Abstract
Background
Renal hyperfiltration (RHF), recently established as a risk factor for mortality, is linked to current and subsequent diabetes mellitus (DM). DM could be seen as a mediator in the pathway between RHF and mortality. However, the mediating role of DM in the relationship between RHF and mortality is unclear.
Methods and results
Based on a cohort of 2682 Finnish men from the Kuopio Ischaemic Heart Disease Risk Factor Study (KIHD) followed-up for 35 years, we evaluated the association between RHF and mortality, with DM as a mediator, following two methods: a classic mediation analysis approach, using Cox regression, and a counterfactual framework for mediation analysis, using g-computation, Cox regression, and logistic regression. RHF is associated with an increased risk of mortality. This association was not mediated by DM. Under a counterfactual framework and on a hazard ratio scale, RHF association with mortality had a total effect of 1.54 (95% confidence interval, 1.26–1.98) and a controlled direct effect of 1.66 (1.34–2.16).
Conclusion
An association between RHF and mortality risk, independent of DM, was established. RHF should be considered, managed, and followed-up as a mortality-associated condition, regardless of the status of DM. We suggest clinicians to consider including RHF screening in routine clinical care, especially diabetic care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Abnormal increase in glomerular filtration rate (GFR), termed renal hyperfiltration (RHF), was mainly regarded as an early sign of kidney damage in diabetes mellitus (DM), especially type 1 [1,2,3]. While RHF is prevalent in diabetes mellitus (DM), with figures as high as 75% in type 1 DM [4] and 40% in type 2 DM [4,5,6], RHF was recently established as a risk factor for mortality [7], both cardiovascular [8] and non-cardiovascular [9, 10], in an apparently healthy population, unconstrained by DM [11,12,13]. RHF is linked to subsequent diabetes mellitus (DM). For instance, RHF could be a precursor to DM, manifesting in prediabetes [14]. In addition, RHF is linked to chronic kidney disease (CKD) [15]. Among nearly 17,000 individuals from a cohort study [16], those with RHF had 8.7 times (95% CI: 4.2–18.1) higher risk for a rapid decline of estimated GFR (eGFR), impending an increased risk of CKD. Whilst DM is the most common cause of CKD [17], RHF was particularly associated with diabetic kidney disease, in a meta-analysis by Magee et al. [18]. Further, among patients with DM, those with RHF were at a higher risk of mortality [13]. Concurrently, DM is well established as a risk factor for mortality [19].
DM could be seen as a mediator in the pathway between RHF and mortality. While the link between RHF and mortality was assessed in both diabetic [13] and nondiabetic populations [11, 20], the direct effect of RHF on mortality, independently of future DM, is unclear. Using mediation analysis [21], we aimed through this study on evaluating the mediating role of DM in the relationship between RHF and mortality.
Methods
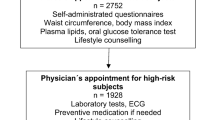
Data source and study population
The study is based on the Kuopio Ischaemic Heart Disease Risk Factor Study (KIHD), a cohort of 2682 men randomly sampled from the population of the region of Kuopio, Finland, between March 1984 and 1989 [22]. The cohort is linked to the Finnish Care Register for Healthcare (HILMO) (License THL/93/5.05.00/2013) and to the cause-of-death registry of Finland (License TK-53-1770-16), among other registries.
After excluding 50 patients with baseline CKD (eGFR ≤ 60 ml/min/1.73 m2) and 258 men with missing values, we excluded 321 men who were abstinent from drinking alcohol at baseline, since they represented a special case differing from the study population in terms of education and socioeconomic status, health behaviors, and overall health [23]. Finally, we excluded 9 men with outlying values of body mass index (BMI), and weekly alcohol consumption, settling for a final study population of 2044 men, followed for a maximum of 35 years (median, 28 years). There was no loss to follow-up in our study.
Variable measurement
Study participants were examined by a physician and a nurse who measured the men’s height, weight, and blood pressure, interviewed them and collected blood samples from them [19]. The men’s medical history, medications, and health behaviors were assessed through interviews and detailed structured questionnaires. Dietary intake was assessed through instructed 4-day food recording.
The study exposure of interest, RHF, was defined as eGFR values above the 95th age-adjusted percentile within the study population. We computed eGFR using the Chronic Kidney Disease Epidemiology Collaboration (CKD-Epi) equation [24], based on Jaffe-corrected [25] serum creatinine values. Follow-up DM (International Statistical Classification of Diseases and Related Health Problems 10th Revision [ICD-10] codes E10-E14) diagnosis was obtained through linkage to HILMO, serving as the study’s mediator of interest. For sensitivity analysis, a 20-year examination also assessed the survivors’ status of DM through interviews on medical and medication history and blood sample analysis for a serum glucose level.
