Abstract
Human inborn errors of immunity (IEIs), previously referred to as primary immunodeficiency disorders (PIDs), are a heterogeneous spectrum of inherited abnormalities of the immune system with different organ involvement. The number of identified IEIs is rapidly increasing, highlighting the non-negligible role of an interdisciplinary approach in clinical diagnosis. Kidney disorders are one of the important comorbidities in some of the affected patients and play a significant role in the diagnosis and course of disease. According to recent studies, 22 types of human IEI with renal manifestations have been identified so far, including immunodeficiency with congenital thrombocytopenia, thymic defects with additional congenital anomalies, complement deficiencies, type 1 interferonopathies, immunity related to non-hematopoietic tissues, congenital neutropenia’s, common variable immunodeficiency disorder (CVID) phenotype and immuno-osseous dysplasia. Based on this classification, we herein review IEIs with renal features and explain the genetic defect, inheritance, and type of renal manifestations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
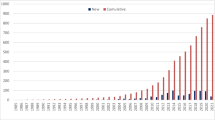
Inborn errors of immunity (IEI) comprise a group of 485 inherited disorders. Damage to the germinal variants of genes is the cause of these hereditary disorders (1). Indeed, deletion or reduction of the protein expression or function (null/hypomorphic) or protein modification to acquire gain-of-function (GOF) result in altering the encoded gene product and cause IEI, on this basis they divided into dominant or recessive, autosomal, or X-linked, and with complete or incomplete penetrance. IEIs are clinically manifested with a wide spectrum of mild to severe symptoms, including recurrent infections, autoimmunity and autoinflammatory diseases, allergy, bone marrow failure, and often malignancy. Manifestations are related to variant type and its inheritance (2). Although IEIs are considered rare disorders and affect 1 in every 10,000 to 50,000 births based on the type, the recognition of new phenotypes can change its prevalence as the estimated prevalence rate is 1 in every 1000 to 10,000 births [3]. In the past few years, several novel gene defects have been found, and more case reports of these patients have been published [2, 4]. In a number of these studies, the role of kidney disorders in the onset, duration, and end of the disease was reported, and the main cause of death in some of them was related to kidney disease [5,6,7,8]. In this study, we review kidney disorders among these patients and discuss the related renal manifestations. To identify relevant articles, we performed an advanced search in PubMed, using the following combination of keywords; nephropathy, renal disorder, renal abnormality, proteinuria, nephrocalcinosis, glomerulonephritis, nephrotic syndrome, autoimmunity, lupus nephritis, hemolytic uremic syndrome (HUS) and Inborn errors of immunity. Based on recent studies 22 types of IEI were described to have kidney disorders as their manifestations, which are listed in Table 1 according to the type of mutation, IEI classification, and the type of kidney disease.
IEIs with renal manifestations
IEIs are classified into 10 groups in the last update of The International Union of Immunological Societies (IUIS) in 2022 [1], and in this study, most renal manifestations were related to the complements. In Table 1, these diseases are given and in the section below, diseases with more evidence in the literature were reviewed.
Complement deficiencies
Factor H-related protein deficiencies
The five Complement Factor H-related proteins (FHR1–5) are structurally related to factor H, an important regulator of complement alternative pathways [9]. Mutations in FHR by creating duplicated dimerization domains lead to C3 glomerulopathy (C3G), which is a heterogeneous group of chronic kidney diseases [10]. Renner et al. (2022) In a study on murine, reported that variation in genes or expression of FHRs can be associated with glomerular damage by disrupting the regulation of complement binding to mesangial, glomerular endothelial, podocytes, and tubular epithelial cells [11]. Medjeral-Thomas et al. [12] and Zhu et al. [13] identified the increased level of FHR-5 in patients with Immunoglobulin A nephropathy (IgAN) as a risk factor for disease progression.
