Abstract
Objectives
To investigate factors associated with low-compliance bladders (LCB) in pretransplant patients with end-stage renal disease (ESRD) and develop a clinical prediction model for urodynamic studies.
Methods
This study was a prospective cohort study. Patients with ESRD on the renal transplantation waiting list were recruited and underwent the urodynamic study. Demographics data, predictor factors related to the bladder compliance such as underlying disease of the lower urinary tract disease (LUTD), duration of urine < 250 mL/day, type and duration of renal replacement therapy (RRT), urine volume per day and urodynamic study information were collected. Univariable and multivariable logistic regression models were used to assess the independence of explanatory factors, then we developed the clinical prediction model.
Results
One hundred fifty-two patients participated in the study: 94 patients in the normal bladder group and 58 patients in LCB group. Demographic data were not significantly different between the two groups, except diabetes. Cystometric capacity, detrusor pressure, compliance were significantly different. From the univariate analysis, DM status, duration of RRT, and passing < 100 mL of urine per day were related to LCB. We named the prediction model, the DUDi score based on the predictors (Duration of RRT, Urine volume/day, Diabetes). Higher scores predicted a higher risk of low-compliance bladder [P value = 0.464 according to the Hosmer–Lemeshow test, and the AUC was 0.87 (95% CI 0.81–0.92)].
Conclusions
Our clinical prediction model is easy to use and provides a high predictive value that is appropriate for patients who have no known LUTD to identify low-compliance bladder.
Trial registration number and date of registration for prospectively registered trials
This study was approved by the Thai Clinical Trials Registry Committee on 09 February 2021. The TCTR identification number is TCTR20210209006.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The bladder is one of the most important organs and has a critical role in the success of renal transplantation. A good bladder reservoir is essential to prevent transplant related complications and failure of the transplantation. It has recently become routine to perform at least a Voiding Cystourethrography (VCUG) and/or cystoscopy as part of the pre-renal transplantation evaluation to ensure the bladder has a good functional reservoir and can empty properly.
Patients with chronic oliguria may develop bladder dysfunction, characterized by low volume capacity and low compliance [1] and most patients with low capacity bladders have low-compliance bladders (LCB). Moreover, some patients may have other functional bladder abnormalities, like a neurogenic bladder, or dysfunctional voiding that cannot be diagnosed by VCUG or cystoscopy. These abnormalities may result in renal damage and if a renal transplantation were performed in these patients, complications would occur that might lead to allograft damage.
Although several studies report that bladder capacity and storage pressure may improve within 24 weeks of renal transplantation [1, 2], high storage pressure may still cause complications while waiting for bladder function to improve, such as urinary reflux into the allograft, urinary tract infection, or anastomosis leakage. Moreover, some patients with LCB or very low capacity bladder may not improve post-transplant and might require augmentation or diversion before or after transplantation [2, 3]. Several studies support pretransplant bladder evaluation and pretransplant correction of LCB, especially in patients whose bladder dysfunction results from urological etiologies [4,5,6]. Moreover, a study report that LCB in kidney transplant patients leads to decrease graft survival and increase risk of complications such as urinary tract infection [7].
A urodynamic study can identify LCB and lower urinary tract dysfunction, however, there is still no consensus, and there are no guidelines, regarding optimal pretransplant urodynamic evaluation, notably in asymptomatic patients and those who have unknown lower urinary tract diseases (LUTD). Remarkably, some 30–50% of patients with no lower urinary tract symptoms (LUTS) have lower urinary tract (LUT) abnormalities revealed by urodynamic evaluation [8, 9]. These patients should be managed before transplantation.
Given the continuing lack of standard guidelines for LUT evaluation and the need for more data [6, 8, 9], we undertook this study to investigate factors associated with low-compliance bladders in pretransplant patients with end-stage renal disease (ESRD) and to develop a clinical prediction model for urodynamic studies. The prediction model aims to identify high risk of LCB and lower urinary tract dysfunction in patients with ESRD prior to transplantation. These patients would benefit from urodynamic evaluation, to identify LCB or lower urinary tract dysfunction, for proper management prior to or after transplantation, which would help increase graft survival and reduce complications from lower urinary tract dysfunction.
