Abstract
Objectives
To test if the Community Complex Care Response Team (C3RT), a coordinated community response model, impacts the likelihood of abuse, neglect, and financial exploitation among at-risk community-dwelling older adults.
Methods
One hundred forty-six participants were randomly assigned to receive either the C3RT intervention (n = 74) or the standard practice (n = 72). Cox regression analyses were used to test whether the intervention delayed incidents of EANF victimization measured by when adult protective services opened an investigation, when the police recorded a victimization, and when a hospital admission took place.
Results
Assignment to the C3RT intervention program did not significantly delay incidents of EANF victimization indicator.
Conclusions
This C3RT approach did not produce the desired outcomes, though the project demonstrates that it is ethical and feasible to implement an RCT to test an intervention with vulnerable populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Elder abuse includes acts of physical assault, neglect, and financial exploitation (i.e., EANF) committed by an individual in a trusted relationship with an older adult, which have a high likelihood of causing harm (e.g., Hall et al., 2016). The United States National Elder Mistreatment Study, a representative sample of community-dwelling older adults, estimated past-year prevalence across the subtypes of EANF as follows: 5% emotional abuse, 2% physical abuse, 1% sexual abuse, 5% potential neglect, and 5% financial exploitation (Acierno et al., 2010). However, several subpopulations are likely at even greater risk of EANF, such as individuals with dementia, with studies finding EANF rates ranging from 49 among clinic samples to 74% produced by anonymous community samples (Pickering et al., 2020; Wiglesworth et al., 2010).
EANF often leads to a range of adverse, harmful outcomes, including emergency department utilization (Dong & Simon, 2013), nursing home placement (Lachs et al., 2002), depression (Acierno et al., 2018), increased mortality (Baker et al., 2009), and financial losses (MetLife Mature Market Institute, 2009). However, despite these adverse outcomes, options for community-based interventions are limited because researchers have yet to produce an EANF prevention model validated by a rigorous evaluation (Fearing et al., 2017; Pillemer et al., 2011).
What likely distinguishes EANF from other forms of family violence is the role of vulnerability, or the financial, physical, or emotional dependence of an older adult on others because of their diminished capacity for self-care (National Research Council., 2003). An older adult’s vulnerability is the basis of most state statutory definitions of EANF and the Centers for Disease Control and Prevention’s (CDC) uniform guideline definitions (Hall et al., 2016). Since vulnerability is a necessary condition for EANF, services and intervention programs that seek to increase an older adult’s independence and capacity for self-care are practical, if not a theoretically grounded approach for preventing and reducing EANF.
Since the reason for an older person’s vulnerability is often multifaceted and interlinked, crossing physical and mental health, substance use, social dependency, and economic and interpersonal problems (Storey, 2020), more than one service or program is likely needed to substantially mitigate or lessen the vulnerability. Within the context of intimate partner violence, the identification and management of risks by practitioners arose in the 2000s as a model to efficiently readdress the risk for IPV (Hart, 2008; Mann & Tosun, 2021; Pavlou & Scott, 2019; Storey et al., 2014), particularly when implemented within a CCR framework (Maxwell et al., 2020). And now, scholars are also promoting elder abuse risk management through a collaborative approach model (Fraga Dominguez et al., 2021; Storey, 2020). These efforts are also commonly described as providing “wraparound services.” These collaborative modalities seek to place their client at the center to identify their strengths and needs while facilitating access to community-based support and services. Unfortunately, in the context of violence prevention efforts, these “wraparound” programs remain largely untested (c.f., DePrince et al., 2011, 2019).
Accordingly, a novel coordinated case management model program entitled the Community Complex Care Response Team (C3RT) was developed through a grassroots community effort to reduce EANF. The program developers sought to mitigate older adults’ vulnerabilities to victimization by increasing their independence and capacity to live in their community safely. Their model aimed to align the mechanisms of service provisions across healthcare, emergency response, and home and community-based healthcare. The model relies on a broad-based, electronically linked group of community-based health and human service providers to identify, assess, coordinate, and deliver services to older adults. In contrast to the standard case management approach, which is passive by design, the C3RT model provides the means to proactively align services across allied sectors to increase the overall availability and use of preventative interventions and supportive services for vulnerable older adults. While the same community-based services are available to all participants regardless of group assignment, it is likely that participants assigned to the I&R model will not receive enough assistance due to the frustration and fatigue with seeking and navigating the services on their own (Greeson & Campbell, 2013).
To implement the C3RT model, the service partners share decision-making and exchange information through a coordinated case management system to better assess, plan for, and deliver a range of healthcare, social, and community services (Pickering et al., 2022). The shared decision-making and information exchange is facilitated by a shared electronic service record management system which all community partner agencies can access 24/7. Two interventionists at the local Area Agency on Aging (AAA), a patient navigator and a community health worker, completed the enrollment and assessment process. The patient navigator is responsible for the “behind the scenes” coordination and service enrollment. The community health worker completes an in-home needs assessment with the participant. This assessment focuses on the participant’s perceived needs related to their safety and independence. During this visit, the community health worker also seeks the participant’s consent to share their information among partner agencies documented on a uniform consent form. Together, the two interventionists create a service plan reflecting the participant’s wishes that focuses on immediate safety issues and structural deficits to safe long-term community-dwelling. The patient navigator completes extensive documentation in the system and then pushes out electronic referrals to other members of the C3RT coalition through the shared record management system. Members of the coalition can communicate about each participant and access their assessment data within this records management system (RMS). A range of services is available through local partners in the coalition, including services such as managed care, home-delivered meals, in-home assistance, home repair, and money management (Maxwell et al., 2022).