Thrombomodulin deficiency
Thrombomodulin is a membrane protein and cofactor for thrombin which has a strategic role in coagulation, innate immunity and complement regulation [14]. This protein is encoded by the THBD gene and variants including A43T (Impaired binding of Complement factor H (CFH) and C3b) [15], P495S and P501L (Moderate reduction of thrombomodulin expression on the cell surface) [16] and D486Y (Less common in patients with venous thrombosis) [17] are identified. It seems that, these variants can cause endothelial damage and microvascular thrombosis and manifest atypical hemolytic-uremic syndrome (aHUS) clinically. Microangiopathic hemolytic anemia in association with thrombocytopenia and acute kidney injury are features of typical aHU. Raina et al. (2022) in a systematic review showed that C3; CH50; AH50; and CFB were lower in aHUS as compared with the reference range [18].
Membrane cofactor protein (CD46) deficiency
It has been shown that deficiency in soluble or membrane-bound proteins of the complement system is mainly associated with systemic lupus erythematosus, infection, aHUS, and angioedema [19]. Membrane cofactor protein (MCP; CD46) is an inhibitor of complement activation, whose role in immune complex syndromes has recently been noticed [20]. This protein is involved in inactivating C3b and C4b by serine protease factor I (FI). More than 80 mutations associated with aHUS phenotype are identified in MCP [21,22,23,24], accounting for ∼10 − 15% of aHUS cases [25]. It seems necessary to perform related genetic evaluations in children with HUS who develop kidney failure.
Common variable immunodeficiency (CVID)
CD19 & CD81 deficiency
Mutation in CD19 gene causes symptoms similar to common variable immunodeficiency disorder (CVID) due to strong reduced in antibody production [26]. Recent case-reports presented kidney involvement in children with CD19 defect in the early years of their lives. Primary manifestations may include recurrent hematuria or meningitis and frequent respiratory infections as a result of antibody response to vaccination [26]. Findings such as IgA, IgG and IgM deficiencies and a kidney biopsy result of endocapillary proliferative glomerulonephritis and intense mesangial IgA deposits, can indicate IgA nephropathy in these patients [26]. It seems IgA nephropathy might not be attributable directly to CD19 deficiency since its functions accompany with CD21, CD81, and CD225 and they may also play a significant role [27,28,29]. Further investigations are needed in this field.
RAC2 deficiency
The large family of guanosine triphosphatases (GTPase) enzymes are involved in the hydrolysis of GTP nucleotides to guanosine diphosphate (GDP). The Rac family consists of Rac1, Rac2 (GTPase, exclusively expressed in hematopoietic cells), and Rac3, RhoG, and Rac associated GTPase. Rac2 is the major isoform in human neutrophils that regulate them in neutrophil chemotaxis [6, 30]. RAC2 deficiency impact on wide spectrum of immunity system such as innate arm and B- and T-cell migration, activation, development. Indeed, genetic defect in RAC2 gene can be associated with a wide range of immune symptoms such as soft-tissue infections which presented few weeks after birth [30]. W56X, D57N, P34H, E62K, N92T, G12R variants have been reported in the Rac2 subset [31]. Alkhairyet et al. reported in 2014 the homozygous loss-of-function mutation in the RAC2 gene, (W56X) causes: CVID, glomerulonephritis, coagulopathy, multiple hormone deficiencies potentially on the autoimmune basis and abnormalities of neutrophil granules [32]. Among patients reported to date due to RAC2 mutations [5, 33], recurrent sinopulmonary infections was the major clinical manifestation during their first admission. Despite the presence of various types in these patients, only 2 family cases (sister/brother) with W56X diagnosed with post streptococcal glomerulonephritis (PSGN) [34].
Sphingosine phosphate lyase insufficiency (SPLIS)
Sphingosine phosphate lyase insufficiency syndrome (SPLIS), caused by defect in SGPL1 gene, is a childhood syndrome that mainly manifests with steroid-resistant nephrotic syndrome (SRNS), primary adrenal insufficiency, rapid or insidious neurologic deterioration, immunodeficiency, and acanthosis [35]. Sphingosine-1-phosphate lyase (SPL) enzyme is involved in irreversible degradation of sphingolipid into phosphoethanolamine and hexadecimal and its removal [36]. Kidney involvement mainly manifests as steroid-resistant nephrotic syndrome, which can be congenital or occur during infancy, may progress into end-stage kidney disease in the first year of life, and seems to be correlated with a higher mortality rate [37]. In these patients, nephrotic syndrome may be the primary or isolated manifestation, and the outcome of kidney transplantation is largely unknown [38].
