Abstract
Purpose
To investigate whether extensive renal artery isolation during robotic-assisted partial nephrectomy (RAPN) for renal cell carcinoma (RCC) affects blood pressure (BP) of patients with poorly controlled hypertension.
Methods
We included 60 patients diagnosed with poorly controlled hypertension who underwent RAPN by an experienced surgeon. The renal artery of the treated kidney was sufficiently isolated. Systolic BP (SBP), diastolic BP (DBP) and antihypertensive medication information were obtained at baseline and 3- and 6-month follow-up after surgery. Primary endpoints were changes in BP, and medications. Predictors of SBP reduction at 3 months were assessed by multivariable logistic regression.
Results
All 60 RAPN procedures were successful, with no major intra- or postoperative complications. Mean SBP and DBP decreased significantly at 3 months after surgery (SBP, −7.8 ± 6.3 mmHg, P < 0.001; DBP, −4.2 ± 6.4 mmHg, P = 0.01). SBP and DBP did not differ between 3- and 6-month follow-up. The mean number of BP medications prescribed was lower at 3 months than baseline (1.7 ± 1.0 vs 2.1 ± 1.0, P = 0.016). The only significant predictor of SBP reduction at 3 months was baseline SBP.
Conclusions
Renal denervation with extensive renal artery isolation during RAPN may improve BP control among patients with poorly controlled hypertension in short term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Renal cell carcinoma (RCC) represents approximately 90% of all kidney malignancies. The incidence has shown an increasing trend worldwide [1]. The incidence rates tend to be elevated in older individuals, with a peak incidence at age 60–70 years. Smoking, obesity, and hypertension are important etiologic factors [2]. Partial nephrectomy (PN) has been the standard treatment for small, organ-confined RCC, and robotic-assisted PN (RAPN) has been widely applied.
Hypertension is an important global health issue because of its high prevalence and is a pivotal risk factor of cardiovascular disease and chronic kidney disease [3]. Moreover, numerous studies, including several large, prospective cohort studies, proposed a possible relation between hypertension and RCC [4, 5]. Despite the great progress in pharmaceutical treatment, many hypertensive patients still have poor blood pressure (BP) control. Renal denervation (RDN) has been a promising treatment for resistant hypertension in the past decade. The mechanism for RDN to treat resistant hypertension is breaking renal sympathetic nerves (RSNs) around renal arteries, thus decreasing autonomic sympathetic tone, renin release and renal tubular reabsorption [6].
During RAPN, the renal hilum is identified and exposed and the renal artery is isolated to prepare for temporary clamping. Then the kidney is separated to expose the tumor margin fully for tumor resection and reconstruction. On the basis of the effect of RDN, we hypothesized that thorough peri-arterial tissue stripping may affect RSNs and lead to altered BP. The aim of the present study was to investigate the effect of RAPN with relatively complete isolation of the renal artery on BP in patients with poorly controlled hypertension.
Materials and methods
Patient population
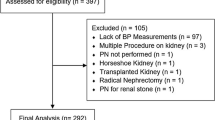
We prospectively investigated consecutive patients with kidney neoplasms and poorly controlled hypertension who underwent RAPN in our center between June 2018 and March 2020. The inclusion criteria were age between 25 and 85 years, indication for RAPN, and a history of hypertension and taking antihypertensive medications but with poor BP control [systolic BP (SBP) ≥ 140 mmHg and/or diastolic BP (DBP) ≥ 90 mmHg] at hospital admission. We excluded patients with bilateral renal tumors, tumors larger than 7 cm and severe atherosclerosis. Eligible patients underwent comprehensive assessments, which ruled out secondary hypertension (Fig. 1). The study was approved by the medical ethical committee of Nanjing Drum Tower hospital and were in accordance with the Helsinki Declaration. All patients gave their informed consent.