We considered the following variables measured at baseline as covariates in our analyses: age, BMI [26] (as a categorical variable), hypertension status [27] (medication or medical history of hypertension or an elevated mean systolic (≥ 140 mm Hg) or diastolic (≥ 90 mm Hg) blood pressure), smoking status [28, 29] (current-, previous-, or never smoker), alcohol consumption [30] (grams per week), vitamin D level [31] (indicated by serum 25(OH)D3 [32], 25th percentile within the study population [29.02 ng/mL] as the cutoff between low and normal vitamin D levels), and the healthy Nordic diet (HND) score [33] (based on the Baltic Sea Diet Score, a validated indicator of diet quality in the Nordic countries [34]).
The outcome of our study, mortality due to any cause, was sourced through the Finnish cause-of-death registry and ascertained using the Finnish personal identification code.
Data analysis
First, we described the study population in terms of baseline characteristics and occurrence of DM during follow-up, with comparisons between survivors and non-survivors, using Chi-square, Kruskal–Wallis, and Mann-Whitey U tests. Then, in a classic mediation analysis approach [35], we examined the hazard ratio (HR) of the association between RHF and mortality, with DM as the mediator (Fig. 1), in a. all the study population (no adjustment for baseline or follow-up DM) and b. excluding those who had a DM diagnosis at baseline or during follow-up. These HRs were estimated using Cox proportional hazard models, with a period at risk from baseline until the occurrence of the outcome or the last day of follow-up on 31 December 2018, crude (age-adjusted only) and adjusted for the following baseline covariates: age, BMI, hypertension, smoking status, alcohol consumption, vitamin D level, and HND score. This approach assumes that there is no confounding between the RHF and DM, RHF and mortality, and DM and mortality, and that there is no interaction between RHF and DM, and that no variable confounding the relation between DM and mortality is affected by RHF. A relation of mediation would be suggested if the effect of RHF on mortality would disappear after adjustment for the mediator.
Directed acyclic graph illustrating the relation between the exposure of interest, renal hyperfiltration (RHF), the mediator, diabetes mellitus (DM), the outcome of interest, mortality, and potential confounders (C). The box around DM suggests that conditioning was done on this variable (through restriction)
Third, to better examine the mediating role of DM in the RHF-mortality relationship, we performed a mediation analysis, in a counterfactual framework [36, 37], using non-parametric g-computation [38, 39], with RHF as the exposure, DM as the mediator, and mortality as the outcome (Fig. 2). This approach is justified considering that conditioning on the mediator, as per the classic approach, may create a situation of collider bias (Fig. 2), confounding the relation between exposure and outcome [40, 41]. Additionally, considering that DM is associated with mortality through multiple pathways and that the long-term consequences of RHF are not well explored, unmeasured variables (L, Fig. 2) could be a source of exposure-induced confounding between the mediator and the outcome. In addition, our approach permits consideration for potential RHF-DM interactions [37].
We regressed the outcome variable using a Cox proportional hazard model and the mediator using logistic regression. We adjusted our models for age, DM, BMI, smoking, hypertension, alcohol consumption, vitamin D level, and HND score, all measured at baseline. Applying the g-formula [38], we used direct counterfactual imputation as the estimation method of the causal effects, expressed in HRs, and bootstrapping to obtain their 95% confidence intervals [42]. We decomposed the total RHF effect on mortality considering direct, indirect, and pure natural effects [43, 44].
Finally, as a sensitivity analysis (SA) of the classic mediation analysis, SA1. We included in the fully adjusted Cox regression model examining the association between RHF and mortality in all study population an interaction term between RHF and baseline DM. As SAs of the mediation analysis performed according to the counterfactual framework, SA2. We used KIHD diagnoses of DM at 20 years of follow-up as the mediator instead of the diagnosis collected via linkage with HILMO throughout the follow-up, and SA3. We used baseline DM instead of follow-up DM as a mediator.
All computations were performed by means of R version 4.2.2 (https://www.R-project.org).
