Abstract
Background
Acute kidney disease (AKD) following coronary angiography (CAG) indicates a higher risk of chronic kidney disease and follow-up cardiovascular comorbidities. However, the predictive risk factor of AKD is not clear. We sought to verify whether preoperative N-terminal pro-B-type natriuretic peptide (NT-proBNP) level was associated with AKD in patients undergoing CAG.
Method
We analyzed 7602 patients underwent CAG in this multi-center registry cohort study. Cardiorenal ImprovemeNt II (CIN-II) in five Chinese tertiary hospitals from 2007 to 2020. The primary outcome was AKD, defined as a ≥ 50% increase of serum creatinine within 7–90 days. Multivariable logistic regressions were used to assess the association between NT-proBNP and AKD.
Result
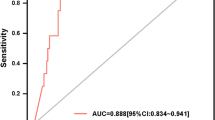
1009 patients (13.27%) eventually developed AKD, who were more likely to be female, older, and with comorbidities of chronic heart failure and anemia. After adjusting to the potential confounders, the NT-proBNP level remained an independent predictor of AKD (lnNT-proBNP OR: 1.20, 95% CI 1.13–1.28, p < 0.005). Restricted cubic spline analysis demonstrated a linear relationship between elevated NT-proBNP and AKD (p for trend < 0.001). In the subgroup analysis, elevated NT-proBNP level in patients with percutaneous coronary intervention (p for interaction < 0.001) or without previous congestive heart failure (p for interaction = 0.0346) has a more significant value of AKD prediction.
Conclusion
Pre-operative NT-proBNP level was independently associated with the risk of AKD in patients following CAG. Perioperative strategies are warranted to prevent AKD in patients with elevated NT-proBNP levels.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
McCullough PA, Choi JP, Feghali GA, Schussler JM, Stoler RM, Vallabahn RC, Mehta A (2016) Contrast-induced acute kidney injury. J Am Coll Cardiol 68(13):1465–1473
Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, Bittleman D, Cruz D, Endre Z, Fitzgerald RL et al (2017) Acute kidney disease and renal recovery: consensus report of the acute disease quality initiative (ADQI) 16 workgroup. Nat Rev Nephrol 13(4):241–257
Xiao YQ, Cheng W, Wu X, Yan P, Feng LX, Zhang NY, Li XW, Duan XJ, Wang HS, Peng JC et al (2020) Novel risk models to predict acute kidney disease and its outcomes in a Chinese hospitalized population with acute kidney injury. Sci Rep 10(1):15636
James MT, Levey AS, Tonelli M, Tan Z, Barry R, Pannu N, Ravani P, Klarenbach SW, Manns BJ, Hemmelgarn BR (2019) Incidence and prognosis of acute kidney diseases and disorders using an integrated approach to laboratory measurements in a universal health care system. JAMA Netw Open 2(4):e191795
Nagata K, Horino T, Hatakeyama Y, Matsumoto T, Terada Y, Okuhara Y (2021) Effects of transient acute kidney injury, persistent acute kidney injury and acute kidney disease on the long-term renal prognosis after an initial acute kidney injury event. Nephrology (Carlton) 26(4):312–318
Peerapornratana S, Priyanka P, Wang S, Smith A, Singbartl K, Palevsky PM, Chawla LS, Yealy DM, Angus DC, Kellum JA (2020) Sepsis-associated acute kidney disease. Kidney Int Rep 5(6):839–850
Ostermann M, Bellomo R, Burdmann EA, Doi K, Endre ZH, Goldstein SL, Kane-Gill SL, Liu KD, Prowle JR, Shaw AD et al (2020) Controversies in acute kidney injury: conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) Conference. Kidney Int 98(2):294–309
Kimmel LA, Wilson S, Janardan JD, Liew SM, Walker RG (2014) Incidence of acute kidney injury following total joint arthroplasty: a retrospective review by RIFLE criteria. Clin Kidney J 7(6):546–551
Hassan BK, Sahlström A, Dessau RB (2015) Risk factors for renal dysfunction after total hip joint replacement; a retrospective cohort study. J Orthop Surg Res 10:158
Praga M, Sevillano A, Auñón P, González E (2015) Changes in the aetiology, clinical presentation and management of acute interstitial nephritis, an increasingly common cause of acute kidney injury. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc Eur Renal Assoc 30(9):1472–1479
Naruse H, Ishii J, Takahashi H, Kitagawa F, Nishimura H, Kawai H, Muramatsu T, Harada M, Yamada A, Motoyama S et al (2018) Predicting acute kidney injury using urinary liver-type fatty-acid binding protein and serum N-terminal pro-B-type natriuretic peptide levels in patients treated at medical cardiac intensive care units. Crit Care (Lond Engl) 22(1):197
Haines R, Crichton S, Wilson J, Treacher D, Ostermann M (2017) Cardiac biomarkers are associated with maximum stage of acute kidney injury in critically ill patients: a prospective analysis. Crit Care (Lond Engl) 21(1):88
Fujii T, Uchino S, Takinami M, Bellomo R (2014) Subacute kidney injury in hospitalized patients. Clin J Am Soc Nephrol CJASN 9(3):457–461
Matsuura R, Iwagami M, Moriya H, Ohtake T, Hamasaki Y, Nangaku M, Doi K, Kobayashi S, Noiri E (2020) The clinical course of acute kidney disease after cardiac surgery: a retrospective observational study. Sci Rep 10(1):6490
