Abstract
Objective
To determine the efficacy of novel wearable transcutaneous tibial nerve stimulation (TTNS) device on bladder reflex in cats compared to implantable tibial nerve stimulation (ITNS).
Materials and methods
Two self-adhesive electrodes of the TTNS device were placed at the left leg, and ITNS was applied to stimulate the tibial nerve of the right leg, respectively. The intensity threshold (T) was defined as inducing observable toe movement. Multiple cystometrograms (CMGs) with normal saline (NS) infusion were performed to determine the inhibitory effects of TTNS and ITNS on the micturition reflex.
Results
TTNS at 4 times T (4 T), 6 times T (6 T), and the maximum output current intensity 24 mA significantly increased the bladder capacity (BC) compared to the control level (8.70 ± 2.46 ml) (all p < 0.05); however, there was no statistical significance among the three intensities. At the same time, ITNS at 2 times T (2 T), 4 T, 6 T, and the current intension 24 mA could significantly increase the BC compared to the control level (all p < 0.05). Likewise, no significant difference was observed among the four intensities (p > 0.05). The T values of TTNS were higher than those of ITNS (p = 0.02). The inhibitory effects of TTNS and ITNS revealed no significant difference at their respective 2 T, 4 T, 6 T, and 24 mA. Neither TTNS nor ITNS changed the contraction duration and amplitude (all p > 0.05).
Conclusions
TTNS was effective in increasing BC. The non-invasive neuromodulation technique could achieve a similar effect as ITNS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive bladder (OAB) describes the symptom complex of urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology [1]. Even though sacral neuromodulation (SNM) is the U.S. Food and Drug Administration-approved therapy that treats OAB, a certain period of time is needed to assess effectiveness before the implantation of a permanent pulse generator and the economic cost may be a big challenge for patients [2, 3]. Similar to SNM, intra-vesical injections of onabotulinumtoxinA (BoNT-A) is an invasive therapy which benefits patients with refractory symptoms who did not experience any improvement with conservative and pharmacological measures. BoNT-A can be performed under cystoscope guidance using intravenous sedation, so it is minimally invasive. However, reinjection may be needed every 6 months because of its self-limited duration and effect [4]. Tibial nerve stimulation (TNS) is an option for OAB patients who are refractory to conservative therapies [5]. At present, there are three types of TNS methods: percutaneous tibial nerve stimulation (PTNS), implantable tibial nerve stimulation (ITNS), and transcutaneous tibial nerve stimulation (TTNS) [6]. During PTNS, the tip of a needle electrode is inserted into the medial malleolus, which may cause a series of complications, such as bleeding, infection, and pain. ITNS requires implantation of a stimulator into the tibial nerve, which may induce similar side effects as PTNS. In addition, both PTNS and ITNS need to be performed by professional medical workers. Given all this, there is an urgent need for exploiting a non-invasive TTNS device that can be used at home, especially during the time of the COVID-19 pandemic.
Even though the effectiveness of TTNS compared to PTNS has been investigated by some researchers and results indicated that TTNS has efficacy equal to PTNS in the management of OAB [7, 8], a few studies explored the effects of TTNS compared with ITNS.
In this study, we examined the effects of a novel wearable homemade TTNS device on bladder reflex with normal saline (NS) infusion. Meanwhile, we evaluated the effects of TTNS compared with ITNS.
Materials and methods
TTNS device introduction
The butterfly-shaped TTNS device (General Stim Inc., Hangzhou, Zhejiang, China), which has esthetic qualities and is convenient to hold, consists of three parts: the stimulation unit, surface electrodes, and the mobile terminal unit (Fig. 1). The dimension of the stimulation unit with a rechargeable lithium battery is 58.3 * 55.6 * 12.8 mm (width, height, and depth), and the weight is only 70 g. With two working modes (program-controlled mode and offline mode), the patients can apply the simulator themselves regardless if they have an intelligent terminal or not. However, more simulated parameters can be modulated under the program-controlled mode; thus, patients can adjust stimulation parameters by themselves or following the instruction of doctors on the terminal device. The ranges for stimulation parameters are as follows: 0–30 mA intensity; 1–200 Hz frequency; and 100–1000 µs pulse width. The adhesive electrodes are removable and replaceable, and the surface is made of conductive silicone for comfortable use. The program control software in the mobile terminal connects with the stimulator by Bluetooth. Also, it is possible to export the treatment history in different formats: trend, bar, and pie charts, thus providing a more visual reference for the follow-up with a doctor.
