Abstract
Background
N-terminal B-type natriuretic peptide (NT-proBNP) discriminates mortality risk in diabetes mellitus (DM) and in heart failure (HF) populations. Whether DM status modifies the association between NT-proBNP and all-cause mortality risk in ischemic HF is unknown.
Methods
This was a single-center, prospective cohort study conducted with 2287 ischemic HF patients. Subjects were divided into with DM group and without DM group. Multivariate Cox proportional-hazards models were conducted to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs). The product of DM status and NT-proBNP were used to assess the interaction. Propensity score matching analysis was used to verify the robustness of the results.
Results
Of 2287 ischemic HF participants, 1172 (51.2%) had DM. After a median follow-up of 3.19 years (7287 person-years), 479 (20.9%) of the participants died. After adjusting for the covariates, continuous NT-proBNP was more prominently associated with risk of mortality in HF patients with DM (HR: 1.65, 95% CI: 1.43–1.91) than those without (HR: 1.28, 95% CI: 1.09–1.50). A significant interaction of DM status and NT-proBNP was observed (P-interaction = 0.016). The relationships were consistent when NT-proBNP was considered as a categorical variable and in the propensity matching analysis.
Conclusions
DM status modified the association between NT-proBNP and all-cause mortality in ischemic HF patients, suggesting that NT-proBNP was more prominently associated with risk of mortality in patients with DM than those without. Future studies to clarify the mechanisms underlying these observations are needed.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) and heart failure (HF) commonly co-exist, and the presence of type 2 DM increases the incidence of HF and subsequent events [1,2,3,4,5]. The prevalence of DM and HF is projected to further increase with aging populations and lifestyle changes [6,7,8]. Improvement in prognosis prediction in HF patients complicated with DM is a top priority.
N-terminal B-type natriuretic peptide (NT-proBNP) is of greatest importance in the diagnosis and prognosis prediction in HF patients. Previous studies consistently demonstrated a clear relationship between NT-proBNP and subsequent risk of adverse cardiovascular outcomes [9, 10]. Recently, a report from a community-based cohort study consisting of 5861 subjects showed that NT-proBNP alone discriminated mortality risk better than traditional risk factors in people with DM. While in individuals without DM, the predicting ability of NT-proBNP was similar to the conventional risk factors, suggesting that NT-proBNP performed especially well in predicting death in general DM populations [11]. However, whether the association of NT-proBNP and all-cause mortality in HF patients varies by DM status remains unknown.
Accordingly, we hypothesized that DM status might modify the association between NT-proBNP and mortality risk in HF patients. Leveraging an ongoing prospective ischemic HF cohort, we aimed to evaluate the relationship between NT-proBNP and all-cause mortality among patients with and without DM.
Methods
Study design and participants
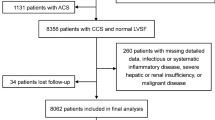
Designs and details of this prospective, single-center, ischemic HF cohort study have been described previously [12, 13]. Briefly, patients hospitalized at the department of cardiology of Guangdong Provincial People’s Hospital from December 2015 to October 2020 were screened and enrolled after informed consent was obtained. Ischemic HF was defined as prior myocardial infarction (MI) or prior revascularization, or being confirmed by coronary angiography during hospitalization, and left ventricular ejection fraction (LVEF) ≤ 50% evaluated by echocardiography (subjects with LVEF ≤ 45% were screened before 2019). Patients who were without NT-proBNP data, lost to follow-up, or died in the hospital were excluded (Fig. 1). This study was approved by the Clinical Research Ethics Committee of Guangdong Provincial People’s Hospital (No. 2,017,128 H) and performed in accordance with the Declaration of Helsinki.
Study procedure
Baseline data of demographics, vital signs at admission, reasons for admission, comorbidities, laboratory, angiographic findings, and medical treatment at discharge were extracted from the medical records of Guangdong Provincial People’s Hospital. Non-fasting venous blood was drawn to evaluate NT-proBNP using an electrochemiluminescence automatic immunoassay system (Roche Eleesys ~ 2010disk, Switzerland) in the clinical laboratory. Other laboratory tests were completed in the clinical laboratory of Guangdong Provincial People’s Hospital. DM was defined as currently using anti-hypertensive treatment, being diagnosed by a physician, fasting blood glucose (FBG) ≥ 7.0mmol/L, or glycated hemoglobin A1c (HbA1C) ≥ 6.5%[14].