Combined immunodeficiency (CID)
Wiskott—Aldrich syndrome (WAS)
X-linked Wiskott–Aldrich syndrome (WAS), first recognized in 1937 by Dr. Alfred Wiskott, and then in 1957, confirmed by Robert Aldrich [39].it is estimated to involve 1–10 live births per million males. The WAS gene encodes a cytosolic protein known as WAS protein (WASp) and it expressed in myeloid, lymphoid, and hematopoietic stem cells (HSCs), which can lead to various clinical manifestations, but thrombocytopenia (X-linked thrombocytopenia [XLT]), eczema, and recurrent infections with increased risk of lymphoid malignancies, autoimmune disorders or congenital neutropenia (X-lined neutropenia [XLN]) are classic phenotype of WAS [40, 41]. The patients with thrombocytopenia show a different range of symptoms from a mild petechiae and purpura to serious intracranial and/or intestinal bleeding, which lead to death in 4–10%. The mean platelet volume (MPV) in WAS is often < 5 fL, so it can reach < 2 fL in the patients with severe bleeding symptoms. In addition, this disease is usually misdiagnosed with immune thrombocytopenia (ITP), and it should be noted that the WAS hallmark is micro thrombocytopenia (small platelets) [41]. Eczema can affect 75% of these patients, and usually shows itself as refractory and the patient is not able to treat it quickly [42]. Recent studies reported renal involvements including IgA nephropathy (IgAN), membranoproliferative glomerulonephritis (MPGN) and interstitial nephritis in 3.5–19% of the patients, often progressing to renal failure and require transplantation [40, 43,44,45]. Although various studies have investigated the role of different markers in the occurrence of renal complications in WAS, no specific etiology has been elucidated [46,47,48,49].
Interleukin 6 cytokine family signal transducer
Interleukin-6 signal transducer (IL6ST) encodes the GP130 protein. In pro-inflammatory conditions, GP130 signaling IL6 cytokine. IL-6 family cytokines are involved in the regulation of the hepatic acute-phase reaction, in B-cell stimulation, in the regulation of the balance between regulatory and effector T cells, in metabolic regulation, and in many neural functions [50]. Biallelic loss-of-function IL6ST variants cause autosomal recessive hyper-IgE syndrome or a variant of the Stuve–Wiedemann syndrome (skeletal dysplasia, lung dysfunction, congenital thrombocytopenia, dermatitis, renal abnormalities, and defective acute-phase response) [34]. Chen et al. (2020) reported a Saudi Arabic family with two fetuses with mutations in IL6S and were homozygous for c.841C > T; p.Arg281*.The first fetus had short femora (less than fifth centile), bowed tibia, multicystic dysplastic right kidney, dilated cisterna magna, and a small chest and died 3 h after delivery [34].
Schimke immuno-osseous dysplasia
Schimke Immuno-Osseous Dysplasia (SIOD) is an autosomal recessive multi-system disorder, with the genetic cause of biallelic loss-of-function mutation in SMARCAL1 (SWI/SNF-related, matrix-associated, actin-dependent regulator of chromatin, subfamily a-like 1) gene [8]. The incidence rate of SIOD is 1 per 1–3 million live births and is clinically manifested by growth failure, spondyloepiphyseal dysplasia, lymphopenia, and proteinuria. Hypothyroidism, cerebral ischemia, and bone marrow failure were also reported in half of these patients [7]. Nephropathy in SIOD children is described as progressive and steroid-resistant [51]. The pathophysiology of nephropathy in SIOD remained unknown but the role of the SMARCAL1 gene in the renal progenitor population is suggested in the study of Dekel et al. [52]. In this study, according to the neonatal/adult murine kidney, it is explained that peak levels of SMARCAL1 and localization in glomerular podocytes can explain proteinuria and progressive nephropathy in SIOD children.
