Abstract
Objectives
Extranodal lymphomas affecting the head and neck infrequently arise within the jaw bones. Although clinical examination and conventional radiography may initially suffice for such lesions arising within the mandible, those arising within the maxillary alveolus generally require cross-sectional imaging because of the complex anatomy of this region. This study was performed to determine the prevalence, demographic characteristics, and clinical presentations of these lesions and the imaging modalities used for their diagnosis.
Study design
A systematic review (SR) on case series and another SR on case reports were performed to investigate the demographic, clinical, and radiological features of extranodal lymphomas arising within the maxillary alveolus.
Results
Most case series were derived from just four nations, whereas the case reports were derived from a wider range of ethnicities. The more detailed case reports significantly reported at least one imaging modality. Most patients were aware of their lesions for nearly 2 months before presentation. The most frequent symptom was swelling. Most case reports included a provisional diagnosis, the most frequent of which was dental infection followed by squamous cell carcinoma.
Discussion
Extranodal lymphomas arising within the maxillary alveolus were sufficiently frequent in four communities to be reported in two or more case series, and the occasional single case report indicated that such lesions are more widespread globally. Although the SR on case series revealed differences in the relative period prevalence and maxillary/mandibular ratio, the SR on case reports revealed details of the clinical presentation and imaging modalities used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymphoma accounts for about 5% of head and neck malignancies [1]. During the last 50 years, a new classification of lymphoma has appeared almost every decade; the 2016 revision of the World Health Organization classification [2] is the most recent. Lymphoma is divided into Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) based on its histopathological and clinical features. NHL is further divided into B- and T-cell lymphoma.
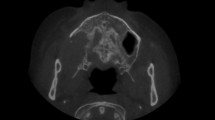
Thirty percent of lymphomas arise in tissues outside the lymph nodes. These are called extranodal lymphomas [1] and can be either HL or NHL [3]. Extranodal lymphoma arising within the jawbones is so rare that no cases were present in a case series of 361 oral and paraoral lymphomas [4]. Since the case series reported by Eisenbud et al. [5] in 1984, increasingly, more cases of extranodal lymphomas arising within the jawbones have been reported. A possible cause of the initial accumulation of lymphoid tissue (from which the lymphoma arises) within the jawbones is chronic dental disease, which may arise from an untreated or inadequately treated nonvital tooth or periodontal disease. Although such lesions affecting the mandibular alveolus are adequately displayed by the conventional radiography, those in the maxillary alveolus are not readily displayed. Cross-sectional imaging modalities, including cone-beam computed tomography (CBCT), are necessary for lesions arising within the anatomically complex maxilla [6,7,8]. A recent case report appeared to be the first to compare the merits of the conventional radiography, CBCT, computed tomography (CT), and magnetic resonance imaging (MRI) in the diagnosis of NHL arising within the maxillary alveolus [9].
We performed two systematic reviews (SRs) to examine the demographic and the clinical features at the first presentation and the radiological modalities used to investigate this rare but important phenomenon. The particular demographic and clinical features and radiological modalities considered by both SRs were prompted by the aforementioned recent case report [9]. The overall aim of these SRs was broadly similar to those of earlier SRs of other oral and maxillofacial lesions [10,11,12,13,14,15,16,17,18,19,20,21]: to determine whether the demographics, clinical presentation, and imaging modalities differ between case series and case reports of European, East Asian, and sub-Saharan origin. The following more specific questions were asked to both address the above aim and extract further information pertinent to clinical practice.
-
a.
What is the relative period prevalence of NHLs arising within the maxillary alveolus within an SR of case series?
-
b.
Which global communities have a greater prevalence of NHLs arising within the maxillary alveolus?
-
c.
Which demographic and clinical details are most likely to be associated with the first presentation of NHLs arising within the maxillary alveolus? This includes the patient’s prior awareness of the lesion before the first presentation.
-
d.
What advanced imaging modalities were prescribed in the course of diagnosis of NHLs arising within the maxillary alveolus?
Methods
The approach to these SRs followed the procedure set out in earlier SRs for other oral and maxillofacial lesions [10,11,12,13,14,15,16,17,18,19,20,21]. This approach was based on the format established for this purpose [22]. An essential element of an SR is a meta-analysis [22]. A meta-analysis, as defined by the dictionary of epidemiology, is “the process of using statistical methods to combine the results of different studies” [23]. Fisher’s exact test (FET) was applied to categorical data, because the total sample sizes were small [24]. Significance was defined by a two-tailed P value of < 0.05. All calculations were performed using the VassarStats software [25]. Although the literature search performed for the case reports revealed that extranodal lymphomas affecting the jaws were NHLs, a search strategy was developed that would enhance capture of HLs.
The Medline PubMed database was searched. The PubMed Medical Subject Heading (MeSH) “Lymphoma” is defined as “a general term for various neoplastic diseases of the lymphoid tissue.” It includes HLs and NHLs and was used in conjunction with “jaw” in the present study. Text word searches [22] of “lymphoma AND jaw” and “non-Hodgkin lymphoma maxilla” were also performed. These searches were last conducted on 30 August 2017.
Emphasis was placed on recall rather than precision to include as many reports as possible [22]. This strategy was further augmented by examination of the reference lists of the reports identified by the MeSH and text word searches. Major journals were also hand-searched.
