Abstract
Background
Postinfectious glomerulonephritis with C3-dominant glomerular deposition (C3-PIGN) involves C3-dominant glomerular deposition without immunoglobulin. Atypical C3-PIGN involves persistent hypocomplementemia. We investigated the clinical features and explored complement-related gene mutations in atypical PIGN patients.
Methods
We enrolled atypical C3-PIGN patients and collected data regarding the clinical presentation and pathological characteristics and follow-up data. We measured the levels of complement associated antibodies and performed whole-exome sequencing (WES) to detect mutations in complement-related genes.
Results
The analysis included six atypical C3-PIGN patients. All patients were antistreptolysin-O (ASO) positive. All patients had varying degrees of hematuria, and four patients had proteinuria. None of the patients were positive for complement-related antibodies. All patients possessed mutations of genes related to the complement pathway, including alternative complement pathway genes—CFI, CFH, CFHR3, CFHR5; the lectin pathway gene—MASP2; and the common complement pathway gene—C8A. The rare variant of CFHR3 has been reported in C3 glomerulonephritis. During 56–73 months of follow-up, the levels of urine markers in three patients recovered within 6 months, and the remaining patients had abnormal urine test results over 12 months. Patients who received glucocorticoid therapy recovered faster.
Conclusions
Our study suggested that complement-related gene mutations may be an important cause of persistent hypocomplementemia in atypical C3-PIGN patients. In addition to variations in alternate pathway-related genes, we also found variations in lectin pathway-related genes, especially MASP2 genes. Although the overall prognosis was good, atypical C3-PIGN patients exhibited a longer period for recovery. Our results suggested that atypical C3-PIGN patients should receive more medical attention and need testing for mutations in complement-related genes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute postinfectious glomerulonephritis (PIGN) is a complication of streptococcal and other infections and can occur in both children and adults [1, 2]. The primary clinical manifestation of PIGN is acute nephritis syndrome [3]. In PIGN, glomerular injury is mediated by a host immune response that is triggered by an infectious agent. The activation of complement plays a pivotal role in PIGN. Hypocomplementemia is an important feature of active PIGN, which is characterized by low serum levels of complement C3 and normal levels of C4, thus suggesting that the infection induces the activation of the complement system.
The primary histological manifestation of PIGN during the acute phase is proliferative lesions and exudative lesions in the glomerular capillaries, while the recovery period is associated with proliferative lesions in the glomerular mesangial cells. There are two PIGN immunophenotypes: one type is Ig + C3-PIGN, which involves glomerular deposition of immunoglobulin G (or IgA) and C3, while the other is C3-PIGN, which is mainly characterized by the glomerular deposition of C3, with or without weakly positive immunoglobulin results [4]. C3-PIGN exhibits similar histological and immunofluorescence characteristics to C3 glomerulonephritis (C3GN).
Most patients with C3-PIGN have an excellent prognosis. In the majority of cases, hypocomplementemia resolves within 6–8 weeks; hematuria and proteinuria are likely to resolve within weeks or months. This trajectory is in stark contrast with the poor long-term outcomes of C3GN patients, which often include persistent hypocomplementemia, proteinuria and hematuria. It is currently believed that the complement system in patients with C3GN is abnormally regulated and that this pathology is very difficult to correct. However, long-term follow-up observations have shown that few patients with C3-PIGN are affected by persistent hypocomplementemia and kidney damage [5,6,7,8]. This is an atypical form of C3-PIGN and is very difficult to distinguish from C3GN [9].
Previous studies indicate that C3GN patients have various complement-related gene mutations, including mutations in the C3, membrane cofactor protein (MCP), thrombomodulin (THBD), complement factor H (CFH), complement factor I (CFI), complement factor B (CFB) and complement factor H-related proteins (CFHR) genes [10,11,12]. These mutated genes caused abnormal regulation of the complement system. Due to the similar clinical and pathological features between C3GN and atypical C3-PIGN patients, we hypothesize that atypical C3-PIGN patients may carry mutations in complement-related genes. In this study, we investigated the clinicopathological characteristics and long-term prognosis of atypical C3-PIGN patients. In addition, we performed whole exon sequencing (WES) to identify the mutations in all genes related to the complement pathway.