Type-1 interferonopathies
Pediatric systemic lupus erythematosus due to DNASE1L3 deficiency
The prevalence and incidence of lupus in children is not precisely known due to different age definitions [35]. But since the role of gender and sex hormones in the occurrence of lupus is less prominent at a young age, the role of genetics in this field becomes more prominent. The disease usually involves skin, musculoskeletal system, and kidneys, of which the latter is the determinative manifestation for prognosis [53]. Al-Mayouf et al. (2011) investigated six families with pediatric lupus and found a role for DNASE1L3 loss-of-function mutations in these patients [36]. Loss-of-function mutations in DNASE1L3 cause high disease activity with variable degrees of renal involvement in children. Also, In the study by Kisla et al. (2021) a child with DNASE1L3 deficiency who suffered from urticarial skin lesions, frequent hemoptysis, and kidney involvement, was finally diagnosed as this rare monogenic lupus [53].
Primary immune regulatory disorders
Immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome
The significant number of new cases of this syndrome indicates that Immune Dysregulation, Polyendocrinopathy, Enteropathy, X-linked Syndrome (IPEX) is a rare disease that is underestimated. IPEX is characterized by immune dysregulation, polyendocrinopathy, enteropathy, and an X-linked inheritance pattern. Mutations related to the fork head box p3 (FOXP3) transcription factor, which is the main gene of regulatory T-cells (Treg), are involved in the development of this disease in interaction with environmental factors. Various studies have investigated the clinical manifestations of these patients. Some of These manifestations include autoimmune enteropathy, Type-1 diabetes mellitus, Dermatitis, and frequent infections. In the study of Rao et al. [54] (2007) and Moudgil et al. [55] (2007), renal involvement in these patients was reported as Membranous glomerulonephritis (MGN). Other reported kidney involvement in these patients were Renal failure, tubulointerstitial nephritis (TIN) and nephrotic syndrome [56].
Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED)
Mutations in the gene encoding immune regulatory (AIRE) protein cause autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED) with recessive or dominant autosomal inheritance. In this syndrome, the patient suffers from chronic Candida infection in childhood and then autoimmune hypoparathyroidism and autoimmune primary adrenocortical failure [57].If there are two of these three components or a previous diagnosis in the patient's sibling, this disease is raised. Tissue-specific antibodies and cytokines created during this syndrome can rarely cause kidney involvement and autoimmune TIN [58]. The symptoms of TIN are non-specific and sometimes less clear, but unexplained fever is one of its notable features [59]. Increased creatinine, ESR, abnormal urinalysis, proteinuria or decreased kidney function without abnormalities in urinalysis can be a clue to suspect this syndrome in susceptible patients (58).
Conclusion
Inborn errors of immunity are multi-system disorders and require interdisciplinary approach for optimal diagnosis and management. Among others, the characteristics of kidney and urinary system in IEIs have remained obscure and need more consideration by the pediatrics, nephrologists and immunologists. As illustrated in Fig. 1, a thorough evaluation of kidney and urinary system in patients with abnormal initial renal screening should be performed concomitantly with immunology workup. This evaluation is divided in primary and secondary steps and will be helpful in earlier clinical diagnosis of the underlying IEIs before the result of the genetic study become ready. In this review, we tried to summarize the IEIs reported to manifest renal abnormalities, however, the list provided here is according to the well-established IEIs and certainly in the future it will be extended.
Data Availability
Data available within the article.