SR of consecutive case series of extranodal lymphomas arising within the maxillary alveolus (Table 1)
The selection criteria for the case series were as follows:
-
1.
The article revealed that the case was a lymphoma.
-
2.
The article intended to report the entire case series of lymphomas and not a selection of cases. Case series that were restricted to a particular age group or type of lymphoma (e.g., B-cell type or Burkitt lymphoma) or clinicopathological group (e.g., patients with acquired immunodeficiency syndrome) were excluded. The only exception was case series of NHL.
-
3.
The article intended to include cases that primarily arose from the alveolus of both jaws. Although such a case series may not include a maxillary case, it was included to allow the SR to determine the ratio of maxillary to mandibular cases (maxilla/mandible ratio). Nevertheless, case series that were expressly concerned only with mandibular cases were excluded, whereas those expressly concerned with maxillary cases were included (although the latter were unable to contribute to the maxilla/mandible ratio).
-
4.
The case series revealed that the lymphoma(s) arose from within the alveolus of the jaws. In the absence of radiological evidence (or, failing that, clinical evidence) to the contrary, an unequivocal statement that the lymphoma arose within the alveolus of the jaws would be sufficient for inclusion of the report. Cases indicating secondary involvement of the maxillary alveolus from a lymphoma arising from the palate or from within the maxillary sinus were excluded.
SR of reported cases (case reports) of extranodal lymphomas arising within the maxillary alveolus (Table 2 [26])
A case report is used to describe the medical history of a single patient in the form of a story or anecdote. The case report is frequently used to alert colleagues to cases that deviate from the norm in important ways with regard to presentation, treatment, or outcome. The case report is also invaluable for detailed descriptions of rare lesions [27, 28], such as extranodal lymphomas arising within the alveolus of the maxilla. Individual case reports are “often run together to form a case series, in which the demographic, clinical, and other presentations of more than one patient with a particular condition are described to illustrate an aspect of the condition” [27]. However, the amount of detail available for each individual case in that case series may be lost. This will be further explored in the “Discussion”. For this reason, the present study included an SR of case reports in addition to an SR of case series.
The SR of case reports focused solely on cases of extranodal lymphomas of any kind arising within the alveolus of the maxilla. Included in this SR of case reports were individual cases reported with adequate detail in the case series (Table 1). Such cases provided details on at least the demographics, clinical features, and imaging modalities used at the first presentation.
To assist in answering the above-mentioned research questions, the case reports included in the SR were divided into four global groups broadly reflecting their ethnic origin: European, sub-Saharan African, East Asian, and Indian.
Results
Forty-six reports satisfied the selection criteria: 4 of the 146 hits in the search of the MeSH terms “Lymphoma AND Jaw,” 24 of the 739 hits in the search of the text words “lymphoma AND jaw,” 4 of the 105 hits in the search of the text word “non-Hodgkin lymphoma maxilla,” and 14 reports obtained from the reference lists and hand-searching.
The 16 case series [5, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43] included in the SR are shown in Table 1. Two case series were excluded. Velez and Hogge [44] reported only B-cell NHLs, and Kemp et al. [45] grouped NHLs arising in the maxillary alveolus together with those arising in the hard palate. For 3 of the 16 case series [30, 36, 37] that did not include a case arising within the maxillary alveolus, “Nil” is entered in the “relative period prevalence” column in Table 1. The relative period prevalence indicates the likelihood of a particular lesion presenting within a particular community each year. This is an average for that particular report depending on the total number of cases reported and the number of years covered by that report. The relative period prevalence was determinable in 8 of the 16 case series. Among all studies, a mean of 0.38 ± 0.18 extranodal lymphomas arose within the maxillary alveolus per year, suggesting that globally, an NHL may arise in the maxillary alveolus in such a case series every third year.
Of the 16 case series in Table 1, 10 were derived from 4 countries (3 from the United States, 3 from Holland, 2 from Greece, and 2 from Iran). Most of these reports were derived from different cities in the United States, Holland (Amsterdam and Utrecht), and Iran (Teheran and Mashhad). Two of the three Dutch reports were from Amsterdam and published a decade apart, and the two Greek reports were from different hospitals in the same city (Thessaloniki) and published about the same time. One of these hospitals in Thessaloniki had a higher relative period prevalence than the other. Teheran had a higher relative period prevalence than Mashhad, which had almost the lowest relative period prevalence overall. The maxilla/mandible ratio declined over time in both the US and Dutch reports. Patients of European origin predominated in both the SRs of case series (76%) and case reports (73%) (Tables 1, 2, respectively).
Of the cases shown in Table 2, 29 [9, 46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72] were reported as single case reports. A case series of three B-cell NHLs [44] and a double case report [73] are included in the SR in Table 2. To these were added cases for which the demographic and clinical details were reported in the case series. Four case series provided these details for at least one of their cases [5, 29, 34, 35]. Details about the imaging modalities used for diagnosis were added for some of these cases. Ten more nations are represented in Table 2 than Table 1. Although many of those case reports were European (UK, Poland, Croatia, Italy, Spain, and Switzerland), China, India, Brazil, and Canada were also represented.
Table 1 includes four cases of T-cell lymphoma, whereas Table 2 shows only one [53]. Table 2 includes one case of HL, whereas almost every other case was identified as an NHL, many of which were identified as B-cell lymphomas.