Follow-up and study endpoint
Follow-ups were completed by two treated investigators blinded to the baseline data using phone-call interviews. All-cause mortality was defined as the only study endpoint because the death reasons cannot be accurately assessed through telephone visits. The length of follow-up was calculated as the death date or the last follow-up date minus the discharge date, whichever came first. All participants were followed through on June 30th, 2022.
Statistical analysis
Subjects were first categorized as with DM and without DM according to the above criteria. Continuous variables were presented as mean value ± standard deviation (SD) or median (interquartile range) and categorical variables were presented as numbers (percentage). Differences between patients with and without DM were compared using Student’s t-test, Wilcoxon rank sum test, and chi-square test accordingly.
The Kaplan–Meier (KM) method was used to estimate the cumulative rate of all-cause mortality stratified by categorical NT-proBNP groups (≥ 1800 pg/ml and < 1800 pg/ml) and DM status (with and without DM). The Cox proportional-hazards models were conducted to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) with adjustment for covariates presented in Table 1. 5 models were constructed. Model 1 adjusted for age and sex; Model 2 adjusted for model 1 plus smoking status, heart rate, NYHA class, and reasons for admission; Model 3 adjusted for model 2 plus laboratory at admission, left ventricular ejection fraction, coronary angiography, and in-hospital percutaneous coronary intervention; Model 4 adjusted for model 3 plus comorbidities; Model 5 adjusted for model 4 plus medications at discharge. The product of DM status and NT-proBNP were included in each model to assess the interaction.
A 1:1 ratio propensity-matched analysis with a caliper value of 0.02 was further performed to verify the robustness of the results. 29 variables, including sex, age, vital signs at admission, reasons for admission, NYHA class, coronary angiography, LVEF, laboratory, smoking status, and comorbidities, were selected based on investigator judgment for the propensity model. The propensity to DM versus non-DM was predicted by the multivariable logistic regression model, and post-estimations for propensity score-matched were evaluated by standardized bias and propensity score density [15]. Subjects were matched to the nearest available propensity score and those who have been successfully matched were removed from the model. The procedure was repeated until all DM patients were matched. 2 Cox models were then constructed. Model 1 adjusted for none, and model 2 adjusted for medications at discharge (which did not include in the propensity-matched model but had a significant impact on the mortality).
All analyses were performed using Stata version 15.1 (StataCorp LLC, College Station, TX, USA). Two-sided p-values < 0.1 for interaction tests and p-values < 0.05 for other analyses were considered statistically significant.
Results
Baseline characteristics of participants with and without diabetes mellitus
A total of 2287 ischemic HF patients with LVEF ≤ 50% were enrolled, and 1172 (51.2%) participants had DM. Overall, participants were on average 63.7 years old and 84.4% of them were male. The mean LVEF and median NT-proBNP were 36.3% and 1568 pg/ml, respectively. The histograms of log-NT-proBNP values for all participants (Panel A) and participants with (Panel B) and without DM (Panel C) were also displayed in Fig. 2. The most prevalent comorbidity was coronary artery disease, with 55.4% of subjects having prior revascularization, followed by hypertension (53.7%), DM (51.2%), MI (38.7%), and chronic kidney disease (CKD) (27.1%).
