Abstract
Background
Previous studies have proved that irisin is related to the development of chronic kidney disease. In this study, we aimed to compare serum irisin level in patients treated with peritoneal dialysis (PD) and hemodialysis (HD).
Methods
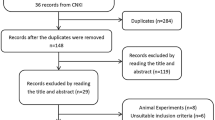
Two hundred and fifty-two dialysis patients (146 PD patients and 106 HD patients) were included in the study. Levels of serum irisin and other parameters were compared between the two groups’ patients.
Results
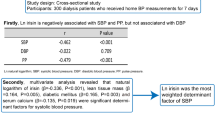
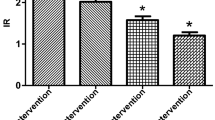
There were higher serum irisin levels in PD patients than those in HD patients [113.10 (106.15 ~ 119.15) ng/ml vs. 45.72(21.67 ~ 79.71) ng/ml, P < 0.001]. Moreover, body fat mass, percent body fat, serum calcium, high-density lipoprotein, low-density lipoprotein, carbon dioxide combining power (CO2CP) and residual renal function were higher in patients on PD than that in those on HD, whereas levels of lean body mass, systolic blood pressure, albumin, serum uric acid, potassium, and phosphorus(It should be “were" replace are) are higher in HD patients in comparison to PD patients. Dialysis modality (PD/HD), serum CO2CP level, lean body mass, and percent body fat independently positively correlated with natural logarithm of irisin (lnirisin) by multivariate linear regression analysis.
Conclusions
In this study, we prove that serum irisin level is significantly higher in patients treated with peritoneal dialysis than that with hemodialysis. As well as, increasing skeletal muscle mass and fat body percent, and correcting metabolic acidosis may increase serum irisin levels.
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
References
Hoppe K, Schwermer K, Kawka A, Klysz P, Baum E, Kaluzna M, Sikorska D, Scigacz A, Lindholm B, Pawlaczyk K, Oko A (2018) Dialysis vintage stratified comparison of body composition, hydration and nutritional state in peritoneal dialysis and hemodialysis patients. Arch Med Sci 14(4):807–817. https://doi.org/10.5114/aoms.2016.61902
Vanholder R, Van Laecke S, Glorieux G (2008) The middle-molecule hypothesis 30 years after: lost and rediscovered in the universe of uremic toxicity? J Nephrol 21(2):146–160
Gan W, Chen W, Li T, Shao D, Xu F, Huo S, Li C, Yang Z, Zeng X (2022) Circulating irisin level in chronic kidney disease patients: a systematic review and meta-analysis. Int Urol Nephrol 54(6):1295–1302. https://doi.org/10.1007/s11255-021-03000-8
Gouveia MC, Vella JP, Cafeo FR, Affonso Fonseca FL, Bacci MR (2016) Association between irisin and major chronic diseases: a review. Eur Rev Med Pharmacol Sci 20(19):4072–4077
Roca-Rivada A, Castelao C, Senin LL, Landrove MO, Baltar J, Belén Crujeiras A, Seoane LM, Casanueva FF, Pardo M (2013) FNDC5/irisin is not only a myokine but also an adipokine. PLoS ONE 8(4):e60563. https://doi.org/10.1371/journal.pone.0060563
Yazdanimoghaddam F, Aghaei M, Ghasemi M, Soltani N, Rezazadeh H, Zadhoush F (2022) Beneficial effects of MgSO4 on TFAM, UPC3 and FNDC5 mRNA expressions in skeletal muscle of type 2 diabetic rats: a possible mechanism to improve insulin resistance. Mol Biol Rep 49(4):2795–2803. https://doi.org/10.1007/s11033-021-07091-5
Luo Y, Qiao X, Xu L, Huang G (2022) Irisin: circulating levels in serum and its relation to gonadal axis. Endocrine 75(3):663–671. https://doi.org/10.1007/s12020-022-02981-5
Li Q, Zhang M, Zhao Y, Dong M (2021) Irisin protects against LPS-stressed cardiac damage through inhibiting inflammation, apoptosis, and pyroptosis. Shock 56(6):1009–1018. https://doi.org/10.1097/SHK.0000000000001775
Fu J, Li F, Tang Y, Cai L, Zeng C, Yang Y, Yang J (2021) The emerging role of irisin in cardiovascular diseases. J Am Heart Assoc 10(20):e022453. https://doi.org/10.1161/JAHA.121.022453
Rodríguez-Carmona A, Pérez Fontán M, Sangiao Alvarellos S, García Falcón T, Pena Bello ML, López Muñiz A, Cordido F (2016) Serum levels of the adipomyokine irisin in patients with chronic kidney disease. Nefrologia 36(5):496–502. https://doi.org/10.1016/j.nefro.2016.05.019
