Abstract
Objectives
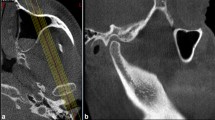
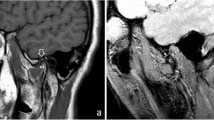
The aim of this study was to evaluate, using cone-beam computed tomography (CBCT), the relationship of persistent foramen tympanicum (PFT) with degenerative changes in the temporomandibular joint (TMJ) and the presence of pneumatized glenoid fossae and articular eminences.
Method
Two experienced oral and maxillofacial radiologists evaluated 510 CBCT scans, from which 94 patients were divided into two groups: G1—patients with PFT and G2—control group. The location of the PFT, presence, or absence of degenerative TMJ changes and morphology were evaluated. Similarly, all images were evaluated for the presence of pneumatized articular eminence and glenoid fossa. The Chi-square test and Fisher’s Exact test were used for the categorical variables. A multinomial logistic regression model was performed for subgroup analysis. To assess the estimation-chance occurrence of TMJ alterations the Odds Ratio analysis was used.
Results
Statistically significant results were found for erosion, planning, and subchondral cyst. Regarding TMJ morphology, significant results were found for: round, flat, and others. Moreover, it was possible to observe that patients who had the PFT were approximately 48 times more likely to manifest TMJ alterations and approximately 3 times more likely to manifest articular eminence pneumatization.
Conclusion
Since individuals who have FTP have a greater chance of having TMJ and PEA changes, it is important for the dental radiologist to be aware of these signs in CBCT scans for a correct diagnosis.
Trial registration number
CAAE: 34328214.3.0000.0104 (11/30/2014).



Similar content being viewed by others
References
Lacout A, Marsot-Dupuch K, Smoker WR, Lasjaunias P. Foramen tympanicum or foramen of Huschke: pathologic cases and anatomic CT study. Am J Neuroradiol. 2005;26:1317–23.
Akcam T, Hidir Y, Ilica AT, Kilic E, Sencimen M. Temporomandibular joint herniation into the external ear canal through foramen of Huschke. Auris Nasus Larynx. 2011;38:646–9.
Hashimoto T, Ojiri H, Kawai Y. The foramen of Huschke: age and gender specific features after childhood. Int J Oral Maxillofac Surg. 2011;40:743–6.
Ertugrul S, Keskin NK. Relationship of age to foramen of Huschke and investigation of the development of spontaneous temporomandibular joint herniation. Int J Oral Maxillofac Surg. 2019;48:534–9.
Williams PL, Warwick R, Dyson M, Bannister LH. GRAY Anatomy. Rio de Janeiro: Guanabara; 1995.
Ahmad M, Jenny J, Downieà M. Application of cone beam computed tomography in oral and maxillofacial surgery. Aust Dent J. 2012;57:82–94.
Ahmad L, Hollender Q, Anderson Q, Kartha K, Ohrbach R, Truelove ED, John MT, Schiffman EL. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–60.
Chicarelli M, França VTB, Walewski LA, Iwaki LCV, Tolentino ES. Temporal bone pneumatization in patients with dentofacial deformities: cone beam computed tomography study. Int J Oral Maxillofac Surg. 2019;48:1564–9.
Bhanu PS, Sankar KD. Incidence of Foramen of Huschke in South Andhra Population of India. J Clin Diagn Res. 2016;10:1–3.
Park YH, Kim HJ, Park MH. Temporomandibular joint herniation into the external auditory canal. Laryngoscope. 2010;120:2284–8.
Akbulut N, Kursun S, Aksoy S, Kurt H, Orhan K. Evaluation of foramen tympanicum using cone-beam computed tomography in orthodontic malocclusions. J Craniofac Surg. 2014;25:105–9.
Olarinoye-Akorede SA, Olanrewaju IS, Suleiman AO. Forame de Huschke (tímpano) em um homem nigeriano com herniação articular de partes moles no conduto auditivo externo. Ann Afr Med. 2014;13:226–8.
Deniz Y, Geduk G, Zengin AZ. Examination of foramen tympanicum: an anatomical study using cone-beam computed tomography. Folia Morphol (Warsz). 2018;77:335–9.
Hawke M, Kwok P, Mehta M, Wang RG. Bilateral spontaneous temporomandibular joint herniation into the external auditory canal. J Otolaryngol. 1987;16:387–9.
Greene MW, Hackney FL, Van Sickels JE. Arthroscopy of the temporomandibular joint: an anatomic perspective. J Oral Maxillofac Surg. 1989;47:386–9.
Herreira-Ferreira M, Tolentino ES, da Silva MC, Walewski LÂ, Iwaki LCV. Cone-beam computed tomographic study of the persistent foramen tympanicum according to age, sex, and skeletal patterns. Br J Oral Maxillofac Surg. 2020;58:57–61.
Meazzini MC, Brusati R, Caprioglio A, Diner P, Garattini G. True hemifacial microsomia and hemimandibular hypoplasia with condylar-coronoid collapse: Diagnostic and prognostic differences. AJO-DO. 2011;139(435):447.
Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28(1):6–27. https://doi.org/10.11607/jop.1151.
Tyndall SA, Matteson SR. Radiographic appearance and population distribution of the pneumatized articular eminence of the temporal bone. J Oral Maxillofac Surg. 1985;43:493–7.
Ladeira DB, Barbosa GL, Nascimento MC, Cruz AD, Freitas DQ, Almeida SM. Prevalence and characteristics of pneumatization of the temporal bone evaluated by cone beam computed tomography. Int J Oral Maxillofac Surg. 2013;42:771–5.