Abbreviations
- IEI:
-
Inborn error of immunity
- GOF:
-
Gain-of-function
- FI:
-
Factor I
- CFH:
-
Complement factor H
- aHUS:
-
Atypical hemolytic-uremic syndrome
- MCP:
-
Membrane cofactor protein
- IgAN:
-
Immunoglobulin A nephropathy
- SIOD:
-
Schimke Immuno-Osseous Dysplasia
- FHR1–5:
-
Factor H-related proteins
- WAS:
-
Wiskott–Aldrich syndrome
- WASp:
-
WAS protein
- HSCs:
-
Hematopoietic stem cells
- XLT:
-
X-linked thrombocytopenia
- XLN:
-
X-lined neutropenia
- MPV:
-
Mean platelet volume
- MPGN:
-
Membranoproliferative Glomerulonephritis
- CVID:
-
Common variable immunodeficiency disorder
- C3G:
-
C3 glomerulopathy
- GTPase:
-
Guanosine Triphosphatases
- GDP:
-
Guanosine Diphosphate
- PSGN:
-
Poststreptococcal glomerulonephritis
- JAK/STAT:
-
Janus kinase signal transducers and activators of transcription pathway
- IUIS:
-
International Union of Immunological Societies
- MGN:
-
Membranous glomerulonephritis
- IPEX:
-
Immune Dysregulation, Polyendocrinopathy, Enteropathy, X-linked Syndrome
- FOXP3:
-
Fork head box P3
- Treg:
-
Regulatory T-cell
- SPLIS:
-
Sphingosine phosphate lyase insufficiency syndrome
- SRNS:
-
Steroid resistant nephrotic syndrome
- SPL:
-
Sphingosine-1-phosphate lyase
References
Bousfiha A, Moundir A, Tangye SG, Picard C, Jeddane L, Al-Herz W et al (2022) The 2022 Update of IUIS Phenotypical Classification for Human Inborn Errors of Immunity. J Clin Immunol 42(7):1508–1520
Tangye SG, Al-Herz W, Bousfiha A, Cunningham-Rundles C, Franco JL, Holland SM et al (2022) Human Inborn Errors of Immunity: 2022 Update on the Classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol 42(7):1473–1507
Tangye S, Al-Herz W. Bous ha A, Chatila T, Cunningham-Rundles C, Etzioni A, et al. Human inborn errors of immunity: 2019 update on the classification from the International Union of Immunological Societies Expert Committee. Journal of clinical immunology. 2020;40(1):24–64.
Bousfiha A, Jeddane L, Picard C, Al-Herz W, Ailal F, Chatila T et al (2020) Human Inborn Errors of Immunity: 2019 Update of the IUIS Phenotypical Classification. J Clin Immunol 40(1):66–81
Sharapova SO, Haapaniemi E, Sakovich IS, Kostyuchenko LV, Donkó A, Dulau-Florea A et al (2019) Heterozygous activating mutation in RAC2 causes infantile-onset combined immunodeficiency with susceptibility to viral infections. Clin Immunol 205:1–5
Nagase M, Kurihara H, Aiba A, Young MJ, Sakai T (2016) Deletion of Rac1GTPase in the myeloid lineage protects against inflammation-mediated kidney injury in mice. PLoS ONE 11(3):e0150886
Malhotra R, Sharma M, Dwivedi A, Kalra S (2021) A Case of Schimke Immunoosseous Dysplasia Caused by Large Deletion of SMARCAL1 Gene. Indian journal of endocrinology and metabolism 25(4):358–360
Castellano-Martinez A, Acuñas-Soto S, Varga-Martinez R, Rodriguez-Gonzalez M, Mora-Lopez F, Iriarte-Gahete M et al (2022) Different Phenotypes of Schimke Immuno-Osseous Dysplasia (SIOD) in Two Sisters with the Same Mutation in the SMARCAL1 Gene. Endocr Metab Immune Disord Drug Targets 22(8):888–894
Guo W-y, Sun L-j, Dong H-r, Wang G-q, Xu X-y, Zhao Z-r et al (2021) Glomerular Complement Factor H-Related Protein 5 is Associated with Histologic Injury in Immunoglobulin A Nephropathy. Kidney International Reports 6(2):404–413
Márquez-Tirado B, Gutiérrez-Tenorio J, Tortajada A, Lucientes Continente L, Caravaca-Fontán F, Malik TH et al (2022) Factor H-Related Protein 1 Drives Disease Susceptibility and Prognosis in C3 Glomerulopathy. J Am Soc Nephrol 33(6):1137–1153
Renner B, Laskowski J, Poppelaars F, Ferreira VP, Blaine J, Antonioli AH, et al. Factor H related proteins modulate complement activation on kidney cells. Kidney International. 2022.