Surgical technique
The surgical procedures were performed as described by a single experienced surgeon [7]. Briefly, the da Vinci Surgical System was used with a standard 3-arm approach, with fourth and fifth trocars for the assistant. The renal pedicle was identified and carefully isolated. Renal arteries were extensively isolated. The peri-arterial tissues were fully stripped, divided and cauterized, to clear the arterial adventitia surface (Fig. 2c, d). Accessory renal arteries and branches were also isolated under appropriate conditions (Fig. 2a, b). Then, the perinephric fat was separated to identify the tumor margin and exclude satellite lesions. Robotic scissors were used to excise the renal mass. The renal artery was clamped with vascular clips in most cases. For reconstruction, the parenchymal defect was closed using the single-layer renorrhaphy technique.
Representative renal arteries in CTAs and surgery videos. a A small accessory renal artery arising from the abdominal aorta feeds the left kidney with a mass at the superior pole. b There is only a main renal artery supplying the left kidney with a neoplasm in the middle zone. c, d The process of renal arteries dissection, during which the peri-arterial tissues were stripped, divided and cauterized to clear the arterial adventitia surface (blue arrow)
BP assessments
SBP and DBP were assessed at baseline and at 3 and 6 months after RAPN, and changes were analyzed. Every BP value was calculated as the mean of three readings, with a 5-min rest between each measurement. BP measurements were collected twice a day, in the morning (9:00) and afternoon (16:00). Daily BP was the average of the two results. At least 2 days of BP measurements were obtained. The final BP value was calculated as the mean of the daily BPs.
Medications
Detailed information on medication was recorded. If necessary, we invited cardiologists to adjust the background BP-lowering medications before surgery. The prescription after adjustment was considered the baseline medication, and baseline BP was calculated after the medication adjustment. Participants were instructed to maintain their medications at the adjusted doses from hospital discharge to the first visit at 3 months.
At 3 months, cardiologists in the cardiovascular specialist outpatient clinic of our center reconciled the medication, with blinding to the study. Changes in number of antihypertensive medications or dosage adjustment were obtained and documented. Furthermore, the re-modified prescription was maintained until the 6-month follow-up.
Drug enhancement was defined as upregulated number, dose or class of BP medication to improve BP control. Drug mitigation was defined as downregulated number, dose or class of medication intending to weaken the suppression effect.
Other assessments
Preoperative urinary CT angiography was performed as routine and 3-D reconstructions of renal arteries were produced. Additional arteries (containing accessory renal artery and aberrant branches) were noted. Surgical videos were all archived and reviewed to record the number of arteries isolated.
Other data collected included patient demographics, personal history, nephrometry score, clinical data, surgical procedures, intraoperative or postoperative complications, perioperative outcomes and pathology. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Diseases equation [8]. Plasma renin activity (PRA) and angiotensin II and aldosterone levels were measured at baseline and 3 months after surgery for patients without renin–angiotensin blocker drugs (anti-renin drugs, angiotensin-converting enzyme (ACE) inhibitor or angiotensin receptor blocking drugs) or antiadrenergic anti-hypertensive drugs. The specific time for blood sampling was 8:00 in the morning and the patient was asked to sit for half an hour before blood samples were taken.
Statistical analysis
Data are presented as mean ± SD, median and interquartile range (IQR) for continuous variables or number (%) for categorical variables. Student t test was used to analyze continuous variables and chi-square test for categorical variables. Mean BP and other paired data at follow-up were compared with those at baseline by paired t test as appropriate. Univariable and multivariable stepwise logistic regression was used to explore potential factors relating to reduced BP. Variables with P < 0.15 on univariable analysis were included in multivariable models. Two-sided P < 0.05 was considered statistically significant. Statistical analysis was performed with SPSS v17.0 (SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc.).
Results
Study population
Between January 2018 and November 2019, we included 60 patients (41 men): median age was 61 (IQR 52–66) years, median body mass index 25.5 (IQR 23.4–27.7) kg/m2 and median duration of hypertension 9.5 (IQR 5–14) years (Table 1).