Methods
Study design, setting and participants
This study was a prospective cohort study conducted between February 2021 and March 2022 at Thammasat University Hospital (TUH), Pathum Thani, Thailand. We recruited patients with ESRD on the renal transplantation waiting list who were attending the TUH Nephrology and Urology clinic if they were aged more than 18 years old and gave consent to undergo the urodynamic study. We excluded patients who were physically unable to undergo a urodynamic study, for example; patient who could not insert the urethral catheter, patients who refused to perform urodynamic study.
Variables and data measurement
Data were collected on a standardised case record form, including demographics, age, sex, body mass index (BMI), underlying diseases, cause of their renal failure, history of surgery, trauma, previous urological disease, bowel history, medications (beta-blockers, calcium channel blockers), and menstruation. Constipation was defined using the ROME IV criteria and the Bristol stool criteria. Women with normal menstrual periods were defined as normal hormonal status, while those with abnormal or absent menstrual periods were defined as abnormal hormonal status.
To analyze factors related to bladder compliance, we collected data on underlying disease of the LUTD: neurogenic bladder, posterior urethral valve, tuberculosis, benign prostatic hypertrophy (BPH), dysfunctional voiding, overactive bladder, urethral stricture, vesicoureteral reflux, chronic cystitis, interstitial cystitis, duration of very low (< 250 mL/day) urine output, type and duration of renal replacement therapy (RRT), and urine volume per day [1, 10, 11]. We used a three-day bladder diary to measure the functional capacity and the volume of urine output/day.
The data collected from the VUDS were cystometric capacity, bladder compliance, vesicoureteral reflux, maximal flow rate, maximal detrusor pressure at the maximal flow rate, and post-void residual urine.
Urodynamic evaluation
All VUDS procedures were performed, according to good urodynamic practice (International Continence Society guidelines). All patients underwent a rectal enema the night before the study. We used a computerized urodynamic study machine (MMS, solar intelligent) and water-filled catheters with external transducers at the reference level of the upper edge of the symphysis pubis concomitantly with fluoroscopy. Intravesical pressure was measured using a 6Fr, side-holed, water-filled transurethral, double-lumen catheter. The bladders were filled with normal saline mixed with contrast media at a ratio of 1:4 at a rate of 12 mL/min. Zero pressure corresponded to the surrounding atmospheric pressure. Patients were examined in the sitting position for women and standing position for men. All patients were prescribed antibiotic to prevent urinary tract infection after performing urodynamics.
The cystometric capacity was defined as the volume that patient’s desired to void [12]. Bladder compliance was calculated from the detrusor pressure and volume of the two standard points of the tracing, that is, at the start of bladder filling with volume zero and at cystometric capacity without detrusor contraction [13]. The maximum flow rate (Qmax) was recorded while voiding and the maximal detrusor pressure at the maximum flow (PdetQmax) rate was also noted. Low-compliance bladder (LCB) was defined as a < 12.5 mL/cm H2O [14].
Sample size calculation
To analyze the factors associated with the LCB using multivariable logistic regression model, this study needs 10 samples per variable [15]. Based on previous research, there were five interesting factors that could affect the compliance of the bladder; underlying diseases that can affect lower urinary tract function, constipation, medications (beta-blockers, calcium channel blockers), duration of renal replacement therapy, and urine volume/day. Also, the prevalence of low-compliance bladder in patients with ESRD is about 30–50% [8, 9]. Therefore, we calculated that we would need a total of at least 125 samples with 50 index cases to analyze in this cohort study.
Data analysis and development of a prediction model
We classified patients into two groups, those with a normal bladder and those with LCB, and compared the data between the two groups. We used the student’s t test for normally distributed continuous data [expressed as mean and standard deviation, (SD)] and the Wilcoxon Rank Sum test for skewed data [expressed as median and interquartile range (IQR)]. We used the Fisher’s exact test for categorical data. Univariable and multivariable logistic regression models were used to assess the independence of explanatory factors by backward elimination. The selection criterion of p < 0.2 was used for the elimination of a variable in univariable analysis that was not statistically significant. Some variables were initially excluded from the multivariable model to avoid multicollinearity. Then the β coefficients of each predictor factor was calculated. Finally, to determine the score of each factor, its β coefficient was divided by the lowest β coefficient. As a result, we were able to develop an integer score-based prediction model. Data were analyzed using STATA version 15.0 (Stata Corp., College Station, TX, USA). The statistical significance of the Hosmer–Lemeshow test was set at p > 0.05. We assessed the diagnostic ability of a derived score, the DUDi score (see below) for predicting the presence of an LCB.