Surgical procedure
Animals were housed under standard conditions. All experimental protocols were approved by the Institutional Animal Care and Use Committee of Capital Medical University (AEEI-2021–217). Experiments were performed in 9 male cats (2.5–3.5 kg, 6–12 months old, domestic shorthairs) under α-chloralose anesthesia (initial 65 mg/kg intravenously that were supplemented with 15–25 mg/kg as needed) after induction with isoflurane (2–5% in oxygen) by tracheal cannula connected to an anesthesia machine (Matrx VMR; Midmark, Dayton, OH, USA). Heart rate, blood oxygen level, and systemic blood pressure were monitored throughout the experiment. Fluid was administered via the cephalic vein. The body temperature was maintained at 37 ℃ with a heating pad.
Through an abdominal incision, the ureters were isolated, tied, cut, and externally drained. The bladder was inserted via a double lumen catheter through the urethra, after which the catheter was secured by making a small V-shaped opening on the proximal urethra and fixed with 4–0 silk sutures (Fig. 2D). One lumen of the catheter was used to infuse the bladder with 0.9% NS at a rate of 1–2 mL/min after connecting to a pump. The other lumen was connected to a pressure transducer (MP150; BIOPAC Systems, Inc., Camino Goleta, CA, USA) to measure the bladder pressure.
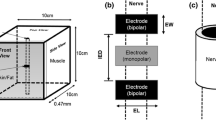
A ITNS: a bipolar nerve cuff with stranded stainless-steel wire was used, and rubber elastomer tubing was placed around the nerve and connected to a pulse generator. B TTNS: two self-adhesive electrodes that were respectively placed at about 3–4 cm above the medial malleolus are used. C The real ITNS device. D A double lumen catheter. E The real TTNS device
After shaving the bilateral hind limb, hair removal ointment was used for the left leg to make two self-adhesive electrodes (General Stim Inc., Hangzhou, Zhejiang, China) that were placed at about 3–4 cm above the medial malleolus of the left leg and behind the medial tibial edge (Fig. 2B, E). Two snap structures served as the joints between the pulse transmitter and the self-adhesive electrodes (Fig. 1). A 2- to 3-cm incision was made on the medial side of the contralateral hind limb above the ankle to expose the tibial nerve. Then, two custom-fabricated bipolar nerve cuff electrodes (platinum contacts) were implanted on the tibial nerve, and electrical pulses were given out by an external stimulus generator (Master-8; AMPI, Jerusalem, Israel) (Fig. 2A and C). During the procedure, the stimulator was activated to confirm function and placement. Toe movement was observed when the stimulator was properly positioned. At the end of the surgery, all the incisions were closed and sutured.
Stimulation protocol
A series of acute experiments were performed approximately 60 min after surgery. Both stimulation parameters were delivered through the nerve cuff electrode or self-adhesive electrodes with uniphasic, rectangular pulses (0.2 ms pulse width, 15 Hz frequency). By gradually increasing the stimulation intensity, the intensity threshold (T) inducing toe movement was determined. After the appearance of the first large amplitude (> 30 cmH2O) and long duration (> 20 s) bladder contraction, the bladder infusion was stopped. Bladder capacity (BC) was defined as the infusion volume into the bladder. After emptying the bladder, multiple cystometrograms (CMGs) were performed without stimulation to obtain the control BC. After the BC was stabilized, stimulation was given to observe the effects on bladder reflex. TTNS and ITNS with respective 2 times T (2 T), 4 times T (4 T), 6 times T (6 T), and 24 mA were used to stimulate the tibial nerve during a series of CMGs. Finally, another control CMG was performed to decide whether there were any post-stimulation effects. The bladder was emptied after each CMG, and a 10 min rest period was permitted between successive CMGs to allow the distended bladder to recover [9]. All the simulations were performed in the same order, i.e., TTNS followed by ITNS. ITNS stays off during TTNS, and TTNS stays off during ITNS, respectively.