Although most NHLs arising within the maxillary alveolus first presented in the posterior sextant in both Tables 1 and 2, seven cases in Table 2 first presented in both the anterior and posterior sextants. Five were reported in the last 5 years, all with a provisional diagnosis of a malignancy.
In Tables 1 and 2, NHLs arising within the maxillary alveolus presented more frequently in males. This predilection for males (23 males to 6 females) was more significant for patients of European origin than for those of sub-Saharan African origin (3 males to 5 females; FET = 0.035).
The vast majority of extranodal lymphomas arising within the alveolus of the maxilla presented in the patient’s fifth decade of life. Table 2 shows that the mean age for all 43 patients at the first presentation was 48.26 ± 18.89 years. For the 29 patients of European origin, the mean age at presentation was 52.18 ± 19.67 years; that for the 4 patients of East Asian origin was 52.50 ± 13.38 years; that for the 8 patients of sub-Saharan African origin was 36.11 ± 16.01 years; and that for the 3 Indians was 43.67 ± 15.18 years. The difference in the age at the first presentation between patients of European versus sub-Saharan African origin was significant (t = 2.46; 34 degrees of freedom P > 0.01).
As shown in Table 1, two case series reported a period of prior awareness. This period was a mean of 1 month in a European case series [29] and 2 months in a sub-Saharan African case series [35]. As shown in Table 2, 30 case reports reported a mean period of prior awareness of nearly 2 months.
Almost all patients in Table 2 presented with symptoms; < 10% were discovered incidentally. The most prevalent symptom in almost all cases was swelling (84%), whereas only 41% presented with pain. Eight patients (23%) presented with numbness. Nine patients in Table 2 had a pre-existing infection (the lymphoma was detected secondary to extractions in three reports and endodontic treatment in the other six).
Unlike Table 1, Table 2 recorded non-comments with regards important symptoms such as swelling, pain, discharge, ulcers and tooth mobility at presentation as “No.” The reasoning for this was that if the report included at least one symptom, then it is reasonable to assume that the clinicians also assessed the patients for other symptoms. The exception was numbness, which is addressed later in the “Discussion”. Non-comments with regard to imaging modalities were recorded as “No” simply because case reports are likely to be more detailed than case series. Furthermore, it is also unlikely that a case report would deliberately exclude mentioning the use of advanced imaging modalities.
With the exception of the three Nigerian case reports, all case reports in Table 2 described at least one imaging modality. Although all case reports in Table 2 reported at least one imaging modality, only 3 of the 16 case series in Table 1 did so. Eighteen cases that were derived from case reports (not included in Table 1) reported at least one advanced imaging modality (CT, MRI, or CBCT) compared with 0 of the 7 cases listed in Table 1; this difference was significant (FET = 0.011). All three advanced imaging modalities were reported more recently in accordance with the time periods of their general clinical availability globally and nationally. The earliest reported use of CBCT [54], which was performed to investigate a lymphoma, was reported within a few years of its initial clinical availability.
Eight of the 13 cases that reported the size of the lesion in Table 2 were derived for measurements made by advanced imaging modalities.
The radiological features observed in the conventional radiography and advanced imaging modalities in Table 2 were previously addressed in a recent case report [9].
A differential diagnosis was available for 23 of the 44 cases in Table 2. Twenty of the 23 cases were from case reports. Nine were provisionally diagnosed as dental infections, seven as squamous cell carcinoma (SCC), and three as malignancies. One case was suspected to be a recurrent case of NHL based on the patient’s medical history.
Discussion
Although consecutive case series allow for better determination of the relative period prevalence of a lesion affecting a particular community during a specified period [10], they are frequently lacking in clinical details other than the patients’ age, sex, and affected jaw. Earlier SRs [10,11,12,13,14,15,16,17,18,19,20,21] are often even less forthcoming with radiological details. Conversely, case reports are more detailed with regard to clinical and radiological presentations and a differential or provisional diagnosis. Although the value of the case report is generally somewhat restricted to a particular lesion with an unusual presentation, be it clinical, radiological, and/or histopathological, an extranodal lymphoma arising within the alveolus of the jaws is already unusual as revealed earlier by the absence of any such lesions appearing in a very large case series of oral lymphomas [4]. Therefore, when assessed in an SR, these more detailed reports of individual cases give the best current overall picture to the clinician until even more detailed case series are published.
Although the markedly higher prevalence of males in Table 1 is consistent with the overall higher prevalence of males with NHL across all age groups and ethnicities, recent reports have indicated that this prevalence is particularly higher in Africans, Middle Easterners, and East and South Asians than in North Americans [74,75,76,77].
Although extranodal lymphomas arising within the jaws are relatively frequent, with at least two case series reported in the United States, Holland, Greece, and Iran (Table 1), occasional single case reports appear in a wider range of ethnicities from every inhabited continent (Table 2). This should prompt global vigilance regarding the presence of this lesion in all populations.