The Histograms for Log-NT-proBNP Values. (A) The histograms for log-NT-proBNP values in all participants. (B) The histograms for log-NT-proBNP values in participants with DM. (C) The histograms for log-NT-proBNP values in participants without DM. NT-proBNP, N-terminal pro-B-type natriuretic peptide; DM, diabetes mellitus
Compared with the DM group, patients without DM had lower heart rates, were less likely to present with acute HF and NYHA III-IV, and had higher hemoglobin and estimated glomerular filtration rate (eGFR) levels. The prevalence of triple vessel disease, hypertension, and CKD was higher in the DM group than in those without DM. Besides, patients with DM also had higher high-sensitivity cardiac troponin-T and NT-proBNP levels. (Table 1)
NT-proBNP and all-cause mortality risk in patients with and without diabetes mellitus
After a median follow-up of 3.19 years (7287 person-years), 479 (20.9%) of the participants died. The incidence rates of patients with and without DM were 7.3 (6.5–8.3) and 5.8 (5.1–6.7) per 100 person-years. When NT-proBNP was considered as a continuous variable, 1-SD NT-proBNP increase was significantly associated with mortality risk in ischemic HF patients (HR: 1.46, 95% CI: 1.31–1.62) even after adjusting for the covariates, and the association was more pronounced in those with DM (HR: 1.65, 95% CI: 1.43–1.91) than those without (HR: 1.28, 95% CI: 1.09–1.50) (P-interaction = 0.016). When NT-proBNP was considered as a categorical variable, NT-proBNP ≥ 1800pg/ml was consistently and positively associated with mortality risk (HR: 1.88, 95% CI: 1.48–2.41) (Fig. 3 Panel A and Table 2). Similarly, the association was also more pronounced in those with DM (HR: 2.39, 95% CI: 1.70–3.36) than those without (HR: 1.50, 95% CI: 1.04–2.18) (P-interaction = 0.042) (Table 2).
NT-proBNP and all-cause mortality risk in propensity-matched participants
We matched 777 patients with DM to those without DM in a 1:1 ratio. After propensity matching, difference and standardized bias in baseline characteristics between groups significantly reduce (Supplemental Figs. 1 and 2), and there was no difference in baseline characteristics between patients with and without DM (Supplemental Table 1). In the propensity matching analyses, both continuous and categorical NT-proBNP was more prominently associated with the risk of mortality in the DM group than the non-DM group. The association remained consistent even after adjusting for the prescribed medications at discharge. (Fig. 3 Panel B and Table 3)
Discussion
The current study re-emphasized that higher NT-proBNP level was significantly related to all-cause mortality risk among ischemic HF patients. What’s interesting was that DM status might modify such association, indicating that NT-proBNP was more prominently associated with risk of mortality in HF patients with DM than those without. Furthermore, the results remained consistent even after adjusting for conventional risk factors or after propensity matching.
NT-proBNP is strongly associated with adverse cardiovascular outcomes and mortality in HF populations [16] and plays an important role in the diagnosis and management of HF [17, 18]. Beyond HF, NT-proBNP also has a good ability to predict death in general populations [10] and patients with DM [19]. Furthermore, a recent study from the Atherosclerosis Risk in Communities (ARIC) cohort showed that NT-proBNP discriminated mortality risk better than conventional risk factors only in subjects with DM instead of non-DM people after a median of 7.2 years of follow-up [11], which suggested that DM status may modify the relationship between NT-proBNP and risk of death. However, this study only involved general people from the western country [11], and whether the conclusions can be generalized to Chinese HF patients remains inconclusive. To the best of our knowledge, the present study was the first to investigate the relationship between NT-proBNP and mortality in ischemic HF with and without DM and demonstrated that DM status did modify this association among HF patients. The conclusions were robust even in the propensity-matching cohort.
The current study did not clarify the mechanisms underlying these observations, and the theories to explain are hypothetical. First, people with DM tend to have higher body mass index (BMI)[20] and NT-proBNP is inversely associated with BMI [21]. Hence, an equivalent increasement of NT-proBNP may reflect higher atrial pressure in DM individuals than their counterparts without DM, indirectly representing worse cardiac function among DM subjects. Second, although NT-proBNP is inversely associated with the incidence of DM [22,23,24], a study including 1294 individuals showed that NT-proBNP was positively associated with microvascular (HR: 1.20; 95% CI: 1.01–1.43) and macrovascular (HR: 1.37; 95% CI: 1.03–1.83) complications in those with incident DM [24], which have a deleterious impact on human health. At present, NT-proBNP and DM were deemed as partners in crime in the incidence and progression of HF [25], better clarification of the mortality risk of NT-proBNP between HF patients with different DM statuses might have a significant impact on public health and thus improve risk stratification.