Materials and methods
Patients
A total of 74 patients with C3-PIGN who had been registered in the Nanjing Glomerulonephritis Registry at the National Clinical Research Center of Kidney Diseases, Jinling Hospital, from January 2010 to December 2018 were included in this study using the diagnostic criteria as follows: (1) history of preceding infection; (2) hematuria with or without proteinuria(> 0.4 g/24 h); (3) decreased serum C3 level; (4) characteristics of postinfectious glomerulonephritis—(a) proliferative glomerulonephritis on light microscopy (LM); (b) C3 deposition without immunoglobulin and C1q on immunofluorescence (IF) microscopy; (c) ‘hump-like’ subepithelial electron-dense deposits on electron microscopy (EM).
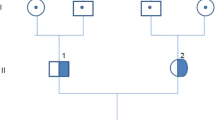
The atypical C3-PIGN was identified as C3-PIGN combined with hypocomplementemia lasting more than 12 months. Six patients were diagnosed with atypical C3-PIGN (Supplementary Fig. 1). We collected a range of baseline clinical and pathological data, measured the levels of complement-related antibodies and performed WES. All patients provided informed written consent. The study adhered to the guidelines of the Declaration of Helsinki and was approved by the Local Ethics Committee of National Clinical Research Center for Kidney Diseases, Jinling Hospital (2022DZKY-060-01, Nanjing, China).
All 6 atypical C3-PIGN patients were followed up regularly. All patients were followed-up at 1, 3, 6 and 12 months after discharge and twice a year after 12 months. The follow-up time ranged from 56 to 73 months.
Renal pathological changes
The renal biopsy tissues were examined by light microsope (LM), Immunofluorescence (IF) and electron microscope (EM). The paraffin-embedded tissue sections were stained with hematoxylin–eosin (HE), periodic acid-Schiff (PAS), methenamine silver, and Masson trichrome. A direct immunofluorescence method was used to detect IgG, IgA, IgM, C3c, C4c, C1q, mannan-binding lectin associated serine protease-2 (MASP2) and fibrin expression. The EM tissue was first fixed with 3.75% cold glutaraldehyde, then fixed with 1% osmium tetroxide and embedded in resin. Ultrathin sections were cut at 70–80 nm, double stained with uranium acetate and lead citrate, and examined with a Hitachi 7500 transmission electron microscope.
Renal biopsy specimens were examined by two renal pathologists. The pathological score of each patient's kidney biopsy specimen was determined. According to the pathological classification criteria, acute tubular injury (ATI) and interstitial fibrosis and renal tubular atrophy (IFTA) were defined based on the percentage of lesions in the cortical area. Crescents were described according to the number of lesions. Immunofluorescence intensity was semiquantitatively graded as follows: −, trace, 1 + , 2 + , and 3 + .
Complement and complement-related antibody testing
Serum C3 and C4 levels were measured by nephelometry (Beckman Coulter, California, USA). C3 nephritic factor (C3NeF) level was evaluated by hemolytic assays using preactivated sheep erythrocytes [13, 14], and the presence of Factor H autoantibody was detected by Enzyme Linked Immunosorbent Assay (ELISA) [15, 16]. Normal ranges were defined as follows: C3, 80–180 mg/dl [mean ± 2 standard deviations (SD)]; C4, 10–40 mg/dl (mean ± 2 SD). All functional assays were repeated three times.
Whole-exome sequencing
Library preparations and sequencing
Genomic DNA was extracted from patients using a DNeasy Blood & Tissue Kit (QIAGEN). Exome capture was performed using SureSelect Human All Exon V6 (Agilent Technologies) according to the manufacturer’s instructions. The concentration of the libraries was measured by Qubit® 2.0 Fluoromete. The quality and size of the libraries were measured by a 2100 Bioanalyzer High Sensitivity DNA Assay according to the reagent kit guide. For Illumina sequencing, the qualified libraries were subjected to 2 × 150 bp paired-end sequencing on the Illumina HiSeq X-ten platform (Illumina).
Variant calling and annotation
Variants [single-nucleotide variants (SNVs) and indels] were genotyped from recalibrated BAM files using the multisample processing mode of the Unified Genotyper tool from GATK. Then, VQSR (Variant Quality Score Recalibration) was used to reduce the number of false positives during variant calling. Copy number variation was identified by XHMM (eXome Hidden Markov Model) v1.0. SNVs and indels were annotated using ANNOVAR software against multiple databases, including HGVS variant description, population frequency, disease or phenotype and variant functional prediction. Screening for CFH, MCP, CFI, CFB, C3 and THBD coding sequences was performed by amplicon-based next-generation sequencing [14]. Rare functional variants (missense, nonsense, indel, or splicing variants with minor allele frequency, MAF < 0.001 in 1000 Genomes and ExAC databases) were selected and defined as likely pathogenetic or pathogenetic when published functional studies were available.