The decline in the maxilla/mandible ratio in the US and Dutch case series over time suggests that lymphomas arising within the maxillary alveolus in these two nations are decreasing in prevalence. The absence of such a pattern in the Iranian pair of case series reported 1 year apart could reflect ethnic differences between the two Iranian cities in these case series. They were from the two largest Iranian cities, Teheran and Mashhad. Mashhad has a substantial Turkmen community, which is East Asian in contrast to the mainly Indo-European community in Teheran. The relative period prevalence in Teheran was 0.74 [41], the highest of all case series in Table 1, whereas that of Mashhad was 0.20 [40], almost the lowest of all case series. The difference in the maxilla/mandible ratio between these two case series tended to significant (FET = 0.080). Ethnicity may also play a role in some of the other outliers observed in Tables 1 and 2. After the Teheran Iranians [41], the Nigerians [35] had the second highest relative period prevalence of 0.60.
The significantly earlier first presentation of NHLs arising within the maxillary alveolus in patients of sub-Saharan African origin is noteworthy and should prompt suspicion of NHL or at least another malignancy whenever such a lesion fails to respond to treatment for dental inflammation or its presentation suggests a malignant lesion.
Although Indians, certainly North Indians, are genetically similar to Middle Easterners and Europeans [78], significant differences in the presentation of nevoid basal cell carcinoma between these patients and North Europeans have been observed [79]. Although the age of two [69, 70] of the three Indian patients at the first presentation was well within the first standard deviation of the mean age for Europeans, the third Indian patient was younger and outside the first standard deviation. This third Indian was a 30-year-old woman in otherwise good health. Her initial complaint was related to pain and swelling at an extraction site. The swelling increased to a substantial size during a 2-week period, at which time she was referred. A substantial increase in size during a > 1-week period was also observed in a recent report of a Chinese woman [9]. Two other outliers were observed in patients of European origin: a 5-year-old Spanish boy [57] and a 31-year-old Canadian woman [73]. The boy had Burkett lymphoma, which is generally endemic in sub-Saharan Africa but occurs sporadically elsewhere [57]. Unlike the Indian woman, the Canadian woman reported recurring swelling which recurred despite endodontic treatment [73]. Therefore, as mentioned above for patients of sub-Saharan African origin, failure to respond to the usual treatment for dental inflammation should prompt an appropriate referral.
Environmental and health care factors (e.g., vaccinations) can influence Epstein–Barr virus positivity [80]. In one report, the rate of Epstein–Barr virus positivity in T- and B-cell lymphomas was 36 and 7%, respectively [81]. The sole case of T-cell lymphoma in Table 2 involved a Japanese patient from Kyushu [58], where T-cell lymphomas account for 74% of NHLs in contrast to 25% for most of East Asia and about 5% for communities largely of European origin (see Table 5 in the report by Peh [81]). Fukuda et al. [30] reported that 2 of their 20 cases of mandibular lymphomas in Japanese patients were T-cell lymphomas.
One-third of patients in Table 2 were clearly aware of their lesions 1 month prior to their first presentation, which is generally a shorter time period than that for most benign neoplasms and cysts arising within the jaws [10,11,12,13,14,15,16,17,18,19,20,21]. Therefore, the brevity of this period of prior awareness may serve as an additional prompter to consider a more serious disease if a lesion, provisionally diagnosed as an inflammatory lesion, does not respond promptly to appropriate treatment. Nevertheless, the period of awareness of a lesion that is eventually diagnosed as an extranodal lymphoma arising within the alveolus of the jaws may vary among different ethnicities (e.g., 2 months for Nigerians [32] but only 1 month for Dutch patients [29]).
Swelling is the predominant symptom at the first presentation, whereas pain and numbness are less frequent. Numbness, an important indicator of malignancy within the mandible [82], is a frequently reported symptom of mandibular lymphoma [34]. Nevertheless, numbness has been infrequently reported for lymphomas arising within the alveolus of the maxilla. This may reflect the fact that the inferior orbital nerve, the supplier of innervation to the upper lip, is separated from an extranodal lymphoma arising with the alveolus by the frequently voluminous lumen of the maxillary sinus. Conversely, the inferior alveolar nerve, the supplier of innervation to the lower lip, courses through the mandibular canal and is, therefore, in closer proximity to an extranodal lymphoma arising within the mandibular alveolus. More than half of the 13 lymphomas in Table 2 measured by advanced imaging modalities were of substantial dimensions, and although some can be expected to have reached the inferior orbital nerve, this may not be enough to cause numbness. Evidence for this comes from a case series of NHLs and SCCs arising within the maxillary sinus itself. Although it is reasonable to expect that NHLs arising within the maxillary sinus are in closer proximity to the inferior orbital nerve and are, therefore, more likely to be associated with a numb upper lip, Kato et al. [83] made no mention of this. Instead, they reported that the most frequent symptoms of NHL arising within the maxillary sinus are facial swelling, epistaxis, nasal obstruction, and headaches [83].
Although the relative paucity of clinical detail in the case series of our SR (Table 1) is not dissimilar to that in SRs performed for other lesions [10,11,12,13,14,15,16,17,18,19,20,21], the complete exclusion of the conventional radiography is remarkable (although understandable). Most the case series included in the SR (Table 1) focused on the prevalence and outcomes of treatment or how the latter may be related to the histopathology. Because the histopathological diagnosis is generally obtained after the clinical and radiological examinations have been completed, the clinical and radiological features at the first presentation may not have been considered particularly relevant to the subsequent management and patient outcomes. Nevertheless, it is reasonable to assume that conventional radiography had been completed in every case at the appropriate time. Likewise, this assumption may be extended to medical CT for all cases (Table 2), except for the earliest case series when this technology was not yet available. This last remark is even truer for MRI and CBCT, which only really became widely available 25 and 10 years ago, respectively.