Result
Patients’ characteristic
A total of 152 patients participated in the study: 94 patients in the normal bladder group and 58 patients in LCB group. Age, sex, BMI, underlying diseases, cause of ESRD, constipation and hormonal status in women were not significantly different between the two groups and their mean ages were 42 years (Table 1). Only DM was significantly more common in the normal bladder group. It is interesting to note that there were only 3 patients in each group who had a history of LUTD and none of the patients in this study reported LUTS. The use of beta-blockers and calcium channel blockers were similar between the two groups as were the types of RRT but RRT duration was significantly longer in the LCB group. Urine volume/day, duration of passing < 250 mL/d and maximal functional capacity were significantly different.
The video urodynamic result of normal bladder and bladder dysfunction groups
In the filling phase, six variables were highly significantly different between the two groups: cystometric capacity, volume at first desire to void, volume at strong desire to void, detrusor pressure, compliance and bladder shape as shown in Table 2. There were no significant variables in the void phase but there were trends for detrusor pressure and post-void urine volume.
Development of the clinical prediction model
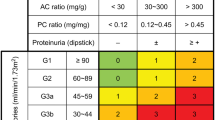
We examined a number of factors for bladder compliance in the univariate analysis and found only three significant factors, DM status, duration of RRT, and passing < 100 mL of urine per day (Table 3). When assessed in the multivariable model, there was collinearity between the duration of having a urine output < 250 mL/day and the duration of RRT; therefore, we opted to use the duration of RRT because this is an objective measure. Previous studies, and also statistical analysis of this study, demonstrated that duration of RRT longer than 24 months and 48 months was significantly associated with decreased detrusor compliance and capacity; therefore, we used cut off durations of RRT at less than 24 months, 24–48 months and more than 48 months for analysis in this study [2, 8, 9]. Long-term dialysis patients will develop decreased urine output over time and nephrologists define low urine output at < 100 mL/day. Therefore, we also chose this cut off [16]. DM status, RRT duration and passing < 100 mL/day of urine were the only three independent variables in the multivariable analysis.
Tables 4 and 5 show the developed clinical prediction model called the DUDi score: Duration of RRT, Urine volume per day, and Diabetes. The lowest score was 0 and the highest score was 7 points. Higher scores predicted a higher risk of low-compliance bladder.
Model performance
The statistical significance of the DUDi score was p = 0.464 according to the Hosmer–Lemeshow test, and the AUC was 0.87 (95% CI 0.81–0.92) (Fig. 1). The relationship between the DUDi score and the predicted probability of bladder dysfunction is shown in Tables 4 and 5 and Figs. 1 and 2.
A score ≥ 6 is associated significantly with LCB (LHR 4.25 [2.65–6.83], p < 0.001) and a score ≤ 3 has a low probability of bladder dysfunction (LHR 0.15, [0.07–0.32], p < 0.001). When translating into absolute risks, the DUDi score predicts an increase risk with increasing score and this has a curvilinear relationship (Fig. 2).
Internal validation of the clinical prediction model
To internally validate our clinical prediction model, we retrospectively categorized risk of low-compliance bladder in patients with ESRD who underwent renal transplantation using the DUDi score, and we reviewed the urological complications which occurred within the first year following transplantation. There were 67 patients with ESRD who underwent renal transplantation between January 2014 and December 2021. Of these, 31 patients were classified as low probability of low-compliance bladder, 9 patients as moderate probability, and 27 patients as high probability. In the high probability group, nine patients had recurrent urinary tract infection, six patients developed allograft hydronephrosis, which urodynamic study revealed to be associated with low-compliance bladder, one patient had overactive bladder, and three patients had dysfunctional voiding. These patients were treated by antimuscarinic. One patient was treated by intravesical Botox injection due to failed antimuscarinic, and biofeedback was used in the dysfunctional voiding patients. Two patients in the moderate group had urinary tract infection and allograft hydronephrosis; they were treated by antimuscarinic. None of patients in low probability group developed urinary tract complications (Table 6).