We used SIFT, PolyPhen-2 and Mutation Taster to predict the functional effects of each missense and amino acid substitution. To predict the three-dimensional protein structure and the internal molecular segments, we constructed a mimetic human GDF3 protein by using the SWISS–MODEL (http://swissmodel.expasy.org) server.
Results
Clinical features of atypical C3-PIGN patients
The six patients included four males and two females; three patients were adults. Three of these patients had a history of prodromal infection in the upper respiratory tract, and the time from infection to the appearance of acute nephritis syndrome in each patient was 13 days, 14 days, and 18 days. The levels of serum creatinine (Scr) at renal biopsy ranged from 0.55 to 2.7 mg/dl. These patients had varying degrees of hematuria. Four patients were positive for proteinuria, and two patients experienced proteinuria > 1 g/24 h. All patients were ASO positive, one patient was antinuclear antibody (ANA) positive, and one patient was positive for the hepatitis B antigen. Three patients had hypertension, and all patients had a normal serum level of C4 (Table 1).
Three patients were treated with corticosteroids, and two of them additionally received angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB) therapy. The other three patients were treated conservatively by renin–angiotensin system blockade alone and did not receive steroids or other forms of immunosuppressive therapy.
The levels of urinary markers in three patients returned to normal levels within 6 months. However, the abnormal levels of urinary markers in patients 1, 4 and 5 returned to normal after 8 months, 18 months and 27 months, respectively (Fig. 1). In general, patients did well with no significant decline in renal function, both over the short and long terms. The serum creatinine levels in patient 2 returned to normal by the 6 month follow-up. Normal renal function was maintained in the other five patients.
The plasma levels of C3 in 2 patients had recovered by 12 month follow-up. Four patients had hypocomplementemia, with a duration ranging from 12 to 60 months (Fig. 2). The plasma C3 level was normal in patient 1 after repeated testing at the 24-month follow-up but had become substantially reduced by the 30 month follow-up; this was complicated by proteinuria and microscopic hematuria.
Pathological features of atypical C3-PIGN
The pathological features of atypical C3-PIGN patients are shown in Table 2. Four patients exhibited mesangial proliferative glomerulonephritis; numerous infiltrating neutrophils were observed in the glomerular capillaries, 1 patient showed mesangial proliferation with segmental membranoproliferative glomerulonephritis, and the remaining patients had mesangial proliferative with segmental endocapillary proliferative glomerulonephritis. Immunofluorescence analysis further revealed C3 deposition in the mesangial area and the capillary wall in 5 patients; the other patient showed intense C3 (3 +) staining with mild IgA ( +) staining. EM revealed a hump-like subepithelium and electron dense deposits of mesangial cells in all patients. Four patients exhibited intramembranous deposits, and 3 patients had subendothelial deposits (Fig. 3).
Light microscopy (LM), Immunofluorescence microscopy (IF) and electron microscopy (EM) in atypical C3-PIGN. a Shows a predominantly mesangial proliferative with segmental membranoproliferative glomerulonephritis (PAS 400 ×), b shows C3 deposited along the glomerular capillary and mesangial area (IF 400 ×), c shows C4 (trace) segmental deposited along the glomerular capillary and mesangial area (IF 400 ×), d–e EM showing subepithelial (thick black arrow), mesangial (thick white arrow)and subendothelial deposits (white arrow). f Shows a predominantly mesangial proliferative with segmental endocapillary proliferative glomerulonephritis (PAS 400 ×), g shows C3 deposited along the glomerular capillary and mesangial area (IF 400 ×), (h, i) EM showing subepithelial (thick black arrow) and intramembranous deposits (white arrow)
Complement-related antibody testing
We detected C3NeF, factor H, and anti-factor H in all patients, and none were positive.
The identification of mutations in complement-related genes
Six patients possessed mutations in complement-related genes. Seven mutations were identified in four genes in the alternative complement pathway. We identified two missense mutations in the CFH gene (p. V837I and p. I551T), one mutation in the CFHR3 gene (p. R142C), one mutation in the CFHR5 gene (p. G145E) and three mutations in the CFI gene (p. R399H, p. R406H and p.R414H). We also identified two mutations (p. D371Y and p. H155R) in the MASP2 gene, which is a gene that is involved in the lectin pathway, and one mutation (p. R485L) in C8A, which is a common gene that encodes the alpha subunit of C8 and participates in the formation of the membrane attack complex (Table 3).