Most of the cases in Table 2, particularly the case reports [9, 46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73], were associated with a provisional diagnosis of a dental infection or SCC. Only the provisional diagnosis of a single maxillary lesion indicated NHL [70], simply because this had already been diagnosed and treated and had been in remission for 2 years. That maxillary lesion was considered to reflect recurrent disease, which was found elsewhere in the patient and led to her death shortly thereafter. The importance of oral and maxillofacial clinicians’ awareness of lymphomas is that lymphoid cancers, which in addition to NHL and HL include myeloma and lymphocytic leukemia, vary among global communities. Specifically, NHL and HL are lowest in East Asians, particularly the Hong Kong Chinese, and highest in Western Europe, the United States, and Australia [75,76,77].
Our overall conclusions are as follows:
-
1.
Although extranodal lymphomas arising within the alveolus of the jaws were sufficiently frequent in four communities to be reported in two or more case series, the occasional single case report indicates that such lymphomas are more widespread globally.
-
2.
Although HL can occasionally arise within the alveolus, the overwhelming majority are NHLs.
-
3.
Although the SR of case series displayed differences between HL and NHL with regard to the relative period prevalence and maxillary/mandibular ratio, the SR of case reports revealed details regarding the clinical presentation and imaging modalities used.
-
4.
The most frequent clinical feature at the first presentation of an extranodal lymphoma arising in the maxillary alveolus was a swelling followed by pain or discomfort. Numbness is an important feature of extranodal lymphoma arising with the mandibular alveolus; nevertheless, numbness of the upper lip occurred in nearly one-quarter of cases of NHL arising within the maxillary alveolus.
-
5.
Many patients were aware of their lesions 1–2 months prior to their first presentation. This brevity of the period of prior awareness should prompt consideration of more serious disease, particularly if the lesion does not respond promptly to appropriate treatment for a dental infection.
-
6.
Most of the case reports included a provisional diagnosis. The most frequent was a dental infection, and the next most frequent was SCC.
Change history
14 July 2018
Owing to an unfortunate mistake at Springer?s end, the original article was published with errors which are corrected with this erratum as suggested by the author. The authors are not responsible for this procedural lapse.
14 July 2018
Owing to an unfortunate mistake at Springer?s end, the original article was published with errors which are corrected with this erratum as suggested by the author. The authors are not responsible for this procedural lapse.
14 July 2018
Owing to an unfortunate mistake at Springer���s end, the original article was published with errors which are corrected with this erratum as suggested by the author. The authors are not responsible for this procedural lapse.
References
Lubek JE, Shihabi A, Murphy LA, Berman JN. Hematopoietic neck lesions. Atlas Oral Maxillofac Surg Clin N Am. 2015;23:31–7.
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Paes FM, Kalkanis DG, Sideras PA, Serafini AN. FDG PET/CT of extranodal involvement in non-Hodgkin lymphoma and Hodgkin disease. Radiographics. 2010;30:269–91.
Epstein JB, Epstein JD, Le ND, Gorsky M. Characteristics of oral and paraoral malignant lymphoma: a population-based review of 361 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:519–25.
Eisenbud L, Sciubba J, Mir R, Sachs SA. Oral presentations in non-Hodgkin’s lymphoma: a review of thirty-one cases. Part II. Fourteen cases arising in bone. Oral Surg Oral Med Oral Pathol. 1984;57:272–80.
MacDonald DS, editor. Maxillary antrum. In: Oral and maxillofacial radiology: a diagnostic approach. Ames: Wiley; 2011. pp. 197–9.
MacDonald DS. Maxillofacial fibro-osseous lesions. Clin Radiol. 2015;70:25–36. https://doi.org/10.1016/j.crad.2014.06.022.
MacDonald DS. Lesions of the jaws presenting as radiolucencies on cone-beam computed tomography. Clin Radiol. 2016;71:972–85. https://doi.org/10.1016/j.crad.2016.05.018.
MacDonald DS, Li T, Leung SF, Curtin J, Leung A, Martin MA. Extranodal lymphoma arising within the maxillary alveolus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2017;124:e233–e8. https://doi.org/10.1016/j.oooo.2017.04.015.
MacDonald-Jankowski DS, Yeung R, Lee KM, Li TK. Odontogenic myxomas in the Hong Kong Chinese: clinico-radiological presentation and systematic review. Dentomaxillofac Radiol. 2002;31:71–83.
MacDonald-Jankowski DS, Yeung R, Lee KM, Li TK. Ameloblastoma in the Hong Kong Chinese. Part 1: systematic review and clinical presentation. Dentomaxillofac Radiol. 2004;33:71–82.
MacDonald-Jankowski DS, Yeung R, Lee KM, Li TK. Ameloblastoma in the Hong Kong Chinese. Part 2: systematic review and radiological presentation. Dentomaxillofac Radiol. 2004;33:141–51.
MacDonald-Jankowski DS. Florid cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2003;32:141–9.