Medjeral-Thomas NR, Lomax-Browne HJ, Beckwith H, Willicombe M, McLean AG, Brookes P et al (2017) Circulating complement factor H–related proteins 1 and 5 correlate with disease activity in IgA nephropathy. Kidney Int 92(4):942–952
Zhu L, Guo W-y, Shi S-f, Liu L-j, Lv J-c, Medjeral-Thomas NR, et al. Circulating complement factor H–related protein 5 levels contribute to development and progression of IgA nephropathy. Kidney international. 2018;94(1):150–8.
Delvaeye M, Noris M, De Vriese A, Esmon CT, Esmon NL, Ferrell G et al (2009) Thrombomodulin mutations in atypical hemolytic–uremic syndrome. N Engl J Med 361(4):345–357
Norlund L, Zöller B, Öhlin A-K (1997) A novel thrombomodulin gene mutation in a patient suffering from sagittal sinus thrombosis. Thromb Haemost 78(10):1164–1166
Kunz G, Ohlin A-K, Adami A, Zöller B, Svensson P, Lane DA (2002) Naturally occurring mutations in the thrombomodulin gene leading to impaired expression and function. Blood, The Journal of the American Society of Hematology 99(10):3646–3653
Öhlin A-K, Marlar RA (1999) Thrombomodulin gene defects in families with thromboembolic disease–a report on four families. Thromb Haemost 81(03):338–344
Raina R, Sethi SK, Dragon-Durey M-A, Khooblall A, Sharma D, Khandelwal P et al (2022) Systematic review of atypical hemolytic uremic syndrome biomarkers. Pediatr Nephrol 37(7):1479–1493
Sullivan KE. 10 - Inherited Complement Deficiencies. In: Pyeritz RE, Korf BR, Grody WW, editors. Emery and Rimoin' s Principles and Practice of Medical Genetics and Genomics (Seventh Edition): Academic Press; 2023. p. 303–19.
Liszewski MK, Atkinson JP (2021) Membrane cofactor protein (MCP; CD46): deficiency states and pathogen connections. Curr Opin Immunol 72:126–134
Bruel A, Kavanagh D, Noris M, Delmas Y, Wong EK, Bresin E et al (2017) Hemolytic uremic syndrome in pregnancy and postpartum. Clin J Am Soc Nephrol 12(8):1237–1247
Gaggl M, Aigner C, Csuka D, Szilágyi Á, Prohászka Z, Kain R et al (2018) Maternal and fetal outcomes of pregnancies in women with atypical hemolytic uremic syndrome. J Am Soc Nephrol 29(3):1020–1029
Phillips E, Westwood J, Brocklebank V, Wong E, Tellez J, Marchbank K et al (2016) The role of ADAMTS-13 activity and complement mutational analysis in differentiating acute thrombotic microangiopathies. J Thromb Haemost 14(1):175–185
Zhang T, Lu J, Liang S, Chen D, Zhang H, Zeng C et al (2016) Comprehensive analysis of complement genes in patients with atypical hemolytic uremic syndrome. Am J Nephrol 43(3):160–169
Osborne AJ, Breno M, Borsa NG, Bu F, Frémeaux-Bacchi V, Gale DP et al (2018) Statistical validation of rare complement variants provides insights into the molecular basis of atypical hemolytic uremic syndrome and C3 glomerulopathy. J Immunol 200(7):2464–2478
Van Zelm MC, Smet J, Adams B, Mascart F, Schandené L, Janssen F et al (2010) CD81 gene defect in humans disrupts CD19 complex formation and leads to antibody deficiency. J Clin Investig 120(4):1265–1274
van Zelm MC, Reisli I, van der Burg M, Castaño D, van Noesel CJM, van Tol MJD et al (2006) An Antibody-Deficiency Syndrome Due to Mutations in the CD19 Gene. N Engl J Med 354(18):1901–1912
Zelm MCv, Reisli I. CD19 Deficiency due to Genetic Defects in the CD19 and CD81 Genes. Humoral Primary Immunodeficiencies: Springer; 2019. p. 83–95.
