypoxia-induced neuronal injuries involves p42/44 MAPK activation. Neurochem Int 46:513
Ping P, Zhang J, Huang S et al (1999) PKC-dependent activation of p46/p54 JNKs during ischemic preconditioning in conscious rabbits. Am J Physiol 277:H1771–H1785
Zhao Y, Zhang L, Longo LD (2005) PKC-induced ERK1/2 interactions and downstream effectors in ovine cerebral arteries. Am J Physiol Regul Integr Comp Physiol 289:R164–R171
Cignarella A, Engel T, von Eckardstein A et al (2005) Pharmacological regulation of cholesterol efflux in human monocyte-derived macrophages in the absence of exogenous cholesterol acceptors. Atherosclerosis 179:229′36
Mauch DH, Nagler K, Schumacher S et al (2001) CNS synaptogenesis promoted by glia-derived cholesterol. Science 294:1354′357
Pfrieger FW, Barres BA (1996) New views on synapse–glia interactions. Curr Opin Neurobiol 6:615′21
Liang Y, Lin S, Beyer TP et al (2004) A liver X receptor and retinoid X receptor heterodimer mediate apolipoprotein E expression, secretion and cholesterol homeostasis in astrocytes. J Neurochem 88:623′34
Rathbone MP, Middlemiss PJ, Gysbers JW et al (1992) Purine nucleosides and nucleotides stimulate proliferation of a wide range of cell types. In Vitro Cell Dev Biol 28A:529′36
Rathbone MP, Middlemiss P, Andrew C et al (1998) The trophic effects of purines and purinergic signaling in pathologic reactions of astrocytes. Alzheimer Dis Assoc Disord 12 [Suppl 2]:S36–S45
Caciagli F, Di Iorio P, Giuliani P et al (2000) The neuroprotective activity of guanosine involves the production of trophic factors and the outflow of purines from astrocytes. Drug Dev Res 50:32 R02-02
Frizzo ME, Lara DR, Dahm KC et al (2001) Activation of glutamate uptake by guanosine in primary astrocyte cultures. Neuroreport 12:879′81
Lara DR, Schmidt AP, Frizzo ME et al (2001) Effect of orally administered guanosine on seizures and death induced by glutamatergic agents. Brain Res 912:176′80
Tort AB, Mantese CE, dos Anjos GM et al (2004) Guanosine selectively inhibits locomotor stimulation induced by the NMDA antagonist dizocilpine. Behav Brain Res 154:417′22
Jiang S, Khan MI, Lu Y et al (2003) Guanosine promotes myelination and functional recovery in chronic spinal injury. Neuroreport 14:2463′467
See RH, Caday-Malcolm RA, Singaraja RR et al (2002) Protein kinase A site-specific phosphorylation regulates ATP-binding cassette A1 (ABCA1)-mediated phospholipid efflux. J Biol Chem 277:41835′1842
Kiss RS, Maric J, Marcel YL (2005) Lipid efflux in human and mouse macrophagic cells: evidence for differential regulation of phospholipid and cholesterol efflux. J Lipid Res 46:1877′887
Chambenoit O, Hamon Y, Marguet D et al (2001) Specific docking of apolipoprotein A-I at the cell surface requires a functional ABCA1 transporter. J Biol Chem 276:9955′960
Acknowledgement
This research was supported by grants from the Italian Ministero dell’Istruzione, dell’Università e della Ricerca (MIUR): PRIN 2003053992; Centre of Excellence on Ageing (CEA), University of Chieti-Pescara, Italy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Ballerini, P., Ciccarelli, R., Di Iorio, P. et al. Guanosine effect on cholesterol efflux and apolipoprotein E expression in astrocytes. Purinergic Signalling 2, 637–649 (2006). https://doi.org/10.1007/s11302-006-9011-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-006-9011-5