MacDonald-Jankowski D, Chan KC. Clinical presentation of dentigerous cysts: systematic review. Asian J Oral Maxillofac Surg. 2005;15:109–20.
MacDonald-Jankowski DS. Focal cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2008;37:350–60. https://doi.org/10.1259/dmfr/31641295.
MacDonald-Jankowski D. Fibrous dysplasia: a systematic review. Dentomaxillofac Radiol. 2009;38:196–215. https://doi.org/10.1259/dmfr/16645318.
MacDonald-Jankowski DS. Ossifying fibroma: a systematic review. Dentomaxillofac Radiol. 2009;38:495–513. https://doi.org/10.1259/dmfr/70933621.
MacDonald-Jankowski DS. Orthokeratinized odontogenic cyst: a systematic review. Dentomaxillofac Radiol. 2010;39:455–67. https://doi.org/10.1259/dmfr/19728573.
MacDonald-Jankowski DS. Glandular odontogenic cyst: systematic review. Dentomaxillofac Radiol. 2010;39:127–39. https://doi.org/10.1259/dmfr/30943934.
MacDonald-Jankowski DS. Keratocystic odontogenic tumour: systematic review. Dentomaxillofac Radiol. 2011;40:1–23. https://doi.org/10.1259/dmfr/29949053.
MacDonald DS. A systematic review of the literature of nevoid basal cell carcinoma syndrome affecting East Asians and North Europeans. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:396–407.
MacDonald-Jankowski DS, Dozier MF. Systematic review in diagnostic radiology. Dentomaxillofac Radiol. 2001;30:78–83.
Clarkson JE, Bonner BC, Deery C, Grimshaw J. Evidence-based dentistry for effective practice. London: Martin Dunitz; 2003. pp. 68, 75.
Brunette DM. Critical thinking: understanding and evaluating dental research. 2nd ed. Hanover Park: Quintessence Publishing; 2007. pp. 127–8.
VassarStats. 2 × 2 contingency table. http://vassarstats.net/tab2x2.html. Accessed 30 Aug 2017.
Yepes JF, Alawi F, Stanton DC, Stoopler ET. Extranodal marginal zone lymphoma: a case report and review of the literature. Gen Dent. 2005;53:335–8.
Greenhalgh T. How to read a paper. Getting your bearings (deciding what the paper is about). BMJ. 1997;315:243–6.
Vandenbroucke JP. In defense of case reports and case series. Ann Intern Med. 2001;134:330–4.
Slootweg PJ, Wittkampf AR, Kluin PM, de Wilde PC, van Unnik JA. Extranodal non-Hodgkin’s lymphoma of the oral tissues. An analysis of 20 cases. J Maxillofac Surg. 1985;13:85–92.
Fukuda Y, Ishida T, Fujimoto M, Ueda T, Aozasa K. Malignant lymphoma of the oral cavity: clinicopathologic analysis of 20 cases. J Oral Pathol. 1987;16:8–12.
Howell RE, Handlers JP, Abrams AM, Melrose RJ. Extranodal oral lymphoma. Part II. Relationships between clinical features and the Lukes-Collins classification of 34 cases. Oral Surg Oral Med Oral Pathol. 1987;64:597–602.
Söderholm AL, Lindqvist C, Heikinheimo K, Forssell K, Happonen RP. Non-Hodgkin’s lymphomas presenting through oral symptoms. Int J Oral Maxillofac Surg. 1990;19:131–4.
Wolvius EB, van der Valk P, van der Wal JE, van Diest PJ, Huijgens PC, van der Waal I, et al. Primary extranodal non-Hodgkin lymphoma of the oral cavity. An analysis of 34 cases. Eur J Cancer B Oral Oncol. 1994;30B:121–5.
Pazoki A, Jansisyanont P, Ord RA. Primary non-Hodgkin’s lymphoma of the jaws: report of 4 cases and review of the literature. J Oral Maxillofac Surg. 2003;61:112–7.
Ugboko VI, Oginni FO, Adelusola KA, Durosinmi MA. Orofacial non-Hodgkins lymphoma in Nigerians. J Oral Maxillofac Surg. 2004;62:1347–50.
Kolokotronis A, Konstantinou N, Christakis I, Papadimitriou P, Matiakis A, Zaraboukas T, et al. Localized B-cell non-Hodgkin’s lymphoma of oral cavity and maxillofacial region: a clinical study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:303–10.
van der Waal RI, Huijgens PC, van der Valk P, van der Waal I. Characteristics of 40 primary extranodal non-Hodgkin lymphomas of the oral cavity in perspective of the new WHO classification and the International Prognostic Index. Int J Oral Maxillofac Surg. 2005;34:391–5.
Djavanmardi L, Oprean N, Alantar A, Bousetta K, Princ G. Malignant non-Hodgkin’s lymphoma (NHL) of the jaws: a review of 16 cases. J Craniomaxillofac Surg. 2008;36:410–4.
Keszler A, Piloni MJ, Paparella ML, Soler Mde D, Ron PC, Narbaitz M. Extranodal oral non-Hodgkin’s lymphomas. A retrospective study of 40 cases in Argentina. Acta Odontol Latinoam. 2008;21:43–8.