Manfredini D, Segù M, Arveda N, Lombardo L, Siciliani G, Rossi A, Guarda-Nardini L. Temporomandibular joint disorders in patients with different facial morphology A systematic review of the literature. J Oral Maxillofac Surg. 2016;74(29):46.
Orhan K, Oz U, Orhan AI, Ulker AE, Delibasi C, Akcam O. Investigation of pneumatized articular eminence in orthodontic malocclusions. Orthod Craniofacial Res. 2010;13:56–60.
Wang RG, Bingham B, Hawke M, Kwok P, Li JR. Persistence of the foramen of Huschke in the adult: an osteological study. J Otolaryngol. 1991;20:251–3.
Rezaian J, Namavar MR, VahdatiNasab V, Nobari ARH, Abedollahi A. Foramen tympanicum or foramen of huschke: a bioarchaeological study on human skeletons from an iron age cemetery at tabriz kabud mosque zone. Iran J Med Sci. 2015;40:367–71.
Ribeiro TMC, Freire AR, Junior ED, Botacin PR, Prado FB, Rossi AC. Foramen tympanicum prevalence in the population of Southeast Brazil: a morphological study in computed tomography scans. Folia Morphol. 2022;17:1042–6.
Lima AT, Leme TC, Barbieri AA, et al. Prevalence of tympanic foramen (or of Huschke) in a Brazilian population: study by cone beam computed tomography. Brazilian Dental Science. 2018;21:204–9.
Hasani M, Hadhnegahdar A, Khojastepour L, Haghighi MJG. Determining the existence of the foramen of Huschke in patients with temporomandibular joint disorders using cone beam computed tomography: retrospective cohort study. BMC Med Imaging. 2022;22:145.
Belgin CA, Serindere G, Aksoy S. Evaluation of the relationship between tympanic plate morphology and degenerative bone changes of condyle and articular eminence. J Stomatol Oral Maxillofac Surg. 2021;122:24–8.
Mathew AL, Sholapurkar AA, Pai KM. Condylar changes and its association with age, TMD, and dentition status: a cross-sectional study. Int J Dent. 2011;2011:413639.
Shahab S, Azizi Z, Damghani FT, Damghani FT. Prevalence of osseous changes of the temporomandibular joint in CBCT images of patients with and without temporomandibular disorders. Biosci Biotech Res Comm. 2017;10:518–24.
Nah KS. Condylar bony changes in patients with temporomandibular disorders: a CBCT study. Imaging Sci Dent. 2012;42:249–53.
Çakur B, Sümbüllü MA, Durna D, Akgül HM. Prevalência dos tipos de fissura petrotimpânica na disfunção da articulação temporomandibular. Acta radiol. 2011;52:562–5.
Gauer R, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician. 2015;91(6):378–86.
Scrivani SJ, Keith DA, Kaban LB. Desordens temporomandibulares. N Engl J Med. 2008;359:2693.
Chisnoiu AM, Picos AM, Popa S, Chisnoiu PD, Lascu L, Picos A. Fatores envolvidos na etiologia das disfunções temporomandibulares uma revisão de literatura. Clujul Med. 2015;88:473.
Li W, Dai C. Spontaneous temporomandibular joint herniation into the external auditory canal. Braz J Otorhinolaryngol. 2015;81:3.
Lim K, Jung J, Rhee J, Choi J. Herniação da articulação temporomandibular através do forame de Huschke com zumbido estalante. Eur Ann Otorhinolaryngol Head Neck Dis. 2019;136:497–9.
Tasar M, Yetiser S, Saglam M, Tasar A. Deformidade congênita da cavidade comum dos seios frontal, etmoidal e esfenoidal. Fenda Palatina Craniofac J. 2003;40:639–41.
Langer J, Begall K. Otosialorréia-diagnóstico e terapia de uma fístula salivar do canal auditivo externo. Laringorrinotologie. 2004;83:606–9.
Miloglu O, Yilmaz AB, Yildirim E, Akgul HM. Pneumatization of the articular eminence on cone beam computed tomography: prevalence, characteristics and a review of the literature. Dentomaxillofac Radiol. 2011;40:110–4.
Rezende Barbosa GL, Nascimento V, Ladeira DB, Bomtorim VV, Cruz AD, Almeida SM. Accuracy of digital panoramic radiography in the diagnosis of temporal bone pneumatization: a study in vivo using cone-beam-computed tomography. J Craniomaxillofac Surg. 2014;42:477–81.
Khojastepour L, Paknahad M, Abdalipur V, Paknahad M. Prevalence and characteristics of articular eminence pneumatization: a cone-beam computed tomographic study. J Maxillofac Oral Surg. 2018;17:339–44.
Koç A, Kaya S. Prevalence of foramen Huschke: evaluation of the association between mastoid pneumatization volume and the existence of foramen Huschke using cone beam computed tomography. Eur Arch Otorhinolaryngol. 2021;278:791–6.
Acknowledgements
The authors would like to thank the State University of Maringa for investing and contributing to science through research and development.
Funding
No funding used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
Informed consent
All authors consent the publication of this study as signed in the Certification Form.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fagundes, R.J., Felipe, B.C., Couto, M.K. et al. The relation between persistent foramen tympanicum and degenerative bone alterations in temporomandibular joint region. Oral Radiol (2024). https://doi.org/10.1007/s11282-024-00749-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11282-024-00749-3