All of these mutations had been reported previously and were heterozygous variants. In addition, all of these mutations were located in the coding region of their respective genes and were missense mutations. Polyphen-2, SIFT and MutationTaster software were used to predict the functional effect of these mutations; the effects of the eight complement-related gene mutations on MASP2, CFHR3, C8A, MASP2, and CFI proteins were predicted to be damaging or probably damaging (Table 3).
rs12711521 in MASP2 was identified in four patients; rs2273343 in MASP2 was only identified in one patient. Four patients had mutations in more than two complement-related genes. Three mutations found in Patient 6 were also previously reported in patients with C3GN; therefore, these mutations were associated with an increased risk of C3GN [17]. Patient 2 possessed C8A and MASP2 mutations; Patient 3 possessed CFH and MASP2 mutations, and Patient 4 possessed CFI and MASP2 mutations.
We detected MASP2 mutations in 5 atypical C3-PIGN patients. MASP2 is a key protein involved in the lectin pathway of complement. To further observe the activation of the lectin pathway, we stained for MASP2 expression in kidney biopsy tissue obtained from all patients. Patient 1 and patient 3 showed 2 + , and patient 2 showed 1 + positive deposition in mesangial areas and capillaries. The other patients were negative (Fig. 4).
rs12711521 leads to the change of aspartic acid 371 to tyrosine (p.D371Y). We demonstrated that the 3D structure of MASP2 included rs12711521. We found that the mutated tyrosine 371 (green color) is located in the CCP2 domain, which is encoded by exon 9, and close to the binding site of C4, which may influence the secondary interaction with C4 (Fig. 5).
Three-dimensional models for the MASP2 protein was based on Protein Data Bank (PDB ID 5JPM) and Key amino acids with the GWAS association (rs12711521) is highlighted. Graphical representations of the 3D models were prepared using the PyMOL Molecular Graphics System, Version 2.5.2. MASP2 is shown in blue and white color, C4 is shown in orange and pink color. The rs12711521 (p.Asp371Tyr) is shown in green color and close to the binding site of MASP2 and C4
Discussion
Most patients with C3-PIGN exhibit a relatively benign disease course, and hypocomplementemia is self-limiting. Approximately 8.8% of C3-PIGN patients exhibit persistent hypocomplementemia accompanied by abnormal urinary parameters; therefore, these atypical C3-PIGN patients need special attention. We found that atypical C3-PIGN patients had heterogeneous phenotypes and exhibited different ranges of microscopic hematuria and proteinuria. The duration of abnormalities in the levels of urinary markers also varied among these patients. Glucocorticoid therapy can significantly reduce the recovery time needed to resolve abnormalities in urinary test results and reverse hypocomplementemia, thus suggesting that immunosuppressive therapy may help to ameliorate the immune response in these patients.
The predominant histological changes associated with atypical C3-PIGN were proliferative mesangial lesions. Some patients have segmental proliferative lesions. In addition to subepithelial hump-like electron-dense deposits, mesangial, subendothelial and intramembranous deposits were also evident. Atypical C3-PIGN and C3GN share the similar immunofluorescence feature of C3-dominated deposition. Our observations indicated that it is difficult to make a differential diagnosis through histological changes. Clinical presentations, autoantibodies against complement components and the presence of gene mutations became important for distinguishing them. Typical PIGN patients with hematuria, proteinuria, and hypocomplementemia normally recover within 12 weeks, and renal function returns to normal. Therefore, in any patient with C3-PIGN, persistent clinical abnormalities, including hypocomplementemia, proteinuria or declining renal function, should lead to further investigation of autoantibodies and gene mutations associated with the complement system.
All of these atypical C3-PIGN patients had negative results in complement-related antibody testing. Persistent hypocomplementemia may be caused by the mutations of genes involved in the complement system. Previous studies demonstrated that gene mutations could be detected in ‘atypical PIGN’ patients with long-term abnormal urinary test results [18,19,20]. However, these reported gene mutations in ‘atypical PIGN’ patients with persistent abnormal urinary test results were all located in genes involved in the alternative pathway (AP), which was consistent with a decrease in serum C3 levels and the deposition of C3 in glomeruli, indicating abnormal activation of AP. Sethi et al. investigated mutations in the genes involved in the AP in 11 ‘atypical PIGN’ patients and found that four patients had mutations located in the CFH and CFHR5 genes [12]. Our atypical C3-PIGN patients also carried mutations in CFH and CFHR5. Additionally, two patients in our study had mutations in the CFI and CFHR3 genes, which are also involved in the alternative pathway. One patient possessed mutations in CFH, CFHR3, and CFHR5. These mutations have been previously reported in C3GN patients and showed obvious linkage disequilibrium, thus increasing the susceptibility to kidney injury. Mechanistic studies confirmed that the mutation site in the CFHR3 gene is located in the binding region of C3b, thus leading to a reduction in the binding affinity of CFHR3 and C3b [17], which may inhibit the inactivation and degradation of C3b.