Table 2 describes tumor and surgery characteristics. The median tumor size was 3.5 (IQR 2.5–4.5) cm. The median R.E.N.A.L score was 8 (IQR 6.5–10). All RAPN surgeries were completed without major intraoperative or perioperative complications. The median surgery time was 140 (IQR 121–160) min and median ischemia time 20 (IQR 15–25) min. The intraoperative estimated blood loss was 100 (IQR 50–200) ml, with no severe hemorrhage. The RCC subtype was clear cell in 45 (75%) cases.
Efficacy endpoints
For all patients, mean baseline SBP/DBP was 146.3 ± 8.3/88.5 ± 8.6 mmHg, and 48 (80%) had high baseline SBP (≥ 140 mmHg) despite medication adjustment; the proportion of high SBP significantly decreased at the two follow-up visits (41.7% and 38.3%) (P < 0.05) (Fig. 3c). At 3 months, SBP and DBP had significantly decreased −7.8 ± 6.3 mmHg [95% confidence interval (CI) −9.5 to −6.2; P < 0.001] and −4.2 ± 6.4 mmHg (95% CI −5.9 to −2.6; P < 0.001), respectively (Fig. 3a). Although the mean BP was slightly lower at 6 than 3 months, we found no significant differences for SBP between 3 and 6 months (138.5 ± 6.4 vs 138.1 ± 5.5 mmHg, P = 0.079) or DBP (84.3 ± 5.7 vs 84.0 ± 5.0 mmHg, P = 0.066) (Fig. 3b). Heart rate (HR) did not significantly change between baseline and 3 months (76.8 ± 9.9 vs 75.2 ± 10.2 bpm, P = 0.298).
Changes in blood pressure (BP) and antihypertensive medication over time. a Office-measured systolic BP (SBP) and diastolic BP (DBP) at baseline, 3 months, and 6 months, respectively. b SBP and DBP reduction at 3 and 6 months after surgery. c Distribution of office-measured SBP at baseline, 3 months, and 6 months, showing a larger proportion of normal SBP postoperatively. d The number of antihypertensive drugs used before and 3 months after surgery
The mean baseline number of antihypertensive drugs was 2.1 ± 1.0 and the mean number of antihypertensive medications prescribed was significantly reduced at 3 months (−0.4 drugs; P = 0.0006) (Fig. 3d). The number of drugs was increased for 4 (6.7%) patients, but 24 (40%) showed drug mitigation, 5 with normal BP and no antihypertensive medication (Table 3).
According to preoperative CT angiography, 27/60 (33.3%) patients had accessory renal arteries or aberrant branches supplying the treated kidneys or tumors. However, additional arteries were not all isolated in 15 cases (Table 2) for various reasons.
Laboratory analyses
From baseline to 3 months, we observed no significant changes in serum creatinine level (0.80 ± 0.18 vs 0.82 ± 0.19 mg/dl, P = 0.064) or eGFR (93.4 ± 14.7 vs 93.0 ± 14.6 ml/min/1.73 m2, P = 0.09) (Table 3).
For the 29 patients not taking drugs that antagonized the renin–angiotensin system, or antiadrenergic anti-hypertensive drugs, baseline PRA was 4.5 ± 7.9 ng/ml/h as compared with 2.0 ± 1.6 ng/ml/h at 3 months after surgery, with mean change −2.5 ng/ml/h (95% CI −5.2 to −0.79; P = 0.01). Mean angiotensin II level was reduced by −11.3 pg/ml (95% CI −69.1 to 6.8; P = 0.106) and mean aldosterone level by −3.5 pg/ml (95% CI −26.6 to 9.5; P = 0 .347) (Table 3).