The service plan aims to mitigate a host of social determinants (e.g., food insecurity) that contribute to the participant’s vulnerability to victimization by focusing on supporting a participant’s independence and capacity for self-care to live safely in the community. This process of connecting participants to services to minimize vulnerability to victimization is why the C3RT protocol is an approach that falls under the now widely deployed coordinated community response (CCR) model used to address intimate partner violence (IPV) victims across communities. Supported by the Center for Disease Control and Prevention and the US Department of Justice, CCR are deployed throughout the USA and abroad to build a coordinated network of services to reduce and prevent IPV across a community (Klevens et al., 2008a). The 1984 US Attorney General’s Task Force on Family Violence report recommended that CCR be a critical DV intervention point. A decade later, the US Bureau of Justice Assistance funded eleven family violence demonstration programs to establish interagency coordinating committees (Bureau of Justice Assistance, 1993; Harrell et al., 1988). Since the Violence Against Women Act’s inception, the US Department of Justice has also required communities to use a CCR approach to receive financial support for their local IPV prevention programs.
Although a standardized protocol for implementing a CCR does not exists (Ranjan & Dmello, 2022), CCR are often described as involving many government agencies and non-governmental organizations (NGO) from across a community, such as law enforcement, social and health care system provides, and vocational programs. They usually form a coalition to develop standard policies, identify service gaps, and build partnerships between service providers to facilitate and coordinate responses. This network of agencies and NGO is designed to provide community members with resources they lack more comprehensively and efficiently to prevent violence and lessen the consequence of past violence. These coalitions are often practitioner-led, sometimes chaired by a government official such as a judge or prosecutor or by a representative of an NGO. Academics often link this design and effort to the ecological systems theory. Indeed, it was this conceptualization that best describes the CCR that developed and implemented the C3RT program tested in this study (Pickering et al., 2022).
Some CCR versions, such as the Family Justice Center model, seek to provide a single-point-of-entry system at one physical location where victims gain access to a range of services through a network of community-based health and human service partners (Hoyle & Palmer, 2014). Like the IPV context, Maxwell et al. (2022) demonstrated that the C3RT model significantly increased interagency communications and services across a broad range of multidisciplinary services compared to standard practice. More specifically, C3RT participants received 44% more provider communications than those assigned to the usual care protocol. Among those accepting services, C3RT participants received more than three times as many types of services as did the participants in the standard care group. Maxwell et al. (2022)’s post hoc analyses also found that, across the available services, a more significant proportion of C3RT participants received referrals to ten types of multisector services than participants receiving standard care. The most substantial difference was found for the Meals on Wheels program (26 vs. 8%). Finally, Maxwell et al. (2022) found that almost three times more financial support was spent on services for the C3RT participants than those assigned to standard care. Therefore, the C3RT model appears to function as the developers intended because it produced more linkages and services for the consenting participants.
However, while researchers have shown that CCR increases access to services (Armstead et al., 2017; Maxwell et al., 2022), researchers to date have either not yet tested whether individual CCR components (Shorey et al., 2014) or their integration prevents or reduces victimization rates. The most extensive assessment, in terms of sample size and the number of participating CCR, of the impact of CCR to date found that they do not affect knowledge, beliefs, or attitudes of IPV, knowledge, and use of available IPV services, nor the risk of exposure to IPV (Klevens et al., 2008b; Post et al., 2010). Other similarly focused studies have also not found that the CCR approach impacts victimization rates (Garner & Maxwell, 2008). But for DePrince et al. (2011)’s and DePrince et al. (2019)’s single site randomized clinical trials (RCT), the CCR assessments have not utilized an experimental design to test for CCR impacts. Thus, to the extent one existed in these studies, their comparison groups were not equivalent, which likely attenuated their effects.
There are several key differences between the IPV-focused CCR model and the C3RT model that we anticipate will produce more positive outcomes. The first difference is that C3RT emphasizes broad access to information about a participant’s unmet needs and service requirements among providers with the participant’s consent (Pickering et al., 2022).Footnote 1 This attribute of the C3RT model is accomplished by creating an Internet-based RMS that “pushes” clients’ information to service providers and permits service providers to access the client’s records to assess whether their program can aid the client. It also allows each service provider to exchange information to refer their clients if they cannot help or their needs are still not met. A second key difference was the development of a community-wide uniform shared consent form. This consent form explained that if permission is granted, information related to planning or providing services would be shared with partner agencies (all were listed) and contained standard language associated with the Federal Health Insurance Portability and Accountability Act (HIPAA) and state mental health code disclosure. As part of this form, the participants who consented to services have the option of not sharing their information with specific organizations. If they choose to exclude an organization, the RMS blocks that organization from accessing the client’s records.