Notably, five patients also possessed MASP2 mutations; these mutations have also been described previously in C3G patients [21]. MASP2 is one of key serine proteases for complement activation in the lectin pathway (LP) and cleaves C2 and C4 to form the C3 convertase C4b2a. Activation of LP pathway plays an important role in IgA nephropathy and systemic lupus erythematosus. MASPs mediate process of coagulation and endothelial and platelet activation. Abnormal levels of MASP2 are associated with infections and inflammatory diseases, but the cases are rare and the clinical penetrance is also low.
In our study, we found four patients with the rs12711521 SNP variant. The tag SNP rs12711521 leads to the change of aspartic acid 371 to tyrosine (p. D371Y), and the predicted 3D structure of MASP2 with rs12711521 showed that tyrosine 371 is close to the serine protease domain which may influence the interaction with C4 and the stability of LP activation.. Interestingly, a previous study reported that the rs12711521 SNP is associated with high serum levels of MASP-2 [22] and susceptibility to numerous infectious diseases [23,24,25], and it is involved in dimerization [26] and increases MBL binding capacity [27]. These results suggested that patients carrying the rs12711521 risk allele are not only more susceptible to infection but also exhibit aberrant complement activation after infection. This speculation may explain why patient 1, who carried rs12711521, had suffered relapse when evaluated during the follow-up. We found that three patients with MASP2 gene mutations exhibited MASP2 deposits in the glomeruli, which suggested that there may be complement activation of the lectin pathway in these patients [28]. The mechanisms underlying the role of MASP2 mutations in the pathogenesis of C3-PIGN need to be further studied.
Expected genes in the alternative complement pathway and lectin pathway and C8A mutation were also found in one patient. C8A is a gene encoding the C8α subunit of complement and is involved in the formation of C5b-9. The polymorphism of C8A is related to Neisseria infection [29]. The majority of the mutations identified in the current patients were predicted to affect protein function when analyzed by SIFT or the Polyphen2 database and may induce abnormal immune responses to infections and cause persistently low serum levels of C3. Collectively, our results suggest that the continuous hypocomplementemia observed in atypical C3-PIGN patients is not only associated with abnormalities in the alternative complement pathway but also may be related to abnormalities in the lectin pathway and the pathway involved in resolving complement processes.
Unlike the gene mutations observed in C3GN patients, the gene mutations detected in atypical C3-PIGN patients may not lead to irreversible complement activation and subsequently severe renal damage. However, the existence of these mutations may induce delayed recovery of the complement system after infection and continuous hypocomplementemia. If stimulation is sustained, these atypical C3-PIGN patients may develop C3GN in the future. A previous publication reported that a second biopsy from patients with PIGN provided confirmation of C3GN [30]. Therefore, preventing repeated infections and continuous monitoring of the complement system are critical in the long-term management of atypical C3-PIGN.
A previous study demonstrated that C3GN patients possessing complement gene mutations may show familial aggregation of disease. The most typical familial disease in C3GN is CFHR5 nephropathy, a condition that has been reported in a family in Cyprus [31]. This condition is associated with autosomal dominant genetic characteristics; the clinical manifestations are continuous microscopic hematuria that may be accompanied by early onset pharyngitis and gross hematuria. Genetic testing showed that all members of this particular family possessed mutations in the CFHR5 gene, which suggests that this may represent a disease involving a single gene. Other studies have reported that a series of mutations in the CFHR gene family were related to the phenomenon of familial aggregation [32, 33]. It is important to note that C3GN is a relatively complex genetic disease and is not often inherited in a Mendelian manner. We found no evidence of a positive family history of kidney disease in our present study.
Long-term follow-up led to the identification of one patient with persistent hypocomplementemia who had suffered relapses. The recurrence of PIGN is relatively rare. The recurrence of PIGN with immunoglobulin deposition has been suggested to be related to IgA deficiency [34]; mutations in CFH and MCP have been detected in patients with recurrent C3-PIGN [9]. We speculate that in the context of complement-related gene mutations, potential abnormalities in complement regulatory function are more likely to increase the possibility of relapse.