Etemad-Moghadam S, Tirgary F, Keshavarz S, Alaeddini M. Head and neck non-Hodgkin’s lymphoma: a 20-year demographic study of 381 cases. Int J Oral Maxillofac Surg. 2010;39:869–72.
Mohtasham N, Babakoohi S, Sarraf-Yazdy M, Sadr B, Ghaffarzadegan K, Shiva A, et al. Oral and jaw lymphoma in an Iranian population. J Craniofac Surg. 2011;22:868–70.
Triantafillidou K, Dimitrakopoulos J, Iordanidis F, Gkagkalis A. Extranodal non-Hodgkin lymphomas of the oral cavity and maxillofacial region: a clinical study of 58 cases and review of the literature. J Oral Maxillofac Surg. 2012;70:2776–85.
Ramanathan A, Mahmoud HA, Hui LP, Mei NY, Valliappan V, Zain RB. Oral extranodal non-Hodgkin’s lymphoma: series of forty two cases in Malaysia. Asian Pac J Cancer Prev. 2014;15:1633–7.
Velez I, Hogge M. Primary maxillofacial large B-cell lymphoma in immunocompetent patients: report of 5 cases. Case Rep Radiol. 2011;2011:108023.
Kemp S, Gallagher G, Kabani S, Noonan V, O’Hara C. Oral non-Hodgkin’s lymphoma: review of the literature and World Health Organization classification with reference to 40 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:194–201.
Keyes GG, Balaban FS, Lattanzi DA. Periradicular lymphoma: differentiation from inflammation. Oral Surg Oral Med Oral Pathol. 1988;66:230–5.
Ronchi P, Epifani C, Lunetta PH. Hodgkin’s disease of the jaw: report of a case. J Oral Maxillofac Surg. 1988;46:155–8.
Li TK, MacDonald-Jankowski DS. An unusual presentation of a high-grade, non Hodgkin’s lymphoma in the maxilla. Dentomaxillofac Radiol. 1991;20:224–6.
Rog RP. Beware of malignant lymphoma masquerading as facial inflammatory processes. Oral Surg Oral Med Oral Pathol. 1991;71:415–9.
Thomas DW, Gray W, Tate RJ. Non-Hodgkin’s lymphoma presenting at the site of a recent dental extraction: a report of two cases. Br J Oral Maxillofac Surg. 1991;29:34–7.
Hokett SD, Cuenin MF, Peacock ME, Thompson SH, Van Dyke TE. Non-Hodgkin’s lymphoma and periodontitis. A case report. J Periodontol. 2000;71:504–9.
Kozakiewicz M, Karolewski M, Kobos JW, Stołecka Z. Malignant lymphoma of the jaw bone. Med Sci Monit. 2003;9:CS110–C4.
Kobler P, Borcic J, Filipovic Zore I, Nola M, Sertic D. Primary non-Hodgkin’s lymphoma of the oral cavity. Oral Oncol Extra. 2005;41:12–4.
MacDonald-Jankowski DS, Orpe E. Computed tomography for oral and maxillofacial surgeons. Part 2: cone-beam computed tomography. Asian J Oral Maxillofac Surg. 2006;18:85–92.
Cavalcante AS, Anbinder AL, Pontes EM, Carvalho YR. B-cell lymphoblastic lymphoma in the maxilla of a child: a rare case report. Int J Oral Maxillofac Surg. 2009;38:1326–30.
Saund D, Kotecha S, Rout J, Dietrich T. Non-resolving periapical inflammation: malignant deception. Int Endod J. 2010;43:84–90.
Valenzuela-Salas B, Dean-Ferrer A, Alamillos-Granados FJ. Burkitt’s lymphoma: a child’s case presenting in the maxilla. Clinical and radiological aspects. Med Oral Patol Oral Cir Bucal. 2010;15:e479–82.
Yamada T, Mishima K, Ota A, Moritani N, Matsumura T, Katase N, et al. A case of ATLL (adult T-cell leukemia/lymphoma) mimicking odontogenic infection. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e51–5.
Agrawal MG, Agrawal SM, Kambalimath DH. Non-Hodgkins lymphoma of maxilla. A rare entity. Natl J Maxillofac Surg. 2011;2:210–3.
Matsuzaki H, Katase N, Hara M, Asaumi J, Yanagi Y, Unetsubo T. Primary extranodal lymphoma of the maxilla: a case report with imaging features and dynamic data analysis of magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e59–69.
Fischer DJ, Klasser GD, Kaufmann R. Intraoral swelling and periapical radiolucency. J Am Dent Assoc. 2012;143:985–8.
Frei M, Dubach P, Reichart P, Schmitt A, Mueller-Garamvolgyi E, Bornstein M. Diffuse swelling of the buccal mucosa and palate as first and only manifestation of an extranodal non-Hodgkin ‘double-hit’ lymphoma: report of a case. Oral Maxillofac Surg. 2012;16:69–74.
Rullo R, Addabbo F, Festa VM. Painless, rapidly increasing maxillary swelling and erythematous mucosa: differential diagnosis and therapy. J Can Dent Assoc. 2012;78:c50.
Koivisto T, Bowles WR, Magajna WA, Rohrer M. Malignant lymphoma in maxilla with cystic involvement: a case report. J Endod. 2013;39:935–8.