Predictive factors
On univariable logistic regression, SBP reduction at 3 months was associated with baseline SBP [odds ratio (OR) 1.249, 95% CI 1.081–1.444, P = 0.003] and additional artery (OR 0.184, 95% CI 0.036–0.930, P = 0.041) (Table 4). We included ‘Cardiovascular disease’ (OR 2.929, 95% CI 0.692–12.401, P = 0.145), ‘Tumor side’ (OR 0.357, 95% CI 0.094–1.351, P = 0.129), ‘Baseline-SBP’ (P < 0.05) and ‘Additional artery’ (P < 0.05) in the multivariable logistic regression model. On multivariable analysis, the only independent predictor of SBP reduction was high baseline SBP (OR 1.267, 95% CI 1.076–1.491, P = 0.005).
Discussion
We wondered whether RAPN for RCC after extensive renal artery isolation affects BP in patients with poorly controlled hypertension. In this study, mean SBP and DBP decreased significantly at 3 months after surgery along with reduced requirement for antihypertensive medication. Extensive renal artery isolation during RAPN may improve BP control among patients with poorly controlled hypertension.
The effect of PN for renal masses on postoperative BP is inconsistent among several observational studies. Novick et al. evaluated the effect of PN for solitary kidneys in 14 patients, finding no changes in BP during a mean follow-up of 7.7 years [9]. In another study, PN was considered to not result in initial or long-term postoperative deterioration in BP [10]. More recently, an interesting retrospective cohort study of solitary kidney patients performed by Gupta et al. suggested that BP remains stable in the short-term and long-term after PN [11]. Conversely, Inoue et al. reported a progression of BP with PN as compared with radical nephrectomy [12]. Hutchinson et al. found PN independently associated with increased number of antihypertension medications [13]. Some case reports have indicated that PN may precipitate postoperative hypertension due to complications or “Page kidney” phenomenon [14, 15]. However, these effects may be transient if there are no renal arterial or peripheral complications [16]. More importantly, the development of hypertension is multifactorial, and other factors such as renal nerves are usually ignored. Differing from the previous PN studies, we focused on the impact of removing RSNs during RAPN.
RSNs to the kidneys terminate in the blood vessels, juxtaglomerular apparatus, and renal tubules. Stimulation of RSNs increases renin release and sodium reabsorption and reduces renal blood flow [17]. RDN was found effective for improving BP by denervating RSNs. The catheter-based RDN system emerged to selectively ablate RSNs using radiofrequency ablation. Although early results of BP control in multiple animal or human studies were encouraging, this therapeutic application has long been debated [18]. In humans, the nerves pass from the sympathetic chain and ganglia to the kidneys via the adventitia of renal arteries, leading to the hilum or just outside in peri-arterial adipose tissue and connective tissue [19]. There is a considerable distance between the arterial lumen and RSNs, which mostly locate in the tunica adventitia or surrounding tissues, especially in the proximal segment [20]. Electrodes placed inside the lumen of the artery cannot deliver radiofrequency energy effectively to all renal nerve bundles along the renal artery, especially to nerves beyond 2 mm from the lumen [21, 22].
The laparoscopic approach has been proposed to overcome the limitations of the catheter approach. Gerber et al. found that the approach was capable of removing nerves that are typically not removed by radiofrequency-based catheter ablation [23]. In a beagle model, Bai et al. reported that RDN was more effective in the adventitial group with laparotomy conducted from outside the renal artery than the intimal group with intervention from inside the artery [24]. Therefore, several laparoscopy-based RDN models were designed to ablate the renal nerves from the exterior of the renal artery [25].
Laparoscopic RDN with no ablation also shows promise in the treatment of carefully selected patients with resistant hypertension. Keisuke reported two cases of unilateral radical nephroureterectomy for renal pelvic cancer, during which the peri-arterial tissues containing RSNs were stripped to expose the vessel and ligated after cauterization; the patients showed reduced BP after surgery [26]. In our study, the renal artery was skeletonized, and adventitia around the renal artery containing RSNs was stripped off, disconnected and cauterized. Also, complete separation of the kidney further helped to remove residual sympathetic nerves that do not enter the hilum through the renal artery. Moreover, because the afferent sympathetic nerves were eliminated together with efferent nerves [19], the artery clamping or parenchyma compression effect signal from the kidney to the central nervous system by sensory pathways might be interrupted during our surgical procedure, which may be another explanation for the decreased BP.