This study had some limitations. First, this was a retrospective study. We could not detect some antibodies, including C4 nephritis factor, C5 nephritis factor, Factor B, anti-C3b and anti-C1q, in these patients. Second, the function and pathological mechanisms of these identified abnormal mutations need further investigation.
In summary, we found that mutations in complement-related genes are relatively common in atypical C3-PIGN patients. The mutations are not only located in alternative complement pathway genes but are also found in genes involved in the lectin pathway and C5b9 combination. Although these patients exhibit a relatively benign disease course and glucocorticoid therapy could accelerate recovery time, atypical C3-PIGN patients with gene mutations exhibit abnormal complement activation reactions and delayed complement recovery periods. Sustained stimulation may cause the recurrence and aggravation of the disease and even lead to the progression to C3GN. Therefore, we emphasize the importance of detecting gene mutations, closely monitoring changes in the complement system, and providing active treatment for atypical C3-PIGN patients to improve long-term outcomes.
References
Ramanathan G, Abeyaratne A, Sundaram M, Fernandes DK, Pawar B, Perry GJ, Sajiv C, Majoni SW (2017) Analysis of clinical presentation, pathological spectra, treatment and outcomes of biopsy-proven acute postinfectious glomerulonephritis in adult indigenous people of the Northern Territory of Australia. Nephrology 22(5):403–411. https://doi.org/10.1111/nep.12797
Hunt EAK, Somers MJG (2019) Infection-related glomerulonephritis. Pediatr Clin North Am 66(1):59–72. https://doi.org/10.1016/j.pcl.2018.08.005
Kanjanabuch T, Kittikowit W, Eiam-Ong S (2009) An update on acute postinfectious glomerulonephritis worldwide. Nat Rev Nephrol 5(5):259–269. https://doi.org/10.1038/nrneph.2009.44
Haas M (2003) Incidental healed postinfectious glomerulonephritis: a study of 1012 renal biopsy specimens examined by electron microscopy. Hum Pathol 34(1):3–10. https://doi.org/10.1053/hupa.2003.53
Pinto SW, Sesso R, Vasconcelos E, Watanabe YJ, Pansute AM (2001) Follow-up of patients with epidemic post streptococcal glomerulonephritis. Am J Kidney Dis 38(2):249–255. https://doi.org/10.1053/ajkd.2001.26083
Luo C, Tang Z, Chen D, Liu Z (2011) Long-term prognosis for Chinese adult patients with acute postinfectious glomerulonephritis. Clin Nephrol 76(3):186–194. https://doi.org/10.5414/cn107001
Stratta P, Musetti C, Barreca A, Mazzucco G (2014) New trends of an old disease: the acute post infectious glomerulonephritis at the beginning of the new millenium. J Nephrol 27(3):229–239. https://doi.org/10.1007/s40620-013-0018-z
Dedeoglu IO, Springate JE, Waz WR, Stapleton FB, Feld LG (1996) Prolonged hypocomplementemia in poststreptococcal acute glomerulonephritis. Clin Nephrol 46(5):302–305
Espinosa-Figueroa JL, Cano-Megias M, Martinez-Miguel P, Velo-Plaza M (2018) Recurrent postinfectious glomerulonephritis: an unusual evolution compatible with C3 glomerulopathy. BMJ Case Rep. https://doi.org/10.1136/bcr-2017-222979
Sethi S, Fervenza FC, Zhang Y, Zand L, Vrana JA, Nasr SH, Theis JD, Dogan A, Smith RJ (2012) C3 glomerulonephritis: clinicopathological findings, complement abnormalities, glomerular proteomic profile, treatment, and follow-up. Kidney Int 82(4):465–473. https://doi.org/10.1038/ki.2012.212
Xiao X, Pickering MC, Smith RJ (2014) C3 glomerulopathy: the genetic and clinical findings in dense deposit disease and C3 glomerulonephritis. Semin Thromb Hemost 40(4):465–471. https://doi.org/10.1055/s-0034-1376334
Sethi S, Fervenza FC, Zhang Y, Zand L, Meyer NC, Borsa N, Nasr SH, Smith RJ (2013) Atypical postinfectious glomerulonephritis is associated with abnormalities in the alternative pathway of complement. Kidney Int 83(2):293–299. https://doi.org/10.1038/ki.2012.384