Results
At the end of follow-up, the study outcome, mortality, occurred in 1289 men out of 2044 (63.06%). In comparison to the survivors, non-survivors had a higher proportion of RHF (7.21 versus [vs.] 2.65%, p < 0.001), a higher proportion of baseline DM (8.15 vs. 2.38%, p < 0.001), and a higher proportion of follow-up DM (15.59 vs. 11.52%; p < 0.001). Descriptive statistics of the study population’s baseline and follow-up characteristics by mortality outcome are described in Table 1.
In the classic mediation analysis, the HR of the total effect of RHF on mortality, with no adjustment for DM, was 1.83 (95% CI 1.48–2.26) in the crude Cox regression model and 1.56 (1.26–1.94) in the adjusted model, when compared to normal eGFR. When restricting the Cox regression analysis to those who did not have DM at baseline or during follow-up, RHF association with mortality presented with an HR of 1.88 (1.50–2.37) in the crude model and 1.57 (1.24–1.99) in the adjusted model.
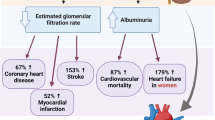
In the mediation analysis under a counterfactual framework, the effect decomposition of RHF on mortality showed, on an HR scale, a total effect of 1.54 (95% CI 1.26–1.98), a controlled direct effect of 1.66 (1.34–2.16), a total natural direct effect of 1.54 (1.27–1.98) and a total natural indirect effect of 0.98 (0.95—1.04). The overall proportion of the effect of RHF on mortality that was mediated by DM was minimal (− 5%, p-value=0.682) (Table 2 and Fig. 3, full details in Supplementary material).
Effect decomposition of the mediation analysis using a counterfactual framework. Total Association: refers to the total effect of renal hyperfiltration on mortality, including both direct and indirect pathways. Controlled Direct Effect: refers to the effect of renal hyperfiltration on mortality that remains after controlling for the effect of the mediator. Pure Natural Direct Effect: refers to the effect of renal hyperfiltration on mortality when the mediator is set at the level that would naturally be observed in the absence of renal hyperfiltration. Total Natural Direct Effect: refers to the effect of renal hyperfiltration on mortality when the mediator is set at the level that would naturally be observed in the presence of renal hyperfiltration. Pure Natural Indirect Effect: captures the effect of the mediator on mortality in the absence of renal hyperfiltration. Total Natural Indirect Effect: captures the effect of the mediator on mortality in the presence of renal hyperfiltration
In the SA of the classic mediation analysis (SA1), the HR of the association between RHF and mortality remained relatively consistent on the inclusion of an interaction term between RHF and baseline DM, which the HR did not show an association with mortality. The SA results related to the mediation analysis in a counterfactual framework also remained relatively consistent with the main analysis (Supplementary material).
Discussion
In a population-based cohort of middle-aged Finnish men with a 35-year follow-up, RHF associated with an increased risk of mortality. This association was not mediated by DM. These results were consistent using a classic mediation analysis approach, in both crude and adjusted models, and using a counterfactual framework, applying the g-formula. In addition, no interaction between RHF and DM regarding mortality was found.
In accordance with previous studies [7, 12], our results found an association between RHF and mortality risk independently of DM. However, to the best of our knowledge, our study is the first to consider the mediating role of follow-up DM in the relation between RHF and mortality. While the mechanism by which RHF associates with death is still unclear, especially that both cardiovascular and non-cardiovascular mortality are concerned, RHF should be considered, managed, and followed-up as a mortality-associated condition, regardless of the status of DM. Particularly in DM, RHF should benefit from special care to limit its extent and consequences. As Penno et al. [13] noted, DM patients with RHF are at a higher mortality risk than DM patients without RHF. In DM, an increase in GFR follows the increase in kidney size and tubular growth secondary to DM-associated hyperglycemia and obesity. In addition, hyperglycemia-induced upregulation of sodium-glucose cotransporters and proximal tubular sodium and glucose reabsorption increases single-nephron GFR by reducing afferent arteriolar resistance [45]. Consequently, glycemic control and weight loss could be efficient measures to reduce the harms of both DM and RHF. Nevertheless, the role of other measures, such as sodium-glucose cotransporter inhibitors [46] and dietary protein intake [47], in controlling RHF, also remains to be assessed. Finally, we suggest clinicians to consider including RHF screening in routine clinical care, especially diabetic care, and the research community to further profile RHF, despite its transient nature, as a disease, and to evaluate its public health burden.
Our study is strong by its long follow-up time, reliable exposure, mediators, covariates, and outcome assessment, and by its advanced and comprehensive methodology, including a number of sensitivity analyses, to which our findings remained consistent. However, multiple limitations could be counted.