DM is common in HF, and sodium-dependent glucose transporter 2 inhibitor (SGLT2i) is a promising drug and provides beneficial cardiovascular effects in DM [26] and in HF [17] in the contemporary era. The protective effects were attributed to several mechanisms, including the diuretic effect of SGLT2i, more efficient production of ATP, and mitochondrial function reestablishment [27,28,29]. The effect of SGLT2i on NT-proBNP was also recognized as another potential pathway to produce a beneficial impact [30, 31] but remains controversial [32]. Our current results provide robust evidence that the association between NT-proBNP and mortality was more remarkable in HF patients with DM than without, suggesting that lowering NT-proBNP levels in patients with HF and DM would be a promising direction to gain benefit. Beyond NT-proBNP, a recent study has also demonstrated that disintegrin and metalloprotease protein-17 were markedly expressed in mice with diabetic cardiomyopathy [33], which was then essential for cleaving angiotensin-converting enzyme 2 and accelerated the cardiac remodeling. Taken together, inhibition of these potential biomarkers might provide a more promising approach to the treatment of HF patients with DM.
Limitations
The present study has some noteworthy limitations. First, this is a single-center cohort study, the study conclusions may not be generalizable to all ischemic HF patients. Second, some unmeasured and unknown confounding factors may still exist and influence the current results, although we have adjusted for multiple covariates and conducted propensity score matching analysis. Third, the current study used all-cause mortality as the only primary endpoint; therefore, whether the conclusions can be generalized to other cardiovascular outcomes is unknown. Forth, whether DM status modifies the effect of SGLT2i on NT-proBNP can not be investigated because of the low usage rate. Fifth, subjects can not be further categorized as non-DM and pre-DM due to the small sample size and inadequate power of the test.
Conclusions
DM status modified the association between NT-proBNP and all-cause mortality in ischemic HF patients, and NT-proBNP was more prominently associated with the risk of mortality in patients with DM than those without. Future studies are needed to clarify the mechanisms underlying these observations and to investigate the drug effect on NT-proBNP in patients with and without DM.
Data availability
The deidentified participant data will be shared on a request basis. Please directly contact the corresponding author to request data sharing.
Abbreviations
- DM:
-
diabetes mellitus
- HF:
-
heart failure
- N-terminal B-type natriuretic peptide:
-
NT-proBNP
- MI:
-
myocardial infarction
- LVEF:
-
left ventricular ejection fraction
- FBG:
-
fasting blood glucose
- HbA1C:
-
hemoglobin A1c
- SD:
-
standard deviation
- HR:
-
hazard ratio
- CI:
-
confidence interval
- CKD:
-
chronic kidney disease
- eGFR:
-
estimated glomerular filtration rate
- ARIC:
-
Atherosclerosis Risk in Communities
- BMI:
-
body mass index
- SGLT2i:
-
sodium-dependent glucose transporters 2 inhibitor
References
Thomas MC. Type 2 diabetes and heart failure: Challenges and Solutions. Curr Cardiol Rev. 2016;12(3):249–55.
Aune D, Schlesinger S, Neuenschwander M, Feng T, Janszky I, Norat T, Riboli E. Diabetes mellitus, blood glucose and the risk of heart failure: a systematic review and meta-analysis of prospective studies. Nutr metabolism Cardiovasc diseases: NMCD. 2018;28(11):1081–91.
Maack C, Lehrke M, Backs J, Heinzel FR, Hulot JS, Marx N, Paulus WJ, Rossignol P, Taegtmeyer H, Bauersachs J, et al. Heart failure and diabetes: metabolic alterations and therapeutic interventions: a state-of-the-art review from the Translational Research Committee of the heart failure Association-European Society of Cardiology. Eur Heart J. 2018;39(48):4243–54.
Seferović PM, Petrie MC, Filippatos GS, Anker SD, Rosano G, Bauersachs J, Paulus WJ, Komajda M, Cosentino F, de Boer RA, et al. Type 2 diabetes mellitus and heart failure: a position statement from the heart failure association of the European Society of Cardiology. Eur J Heart Fail. 2018;20(5):853–72.