Huang BT, Peng Y, Liu W, Zhang C, Huang FY, Wang PJ, Zuo ZL, Liao YB, Chai H, Huang KS, Huang DJ, Chen M (2015) Lean mass index, body fat and survival in Chinese patients with coronary artery disease. QJM 108(8):641–647. https://doi.org/10.1093/qjmed/hcv013
Obi Y, Qader H, Kovesdy CP, Kalantar-Zadeh K (2015) Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr Opin Clin Nutr Metab Care 18(3):254–262. https://doi.org/10.1097/MCO.0000000000000171
Cleland C, Ferguson S, Ellis G, Hunter RF (2018) Validity of the International Physical Activity Questionnaire (IPAQ) for assessing moderate-to-vigorous physical activity and sedentary behaviour of older adults in the United Kingdom. BMC Med Res Methodol 18(1):176. https://doi.org/10.1186/s12874-018-0642-3
Moreno-Navarrete JM, Ortega F, Serrano M, Guerra E, Pardo G, Tinahones F, Ricart W, Fernández-Real JM (2013) Irisin is expressed and produced by human muscle and adipose tissue in association with obesity and insulin resistance. J Clin Endocrinol Metab 98(4):E769–E778. https://doi.org/10.1210/jc.2012-2749
Yilmaz H, Cakmak M, Darcin T, Inan O, Sahiner E, Demir C, Aktas A, Bilgic MA, Akcay A (2016) Circulating irisin levels reflect visceral adiposity in non-diabetic patients undergoing hemodialysis. Ren Fail 38(6):914–919. https://doi.org/10.3109/0886022X.2016.1172918
Hefzollah F, Boushehri SN, Mahmudpour M (2020) Effect of high bicarbonate hemodialysis solution on biochemical parameters and anthropometric indices. Hemodial Int 24(3):317–322. https://doi.org/10.1111/hdi.12842
Wang XH, Mitch WE, Price SR (2022) Pathophysiological mechanisms leading to muscle loss in chronic kidney disease. Nat Rev Nephrol 18(3):138–152. https://doi.org/10.1038/s41581-021-00498-0
Wen MS, Wang CY, Lin SL, Hung KC (2013) Decrease in irisin in patients with chronic kidney disease. PLoS ONE 8(5):e64025. https://doi.org/10.1371/journal.pone.0064025
Cheng BC, Lai YR, Huang CC, Lu CH (2020) Improved cardiovascular autonomic function and decreased protein-bound uremic toxins in patients with end-stage renal disease after peritoneal dialysis. J Int Med Res 48(7):300060520933797. https://doi.org/10.1177/0300060520933797
Sirich TL, Meyer TW (2018) Intensive hemodialysis fails to reduce plasma levels of uremic solutes. Clin J Am Soc Nephrol 13(3):361–362. https://doi.org/10.2215/CJN.00950118
Lee MJ, Lee SA, Nam BY, Park S, Lee SH, Ryu HJ, Kwon YE, Kim YL, Park KS, Oh HJ, Park JT, Han SH, Ryu DR, Kang SW, Yoo TH (2015) Irisin, a novel myokine is an independent predictor for sarcopenia and carotid atherosclerosis in dialysis patients. Atherosclerosis 242(2):476–482. https://doi.org/10.1016/j.atherosclerosis.2015.08.002
Xu F, Yang Y, Wu M, Zhou WH, Wang DX (2022) Cui WPPatients with end-stage renal disease and diabetes had similar survival rates whether they received hemodialysis or peritoneal dialysis. Ther Apher Dial. https://doi.org/10.1111/1744-9987.13890
Mathew MT, Fishbane S, Obi Y, Kalantar-Zadeh K (2016) Preservation of residual kidney function in hemodialysis patients: reviving an old concept for contemporary practice. Kidney Int 90(2):262–271. https://doi.org/10.1016/j.kint.2016.02.037
Acknowledgements
This study was supported by Beijing Municipal Education commission & Beijing Natural Science Foundation (KZ202110025038), and Xuanwu Hospital Huizhi talent leader training program to Aihua Zhang.
Author information
Authors and Affiliations
Contributions
AHZ and XYS: designed the study. XYS and SJZ: collected the data. XYS: drafted the manuscript. JLZ, TZ and SYW: analyzed the data. QP and YJP: assisted in the literature search. AHZ: revised and supervised all the works. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that they have no competing interests.
Ethical approval
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the Human Clinical Study Committee of Xuanwu Hospital.
Informed consent
Informed consent was obtained from all the individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, XY., Zhou, SJ., Zhang, JL. et al. Serum irisin level is higher in peritoneal dialysis than in hemodialysis. Int Urol Nephrol 55, 1329–1334 (2023). https://doi.org/10.1007/s11255-022-03440-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03440-w