Abstract
Purpose
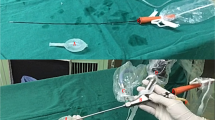
The study aims to compare the clinical efficacy, complications, and patient satisfaction rates of two open hydrocelectomy techniques, Jaboulay’s technique, and sac excision hydrocelectomy using a LigaSure™ device, in a prospective and randomized fashion.
Methods
Eighty-two (82) patients were randomized, one-to-one into two groups. All surgeries were carried out by a single surgeon. Jaboulay’s technique and hydrocelectomy with excision of the sac were carried out in the first and the second groups, respectively. The patients’ data were collected prospectively on the first day, the first week, the first month, and the sixth month after surgery. Patient demographics, length of hospital stay, postoperative complications, and sixth-month cosmetic satisfaction rates were compared between the groups.
Results
We observed better patient satisfaction [73.2% confer (cf.) 92.9%], shorter hospital stay (1.66 cf. 1.29 days), and less incidence of postoperative edemas (31.7% cf. 6%) in the sac excision hydrocelectomy group (p = 0.017, p = 0.011, and p = 0.029, respectively).
Conclusion
We can report that hydrocelectomy with an excision of the sac using a vessel-sealing device, namely LigaSure™, provides less incidences of postoperative edemas and better patient satisfaction rates respective to the Jaboulay’s technique in the treatment of adult hydrocele. The statistical difference between hospital stay times is mostly affected by social factors in our study. Clinically, all patients were amenable to discharge in the first day.

Similar content being viewed by others
References
Sampietro Crespo A, Vaquerizo Gareta A, Fernández Durán A, Fernández Gómez J, Zazo Romojaro A, Alvarez Fernández F, Gómez Rodríguez A (1995) Major outpatient surgery in urology: our experience. Arch Esp Urol. 48(4):343–346 (article in Spanish)
Swartz MA, Morgan TM, Krieger JN (2007) Complications of scrotal surgery for benign conditions. Urology 69(4):616–619
Khaniya S, Agrawal CS, Koirala R, Regmi R, Adhikary S (2009) Comparison of aspiration-sclerotherapy with hydrocelectomy in the management of hydrocele: a prospective randomized study. Int J Surg 7(4):392–395
Rioja J, Sánchez-Margallo FM, Usón J, Rioja LA (2011) Adult hydrocele and spermatocele. BJU Int 107(11):1852–1864
Francis JJ, Levine LA (2013) Aspiration and sclerotherapy: a nonsurgical treatment option for hydroceles. J Urol 189(5):1725–1729
Ho GT, Ball RA, Schuessler W, Kavoussi LR (1993) Efficacy of endoscopic hydrocele ablation. J Endourol 7(1):71–74
Bin Y, Yong-Bao W, Zhuo Y, Jin-Rui Y (2014) Minimal hydrocelectomy with the aid of scrotoscope: a ten-year experience. Int Braz J Urol 40(3):384–389
Emir L, Sunay M, Dadalı M, Karakaya Y, Erol D (2011) Endoscopic versus open hydrocelectomy for the treatment of adult hydroceles: a randomized controlled clinical trial. Int Urol Nephrol 43(1):55–59
Al-Ali BM, Popper H, Pummer K (2012) A case of Fournier’s gangrene after hydrocelectomy. Cent Eur J Urol 65(2):92–93
Ross LS, Flom LS (1991) Azoospermia: a complication of hydrocele repair in a fertile population. J Urol 146(3):852–853
Tsai L, Milburn PA, Cecil CL 4th, Lowry PS, Hermans MR (2019) Comparison of recurrence and postoperative complications between 3 different techniques for surgical repair of idiopathic hydrocele. Urology 125:239–242
Zahalsky MP, Berman AJ, Nagler HM (2004) Evaluating the risk of epididymal injury during hydrocelectomy and spermatocelectomy. J Urol 171(6 Pt 1):2291–2292
Rowe NE, Martin P, Luke PP (2016) The Western snip, stitch, and tug hydrocelectomy: how I do it. Can Urol Assoc J 10(9–10):E328–E330
Onol SY, Ilbey YO, Onol FF, Ozbek E, Arslan B, Akbaş A (2009) A novel pull-through technique for the surgical management of idiopathic hydrocele. J Urol 181(3):1201–1205