Unilateral treatment might reduce BP if complete RDN could be achieved. One case showed that even unilateral RDN can be fully successful and decrease BP to a remarkable extent in a 12-month period [27]. Gao et al. reported considerable BP decrease with laparoscopic-based perivascular unilateral RDN [28]. In an animal model, unilateral RDN improved mean arterial pressure and cardiac autonomic balance in congestive heart failure by reducing sympathetic tone [29].
Measurements of PRA, norepinephrine spillover, or both may help in estimating the activity of the efferent RSNs. In our study, patients not on drugs antagonizing the renin–angiotensin system showed reduced PRA and angiotensin and aldosterone levels, suggesting an effect on RSNs, which was also reported in RDN studies [17]. We evaluated BP changes first at 3 months, which was considered an acceptable time for patients to observe a decrease in BP and can avoid the effects of other factors such as perioperative anesthesia, pain, fluid infusion, lifestyle changes, and seasonal changes on BP [30]. Moreover, we avoid the influence of BP optimization prior to surgery, and the medication remained unchanged during the first 3 months postoperatively, which helped in evaluating the effect of surgery.
It should be noted that the present study has some limitations. This study was terminated prematurely because most enrolled patients were lost to follow-up about 9 months postoperatively as they became reluctant, making this study a preliminary report with relatively small sample size and short follow-up time. Therefore, the finding of the present study should be interpreted carefully, and further investigations are urgently needed. In addition, there could have been a bias due to heightened self-awareness of hypertensive patients in managing blood pressure. The lack of a control arm is another drawback. Besides, we did not quantify the specific degree of RDN, for example the length of renal arterial adventitia surface, nor we took into account drug adherence, the effect of nerve fiber recovery or neuronal regeneration [17]. Moreover, to evaluate the efficacy of RDN, assessing plasma levels or kidney tissue content of norepinephrine should be valuable but was difficult to implement in our study. Furthermore, although we had tried to standardize BP measurements, ambulatory BP monitoring maybe more accurate. Last but not least, despite no attempts to perform RDN with ablation concurrently with RAPN, this combination may have a more pronounced denervation effect. For selected patients, RDN and RAPN combined may confer greater benefit beyond a decrease in BP, such as an improvement in renal function especially for solitary kidney tumors, or even oncological outcome [31]. However, further study is needed to evaluate the feasibility of this treatment mode.
Conclusions
Our short-term findings suggest that RAPN with extensive renal artery isolation may benefit the BP of patients with poorly controlled hypertension. The removal of RSNs may play a role, but the exact mechanism and long-term effects need further investigation.
Data availability statement
The data supporting our findings are presented in the article. The datasets of the current study are available from the corresponding author on reasonable request.