Zareini B, Rørth R, Holt A, Mogensen UM, Selmer C, Gislason G, Schou M, Køber L, Torp-Pedersen C, Lamberts M, et al. Heart failure and the prognostic impact and incidence of new-onset of diabetes mellitus: a nationwide cohort study. Cardiovasc Diabetol. 2019;18(1):79.
Bragazzi NL, Zhong W, Shu J, Abu Much A, Lotan D, Grupper A, Younis A, Dai H. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. Eur J Prev Cardiol. 2021;28(15):1682–90.
GBD 2019 Diabetes Mortality Collaborators. Diabetes mortality and trends before 25 years of age: an analysis of the global burden of Disease Study 2019. The lancet Diabetes & endocrinology. 2022;10(3):177–92.
Tromp J, Ferreira JP, Janwanishstaporn S, Shah M, Greenberg B, Zannad F, Lam CSP. Heart failure around the world. Eur J Heart Fail. 2019;21(10):1187–96.
Natriuretic Peptides Studies Collaboration, Willeit P, Kaptoge S, Welsh P, Butterworth AS, Chowdhury R, Spackman SA, Pennells L, Gao P, Burgess S, et al. Natriuretic peptides and integrated risk assessment for cardiovascular disease: an individual-participant-data meta-analysis. The lancet Diabetes & endocrinology. 2016;4(10):840–9.
Wang TJ, Larson MG, Levy D, Benjamin EJ, Leip EP, Omland T, Wolf PA, Vasan RS. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350(7):655–63.
Wijkman MO, Claggett BL, Malachias MVB, Vaduganathan M, Ballantyne CM, Kitzman DW, Mosley T, Matsushita K, Solomon SD, Pfeffer MA. Importance of NT-proBNP and conventional risk factors for prediction of death in older adults with and without diabetes mellitus- A report from the atherosclerosis risk in Communities (ARIC) study. Diabetes Res Clin Pract. 2022;194:110164.
Cai A, Wu Z, Xu L, Xia S, He X, Zhang Y, Chen J, Zhou Y, Li L. Association of anaemia and all-cause mortality in patients with ischaemic heart failure varies by renal function status. ESC heart failure. 2021;8(3):2270–81.
Qiu W, Xiao X, Cai A, Gao Z, Li L. Pulse pressure and all-cause mortality in ischaemic heart failure patients: a prospective cohort study. Ann Med. 2022;54(1):2701–9.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, et al. 2. Classification and diagnosis of diabetes: Standards of Care in Diabetes—2023. Diabetes Care. 2022;46(Supplement1):19–S40.
Brookhart MA, Wyss R, Layton JB, Stürmer T. Propensity score methods for confounding control in nonexperimental research. Circulation Cardiovasc Qual outcomes. 2013;6(5):604–11.
Levin ER, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998;339(5):321–8.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–726.
Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, et al. 2022 AHA/ACC/HFSA Guideline for the management of Heart failure: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(17):1757–80.
Sabbatinelli J, Giuliani A, Bonfigli A, Ramini D, Matacchione G, Campolucci C, Ceka A, Tortato E, Rippo M, Procopio A, et al. Prognostic value of soluble ST2, high-sensitivity cardiac troponin, and NT-proBNP in type 2 diabetes: a 15-year retrospective study. Cardiovasc Diabetol. 2022;21(1):180.
Choukem S, Dimala C. BMI and diabetes risk in low-income and middle-income countries. Lancet (London England). 2021;398(10296):190–2.
Suthahar N, Meems L, Groothof D, Bakker S, Gansevoort R, van Veldhuisen D, de Boer R. Relationship between body mass index, cardiovascular biomarkers and incident heart failure. Eur J Heart Fail. 2021;23(3):396–402.
Pfister R, Sharp S, Luben R, Welsh P, Barroso I, Salomaa V, Meirhaeghe A, Khaw KT, Sattar N, Langenberg C, et al. Mendelian randomization study of B-type natriuretic peptide and type 2 diabetes: evidence of causal association from population studies. PLoS Med. 2011;8(10):e1001112.
Everett BM, Cook NR, Chasman DI, Magnone MC, Bobadilla M, Rifai N, Ridker PM, Pradhan AD. Prospective evaluation of B-type natriuretic peptide concentrations and the risk of type 2 diabetes in women. Clin Chem. 2013;59(3):557–65.