While prior research has documented the development and implementation of this C3RT model (i.e., Maxwell et al., 2022; Pickering et al., 2022), the purpose of this study is to provide an assessment of whether this C3RT model has prevented EANF victimization among community-dwelling older adults as measured by law enforcement and adult protective service (APS) records detailing their victimization and emergency/inpatient admissions. To reach this objective, we use an experimental design to test whether a well-implemented CCR impacted post-assignment victimization rates, albeit with a narrower focus on addressing elder abuse rates, one of just several forms of domestic violence targeted by the CCR approach. We hypothesize that participants assigned to the C3RT will have an increased time to first victimization (i.e., a reduced hazard rate) compared to those assigned to standard practice. We also hypothesize that C3RT participants who experienced EANF before the random assignment will also have an increased time to subsequent revictimization. Lastly, an exploratory analysis evaluates whether C3RT group assignments have a preventative effect on self-neglect reported to APS.
Methods
The university’s IRB approved all study procedures. Maxwell et al. (2022) provide more details related to staff training on human subjects’ protection. A pragmatic RCT was implemented to test how the C3RT model performs under normal operating circumstances within a typical practice environment (Patsopoulos, 2011). An AAA served as the hub for implementing the C3RT intervention. The USA’s AAA are a mix of public or private non-profit agencies designated by a state to address the needs and concerns of all older persons within a geographic area (e.g., a city, a county, or a multi-county district). They offer a range of services to help older adults who want to remain in their homes.
Several community partners who frequently interact with community-dwelling older adults, including law enforcement, emergency service providers, and hospital discharge planners, were recruited to refer potential clients to the AAA for the C3RT program. The C3RT staff trained the staff within each of the targeted county’s referral agencies to identify applicable clients and make referrals to the AAA through their local electronic referral system or by directly calling the intake officer.Footnote 2 When referral rates were not meeting their anticipated level, the program staff met with the agency’s executive management staff and often retrained the referral staff during their roll calls.
Sample and setting
C3RT implementation was limited to the service area of the municipal law enforcement agency, which covers a suburban city and outlying rural municipalities which rely on them for police services. The area’s population in 2021 was about 130,000 residents. About 75% of the population is White, and less than 10% are Hispanic or Latino. This geographic limitation was necessary because this law enforcement agency’s record system captured one of the three primary outcomes. It was also limited to this service area to help manage the client count, which the AAA staff believed would likely exceed 300 over 18 months. Since the outcomes came from systems-level data not limited to time, there was no a priori determined sample size to guide recruitment.
The partner AAA relies on their state’s Department of Health and Human Services rules and functionality to determine eligibility for reimbursable services. As such, these criteria served as this study’s eligibility criteria. Service eligibility criteria include the presence of one of the following: suspected EANF (practitioner judgment), or 2 + complex chronic conditions such as physical developmental disability, Alzheimer’s disease or other dementia, terminal condition with death expected within a year, severe persistent mental illness, homeless, foreclosure, financial issues, and isolation/no informal supports. Because the AAA was the lead agency and intake site for the experimental C3RT model, they also delivered the standard practice model for the control group. The standard practice implemented the Information and Referral Assistance (I&R) model. I&R is the typical practice and a core competency of all AAA across the nation. The I&R connects older adults to services by providing information on community service providers listed within an established resource directory to those seeking and asking for assistance (Alliance of Information & Referral Systems, 2022; National Information and Referral (I&R) Support Center; US Aging).
Randomization
After enrollment and consent to receive services, participants were randomized in a 1:1 allocation to receive either the C3RT model or the standard practice (I&R) model. What was randomized was the service delivery model. The IRB did not require consent for the randomization step since all services remained available to all willing participants. The research team generated a randomization key using a random-digit table, and then they created a sealed blue diamond pattern and numbered envelopes for the interventionists to open. The envelope included a form that indicated the participant’s group assignment. Participants referred again to the AAA were re-assigned to their original group rather than re-randomized. As this was a pragmatic trial design, complete blinding of group assignment among the AAA staff was not possible, but our system to identify misassignments would “tag” an instance where the assignment was manipulated or there was treatment “crossover.”
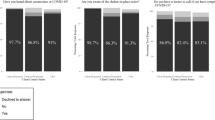
Between January 1, 2017, and May 5, 2019, 159 individuals were referred to the program. After determining the referral’s eligibility and interest in receiving services, the interventionists enrolled 146 participants. Figure 1 provides the consort diagram. The most common exclusion reason noted was that the older adult was not interested in receiving services. Overall, the study’s sample was female (59%) and non-Hispanic whites (87%) with an average age of 77 years old. There were no significant differences between the two randomly assigned groups based on demographics. In the 90 days before randomization, 3% of the participants had contact with law enforcement, and 8% had at least one opened APS case. There was a significant difference between the I&R control group and the C3RT intervention group in the proportion of participants with two or more hospital admissions in the prior 90 days, with the I&R group having more admissions (see Table 1). The hospital discharge planners were the largest source of referral to the program, representing 92% of enrolled participants; as such, most participants (86%) had at least one hospital admission during the 90 days before enrollment.