Discussion
Patients with ESRD may have a dysfunctional bladder characterized by a reduced capacity, LCB and detrusor overactivity [8, 17, 18]. Anuria and oliguria in patients with ESRD can lead to a dysfunctional bladder because of long-term disuse [19], which, in turn, may result in bladder fibrosis, and reduced bladder compliance and capacity [20]. In addition, a low urine output may conceal the symptoms of bladder dysfunction. Patients with LUTD like neurogenic bladder and posterior urethral valves, or those with LUTS, should be investigated. By contrast, a decision to conduct a urodynamic study in asymptomatic patients is more challenging.
Even though many patients with a dysfunctional bladder that is neurologically intact show spontaneous resolution in bladder function 6–12 months post-transplantation [3, 5], they are still at an increased risk of developing complicated urinary tract infections and other complications like high pressure of vesicoureteral reflux to allograft during the period of LCB. Therefore, it would be better to identify LCB patients before transplantation to plan for proper post-transplant management. Bladder cycling has been suggested as a treatment option prior to transplantation for a small, dysfunctional bladder [1], but others suggest that this procedure is not necessary [21]. One advantage of bladder recycling is that it can predict which defunctionalized bladders would improve after resuming normal cycling [22]. It is safer to transplant into a normal bladder, but if the bladder is abnormal, the risk of a poor outcome can be minimised by conducting appropriate pretransplant investigations and planning optimal management [7].
From our study, we developed a new clinical prediction model, called the DUDi score. This prediction model is based on the sum score of the 3 clinical predictors that clinicians can understand and use easily. The DUDi score had an AUC > 0.85, which is classified as high accuracy [23, 24], and so should be a good tool for identifying patients who require a pretransplant urodynamic study.
The DUDi score also has good discriminating power to predict the probability of LCB in patients with ESRD. A score ≤ 3 points predicts a low (10%) probability of LCB and we would not recommend a urodynamic study. If the score is between 4 and 5, the probability is equivocal and decision to perform a urodynamic study should be individualized. If the score is ≥ 6, we recommend performing a urodynamic study because of the high probability of LCB as shown in Fig. 3. Patients who had low-compliance bladder were managed by bladder recycling prior to renal transplantation to estimate the ability to improve compliance of the bladder. Four patients did not improve their compliance after daily self-cycling for 3 months. These patients will be closely monitored after transplantation and reconstruction will be planned for if needed. We cannot perform reconstruction prior transplantation because these patients are waiting for a deceased donor; therefore, we cannot plan the exact time of transplantation. Three patients had prostatic obstruction and were treated by alpha-blocker.
From this study, it was interesting to note that DM patients were more common in patients with bladders of normal compliance. This might be because patients with diabetes, who were poor control hyperglycemia, are at risk of developing diabetic cystopathy over time, characterized by hypocontractility, atonia and overdistension from detrusor muscle underactivity and neuronal impairment [25]. Our study demonstrated that patients with diabetes had a lower number of LCB. These patients have post-renal transplantation complications from LCB may low in these cases. However, these patients may have a risk of developing detrusor underactivity or diabetic cystopathy. Therefore, we recommend urodynamic studies in all patients with known or suspected of diabetic cystopathy and plan for monitoring post-transplant bladder function. For DM patients who are not suspected to have bladder dysfunction, we suggest using the DUDi score for planning further investigations.
The limitation of our study was that it was a single-center study that might not have included the full spectrum of LCB patients; more research should be conducted to validate the DUDi score and include a greater number and spectrum of patients. There were only six patients in our study who had a history of LUTD; therefore, we cannot generalize our DUDi score findings to such patients. Nevertheless, we still recommend performing a complete urinary tract evaluation, including a urodynamic study, in patients with known or suspected LUTD.