Data analysis
Repeated measurements of urodynamic parameters during the control CMGs before any treatment were averaged in the same animal. Then, the urodynamic parameters (bladder capacity, maximal amplitude, duration of micturition contraction, and T) were measured in every CMG and normalized to their averaged control values in each cat.
The normalized BC was presented as a percentage (measured BC/first control BC). The data from different animals are presented as means ± SE. Statistical significance (p < 0.05) was determined by repeated-measures ANOVA followed by Bonferroni multiple comparisons. Statistical analyses were performed using GraphPad Prism software (version 9.1.1, GraphPad Software, La Jolla, CA, USA).
Results
During the NS infusion, TTNS at 4 T (12.98 ± 2.91 ml, 168.2 ± 15.22%), 6 T (14.28 ± 3.09 ml, 186.7 ± 15.94%) and the maximum output current intension 24 mA (15.74 ± 3.50 ml, 205.6% ± 18.47%) significantly increased the bladder capacity (BC) (n = 9) compared to the control level (8.70 ± 2.46 ml) (all p < 0.05); however, there was no statistical significance among the three intensities. TTNS at 2 T did not significantly increase the BC (11.04 ± 2.67 ml, 141.2 ± 12.36%) with baseline level (p > 0.05). At the same time, ITNS at 2 T (13.12 ± 2.83 ml, 171.1 ± 15.12%), 4 T (14.81 ± 3.05 ml, 196.5 ± 19.1%), 6 T (15.62 ± 3.28 ml, 208.7 ± 21.19%) and the current intension 24 mA (17.64 ± 4.10 ml, 229.3 ± 22.29%) significantly increased the BC compared to the control level (all p < 0.05). Likewise, no significant difference was observed among the four intensities (p > 0.05). Finally, the BC could return to the NS control level (Figs. 3 and 4B). The T values of TTNS were higher than those of ITNS (p = 0.02) (Fig. 4A). The inhibitory effects of TTNS and ITNS showed no significant difference at their respective 2 T, 4 T, 6 T, and 24 mA. Neither TTNS nor ITNS significantly changed the contraction duration and amplitude (p > 0.05, respectively) (Fig. 5). The separate effects on bladder function after using TTNS and ITNS are shown in Fig. 6.
A The T value of TTNS was significantly higher than ITNS. B TTNS at 4 T, 6 T, and 24 m A could significantly increase the BC. Meanwhile, ITNS at 2 T, 4 T, 6 T, and 24 mA could increase the BC compared with the baseline level. TTNS at 2 T had no significant effect on BC. BC could return to the NS control level at last. There was no statistical significance comparing the efficacy of TTNS with ITNS at the same intension of 2 T, 4 T, 6 T, and 24 mA
Discussion
TNS is a viable option for OAB patients who are refractory to conservative therapies [5]. The effectiveness of TNS in OAB has been confirmed in both preclinical studies and clinical trials [10,11,12,13,14,15]. Even an animal study revealed that it could increase the bladder capacity, resulting in a large amount of residual volume in the bladder after using 30 min TNS [16]. During PTNS, the tip of a needle electrode is inserted into the medial malleolus, which may bring a series of complications, such as bleeding, infection, and pain. ITNS requires a stimulator to be implanted into the tibial nerve, which induces similar side effects as PTNS. In addition, both PTNS and ITNS need to be performed by professional medical workers. To overcome this limitation, TTNS was invented as an alternative, non-invasive treatment that only uses surface electrodes and allows patients to use the stimulator at any place they like [17]. Currently, there are no specific TTNS devices that have been approved for OAB. The GEKO [18], which some researchers have used to treat OAB, was approved to prevent deep vein thrombosis. The novel wearable device (General Stim Inc., Hangzhou, Zhejiang, China) is esthetic and without trauma associated with the use of adhesive electrodes. OAB patients can use the stimulator at home and modulate the stimulation parameters following the doctors’ instruction to avoid frequent hospital visits, especially during the COVID-19 pandemic.