Wolsk E, Claggett B, Pfeffer MA, Diaz R, Dickstein K, Gerstein HC, Lawson FC, Lewis EF, Maggioni AP, McMurray JJV et al (2017) Role of B-type natriuretic peptide and N-terminal prohormone BNP as predictors of cardiovascular morbidity and mortality in patients with a recent coronary event and type 2 diabetes mellitus. J Am Heart Assoc. https://doi.org/10.1161/JAHA.116.004743
Santaguida PL, Don-Wauchope AC, Oremus M, McKelvie R, Ali U, Hill SA, Balion C, Booth RA, Brown JA, Bustamam A et al (2014) BNP and NT-proBNP as prognostic markers in persons with acute decompensated heart failure: a systematic review. Heart Fail Rev 19(4):453–470
Oremus M, Don-Wauchope A, McKelvie R, Santaguida PL, Hill S, Balion C, Booth R, Brown JA, Ali U, Bustamam A et al (2014) BNP and NT-proBNP as prognostic markers in persons with chronic stable heart failure. Heart Fail Rev 19(4):471–505
Hall C (2004) Essential biochemistry and physiology of (NT-pro)BNP. Eur J Heart Fail 6(3):257–260
Cao Z, Jia Y, Zhu B (2019) BNP and NT-proBNP as diagnostic biomarkers for cardiac dysfunction in both clinical and forensic medicine. Int J Mol Sci 20(8):1820
Silver MA, Maisel A, Yancy CW, McCullough PA, Burnett JC Jr, Francis GS, Mehra MR, Fonarow G, Gibler WB et al (2004) BNP Consensus Panel 2004: a clinical approach for the diagnostic, prognostic, screening, treatment monitoring, and therapeutic roles of natriuretic peptides in cardiovascular diseases. Congest Heart Fail (Greenwich, Conn) 10(5 Suppl 3):1–30
Moltrasio M, Cabiati A, Milazzo V, Rubino M, De Metrio M, Discacciati A, Rumi P, Marana I, Marenzi G (2014) B-type natriuretic peptide and risk of acute kidney injury in patients hospitalized with acute coronary syndromes*. Crit Care Med 42(3):619–624
Goussot S, Mousson C, Guenancia C, Stamboul K, Brunel P, Brunet D, Touzery C, Cottin Y, Zeller M (2015) N-terminal fragment of pro B-type natriuretic peptide as a marker of contrast-induced nephropathy after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol 116(6):865–871
Liu YH, Jiang L, Chen JY, Tan N, Liu Y, He PC (2016) Does N-terminal pro-brain natriuretic peptide add prognostic value to the Mehran risk score for contrast-induced nephropathy and long-term outcomes after primary percutaneous coronary intervention? Int Urol Nephrol 48(10):1675–1682
Welsh P, Woodward M, Hillis GS, Li Q, Marre M, Williams B, Poulter N, Ryan L, Harrap S, Patel A et al (2014) Do cardiac biomarkers NT-proBNP and hsTnT predict microvascular events in patients with type 2 diabetes? Results from the ADVANCE trial. Diabetes Care 37(8):2202–2210
Bidadkosh A, Lambooy SPH, Heerspink HJ, Pena MJ, Henning RH, Buikema H, Deelman LE (2017) Predictive properties of biomarkers GDF-15, NTproBNP, and hs-TnT for morbidity and mortality in patients with type 2 diabetes with nephropathy. Diabetes Care 40(6):784–792
Ronco C, Bellasi A, Di Lullo L (2018) Cardiorenal syndrome: an overview. Adv Chronic Kidney Dis 25(5):382–390
Kofman N, Margolis G, Gal-Oz A, Letourneau-Shesaf S, Keren G, Rozenbaum Z, Shacham Y (2019) Long-term renal outcomes and mortality following renal injury among myocardial infarction patients treated by primary percutaneous intervention. Coron Artery Dis 30(2):87–92
Chalikias G, Drosos I, Tziakas DN (2016) Contrast-induced acute kidney injury: an update. Cardiovasc Drugs Ther 30(2):215–228
Hur M, Koo CH, Lee HC, Park SK, Kim M, Kim WH, Kim JT, Bahk JH (2017) Preoperative aspirin use and acute kidney injury after cardiac surgery: a propensity-score matched observational study. PLoS One 12(5):e0177201
Su X, Xie X, Liu L, Lv J, Song F, Perkovic V, Zhang H (2017) Comparative effectiveness of 12 treatment strategies for preventing contrast-induced acute kidney injury: a systematic review and Bayesian network meta-analysis. Am J Kidney Dis 69(1):69–77
Pattharanitima P, Tasanarong A (2014) Pharmacological strategies to prevent contrast-induced acute kidney injury. Biomed Res Int 2014:236930
Funding
This work was supported by grants from Beijing Lisheng Cardiovascular Health Foundation (LHJJ20141751); Guangdong Provincial science and technology project (2020B1111170011, KJ022021049); Guangdong Provincial People's Hospital Foundation (DFJH201919), and Guangdong Provincial Key Laboratory of Coronary Heart Disease Prevention (No.Y0120220151). The work was not funded by any industry sponsors.
Author information
Authors and Affiliations
Contributions
YL, YH, SC, JC contributed to the study’s conception and design. WG, QL, SY, HH, RZ, ZH, JL contributed to literature search, studies screening and data extraction. YL, YH contributed to the analysis and the first draft of the manuscript. JC, YL, JL, SC commented on and revised the final versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The study was approved by the institutional Ethics Research Committee of Guangdong Provincial People’s Hospital (No. GDREC2012141H).
Consent to participate
Written informed consent was obtained from all involved patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ling, Y., He, Y., Guo, W. et al. Association of N-terminal pro-B-type natriuretic peptide (NT-proBNP) and acute kidney disease in patients undergoing coronary angiography: a cohort study. Int Urol Nephrol 55, 2067–2073 (2023). https://doi.org/10.1007/s11255-023-03491-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03491-7