We prospectively collected data on post-renal transplant bladder status in only 11 patients (follow-up range from 5 to 8 months), because most of the patients have not yet undergone a renal transplant due to the pandemic of COVID-19. Five patients had high DUDi scores and were managed with bladder re-cycling before transplantation. They did not have urological complication after transplantation. A prospective cohort study documenting the complications related to bladder dysfunction and the improvement of bladder function in a large-scale external validation of post-renal transplantation patients would add further information about the benefits of the DUDi prediction score. Patients with neurogenic bladders whose compliance does not normalize after transplantation may benefit from intravesical botulinum toxin. If not, surgical reconstruction, bladder augmentation or ileal conduit in well-selected patients [26, 27].
Low compliance does not directly impact the decision to be a candidate for renal transplantation, but it impacts the pre and post-transplant monitoring and preparation to increase graft survival and reduce the complications from low-compliance bladder. Based on previous studies and our research, we suggest informing the transplantation team about the importance of evaluating bladder function prior to transplantation. Due to the shortage of kidney donor grafts, transplantation teams need to prepare patients properly. Bladder dysfunction is associated with intra and post-operative urological complications, including anastomosis leakage, post-operative LUTS symptoms, UTI, and might impact graft function. Our study helps the transplant team decide which patients on the waiting list need to be evaluated prior to transplant to decrease the risk of urological complications and prolonged graft function.
Conclusion
This study demonstrated that the factors associated with LCB in patients with ESRD are the duration of the RRT, urine volume per day, and not having DM. We used these factors to develop a clinical prediction score, the DUDi Score, to identify patients for pretransplant urodynamic studies. Our clinical prediction model is easy to use and provides a high predictive value that is appropriate for patients who have no known lower urinary tract diseases. More research is needed to validate the score and to assess its usefulness in post-transplant patients to see if its generalizability can be broadened.
References
Joshua D, Chamberlin MLJ (2016) Urological evaluation of the transplant recipient. AUA Update Ser 2016(35):69–78
Mizerski A, Ostrowska Clark K, Ostrowski M, Ciechanowski K, Kaminski M, Sulikowski J et al (2003) Postoperative adaptation of urinary bladder to variable volume of urine in the initial period following kidney transplantation. Transplant Proc 35(6):2174–2175
Inoue T, Satoh S, Obara T, Saito M, Numakura K, Narita S et al (2016) Cystometric evaluation of recovery in hypocompliant defunctionalized bladder as a result of long-term dialysis after kidney transplantation. Int J Urol 23(8):694–700
Nahas WC, Mazzucchi E, Arap MA, Antonopoulos IM, Neto ED, Ianhez LE et al (2002) Augmentation cystoplasty in renal transplantation: a good and safe option–experience with 25 cases. Urology 60(5):770–774
Power RE, Hickey DP, Little DM (2004) Urological evaluation prior to renal transplantation. Transplant Proc 36(10):2962–2967
Silva DM, Prudente AC, Mazzali M, Borges CF, D’Ancona C (2014) Bladder function evaluation before renal transplantation in nonurologic disease: is it necessary? Urology 83(2):406–410
Salman B, Hassan A, Sultan S, Tophill P, Halawa A (2018) Renal transplant in the abnormal bladder: long-term follow-up. Exp Clin Transplant 16(1):10–15
Turunc T, Micozkadioglu H, Dirim A, Kuzgunbay B, Aygun C, Ozkardes H et al (2010) Evaluation of video-urodynamic studies before renal transplantation in chronic renal failure patients. Int Urol Nephrol 42(4):903–907
Tsunoyama K, Ishida H, Omoto K, Shimizu T, Shirakawa H, Tanabe K (2010) Bladder function of end-stage renal disease patients. Int J Urol 17(9):791–795
Averbeck MA, Madersbacher H (2011) Constipation and LUTS - how do they affect each other? Int Braz J Urol 37(1):16–28