Outcomes
EANF was measured as recorded incidents with law enforcement and APS. Incidents that involved the participants as the named victim in the incident report were used for the law enforcement recorded outcomes. The incidents could range from property offenses such as damage, fraud, or theft to violent crimes such as assault, robbery, and murder. The incidents were identified by matching the participant’s name and date of their birth to the county’s master list of people known to law enforcement and emergency services. Incidents by those unknown or strangers were included because for property crimes, many victims did not know who the offender was at the time they reported the offense. The relationship of the victim/offender is also not a requirement of the state’s statute on EANF, where the project was based.
For APS, only instances where APS opened a case to investigate were included, thus indicating that the circumstances met the state’s threshold of EANF. Opened cases were used over substantiated cases as the outcome measure because there are many reasons a claim is not substantiated that are not related to whether EANF occurred (e.g., an older adult does not consent to the APS investigation). Opened APS cases for EANF were included regardless of cause or comorbidity (i.e., one type or multiple), including co-morbid self-neglect because it was often reported as co-occurring with EANF victimization. Data on APS-recorded incidents involving the project participants were provided without their identifiers by APS through a data broker.
Given the increased risk of emergency services use resulting from EANF (Lachs et al., 2002), it was included as a secondary outcome. Emergency services were intended to include contacts with the local emergency department. However, the way these system data were provided, it was impossible to distinguish if inpatient admissions resulted from an emergency department visit, thus potentially underestimating the outcome. As such, the outcome measure was revised to include hospital admissions to either the emergency department or inpatient since most inpatient admissions are the result of an emergency department visit. The research team provided a list of participants to match the hospital’s records to obtain these data. The research team was provided data (e.g., ICD10) from the hospital for the 44 participants that provided a waiver of HIPAA to use their data for research purposes.
Analysis plan
Survival analysis was used to test the hypothesis that the C3RT extended the time-to-first victimization. A survival function estimates the probability that a subject will survive past time t. We used Cox semi-parametric multivariate regression analyses to determine if there are significant differences in the hazard rate (e.g., the event rate at time t conditional on survival until time t) between the C3RT group and the standard practice group. Because the analysis relies on survival analyses and uses administrative system data to capture the outcomes, follow-up was not limited to a specific time frame. Our data analyses plan followed an intent-to-treat approach (Gupta, 2011). The expected time until the next applicable EANF incident (APS, law enforcement) and the subsequent hospital encounter were modeled separately. We also included covariates of the participants’ gender and the frequency of previous service interactions (e.g., victimization known to APS or the police) during the 90 days before enrollment. These later tests were added to assess whether C3RT impacts participants differently if, for example, they had already experienced an adverse event.
Results
The average length of the follow-up observation period varied by the data source. The average observation period across all outcome measures was 422 days (SD 204 days). By group assignment, the observation period for the outcomes was only slightly more extended for those in C3RT (436 days, SD 187 days) than for those assigned to the I&R control group (408 days, SD 220 days). Among the 33 APS complaints following enrollment, 46% included self-neglect, and 45% involved a neglect allegation. There were also allegations of physical (24%) and emotional (15%) abuse and financial exploitation (18%). Among the 17 crime incidents recorded by law enforcement after enrollment, most participants reported property victimization (59%), followed by fraud (24%) and violence (18%). Most of the offenders were unknown (65%), followed by family members (29%) and care providers (6%). After enrollment, most hospital admissions were for the emergency department (61%) rather than inpatient (39%).
The findings produced by a series of Cox regressions do not support the primary hypothesis that participation in C3RT, as compared to standard practice, reduces the odds of victimization across any of the adverse outcome measures (Table 2, model 1 and 2). While two of the three hazard ratios are negative, suggesting that those assigned to C3RT had fewer APS cases and hospital admissions, neither reached statistical significance (e.g., p-value < 0.05). Likewise, there was no statistically significant difference in outcome rates by the participant’s sex. However, with two of the three odds ratios near or larger than two, these findings appear clinically important because they show that males are experiencing disproportionally more negative outcomes than females. The number of prior adverse outcomes within the 90 days before the assignment is the one factor that consistently predicted a greater odds of a future adverse outcome and was statistically significant in two of the three analyses. In one of these instances (i.e., the number of prior APS investigations), the level of risk increased by a factor of four. For another measure (i.e., prior offense recorded by the police), the level of risk rose by nearly a factor of six for each prior incident.
For the second hypothesis, the findings also do not support that participation in C3RT significantly decreased the risk of re-victimization for participants measured as opened APS cases or hospital re-admissions among those who had an incident before randomization (Table 2, model 3). Furthermore, having more opened cases in the last 90 days significantly increased the risk of an opened APS case after enrollment (HR 4.31, CI 20.3–9.11, p < 0.05). Having one or more hospital admissions in the prior 90 days also significantly increased the risk of subsequent hospital admission after group assignment (HR 1.41, CI 1.21–1.64, p < 0.05). Thus, the past is an essential predictor of the future. With only 18 post-assignment crime offenses, the outcomes analysis based upon law enforcement data was too sparse for the third model to converge; therefore, these results are not reported. There were no significant prevention effects for onset or repeat self-neglect (APS cases) among those in C3RT compared to standard practice for the exploratory hypothesis.