Paixao-Cavalcante D, Lopez-Trascasa M, Skattum L, Giclas PC, Goodship TH, de Cordoba SR, Truedsson L, Morgan BP, Harris CL (2012) Sensitive and specific assays for C3 nephritic factors clarify mechanisms underlying complement dysregulation. Kidney Int 82(10):1084–1092. https://doi.org/10.1038/ki.2012.250
Frémeaux-Bacchi V, Weiss L, Demouchy C, May A, Palomera S, Kazatchkine MD (1994) Hypocomplementaemia of poststreptococcal acute glomerulonephritis is a ssociated with C3 nephritic factor (C3NeF) IgG autoantibody activity. Nephrol Dial Transplant 9(12):1747–1750
Jozsi M, Reuter S, Nozal P, Lopez-Trascasa M, Sanchez-Corral P, Prohaszka Z, Uzonyi B (2014) Autoantibodies to complement components in C3 glomerulopathy and atypical hemolytic uremic syndrome. Immunol Lett 160(2):163–171. https://doi.org/10.1016/j.imlet.2014.01.014
Watson R, Lindner S, Bordereau P, Hunze EM, Tak F, Ngo S, Zipfel PF, Skerka C, Dragon-Durey MA, Marchbank KJ (2014) Standardisation of the factor H autoantibody assay. Immunobiology 219(1):9–16. https://doi.org/10.1016/j.imbio.2013.06.004
Ding Y, Zhao W, Zhang T, Qiang H, Lu J, Su X, Wen S, Xu F, Zhang M, Zhang H, Zeng C, Liu Z, Chen H (2017) A haplotype in CFH family genes confers high risk of rare glomerular nephropathies. Sci Rep 7(1):6004. https://doi.org/10.1038/s41598-017-05173-8
Vernon KA, Goicoechea de Jorge E, Hall AE, Fremeaux-Bacchi V, Aitman TJ, Cook HT, Hangartner R, Koziell A, Pickering MC (2012) Acute presentation and persistent glomerulonephritis following streptococcal infection in a patient with heterozygous complement factor H-related protein 5 deficiency. Am J Kidney Dis 60(1):121–125. https://doi.org/10.1053/j.ajkd.2012.02.329
Sandhu G, Bansal A, Ranade A, Jones J, Cortell S, Markowitz GS (2012) C3 glomerulopathy masquerading as acute postinfectious glomerulonephritis. Am J Kidney Dis 60(6):1039–1043. https://doi.org/10.1053/j.ajkd.2012.04.032
Ito N, Ohashi R, Nagata M (2017) C3 glomerulopathy and current dilemmas. Clin Exp Nephrol 21(4):541–551. https://doi.org/10.1007/s10157-016-1358-5
Avasare RS, Canetta PA, Bomback AS, Marasa M, Caliskan Y, Ozluk Y, Li Y, Gharavi AG, Appel GB (2018) Mycophenolate Mofetil in combination with steroids for treatment of C3 glomerulopathy: a case series. Clin J Am Soc Nephrol 13(3):406–413. https://doi.org/10.2215/CJN.09080817
Boldt AB, Grisbach C, Steffensen R, Thiel S, Kun JF, Jensenius JC, Messias-Reason IJ (2011) Multiplex sequence-specific polymerase chain reaction reveals new MASP2 haplotypes associated with MASP-2 and MAp19 serum levels. Hum Immunol 72(9):753–760. https://doi.org/10.1016/j.humimm.2011.05.015
de Rooij BJ, van Hoek B, ten Hove WR, Roos A, Bouwman LH, Schaapherder AF, Porte RJ, Daha MR, van der Reijden JJ, Coenraad MJ, Ringers J, Baranski AG, Hepkema BG, Hommes DW, Verspaget HW (2010) Lectin complement pathway gene profile of donor and recipient determine the risk of bacterial infections after orthotopic liver transplantation. Hepatology 52(3):1100–1110. https://doi.org/10.1002/hep.23782
Boldt AB, Luz PR, Messias-Reason IJ (2011) MASP2 haplotypes are associated with high risk of cardiomyopathy in chronic Chagas disease. Clin Immunol 140(1):63–70. https://doi.org/10.1016/j.clim.2011.03.008
Tulio S, Faucz FR, Werneck RI, Olandoski M, Alexandre RB, Boldt AB, Pedroso ML, de Messias-Reason IJ (2011) MASP2 gene polymorphism is associated with susceptibility to hepatitis C virus infection. Hum Immunol 72(10):912–915. https://doi.org/10.1016/j.humimm.2011.06.016
Gregory LA, Thielens NM, Matsushita M, Sorensen R, Arlaud GJ, Fontecilla-Camps JC, Gaboriaud C (2004) The X-ray structure of human mannan-binding lectin-associated protein 19 (MAp19) and its interaction site with mannan-binding lectin and L-ficolin. J Biol Chem 279(28):29391–29397. https://doi.org/10.1074/jbc.M402687200