Wentink MW, van Zelm MC, van Dongen JJ, Warnatz K, van der Burg M (2018) Deficiencies in the CD19 complex. Clin Immunol 195:82–87
Sharapova SO, Haapaniemi E, Sakovich IS, Kostyuchenko LV, Donkó A, Dulau-Florea A et al (2019) Heterozygous activating mutation in RAC2 causes infantile-onset combined immunodeficiency with susceptibility to viral infections. Clin Immunol 205:1–5
Lougaris V, Baronio M, Gazzurelli L, Benvenuto A, Plebani A (2020) RAC2 and primary human immune deficiencies. J Leukoc Biol 108(2):687–696
Alkhairy OK, Rezaei N, Graham RR, Abolhassani H, Borte S, Hultenby K, et al. RAC2 loss-of-function mutation in 2 siblings with characteristics of common variable immunodeficiency. The Journal of allergy and clinical immunology. 2015;135(5):1380–4.e1–5.
Bahrami S, Arshi S, Nabavi M, Bemanian MH, Fallahpour M, Rezaeifar A et al (2022) Progressive multifocal leukoencephalopathy in a patient with novel mutation in the RAC2 gene: a case report. J Med Case Reports 16(1):235
Alkhairy OK, Rezaei N, Graham RR, Abolhassani H, Borte S, Hultenby K, et al. RAC2 loss-of-function mutation in 2 siblings with characteristics of common variable immunodeficiency. Journal of Allergy and Clinical Immunology. 2015;135(5):1380–4. e5.
Bektas M, Allende ML, Lee BG, Chen W, Amar MJ, Remaley AT et al (2010) Sphingosine 1-phosphate lyase deficiency disrupts lipid homeostasis in liver. J Biol Chem 285(14):10880–10889
Serra M, Saba JD (2010) Sphingosine 1-phosphate lyase, a key regulator of sphingosine 1-phosphate signaling and function. Adv Enzyme Regul 50(1):349–362
Pournasiri Z, Madani A, Nazarpack F, Sayer JA, Chavoshzadeh Z, Nili F, Tran P, Saba JD, Jamee M (2023) Sphingosine phosphate lyase insufficiency syndrome: a systematic review. World journal of pediatrics : WJP 19(5):425–437
Weaver KN, Sullivan B, Hildebrandt F, Strober J, Cooper M, Prasad R, et al. Sphingosine phosphate lyase insufficiency syndrome. GeneReviews®[Internet]. 2020.
Naseem A, Steinberg Z, Cavazza A (2022) Genome editing for primary immunodeficiencies: a therapeutic perspective on Wiskott-Aldrich syndrome. Front Immunol 13:966084
Albert MH, Bittner TC, Nonoyama S, Notarangelo LD, Burns S, Imai K et al (2010) X-linked thrombocytopenia (XLT) due to WAS mutations: clinical characteristics, long-term outcome, and treatment options. Blood 115(16):3231–3238
Hosahalli Vasanna S, Pereda MA, Dalal J (2021) Clinical features, cancer biology, transplant approach and other integrated management strategies for wiskott-aldrich syndrome. J Multidiscip Healthc 14:3497–3512
Ochs HD, Thrasher AJ. The Wiskott-Aldrich syndrome. The Journal of allergy and clinical immunology. 2006;117(4):725–38; quiz 39.
DeSanto NG, Sessa A, Capodicasa G, Meroni M, Capasso G, Esposito L et al (1988) IgA glomerulonephritis in Wiskott-Aldrich syndrome. Child Nephrol Urol 9(1–2):118–120
Hoshino A, Shimizu M, Matsukura H, Sakaki-Nakatsubo H, Nomura K, Miyawaki T et al (2014) Allogeneic bone marrow transplantation appears to ameliorate IgA nephropathy in a patient with X-linked thrombocytopenia. J Clin Immunol 34(1):53–57
Liu CH, Wu KH, Lin TY, Wei CC, Lin CY, Chen XX et al (2013) Wiskott-Aldrich syndrome with IgA nephropathy: a case report and literature review. Int Urol Nephrol 45(5):1495–1500
Bosticardo M, Marangoni F, Aiuti A, Villa A, Grazia RM (2009) Recent advances in understanding the pathophysiology of Wiskott-Aldrich syndrome. Blood 113(25):6288–6295
Marx D, Dupuis A, Eckly AE, Molitor A, Olagne J, Touchard G, et al. A gain-of-function variant in the Wiskott-Aldrich syndrome gene is associated with a MYH9-related disease-like syndrome. Blood advances. 2022.