Discussion
DePrince et al. (2012), DePrince et al. (2019), and Maxwell et al. (2022) RCT-based studies all demonstrated significant, intermediate process benefits among CCR-assigned clients. In other words, CCR clients tend to become more connected and receive more services than those served by more traditional approaches. Unfortunately, this paper’s analysis of impacts shows that the C3RT model did not prevent more EANF than the I&R model as measured by three EANF outcomes: victimization recorded by law enforcement, opened APS case, and hospital admission. While this conclusion is disappointing, like DePrince et al. (2011) and DePrince et al. (2019), this study contributes to the field because it further demonstrates that communities can safely implement a rigorous randomized control trial among vulnerable populations when they compare a new service delivery model to an existing practice. This study overcame the dilemma resulting from some participants not receiving services through careful design, which others have cited as a methodological problem for RCT within the EANF field (Teresi et al., 2016).
Along with DePrince et al. (2019), this study also addresses the “near absence of empirically tested elder mistreatment interventions” (Pillemer et al., 2015). Unfortunately, the lack of a protective effect for EANF among C3RT participants places this study alongside other rigorous evaluations of CCR for IPV (e.g., DePrince et al., 2011; Post et al., 2010) and elder abuse (DePrince et al., 2019). Though there is enthusiasm in the field for multidisciplinary collaborative-based approaches to EANF (Teresi et al., 2016), the findings suggest that the services offered through these models each need rigorous assessments before moving towards multi-component interventions. While others have found support for multidisciplinary collaborative-based approaches, these studies only evaluated the reduction in EANF risk (Mariam et al., 2015; Rizzo et al., 2014). Instead, this study focused on assessing for the prevention of onset and reoccurrence of EANF victimization. Unfortunately, the evidence suggests that more work is needed to identify specific programs that help before pooling them through a multi-component EANF intervention. A similar conclusion was drawn about the state of the science for CCR in domestic violence regarding the need to identify specific individual program components that can produce positive outcomes (Johnson & Stylianou, 2020).
Complex adaptive systems theory provides a helpful framework for understanding the impact of community-level programming (Neely, 2015). This theory emphasizes the non-linear nature between risks, causes, and effects. Due to the dynamic nature of systems, unintended and complex consequences can occur when interventions are introduced (e.g., Hovmand et al., 2004, 2009; Salazar et al., 2007). As applied to this study, previous evaluations have shown support that the mechanisms of the C3RT intervention are as hypothesized, as C3RT successfully produces more service referrals than standard practice (Maxwell et al., 2022). As such, C3RT participants may have more “trusted others” in their lives providing needed services. While this was hypothesized to reduce vulnerability, it may have increased risk by introducing more potential perpetrators. Alternatively, by introducing more “trusted others,” the program may have decreased the overall risk of victimization but inadvertently increased reporting of EANF by capable guardians. Future studies should include victim interviews to disentangle the dynamic and unintended effects of the intervention model.Footnote 3
This study had many strengths, including a pragmatic RCT design and multiple outcome measures. Furthermore, the use of administrative data provided an independent and validated measure of the outcomes (e.g., the APS has rules to ascertain whether to open a case). There is also no missing data because the study did not rely on participant respondents, which permitted a more extended observation period. However, there are several study limitations that future research can address. For example, because the study relied on administrative data, it is possible that victimizations were undercounted, particularly among law enforcement and APS agencies. However, there is no evidence in this study or reported by other scholars to conclude that reporting victimization to administrative agencies would create bias across the two treatment groups. Besides capturing more victimizations, participant interviews would have permitted us to collect more detailed information about the nature of the relationship (when it was known) between the participant and the offender. This additional information could have helped us narrow the impact analysis to just incidents involving “trusted” offenders, which would align with research definitions of EANF. However, it should be noted that this project’s jurisdiction does not limit EANF to only those cases that involve “trusted” offenders, which is why this was not a criterion in the primary analysis. In addition, while we used mechanisms to prevent “misassignment” and “flag” instances of misassignment, a staff member could delay an intake until they knew that the next random assignment was to the C3RT group. We had reminded the intake staff several times that it would likely make it more difficult to find a positive impact from the C3RT program if they took such a step because they felt a person would benefit from C3RT. Fortunately, we do not believe misassignment often happened, if at all, because we did not find significant differences between the two intervention groups on all but one pre-assignment measure.
The C3RT may have failed despite targeting known risk factors because the body of knowledge within the EANF field is not yet sufficiently advanced to design community-based intervention models. While there has been an abundance of observational research describing risk factors related to EANF (Pillemer et al., 2016), there is a lack of theory linking these factors to the mechanisms driving EANF. Additionally, the field lacks longitudinal research assessing the causal relationship between risk factors and subsequent victimization. Nevertheless, this study and others have used these “known” risk factors both as intervention targets and intervention outcomes (Mariam et al., 2015; Rizzo et al., 2014). While the lack of rigorously designed intervention studies is cited as a barrier to the progression of the public health response to EANF (Pillemer et al., 2015), the field will remain stymied even with more rigorous intervention designs without first advancing our understanding of the social and behavioral determinants of EANF.
Notes
The model developers discovered this difference when the local domestic violence shelter partner withdrew from the county’s collaboration team because their leadership felt that the Federal Violence Against Women Act’s client privacy requirements prevented them from sharing information with other community members. This interagency electronic information access and sharing of clients is one of the two keys to ensuring clients have access to what their county provides.