Hall SA, Chiu GR, Kaufman DW, Wittert GA, Link CL, McKinlay JB (2012) Commonly used antihypertensives and lower urinary tract symptoms: results from the Boston Area Community Health (BACH) Survey. BJU Int 109(11):1676–1684
Drake MJ, Doumouchtsis SK, Hashim H, Gammie A (2018) Fundamentals of urodynamic practice, based on International Continence Society good urodynamic practices recommendations. Neurourol Urodyn 37(S6):S50–S60
Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21(3):261–274
Toppercer A, Tetreault JP (1979) Compliance of the bladder: an attempt to establish normal values. Urology 14(2):204–205
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379
Mathew AT, Fishbane S, Obi Y, Kalantar-Zadeh K (2016) Preservation of residual kidney function in hemodialysis patients: reviving an old concept. Kidney Int 90(2):262–271
Chen JL, Lee MC, Kuo HC (2012) Reduction of cystometric bladder capacity and bladder compliance with time in patients with end-stage renal disease. J Formos Med Assoc 111(4):209–213
Theodorou C, Katsifotis C, Bocos J, Moutzouris G, Stournaras P, Kostakis A (2003) Urodynamics prior to renal transplantation–its impact on treatment decision and final results. Scand J Urol Nephrol 37(4):335–338
Zermann DH, Loffler U, Reichelt O, Wunderlich H, Wilhelm S, Schubert J (2003) Bladder dysfunction and end-stage renal disease. Int Urol Nephrol 35(1):93–97
Kashi SH, Wynne KS, Sadek SA, Lodge JP (1994) An evaluation of vesical urodynamics before renal transplantation and its effect on renal allograft function and survival. Transplantation 57(10):1455–1457
Karam G, Giessing M (2011) Bladder dysfunction following renal transplantation is it predictable? Transplant Proc 43(1):387–390
Martín MG, Castro SN, Castelo LA, Abal VC, Rodríguez JS, Novo JD (2001) Enterocystoplasty and renal transplantation. J Urol 165(2):393–396
Lee YH, Bang H, Kim DJ (2016) How to establish clinical prediction models. Endocrinol Metab (Seoul) 31(1):38–44
Fischer JE, Bachmann LM, Jaeschke R (2003) A readers’ guide to the interpretation of diagnostic test properties: clinical example of sepsis. Intensive Care Med 29(7):1043–1051
Yuan Z, Tang Z, He C, Tang W (2015) Diabetic cystopathy: a review. J Diabetes 7(4):442–447
Rude T, Nassiri N, Naser-Tavakolian A, Ginsberg D (2019) The role of urodynamics in the pre-transplant evaluation of renal transplant. Curr Urol Rep 20(5):26
Niu S, Black P, Padmanabhan P (2019) Conservative management of hostile bladders with intravesical botulinum toxin for successful renal transplantation. Urol Case Rep 22:73–75
Acknowledgements
We thank Assistant Professor. Dr.Pitchaya Tantiyavarong (PhD. clinical epidemiology) for being the consultant of the clinical statistical analysis of this study.
Funding
This study received funding from Thammasat University Hospital, Thammasat University and was supported by the Research group in surgery, Faculty of Medicine, Thammasat University (Grant number: 2/2563).
Author information
Authors and Affiliations
Contributions
TT: conceptualization, research design, methodology, research summary and recommendation, writing—review and editing (equal); formal analysis (lead). VS: conceptualization, research design, methodology, data-analysis, research summary and recommendation (equal); investigation, writing—original draft preparation and editing (lead).
Corresponding author
Ethics declarations
Conflict of interest
Both authors have no conflict of interest.
Animal studies
N/A.
Ethical consideration
Both authors have no conflict of interest. The study is approved by The Human Research Ethics Committee of Thammasat University (Faculty of Medicine). The date of approval is April 23, 2020. The approval number is MTU-EC-SU-6-043/63. All patients were informed and signed consent forms before participating in the study. This study is approved by the Thai Clinical Trials Registry Committee on 09 February 2021. The TCTR identification number is TCTR20210209006.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tangpaitoon, T., Swatesutipun, V. Factors associated with low-compliance bladder in end-stage renal disease patients and development of a clinical prediction model for urodynamic evaluation: the DUDi score. Int Urol Nephrol 55, 75–84 (2023). https://doi.org/10.1007/s11255-022-03399-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03399-8