First, the generalizability of our results is limited to middle-aged Finnish men. RHF might have a distinct pathogenesis and mortality profile in women [48]. Second, the ephemeral nature and the inter-day and intraday variations of GFR suggest that a single measure at baseline might not be sufficient to define RHF. Though additional measures at baseline could help ascertain exposure, the study design could benefit from consideration for time-varying exposure, throughout the follow-up.
IN addition, eGFR is not a perfect measure of GFR. While we corrected our serum creatinine measurement for the Jaffe assay [25], it is possible that this last might contribute to the overestimation of RHF in patients with increased serum glucose [49]. Serum cystatin C could be a better alternative to estimate GFR in patients with DM, when assessing RHF. Finally, further adjustment for grip strength [50] and central obesity [51] could improve our estimates, but it is unlikely to impact our findings which were consistent across crude and adjusted analyses.
Clinical significance
Renal hyperfiltration has mostly been regarded under the lens of diabetes mellitus, although it is getting established as an independent risk factor for mortality. Often associated with prediabetes and presenting as a precursor of diabetes mellitus, renal hyperfiltration is linked to subsequent diabetes mellitus. Diabetes mellitus could, thus, be seen as a mediator in the pathway between renal hyperfiltration and mortality. However, the mediating role of diabetes mellitus in the association between renal hyperfiltration and mortality has not been studied. We found an association between renal hyperfiltration and mortality risk. The association was not mediated by diabetes mellitus. Renal hyperfiltration should be assessed and managed as an independent condition, regardless of the status of diabetes mellitus.
Data availability
The University of Eastern Finland can be approached for requests of access to the KIHD dataset.
References
Christiansen JS, Gammelgaard J, Frandsen M, Parving HH (1981) Increased kidney size, glomerular filtration rate and renal plasma flow in short-term insulin-dependent diabetics. Diabetologia 20(4):451–456
Ditzel J, Junker K (1972) Abnormal glomerular filtration rate, renal plasma flow, and renal protein excretion in recent and short-term diabetics. Br Med J 2(5804):13–19
Mogensen CE (1972) Kidney function and glomerular permeability to macromolecules in juvenile diabetes with special reference to early changes. Dan Med Bull 19(Suppl 3):1–40
Jerums G, Premaratne E, Panagiotopoulos S, MacIsaac RJ (2010) The clinical significance of hyperfiltration in diabetes. Diabetologia 53(10):2093–2104
Tomaszewski M, Charchar FJ, Maric C, McClure J, Crawford L, Grzeszczak W et al (2007) Glomerular hyperfiltration: a new marker of metabolic risk. Kidney Int 71(8):816–821
Sasson AN, Cherney DZ (2012) Renal hyperfiltration related to diabetes mellitus and obesity in human disease. World J Diabetes 3(1):1–6
Park M, Yoon E, Lim YH, Kim H, Choi J, Yoon HJ (2015) Renal hyperfiltration as a novel marker of all-cause mortality. J Am Soc Nephrol JASN 26(6):1426–1433
Dupuis ME, Nadeau-Fredette AC, Madore F, Agharazii M, Goupil R (2020) Association of glomerular hyperfiltration and cardiovascular risk in middle-aged healthy individuals. JAMA Netw Open 3(4):e202377
Kim Y, Lee S, Lee Y, Kang MW, Park S, Park S et al (2020) Glomerular hyperfiltration and cancer: a nationwide population-based study. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 29(10):2070–2077
Kang MW, Park S, Lee S, Lee Y, Cho S, Han K et al (2020) Glomerular hyperfiltration is associated with dementia: a nationwide population-based study. PLoS ONE 15(1):e0228361
Eriksen BO, Løchen ML, Arntzen KA, Bertelsen G, Eilertsen BAW, von Hanno T et al (2014) Subclinical cardiovascular disease is associated with a high glomerular filtration rate in the nondiabetic general population. Kidney Int 86(1):146–153
van der Sande NG, Blankestijn PJ, Leiner T, van der Graaf Y, de Borst GJ, Cramer MJ et al (2017) High ratios of kidney function to kidney size are related to mortality and kidney function decline in high-risk patients. Eur J Prev Cardiol 24(9):926–933