The effectiveness of TTNS compared to PTNS has been investigated by some researchers. A 12 week RCT [8] evaluated the effectiveness of the TTNS compared to the PTNS, where both TNS were performed once a week for 30 min. The results demonstrated non-inferiority in decreasing the daytime frequency and no statistical significance in the other voiding diary parameters. Currently, studies comparing TTNS with ITNS are rare. Consequently, we conducted this study, finding that both TTNS and ITNS could increase the BC, but the T values of TTNS were higher than those of ITNS. Also, the effectiveness of TTNS showed no statistical significance compared with ITNS. That results indicated that TTNS could activate the tibial nerve effectively though it needs more energy comparing with ITNS. Previous study in cats discovered that TNS at stimulating the tibial nerve at Aδ- and C-fibers intensities was effective in suppressing spontaneous bladder contractions [19]. As small-diameter fibers, the recruitment of Aδ- and C-fibers needed less stimulation energy than large myelinated Aβ fibers in the afferent tibial nerve and TTNS could offer the energy enough. That may also be the mechanism to explain the similar effects of TTNS and ITNS on bladder function.
Previous studies suggested that the stimulating frequency was a critical parameter that mediates the modulatory effect on bladder activity. A previous study [11] suggested that low-frequency (2 Hz) and high-frequency (5–20 Hz) TNS can cause excitatory and inhibitory bladder reactions. Our results were consistent with those previous studies, confirming that 15 Hz TNS had an inhibitory effect on bladder contraction. The T value of TTNS and ITNS was significantly different (p = 0.02), which may be because the ITNS directly connects the nerve while the energy of the TTNS may be reduced by the skin, muscle, and soft tissue. Another study [16] in cats showed that prolonged 5 Hz TNS reduced the contraction amplitude of control without significantly changing the contraction duration. In the present study, the contraction amplitude and duration were not significantly inhibited. This may be related to the stimulation time, where in the present study, it was acute stimulation compared to prolonged stimulation in the previous study.
This study has some limitations. First, bladder reflex contractions in the current study were evoked by NS infusion, which primarily activated the Aδ fibers under physiological conditions. Yet, bladder irritation by acetic acid infusion activates C fibers under pathological conditions [20]. Although similar results were observed in the studies involving cats infused with saline and acetic acid [21], additional studies are needed to confirm the effectiveness of TTNS compared to ITNS in OAB cats. Second, our experiment only used the parameter of 15 Hz frequency and 200 µs pulse width; thus, more parameters should be tested by future studies. Finally, the stimulation in this study was acute, so prolonged stimulation and the safety of the stimulator should be explored in future studies.
Conclusion
The novel TTNS device was effective in increasing BC. Also, the non-invasive neuromodulation technique could achieve a similar effect with ITNS.
Data availability
All data included in this study are available upon request by contact with the corresponding author.
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J et al (2010) An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21(1):5–26
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al (2002) The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the international continence society. Neurourol Urodyn 21(2):167–178
van Kerrebroeck PE, van Voskuilen AC, Heesakkers JP, Lycklama a Nijholt AA, Siegel S, Jonas U et al (2007) Results of sacral neuromodulation therapy for urinary voiding dysfunction: outcomes of a prospective, worldwide clinical study. J Urol 178(5):2029–2034
Rapp DE, Lucioni A, Katz EE, O’Connor RC, Gerber GS, Bales GT (2004) Use of botulinum-A toxin for the treatment of refractory overactive bladder symptoms: an initial experience. Urology 63(6):1071–1075
Schneider MP, Gross T, Bachmann LM, Blok BF, Castro-Diaz D, Del Popolo G et al (2015) Tibial nerve stimulation for treating neurogenic lower urinary tract dysfunction: a systematic review. Eur Urol 68(5):859–867
Te Dorsthorst M, van Balken M, Heesakkers J (2020) Tibial nerve stimulation in the treatment of overactive bladder syndrome: technical features of latest applications. Curr Opin Urol 30(4):513–518