Saber A (2015) Minimally access versus conventional hydrocelectomy: a randomized trial. Int Braz J Urol. 41(4):750–756
Cocci A, Patruno G, Gandaglia G, Rizzo M, Esperto F, Parnanzini D, Pietropaolo A, Principi E, Talso M, Baldesi R, Battaglia A, Shehu E, Carrobbio F, Corsaro A, La Rocca R, Marchioni M, Bianchi L, Miglioranza E, Mantica G, Martorana E, Misuraca L, Fontana D, Forte S, Napoli G, Russo GI, Senato degli Specializzandi Study Group (2018) Urology residency training in Italy: results of the first national survey. Eur Urol Focus. 4(2):280–287
Hassan JM, Adams MC, Pope JC 4th, Demarco RT, Brock JW 3rd (2006) Hydrocele formation following laparoscopic varicocelectomy. J Urol 175(3 Pt 1):1076–1079
Abe K, Kato N, Miki K, Nimura S, Suzuki M, Kiyota H, Onodera S, Oishi Y (2002) Malignant mesothelioma of testicular tunica vaginalis. Int J Urol 9(10):602–603
Mackenzie CD, Lazarus WM, Mwakitalu ME, Mwingira U, Malecela MN (2009) Lymphatic filariasis: patients and the global elimination programme. Ann Trop Med Parasitol 103(Suppl 1):S41–S51
Thomas G, Richards FO Jr, Eigege A, Dakum NK, Azzuwut MP, Sarki J, Gontor I, Abimiku J, Ogah G, Jindau MY, Jiya JY, Miri ES (2009) A pilot program of mass surgery weeks for treatment of hydrocele due to lymphatic filariasis in central Nigeria. Am J Trop Med Hyg 80(3):447–451
Turner HC, Bettis AA, Chu BK, McFarland DA, Hooper PJ, Mante SD, Fitzpatrick C, Bradley MH (2017) Investment success in public health: an analysis of the cost-effectiveness and cost-benefit of the global programme to eliminate lymphatic filariasis. Clin Infect Dis 64(6):728–735
Kim CJ, Kushima M, Okada Y, Tomoyoshi T (1991) Tunica albuginea cyst associated with hydrocele testis: report of a case. Hinyokika Kiyo 37(9):1065–1068 (article in Japanese)
Marte A, Prezioso M, Sabatino MD, Borrelli M, Romano M, Del Balzo B, Nino F, Parmeggiani P (2009) Syringocele in children: an unusual presentation as scrotal mass. Minerva Pediatr 61(1):123–127 (article in Italian)
Mitsuzuka K, Eriguchi T, Shimada S, Kato SN (2007) Bilateral spermatocele concurrent with bilateral scrotal hydrocele presenting huge scrotal swelling. Hinyokika Kiyo 53(10):729–731
Viers CD, Lele SM, Kirkpatrick T, LaGrange CA (2017) Carcinosarcoma of the tunica vaginalis following radiation therapy for localized prostate cancer. Urol Case Rep 20(13):140–142
Kim YW, Kim JW, Kim JH, Lee J, Lee E, Kim MY, Yang HK, Chang H (2014) Metastatic testicular tumor presenting as a scrotal hydrocele: an initial manifestation of pancreatic adenocarcinoma. Oncol Lett 7(6):1793–1795
Shah VS, Nepple KG, Lee DK (2014) Routine pathology evaluation of hydrocele and spermatocele specimens is associated with significant costs and no identifiable benefit. J Urol 192(4):1179–1182
Zampieri N, El-Dalati G, Ottolenghi A, Camoglio FS (2009) Percutaneous aspiration for hydroceles after varicocelectomy. Urology 74(5):1122–1124
Rodríguez WC, Rodríguez DD, Fortuño RF (1981) The operative treatment of hydrocele: a comparison of 4 basic techniques. J Urol 125(6):804–805
Author information
Authors and Affiliations
Contributions
FO: performance of surgeries, collection of data, and patient follow-up. OUC: interpretation of data, main design of the study, and writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that there is no conflict of interest with any organization regarding the material discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozkaya, F., Cakici, O.U. Jaboulay’s technique contrasted with a novel hydrocelectomy technique using a vessel sealer in the treatment of adult hydrocele: a prospective randomized study. Int Urol Nephrol 52, 447–453 (2020). https://doi.org/10.1007/s11255-019-02342-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02342-8