Penno G, Orsi E, Solini A, Bonora E, Fondelli C, Trevisan R et al (2020) Renal hyperfiltration is independently associated with increased all-cause mortality in individuals with type 2 diabetes: a prospective cohort study. BMJ Open Diabetes Res Care 8(1):e001481
Melsom T, Schei J, Stefansson VTN, Solbu MD, Jenssen TG, Mathisen UD et al (2016) Prediabetes and risk of glomerular hyperfiltration and albuminuria in the general nondiabetic population: a prospective cohort study. Am J Kidney Dis 67(6):841–850
Low S, Zhang X, Wang J, Yeoh LY, Liu YL, Ang KKL et al (2018) Long-term prospective observation suggests that glomerular hyperfiltration is associated with rapid decline in renal filtration function: a multiethnic study. Diab Vasc Dis Res 15(5):417–423
Oh SW, Yang JH, Kim MG, Cho WY, Jo SK (2020) Renal hyperfiltration as a risk factor for chronic kidney disease: a health checkup cohort study. PLoS ONE 15(9):e0238177
Xie Y, Bowe B, Mokdad AH, Xian H, Yan Y, Li T et al (2018) Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int 94(3):567–581
Magee GM, Bilous RW, Cardwell CR, Hunter SJ, Kee F, Fogarty DG (2009) Is hyperfiltration associated with the future risk of developing diabetic nephropathy? A meta-analysis. Diabetologia 52(4):691–697
Murray CJL, Abbafati C, Abbas KM, Abbasi M, Abbasi-Kangevari M, Abd-Allah F et al (2020) Five insights from the global burden of disease study 2019. Lancet 396(10258):1135–1159
OuldSetti M, Kacimi SEO, Niskanen L, Tuomainen TP (2022) Mortality-based definition of renal hyperfiltration in middle-aged men: a 35-year cohort from Finland. Int Urol Nephrol 54(7):1673–1680
Daniel RM, De Stavola BL, Cousens SN (2011) Gformula: estimating causal effects in the presence of time-varying confounding or mediation using the G-computation formula. Stata J 11(4):479–517
Salonen JT (1988) Is there a continuing need for longitudinal epidemiologic research? The Kuopio ischaemic heart disease risk factor study. Ann Clin Res 20(1–2):46–50
Ilomäki J, Hajat A, Kauhanen J, Kurl S, Kaufman JS, Tuomainen TP et al (2012) Relationship between alcohol consumption and myocardial infarction among ageing men using a marginal structural model. Eur J Public Health 22(6):825–830
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek JW et al (2007) Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem 53(4):766–772
Chagnac A, Weinstein T, Herman M, Hirsh J, Gafter U, Ori Y (2003) The effects of weight loss on renal function in patients with severe obesity. J Am Soc Nephrol 14(6):1480–1486
Palatini P (2012) Glomerular hyperfiltration: a marker of early renal damage in pre-diabetes and pre-hypertension. Nephrol Dial Transplant 27(5):1708–1714
Maeda I, Hayashi T, Sato KK, Koh H, Harita N, Nakamura Y et al (2011) Cigarette smoking and the association with glomerular hyperfiltration and proteinuria in healthy middle-aged men. Clin J Am Soc Nephrol 6(10):2462–2469
Mickelsson M, Söderström E, Stefansson K, Andersson J, Söderberg S, Hultdin J (2021) Smoking tobacco is associated with renal hyperfiltration. Scand J Clin Lab Invest 81(8):622–628
Lin M, Su Q, Huang H, Zheng Y, Wen J, Yao J et al (2017) Alcohol consumption and the risk for renal hyperfiltration in the general Chinese population. Eur J Clin Nutr 71(4):500–505
Jhee JH, Nam KH, An SY, Cha MU, Lee M, Park S et al (2018) Severe vitamin D deficiency is a risk factor for renal hyperfiltration. Am J Clin Nutr 108(6):1342–1351
Nurmi T, Tuomainen TP, Virtanen J, Mursu J, Voutilainen S (2013) High-performance liquid chromatography and coulometric electrode array detector in serum 25-hydroxyvitamin D(3) and 25-hydroxyvitamin D(2) analyses. Anal Biochem 435(1):1–9
Tertsunen HM, Hantunen S, Tuomainen TP, Virtanen JK (2021) Adherence to a healthy Nordic diet and risk of type 2 diabetes among men: the Kuopio ischaemic heart disease risk factor study. Eur J Nutr [Internet]. https://doi.org/10.1007/s00394-021-02569-1
Kanerva N, Kaartinen NE, Schwab U, Lahti-Koski M, Männistö S (2014) The Baltic Sea diet score: a tool for assessing healthy eating in Nordic countries. Public Health Nutr 17(8):1697–1705
Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 51(6):1173–1182