Birukov A, Eichelmann F, Kuxhaus O, Polemiti E, Fritsche A, Wirth J, Boeing H, Weikert C, Schulze M. Opposing Associations of NT-proBNP with risks of diabetes and diabetes-related complications. Diabetes Care. 2020;43(12):2930–7.
Bayes-Genis A. Diabetes and NT-proBNP: partners in crime. Diabetes Res Clin Pract. 2022;194:110165.
American Diabetes A. 9. Pharmacologic approaches to Glycemic Treatment: Standards of Medical Care in Diabetes—2021. Diabetes Care. 2020;44(Supplement1):111–S124.
Mudaliar S, Polidori D, Zambrowicz B, Henry RR. Sodium-glucose cotransporter inhibitors: Effects on renal and intestinal glucose transport: from bench to Bedside. Diabetes Care. 2015;38(12):2344–53.
Baartscheer A, Schumacher CA, Wüst RC, Fiolet JW, Stienen GJ, Coronel R, Zuurbier CJ. Empagliflozin decreases myocardial cytoplasmic na(+) through inhibition of the cardiac na(+)/H(+) exchanger in rats and rabbits. Diabetologia. 2017;60(3):568–73.
Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61(10):2108–17.
Januzzi JL Jr, Butler J, Jarolim P, Sattar N, Vijapurkar U, Desai M, Davies MJ. Effects of Canagliflozin on Cardiovascular biomarkers in older adults with type 2 diabetes. J Am Coll Cardiol. 2017;70(6):704–12.
Kusunose K, Imai T, Tanaka A, Dohi K, Shiina K, Yamada T, Kida K, Eguchi K, Teragawa H, Takeishi Y, et al. Effects of canagliflozin on NT-proBNP stratified by left ventricular diastolic function in patients with type 2 diabetes and chronic heart failure: a sub analysis of the CANDLE trial. Cardiovasc Diabetol. 2021;20(1):186.
Nassif ME, Windsor SL, Tang F, Khariton Y, Husain M, Inzucchi SE, McGuire DK, Pitt B, Scirica BM, Austin B, et al. Dapagliflozin Effects on biomarkers, symptoms, and functional status in patients with heart failure with reduced ejection fraction: the DEFINE-HF Trial. Circulation. 2019;140(18):1463–76.
Xue F, Cheng J, Liu Y, Cheng C, Zhang M, Sui W, Chen W, Hao P, Zhang Y, Zhang C. Cardiomyocyte-specific knockout of ADAM17 ameliorates left ventricular remodeling and function in diabetic cardiomyopathy of mice. Signal Transduct Target therapy. 2022;7(1):259.
Acknowledgements
We are indebted to all members who contributed to this work.
Funding
This current study was supported by the Key Area R&D Program of Guangdong Province (No.2019B020227005), the Climbing Plan of Guangdong Provincial People’s Hospital (DFJH2020022), Guangdong Provincial Clinical Research Center for Cardiovascular disease (2020B111117011) and Guangdong Provincial Key Laboratory of Coronary Heart Disease Prevention (No.Y0120220151).
Author information
Authors and Affiliations
Contributions
Dr. Weida Qiu contributed to the data acquisition, analysis and drafted the manuscript. Dr. Anping Cai provided study concept and design, and revised the manuscript. Mrs. Xiaoju Xiao contributed to the data collection. Dr. Zhiping Gao and Prof. Liwen Li contributed to the conception and design of the work. Prof. Liwen Li and Prof. Yingqing Feng contributed to funding obtained and provide administrative, technical, or material support. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Clinical Research Ethics Committee of Guangdong Provincial People’s Hospital (No. 2017128 H) and performed in accordance with the Declaration of Helsinki. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
None declared.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qiu, W., Cai, A., Xiao, X. et al. Diabetes mellitus status modifies the association between N-terminal B-type natriuretic peptide and all-cause mortality risk in ischemic heart failure: a prospective cohort study. Diabetol Metab Syndr 15, 72 (2023). https://doi.org/10.1186/s13098-023-01046-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01046-5