See https://acl.gov/programs/aging-and-disability-networks/area-agencies-aging for a description of how AAAs are managed by U.S. state governments.
Based upon the initial results from the sample reported in this paper, our practitioner partners received additional financial support to continue the evaluation to implement a longitudinal victim interview protocol that mimicked those that have been implemented for other similar evaluations (Davis, Maxwell & Taylor 2006). Unfortunately, this component of the supplementary project was terminated early because we were not sufficiently successful at recruiting participants even though we had developed and tested our interview process (Pickering and Maxwell 2018).
References
Acierno, R., Hernandez, M. A., Amstadter, A. B., Resnick, H. S., Steve, K., Muzzy, W., & Kilpatrick, D. G. (2010). Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: The National Elder Mistreatment Study. American Journal of Public Health, 100(2), 292–297. https://doi.org/10.2105/ajph.2009.163089
Acierno, R., Watkins, J., Hernandez-Tejada, M. A., Muzzy, W., Frook, G., Steedley, M., & Anetzberger, G. (2018). Mental health correlates of financial mistreatment in the National Elder Mistreatment Study Wave II. Journal of Aging and Health, 31(7), 1196–1211. https://doi.org/10.1177/0898264318767037
Alliance of Information and Referral Systems. (2022). How I&R Works. Alliance of Information and Referral Systems,. Retrieved 2022/05/15 from https://www.airs.org/i4a/pages/index.cfm?pageid=3500
Armstead, T. L., Rambo, K., Kearns, M., Jones, K. M., Dills, J., & Brown, P. (2017). CDC’s DELTA FOCUS Program: Identifying promising primary prevention strategies for intimate partner violence. Journal of Women’s Health, 26(1), 9–12. https://doi.org/10.1089/jwh.2016.6251
Baker, M. W., LaCroix, A. Z., Wu, C. Y., Cochrane, B. B., Wallace, R., & Woods, N. F. (2009). Mortality risk associated with physical and verbal abuse in women aged 50 to 79. Journal of the American Geriatrics Society, 57(10), 1799–1809. https://doi.org/10.1111/j.1532-5415.2009.02429.x
Bureau of Justice Assistance. (1993). The social impact of the national citizens’ crime prevention campaign, in Focus on What Works. U.S. Department of Justice. https://www.ojp.gov/pdffiles1/Digitization/144533NCJRS.pdf
Davis, R. C., Maxwell, C. D., & Taylor, B. G. (2006). Preventing repeat incidents of family violence: Analysis of data from three field experiments. Journal of Experimental Criminology, 2(2), 183–210. https://doi.org/10.1007/s11292-006-9002-0
DePrince, A. P., Belknap, J., & Gover, A. R. (2011). Effectiveness of coordinated outreach in intimate partner violence cases: A randomized longitudinal design [Final Report]. U. o. Denver. https://www.ncjrs.gov/pdffiles1/nij/grants/238480.pdf
DePrince, A. P., Belknap, J., Labus, J. S., Buckingham, S. E., & Gover, A. R. (2012). The impact of victim-focused outreach on criminal legal system outcomes following police-reported intimate partner abuse. Violence against Women, 18(8), 861–881. https://doi.org/10.1177/1077801212456523
DePrince, A. P., Hasche, L. K., Olomi, J. M., Wright, N. M., & Labus, J. (2019). A randomized-control trial testing the impact of a multidisciplinary team response to older adult maltreatment. Journal of Elder Abuse & Neglect, 31(4–5), 307–324. https://doi.org/10.1080/08946566.2019.1682097
Dong, X., & Simon, M. A. (2013). Association between elder abuse and use of ED: Findings from the Chicago Health and Aging Project. The American Journal of Emergency Medicine, 31(4), 693–698. https://doi.org/10.1016/j.ajem.2012.12.028
Fearing, G., Sheppard, C. L., McDonald, L., Beaulieu, M., & Hitzig, S. L. (2017). A systematic review on community-based interventions for elder abuse and neglect [Systematic Review]. Journal of Elder Abuse & Neglect, 29(2–3), 102–133. https://doi.org/10.1080/08946566.2017.1308286
Fraga Dominguez, S., Ozguler, B., Storey, J. E., & Rogers, M. (2021). Elder abuse vulnerability and risk factors: Is financial abuse different from other subtypes? Journal of Applied Gerontology, 41(4), 928–939. https://doi.org/10.1177/07334648211036402
Garner, J. H., & Maxwell, C. D. (2008). Coordinated community responses to intimate partner violence in the 20th and 21st centuries [Policy Essay]. Criminology & Public Policy, 7(4), 301–311. https://doi.org/10.1111/j.1745-9133.2008.00525.x
Greeson, M. R., & Campbell, R. (2013). Sexual Assault Response Teams (SARTs). Trauma, Violence, & Abuse, 14(2), 83–95. https://doi.org/10.1177/1524838012470035
Gupta, S. (2011). Intention-to-treat concept: A review [Biostatistics]. Perspectives in Clinical Research, 2(3), 109–112. https://doi.org/10.4103/2229-3485.83221
Hall, J., Karch, D. L., & Crosby, A. E. (2016). Elder abuse surveillance: Uniform definitions and recommended core data elements for use in elder abuse surveillance. Center for Disease Control and Prevention.