Martin-Garcia M, Crampton J (2019) A single-blind, randomized controlled trial to evaluate the effectiveness of transcutaneous tibial nerve stimulation (TTNS) in Overactive Bladder symptoms in women responders to percutaneous tibial nerve stimulation (PTNS). Physiotherapy 105(4):469–475
Ramirez-Garcia I, Blanco-Ratto L, Kauffmann S, Carralero-Martinez A, Sanchez E (2019) Efficacy of transcutaneous stimulation of the posterior tibial nerve compared to percutaneous stimulation in idiopathic overactive bladder syndrome: Randomized control trial. Neurourol Urodyn 38(1):261–268
Shapiro K, Pace N, Morgan T, Cai H, Shen B, Wang J et al (2020) Additive inhibition of reflex bladder activity induced by bilateral pudendal neuromodulation in cats. Front Neurosci 14:80
Ammi M, Chautard D, Brassart E, Culty T, Azzouzi AR, Bigot P (2014) Transcutaneous posterior tibial nerve stimulation: evaluation of a therapeutic option in the management of anticholinergic refractory overactive bladder. Int Urogynecol J 25(8):1065–1069
Moazzam Z, Duke AR, Yoo PB (2016) Inhibition and excitation of bladder function by tibial nerve stimulation using a wirelessly powered implant: an acute study in anesthetized cats. J Urol 196(3):926–933
van Breda HMK, Martens FMJ, Tromp J, Heesakkers J (2017) A new implanted posterior tibial nerve stimulator for the treatment of overactive bladder syndrome: 3-month results of a novel therapy at a single center. J Urol 198(1):205–210
Theisen K, Browning J, Li X, Li S, Shen B, Wang J et al (2018) Frequency dependent tibial neuromodulation of bladder underactivity and overactivity in cats. Neuromodulation 21(7):700–706
Andersen K, Kobbero H, Pedersen TB, Poulsen MH (2021) Percutaneous tibial nerve stimulation for idiopathic and neurogenic overactive bladder dysfunction: a four-year follow-up single-centre experience. Scand J Urol 55(2):169–176
Araujo TG, Schmidt AP, Sanches PRS, Silva Junior DP, Rieder CRM, Ramos JGL (2021) Transcutaneous tibial nerve home stimulation for overactive bladder in women with Parkinson’s disease: a randomized clinical trial. Neurourol Urodyn 40(1):538–548
Li S, Browning J, Theisen K, Yecies T, Shen B, Wang J et al (2020) Prolonged nonobstructive urinary retention induced by tibial nerve stimulation in cats. Am J Physiol Regul Integr Comp Physiol 318(2):R428–R434
MS Alomari, AS Abdulhamid, AA Ghaddaf, KM Alshareef, AK Haneef, MS AlQuhaibi, RA Banjar (2022) Non-inferior and more feasible transcutaneous tibial nerve stimulation in treating overactive bladder: A systematic review and meta-analysis. Int J Urol 29(10):1170–1180
Tucker A, Maass A, Bain D, Chen LH, Azzam M, Dawson H et al (2010) Augmentation of venous, arterial and microvascular blood supply in the leg by isometric neuromuscular stimulation via the peroneal nerve. Int J Angiol 19(1):e31–e37
Sato A, Sato Y, Schmidt RF (1980) Reflex bladder activity induced by electrical stimulation of hind limb somatic afferents in the cat. J Auton Nerv Syst 1(3):229–241
Kovacevic M, Yoo PB (2015) Reflex neuromodulation of bladder function elicited by posterior tibial nerve stimulation in anesthetized rats. Am J Physiol Renal Physiol 308(4):F320–F329
Wang Z, Liao L, Deng H, Li X, Chen G, Liao X (2018) The different roles of opioid receptors in the inhibitory effects induced by sacral dorsal root ganglion stimulation on nociceptive and nonnociceptive conditions in cats. Neurourol Urodyn 37(8):2462–2469
Funding
Research Projects of China Rehabilitation Research Centre, (2021zx-11), Xing Li, Ministry of Science and Technology of the People’s Republic of China, 2018YFC2002203, Limin Liao, Natural Science Foundation of Beijing Municipality, no. 7182188, Xing Li.
Author information
Authors and Affiliations
Contributions
LM.L and X.L designed the experiment; XH.L and X.L performed the experiment. H.Z, and ZH.Z helped to perform the experiment. XH.L wrote the manuscript. LM.L and X.L participated in critical revisions of important knowledge content. All authors have finally approved the version to be released and agree to be responsible for all aspects of the work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declared no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, X., Zhou, Z., Zhao, H. et al. Efficacy of a novel wearable transcutaneous tibial nerve stimulation device on bladder reflex compared to implantable tibial nerve stimulation in cats. Int Urol Nephrol 55, 853–859 (2023). https://doi.org/10.1007/s11255-022-03450-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03450-8