Thiel S, Kolev M, Degn S, Steffensen R, Hansen AG, Ruseva M, Jensenius JC (2009) Polymorphisms in mannan-binding lectin (MBL)-associated serine protease 2 affect stability, binding to MBL, and enzymatic activity. J Immunol 182(5):2939–2947. https://doi.org/10.4049/jimmunol.0802053
Roos A, Rastaldi MP, Calvaresi N, Oortwijn BD, Schlagwein N, van Gijlswijk-Janssen DJ, Stahl GL, Matsushita M, Fujita T, van Kooten C, Daha MR (2006) Glomerular activation of the lectin pathway of complement in IgA nephropathy is associated with more severe renal disease. J Am Soc Nephrol 17(6):1724–1734. https://doi.org/10.1681/ASN.2005090923
Barba GM, Kaufmann TJ, Schneider PM, Rittner C, Brai M (1994) Polymorphism of the complement C8A and -B genes in two families with C8 beta deficiency and neisserial infections. Clin Immunol Immunopathol 72(1):83–89. https://doi.org/10.1006/clin.1994.1110
Al-Ghaithi B, Chanchlani R, Riedl M, Thorner P, Licht C (2016) C3 Glomerulopathy and post-infectious glomerulonephritis define a disease spectrum. Pediatr Nephrol 31(11):2079–2086. https://doi.org/10.1007/s00467-015-3311-3
Gale DP, de Jorge EG, Cook HT, Martinez-Barricarte R, Hadjisavvas A, McLean AG, Pusey CD, Pierides A, Kyriacou K, Athanasiou Y, Voskarides K, Deltas C, Palmer A, Fremeaux-Bacchi V, de Cordoba SR, Maxwell PH, Pickering MC (2010) Identification of a mutation in complement factor H-related protein 5 in patients of Cypriot origin with glomerulonephritis. Lancet 376(9743):794–801. https://doi.org/10.1016/s0140-6736(10)60670-8
Xiao X, Ghossein C, Tortajada A, Zhang Y, Meyer N, Jones M, Borsa NG, Nester CM, Thomas CP, de Cordoba SR, Smith RJ (2016) Familial C3 glomerulonephritis caused by a novel CFHR5-CFHR2 fusion gene. Mol Immunol 77:89–96. https://doi.org/10.1016/j.molimm.2016.07.007
Togarsimalemath SK, Sethi SK, Duggal R, Le Quintrec M, Jha P, Daniel R, Gonnet F, Bansal S, Roumenina LT, Fremeaux-Bacchi V, Kher V, Dragon-Durey MA (2017) A novel CFHR1-CFHR5 hybrid leads to a familial dominant C3 glomerulopathy. Kidney Int 92(4):876–887. https://doi.org/10.1016/j.kint.2017.04.025
Casquero A, Ramos A, Barat A, Mampaso F, Caramelo C, Egido J, Ortiz A (2006) Recurrent acute postinfectious glomerulonephritis. Clin Nephrol 66(1):51–53. https://doi.org/10.5414/cnp66051
Acknowledgements
Samples were from Renal Biobank of National Clinical Research Center of Kidney Diseases, Renal Biobank of Jiangsu Provincial Science and Technology Resources Coordination Service Platform.
Funding
This research was supported by Special Funds of the National Natural Science Foundation of China (32141004), National Natural Science Foundation of China (82370733), Natural Science Foundation of Jiangsu Province (BK20211130) and Jiangsu Provincial Science and Technology Resources Coordination Service Platform (No. BM2015004-2). Dr. Song Jiang is the guarantor of this work.
Author information
Authors and Affiliations
Contributions
SJ supervised and designed this project. FX and SJ wrote the manuscript. FX and CHZ performed histologic assessment. MCZ and XDZ performed IF staining. CMZ performed exon sequencing. SQC and ZC collected patient’s data. FX and SJ contributed to data interpretation. All authors critically read the manuscript and approved the final version of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, F., Zhang, C., Zhang, M. et al. Evaluation of the significance of complement-related genes mutations in atypical postinfectious glomerulonephritis: a pilot study. Int Urol Nephrol 56, 1475–1485 (2024). https://doi.org/10.1007/s11255-023-03831-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03831-7