Vourexakis Z, Dulguerov P. Extensive maxillofacial plasmablastic lymphoma in an immunocompetent patient. BMJ Case Rep. 2014;2014:bcr2014204042. https://doi.org/10.1136/bcr-2014-204042.
Bagan JV, Carbonell F, Gómez MJ, Sánchez M, Navarro A, Leopoldo M, et al. Extra-nodal B-cell non-Hodgkin’s lymphomas of the head and neck: a study of 68 cases. Am J Otolaryngol. 2015;36:57–62.
Buchanan A, Kalathingal S, Capes J, Kurago Z. Unusual presentation of extranodal diffuse large B-cell lymphoma in the head and neck: description of a case with emphasis on radiographic features and review of the literature. Dentomaxillofac Radiol. 2015;44:20140288. https://doi.org/10.1259/dmfr.20140288.
Webber B, Webber M, Keinan D. Extranodal large B cell lymphoma of the anterior maxilla. Case report and review of literature. N Y State Dent J. 2015;81:34–8.
Jayapalan CS, Pynadath MK, Mangalath U, George A, Aslam S, Hafiz A. Clinical diagnostic dilemma in an uncharacteristic rapidly enlarging swelling of the anterior maxilla: extranodal diffuse large B cell lymphoma. BMJ Case Rep. 2016. https://doi.org/10.1136/bcr-2015-213141.
Kumar MS, Gannepalli A, Chandragiri A, Amarnath K. Diffuse large B-cell lymphoma of maxilla: a case report of late relapse. J Clin Diagn Res. 2016;10:ZD12–Z14. https://doi.org/10.7860/JCDR/2016/16139.7695.
Syed A, Singer S, Mupparapu M. Non-Hodgkin’s lymphoma in the oral cavity. J Mich Dent Assoc. 2016;98:40–3.
Dolan J, DeGraft-Johnson A, McDonald N, Ward B, Phillips T, Munz S. Maxillary and mandibular non-Hodgkin lymphoma with concurrent periapical endodontic disease: diagnosis and management. J Endod. 2017;43:1744–9.
Wong GB, Spadafora S, Barbon N, Caputo M. Primary extranodal B-cell non-Hodgkin lymphoma mimicking an endodontic lesion: report of 2 cases. J Can Dent Assoc. 2013;79:d93.
Bassig BA, Au WY, Mang O, Ngan R, Morton LM, Ip DK, et al. Subtype-specific incidence rates of lymphoid malignancies in Hong Kong compared to the United States, 2001–2010. Cancer Epidemiol. 2016;42:15–23.
Perry AM, Perner Y, Diebold J, Nathwani BN, MacLennan KA, Müller-Hermelink HK, et al. Non-Hodgkin lymphoma in Southern Africa: review of 487 cases from the international non-Hodgkin lymphoma classification project. Br J Haematol. 2016;172:716–23.
Perry AM, Diebold J, Nathwani BN, MacLennan KA, Müller-Hermelink HK, Bast M, et al. Relative frequency of non-Hodgkin lymphoma subtypes in selected centres in North Africa, the middle east and India: a review of 971 cases. Br J Haematol. 2016;172:699–708.
Perry AM, Diebold J, Nathwani BN, MacLennan KA, Müller-Hermelink HK, Bast M, et al. Non-Hodgkin lymphoma in the far east: review of 730 cases from the international non-Hodgkin lymphoma classification project. Ann Hematol. 2016;95:245–51.
Moorjani P, Thangaraj K, Patterson N, Lipson M, Loh PR, Govindaraj P, et al. Genetic evidence for recent population mixture in India. Am J Hum Genet. 2013;93:422–38.
MacDonald DS, Li T, Goto TK. A consecutive case series of nevoid basal cell carcinoma syndrome affecting the Hong Kong Chinese. Oral Surg Oral Med Oral Path Oral Radiol. 2015;120:396–407.
Condon LM, Cederberg LE, Rabinovitch MD, Liebo RV, Go JC, Delaney AS, et al. Age-specific prevalence of Epstein-Barr virus infection among Minnesota children: effects of race/ethnicity and family environment. Clin Infect Dis. 2014;59:501–8.
Peh SC. Host ethnicity influences non-Hodgkin’s lymphoma subtype frequency and Epstein-Barr virus association rate: the experience of a multi-ethnic patient population in Malaysia. Histopathology. 2001;38:458–65.
Tejani N, Cooper A, Rezo A, Pranavan G, Yip D. Numb chin syndrome: a case series of a clinical syndrome associated with malignancy. J Med Imaging Radiat Oncol. 2014;58:700–5.
Kato H, Kanematsu M, Watanabe H, Kawaguchi S, Mizuta K, Aoki M. Differentiation of extranodal non-Hodgkins lymphoma from squamous cell carcinoma of the maxillary sinus: a multimodality imaging approach. Springerplus. 2015;4:228. https://doi.org/10.1186/s40064-015-0974-y.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
David MacDonald and Sean Lim declare that they have no conflicts of interest.
Human rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
The original version of this article was revised: Modifications have been made in the result and discussion section. Full information regarding corrections made can be found in the correction article for this article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
MacDonald, D., Lim, S. Extranodal lymphoma arising within the maxillary alveolus: a systematic review. Oral Radiol 34, 113–126 (2018). https://doi.org/10.1007/s11282-017-0309-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-017-0309-5