VanderWeele TJ. Explanation in causal inference: methods for mediation and interaction [Internet]. New York: Oxford University Press; 2015. 1 p. Available from: http://www.site.ebrary.com/id/11006375. Accessed 9 Nov 2022
VanderWeele TJ, Vansteelandt S, Robins JM (2014) Effect decomposition in the presence of an exposure-induced mediator-outcome confounder. Epidemiology 25(2):300–306
Robins J (1986) A new approach to causal inference in mortality studies with a sustained exposure period—application to control of the healthy worker survivor effect. Math Model 7(9):1393–1512
Shi B, Choirat C, Coull BA, VanderWeele TJ, Valeri L (2021) CMAverse: A suite of functions for reproducible causal mediation analyses. Epidemiology 32(5):e20
VanderWeele TJ (2019) Principles of confounder selection. Eur J Epidemiol 34(3):211–219
Pearl J, Glymour M, Jewell NP (2016) Causal Inference in Statistics: a Primer, 1st edn. Wiley, Chichester, p 160
Schomaker M, Heumann C (2018) Bootstrap inference when using multiple imputation. Stat Med 37(14):2252–2266
VanderWeele TJ, Vansteelandt S (2010) Odds ratios for mediation analysis for a dichotomous outcome. Am J Epidemiol 172(12):1339–1348
Rijnhart JJM, Lamp SJ, Valente MJ, MacKinnon DP, Twisk JWR, Heymans MW (2021) Mediation analysis methods used in observational research: a scoping review and recommendations. BMC Med Res Methodol 21(1):226
Tonneijck L, Muskiet MHA, Smits MM, van Bommel EJ, Heerspink HJL, van Raalte DH et al (2017) Glomerular hyperfiltration in diabetes: mechanisms, clinical significance, and treatment. J Am Soc Nephrol 28(4):1023–1039
Vallon V, Gerasimova M, Rose MA, Masuda T, Satriano J, Mayoux E et al (2014) SGLT2 inhibitor empagliflozin reduces renal growth and albuminuria in proportion to hyperglycemia and prevents glomerular hyperfiltration in diabetic Akita mice. Am J Physiol Renal Physiol 306:F194-204
Knight EL, Stampfer MJ, Hankinson SE, Spiegelman D, Curhan GC (2003) The impact of protein intake on renal function decline in women with normal renal function or mild renal insufficiency. Ann Intern Med 138(6):460–467
Yoo KD, Yoon HJ, Hwang SS, Heo NJ, Chin HJ, Yang SH et al (2017) Different association between renal hyperfiltration and mortality by sex. Nephrology 22(10):804–810
Gaspari F, Ruggenenti P, Porrini E, Motterlini N, Cannata A, Carrara F et al (2013) The GFR and GFR decline cannot be accurately estimated in type 2 diabetics. Kidney Int 84(1):164–173
Sundin PO, Udumyan R, Fall K, Montgomery S (2019) Grip strength modifies the association between estimated glomerular filtration rate and all-cause mortality. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Ren Assoc 34(10):1799–1801
Stefansson VTN, Schei J, Jenssen TG, Melsom T, Eriksen BO (2016) Central obesity associates with renal hyperfiltration in the non-diabetic general population: a cross-sectional study. BMC Nephrol 17(1):172
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital. This work was funded by the Aarne Koskelon säätiö and the Aarne ja Aili Turusen säätiö. The funding sources had no role in the design or conduct of the study.
Author information
Authors and Affiliations
Contributions
Conceptualization: MOS, AV, LN. Data curation: AV, TPT. Formal analysis: MOS. Funding acquisition: MOS. Methodology: MOS, AV, LN. Project administration: AV, TPT. Visualization: MOS. Writing—original draft: MOS. Writing—review and editing: MOS, AV, LN, TPT.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
The study protocol was approved by the Research Ethics Committee of the University of Eastern Finland and the Research Ethics Committee Hospital District of Northern Savo, Finland (no. 143/97), and each participant gave written informed consent. The KIHD Study was performed in accordance with the Declaration of Helsinki. Cause of Death registry—Statistics Finland (Licence TK-53-1770-16). Care Register for Healthcare—National Institute for Health and Welfare (Licence THL/93/5.05.00/2013).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ould Setti, M., Voutilainen, A., Niskanen, L. et al. The association between renal hyperfiltration and mortality is not mediated by diabetes mellitus. Int Urol Nephrol 55, 2639–2645 (2023). https://doi.org/10.1007/s11255-023-03562-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03562-9