Harrell, A. V., Roehl, J. A., & Kapsak, K. A. (1988). Family violence intervention demonstration programs evaluation: Case studies. Institute for Social Analysis.
Hart, S. D. (2008). Preventing violence: The role of risk assessment and management. In A. C. Baldry & F. W. Winkel (Eds.), Intimate partner violence prevention and intervention: The risk assessment and management approach (pp. 7–18). Nova Science Publihser, Inc. https://books.google.com/books?id=Ni2cpah07f4C&lpg=PP1&pg=PP1#v=onepage&q&f=false
Hovmand, P. S., Ford, D. N., Flom, I., & Kyriakakis, S. (2009). Victims arrested for domestic violence: Unintended consequences of arrest policies. System Dynamics Review, 25(3), 161–181. https://doi.org/10.1002/sdr.418
Hovmand, P. S., Post, L. A., & Maxwell, C. D. (2004, January). Too busy to hold assailants accountable? Domestic violence caseload pressures in a rural prosecutor’s office. The Annual Conference of the Society for Social Work and Research, New Orleans, LA.
Hoyle, C., & Palmer, N. (2014). Family justice centers: A model for empowerment? International Review of Victimology, 20(2), 191–210. https://doi.org/10.1177/0269758014521738
Johnson, L., & Stylianou, A. M. (2020). Coordinated community responses to domestic violence: A systematic review of the literature [Systematic Review]. Trauma, Violence, & Abuse, 152483802095798https://doi.org/10.1177/1524838020957984
Klevens, J., Baker, C. K., Shelley, G. A., & Ingram, E. M. (2008). Exploring the links between components of coordinated community responses and their impact on contact with intimate partner violence services. Violence against Women, 14(3), 346–358. https://doi.org/10.1177/1077801207313968
Klevens, J., Baker, C. K., Shelley, G. A., & Ingram, I. (2008b). Exploring the links between components of coordinated community responses and their impact on contact with intimate partner violence services. Violence Against Women, 14(3), 346–358. 10.1177%2F1077801207313968
Lachs, M. S., Williams, C. S., O’Brien, S., & Pillemer, K. A. (2002). Adult protective service use and nursing home placement. The Gerontologist, 42(6), 734–739. https://doi.org/10.1093/geront/42.6.734
Mann, L., & Tosun, Z. (2021). Assessing and managing risks in cases of violence against women and domestic violence: Strengthening risk assessments, the risk-management system and inter-agency coordination in Turkey. C. o. Europe. https://rm.coe.int/trk-2021-assessing-and-managing-risks-in-cases-of-vaw-and-domestic-vio/1680a2a7cb
Mariam, L. M., McClure, R., Robinson, J. B., & Yang, J. A. (2015). Eliciting change in at-risk elders (ecare): Evaluation of an elder abuse intervention program. Journal of Elder Abuse & Neglect, 27(1), 19–33. https://doi.org/10.1080/08946566.2013.867241
Maxwell, C. D., Rodgers, K. R., & Pickering, C. E. Z. (2022). Pragmatic randomized control trial of a coordinated community response: Increasing service access for at-risk older adults. Journal of Forensic Nursing, Article JFN-21–002R1. https://doi.org/10.1097/JFN.0000000000000352.
Maxwell, C. D., Sullivan, T. P., Backes, B. L., & Kaufman, J. S. (2020). New approaches to policing high risk intimate partner victims and offenders. NIJ Journal, 282. https://nij.ojp.gov/topics/articles/new-approaches-policing-high-risk-intimate-partner-victims-and-offenders
MetLife Mature Market Institute. (2009). Broken trust: Elders, family & finances. MetLife Mature Market Institute; National Committee for the Prevention of Elder Abuse, Center for Gerontology at Virginia Polytechnic Institute and the State University. https://www.giaging.org/documents/mmi-study-broken-trust-elders-family-finances.pdf
National Information and Referral (I&R) Support Center. What is I&R/A? ADvancing States. Retrieved 2022/05/18 from http://www.advancingstates.org/initiatives/information-and-referralassistance/what-ira
National Research Council. (2003). Concepts, definitions, and guidelines for measurement. In R. J. Bonnie & R. B. Wallace (Eds.), Elder mistreatment: Abuse, neglect, and exploitation in an aging america (pp. 34–59). The National Academies Press.
Neely, K. (2015). Complex adaptive systems as a valid framework for understanding community level development. Development in Practice, 25(6), 785–797. https://doi.org/10.1080/09614524.2015.1060949
Patsopoulos, N. A. (2011). A pragmatic view on pragmatic trials. Dialogues Clinical Neuroscience, 13(2), 217–224. https://doi.org/10.31887/DCNS.2011.13.2/npatsopoulos
Pavlou, S., & Scott, M. (2019). A guide to risk assessment and risk management of intimate partner violence against women for police. In Gender-based violence (pp. 68). Vilnius, Lithuania, EU: Office of the European Union.