Kakio Y, Uchida HA, Kitagawa M, Arata Y, Kato A, Inoue-Torii A et al (2018) IgA nephropathy complicated with x-linked thrombocytopenia. Acta Med Okayama 72(3):301–307
Tilley FC, Gallon M, Luo C, Danson CM, Zhou J, Cullen PJ. Retromer associates with the cytoplasmic amino-terminus of polycystin-2. Journal of cell science. 2018;131(11).
Rose-John S (2018) Interleukin-6 family cytokines. Cold Spring Harb Perspect Biol 10(2):a028415
Lippner E, Lücke T, Salgado C, Boerkoel C, Lewis DB. Schimke Immunoosseous Dysplasia. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, et al., editors. GeneReviews(®). Seattle (WA): University of Washington, Seattle Copyright © 1993–2022, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved.; 1993.
Dekel B, Metsuyanim S, Goldstein N, Pode-Shakked N, Kovalski Y, Cohen Y et al (2008) Schimke immuno-osseous dysplasia: expression of smarcal1 in blood and kidney provides novel insight into disease phenotype. Pediatr Res 63(4):398–403
Kisla Ekinci RM, Balci S, Ozcan D, Atmis B, Bisgin A (2021) Monogenic lupus due to DNASE1L3 deficiency in a pediatric patient with urticarial rash, hypocomplementemia, pulmonary hemorrhage, and immune-complex glomerulonephritis. Eur J Med Genet 64(9):104262
Rao A, Kamani N, Filipovich A, Lee SM, Davies SM, Dalal J et al (2007) Successful bone marrow transplantation for IPEX syndrome after reduced-intensity conditioning. Blood 109(1):383–385
Moudgil A, Perriello P, Loechelt B, Przygodzki R, Fitzerald W, Kamani N (2007) Immunodysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome: an unusual cause of proteinuria in infancy. Pediatric nephrology (Berlin, Germany) 22(10):1799–1802
Barzaghi F, Passerini L, Bacchetta R (2012) Immune dysregulation, polyendocrinopathy, enteropathy, x-linked syndrome: a paradigm of immunodeficiency with autoimmunity. Front Immunol 3:211
Domingues-Ferreira M, Vasconcelos DdM, Bezerra TdA, Bertolini DL, Barros NC, Auler ME. Autoimmune polyendocrinopathy–candidiasis–ectodermal dystrophy (APECED) and esophageal rupture by candida infection: A case report and review. Journal of Medical Mycology. 2022;32(3):101293.
Kluger N, Kataja J, Aho H, Rönn A-M, Krohn K, Ranki A (2014) Kidney involvement in autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy in a Finnish cohort. Nephrol Dial Transplant 29(9):1750–1757
Perheentupa J (2006) Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. J Clin Endocrinol Metab 91(8):2843–2850
Acknowledgements
Mahnaz Jamee is a recipient of the European Academy of Allergy and Clinical Immunology (EAACI) Research Long-term Fellowship 2023 Grant.
Funding
This research has received no funding.
Author information
Authors and Affiliations
Contributions
MJ had the idea for the article; AZA, MMA and MJ performed the literature search and wrote the primary draft, AS, AZA, MMA, TM, MMi, MMo, SS, MT and MJ drafted and/or critically revised the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shajari, A., Zare Ahmadabadi, A., Ashrafi, M.M. et al. Inborn errors of immunity with kidney and urinary tract disorders: a review. Int Urol Nephrol 56, 1965–1972 (2024). https://doi.org/10.1007/s11255-023-03907-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03907-4