Abstract
Objectives
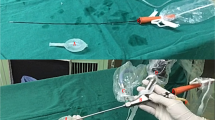
Surgical procedures for vaginal hydroceles have been varied with the aims of preventing recurrence, hematoma and edema formation and providing a better cosmetic outcome. The Jaboulay’s procedure remains a preferred procedure owing to its simplicity and good long term outcome. However, sac eversion during the procedure leads to scrotal edema and mass sensation due to remnant sac in cases of large or secondary hydrocele sacs. Sac excision in these cases may provide better outcomes by removing the excess tissue. We aimed to compare the postoperative outcome after Jaboulay’s procedure and harmonic scalpel excision of the sac in terms of scrotal edema, hematoma formation and the final cosmetic appearance.
Patients and methods
72 adult patients with vaginal hydrocele were randomized into two groups, who underwent harmonic scalpel sac excision and Jaboulay’s procedure respectively, performed by a single surgeon. Preoperatively, patient demographics were noted. Postoperatively, data was recorded on the 1st day, 3rd day & 10th day about postoperative complications, and outcomes. Satisfaction on final cosmetic outcome was compared between the groups at the 3rd month.
Results
Post operative edema and sensation of mass in the scrotum were more (but not significant) in the Jaboulay’s procedure group. Seroma and wound infection rates were similar in both groups. Patient satisfaction on cosmesis was better in the sac excision group.
Conclusion
Hydrocelectomy with excision of the sac using a harmonic scalpel results in a lower incidence of postoperative oedema and better patient satisfaction in terms of cosmetic outcome compared to Jaboulay’s procedure in the treatment of adult hydroceles.



Similar content being viewed by others
Data availability
The data related to this study is not available on any repository and the Data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Francis JJ, Levine LA (2013) Aspiration and sclerotherapy: a nonsurgical treatment option for hydroceles. J Urol 189(5):1725–1729
Ho GT, Ball RA, Schuessler W, Kavoussi LR (1993) Efficacy of endoscopic hydrocele ablation. J Endourol 7(1):71–74
Bin Y, Yong-Bao W, Zhuo Y, Jin-Rui Y (2014) Minimal hydrocelectomy with the aid of scrotoscope: a ten-year experience. Int Braz J Urol 40(3):384–389
Emir L, Sunay M, Dadalı M, Karakaya Y, Erol D (2011) Endoscopic versus open hydrocelectomy for the treatment of adult hydroceles: a randomized controlled clinical trial. Int Urol Nephrol 43(1):55–59
Al-Ali BM, Popper H, Pummer K (2012) A case of Fournier’s gangrene after hydrocelectomy. Cent Eur J Urol 65(2):92–93
Ross LS, Flom LS (1991) Azoospermia: a complication of hydrocele repair in a fertile population. J Urol 146(3):852–853
Zahalsky MP, Berman AJ, Nagler HM (2004) Evaluating the risk of epididymal injury during hydrocelectomy and spermatocelectomy. J Urol 171(6 Pt 1):2291–2292
Tsai L, Milburn PA, Cecil CL 4th, Lowry PS, Hermans MR (2019) Comparison of recurrence and postoperative complications between 3 different techniques for surgical repair of idiopathic hydrocele. Urology 125:239–242
Ku JH, Kim ME, Lee NK; The excisional, plication and internal drainage techniques: a comparison of the results for idiopathic hydrocele.
Jaboulay M. chirurgie des centres nerveux des visceres et des membres;lyon/paris:storck, 1902:192.
Lord PH (1964) A bloodless operation for radical cure of idiopathic hydrocele. British J Surg 51:914–964
Sharma LS, Jhawar PK (1979) Surgery of hydrocele (a simplified minimal dissection technique). Ind J Surg 41:700–704
Rowe NE, Martin P, Luke PP (2016) The western snip, stitch and tug hydrocelectomy: how I do it. Can Urol Assoc J 10(9–10):328–330
Onol SY, Illbey YO, Onol FF, Ozbek E, Arslan B, Akbas A (2009) A novel pull through technique for surgical management of idiopathic hydrocele. J Urol 181(3):1202–1205
Lei J et al (2019) a comparison of novel endoscopic “Su-Wang technique” with the open Jaboulay’s procedure for the surgical treatment of adult primary vaginal hydrocele. Sci Rep 9(1):9152
Kumar RR, Trehan V, Gupta A, Mohan H, Antony T, Chhikara A, Kumar SS, Kishor K (2022) Outcomes after eversion of sac and subtotal excision of sac in cases of primary hydrocele. J Surg Med 6(4):449–454
Shirke MO, Dhaigude B, Panchbhai SV, Chavan S (2019) A comparative study of different surgical procedures in the management of primary vaginal hydrocele. New Indian J Surg 10(2):175–181
Ozkaya F, Cakici OU (2020) Jaboulay’s technique contrasted with novel hydrocelectomy technique using a vessel sealer in treatment of adult hydrocele: a prospective randomized study. Int Urol Nephrol 52(3):447–453. https://doi.org/10.1007/s11255-019-02342-8
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thakur, D.S., Saraf, M., Kateha, D. et al. Jaboulay’s versus harmonic scalpel hydrocelectomy: prospective randomized controlled study. Int Urol Nephrol 56, 29–33 (2024). https://doi.org/10.1007/s11255-023-03768-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03768-x