Pickering, C. E. Z., & Maxwell, C. D. (2018). Recruitment, retention and data collection with victims of elder abuse identified from police reports. Journal of Elder Abuse & Neglect, 30(5), 333–353. https://doi.org/10.1080/08946566.2018.1514342
Pickering, C. E. Z., Maxwell, C. D., Tato, R., Fales, K., & Hogoboom, B. (2022). Development and implementation of a coordinated community response to address elder abuse and neglect. Journal of Forensic Nursing, Article JFN-21–003R1. https://doi.org/10.1097/JFN.0000000000000378
Pickering, C. E. Z., Yefimova, M., Maxwell, C., Puga, F., & Sullivan, T. (2020). Daily context for abusive and neglectful behavior in family caregiving for dementia. The Gerontologist, 60(3), 483–493. https://doi.org/10.1093/geront/gnz110
Pillemer, K., Breckman, R., Sweeney, C. D., Brownell, P., Fulmer, T., Berman, J., Brown, E., Laureano, E., & Lachs, M. S. (2011). Practitioners’ views on elder mistreatment research priorities: Recommendations from a research-to-practice consensus conference. Journal of Elder Abuse & Neglect, 23(2), 115–126. https://doi.org/10.1080/08946566.2011.558777
Pillemer, K., Burnes, D., Riffin, C., & Lachs, M. S. (2016). Elder abuse: Global situation, risk factors, and prevention strategies. The Gerontologist, 56(Suppl_2), S194-S205. https://doi.org/10.1093/geront/gnw004
Pillemer, K., Connolly, M.-T., Breckman, R., Spreng, N., & Lachs, M. S. (2015). Elder mistreatment: Priorities for consideration by the White House Conference on Aging. The Gerontologist, 55(2), 320–327. https://doi.org/10.1093/geront/gnu180
Post, L. A., Klevens, J., Maxwell, C. D., Shelley, G. A., & Ingram, E. (2010). An examination of whether coordinated community responses affect intimate partner violence. Journal of Interpersonal Violence, 25(1), 75–93. https://doi.org/10.1177/0886260508329125
Ranjan, S., & Dmello, J. R. (2022). Proposing a unified framework for coordinated community response. Violence against Women, 28(8), 1873–1889. https://doi.org/10.1177/10778012221086009
Rizzo, V. M., Burnes, D., & Chalfy, A. (2014). A systematic evaluation of a multidisciplinary social work–lawyer elder mistreatment intervention model. Journal of Elder Abuse & Neglect, 27(1), 1–18. https://doi.org/10.1080/08946566.2013.792104
Salazar, L. F., Emshoff, J. G., Baker, C. K., & Crowley, T. (2007). Examining the behavior of a system: An outcome evaluation of a coordinated community response to domestic violence. Journal of Family Violence, 22(7), 631–641. https://doi.org/10.1007/s10896-007-9116-9
Shorey, R. C., Tirone, V., & Stuart, G. L. (2014). Coordinated community response components for victims of intimate partner violence: A review of the literature. Aggression and Violent Behavior, 19(4), 363–371. https://doi.org/10.1016/j.avb.2014.06.001
Storey, J. E. (2020). Risk factors for elder abuse and neglect: A review of the literature. Aggression and Violent Behavior, 50, 101339. https://doi.org/10.1016/j.avb.2019.101339
Storey, J. E., Kropp, P. R., Hart, S. D., Belfrage, H., & Strand, S. (2014). Assessment and management of risk for intimate partner violence by police officers using the brief spousal assault form for the evaluation of risk. Criminal Justice and Behavior, 41(2), 256–271. https://doi.org/10.1177/0093854813503960
Teresi, J. A., Burnes, D., Skowron, E. A., Dutton, M. A., Mosqueda, L., Lachs, M. S., & Pillemer, K. (2016). State of the science on prevention of elder abuse and lessons learned from child abuse and domestic violence prevention: Toward a conceptual framework for research. Journal of Elder Abuse & Neglect, 28(4–5), 263–300. https://doi.org/10.1080/08946566.2016.1240053
US Aging. Information and Referral/Assistance. US Aging. Retrieved 2022/05/18 from https://www.usaging.org/content.asp?contentid=1281
Wiglesworth, A., Mosqueda, L., Mulnard, R., Liao, S., Gibbs, L., & Fitzgerald, W. (2010). Screening for abuse and neglect of people with dementia. Journal of the American Geriatrics Society, 58(3), 493–500. https://doi.org/10.1111/j.1532-5415.2010.02737.x
Acknowledgements
We wish to thank the community partners for their dedicated support to addressing EANF and the C3RT model, including the Michigan Department of Health and Human Services, Adult Protective Services.
Funding
This project was funded in part by Robert Wood Johnson Foundation (Grant No 73692) and Michigan State University’s School of Criminal Justice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The findings and conclusions presented represent the authors’ views and do not necessarily represent the views of the Robert Wood Johnson Foundation, Michigan State University, or the University of Alabama at Birmingham.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maxwell, C.D., Almanza, K.R. & Pickering, C.E.Z. Coordinated community response to prevent elder abuse, neglect, and financial exploitation: randomized control trial. J Exp Criminol 19, 1067–1083 (2023). https://doi.org/10.1007/s11292-022-09521-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11292-022-09521-1