References
Ferlay J, Colombet M, Soerjomataram I et al (2018) Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer 103:356–387
Tahbaz R, Schmid M, Merseburger AS (2018) Prevention of kidney cancer incidence and recurrence: lifestyle, medication and nutrition. Curr Opin Urol 28:62–79
Ettehad D, Emdin CA, Kiran A et al (2016) Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387:957–967
Weikert S, Boeing H, Pischon T et al (2008) Blood pressure and risk of renal cell carcinoma in the European prospective investigation into cancer and nutrition. Am J Epidemiol 167:438–446
Sanfilippo KM, McTigue KM, Fidler CJ et al (2014) Hypertension and obesity and the risk of kidney cancer in 2 large cohorts of US men and women. Hypertension 63:934–941
Ranard LS, Swaminathan RV (2019) Renal artery denervation for hypertension. Curr Treat Options Cardiovasc Med 21:7
Zhao X, Lu Q, Campi R et al (2018) Endoscopic robot-assisted simple enucleation versus laparoscopic simple enucleation with single-layer renorrhaphy in localized renal tumors: a propensity score-matched analysis from a high-volume centre. Urology 121:97–103
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Novick AC, Gephardt G, Guz B et al (1991) Long-term follow-up after partial removal of a solitary kidney. N Engl J Med 325:1058–1062
Lawrentschuk N, Trottier G, Mayo K et al (2012) Effects of partial nephrectomy on postoperative blood pressure. Korean J Urol 53:154–158
Gupta N, Ganesan V, Gao TM et al (2021) The effect of partial nephrectomy on blood pressure in patients with solitary kidney. World J Urol 39:1577–1582
Inoue M, Fujii Y, Yokoyama M et al (2015) Progression of hypertension after partial nephrectomy in patients with renal tumors: a preliminary report. Int J Urol 22:797–798
Hutchinson R, Singla N, Krabbe LM et al (2017) Increased use of antihypertensive medications after partial nephrectomy vs. radical nephrectomy. Urol Oncol 35:660
Zargar H, Aning J, Legiehn G et al (2014) Renovascular hypertension after laparoscopic partial nephrectomy. J Urol 191:1418–1420
Kiczek M, Udayasankar U (2015) Page kidney. J Urol 194:1109–1110
Sakurai T (2015) Editorial comment to progression of hypertension after partial nephrectomy in patients with renal tumors: a preliminary report. Int J Urol 22:798–799
Schlaich MP, Sobotka PA, Krum H et al (2009) Renal denervation as a therapeutic approach for hypertension: novel implications for an old concept. Hypertension 54:1195–1201
Bhatt DL, Kandzari DE, O’Neill WW et al (2014) A controlled trial of renal denervation for resistant hypertension. N Engl J Med 370:1393–1401
Tellman MW, Bahler CD, Shumate AM et al (2015) Management of pain in autosomal dominant polycystic kidney disease and anatomy of renal innervation. J Urol 193:1470–1478
Sakakura K, Ladich E, Cheng Q et al (2014) Anatomic assessment of sympathetic peri-arterial renal nerves in man. J Am Coll Cardiol 64:635–643
Vink EE, Goldschmeding R, Vink A et al (2014) Limited destruction of renal nerves after catheter-based renal denervation: results of a human case study. Nephrol Dial Transplant 29:1608–1610
Atherton DS, Deep NL, Mendelsohn FO (2012) Micro-anatomy of the renal sympathetic nervous system: a human postmortem histologic study. Clin Anat 25:628–633
Gerber RC, Bahler CD, Kraus MA et al (2016) Laparoscopic renal denervation for uncontrolled hypertension due to medication intolerance: a case report. Am J Kidney Dis 68:131–133
Bai M, Yang C, Gao C et al (2015) Effects of renal denervation from the intima and the adventitia of renal arteries on renal sympathetic nerve activity in dogs: a comparative study. Cardiology 131:189–196
Ye E, Baik J, Lee S et al (2018) Design and simulation of novel laparoscopic renal denervation system: a feasibility study. Int J Hyperthermia 35:9–18
Okamura K, Satou S, Setojima K et al (2018) Reduction of blood pressure following after renal artery adventitia stripping during total nephroureterectomy: potential effect of renal sympathetic denervation. Am J Case Rep 19:567–572
Kostka-Jeziorny K, Radziemski A, Tykarski A et al (2015) Effect of unilateral catheter-based renal sympathetic denervation in a patient with resistant hypertension. Kardiol Pol 73:132
Gao C, Zhao L, Zhu L et al (2019) Laparoscopic-based perivascular unilateral renal sympathetic nerve denervation for treating resistant hypertension: a case report. Hypertens Res 42:1162–1165
Schiller AM, Haack KK, Pellegrino PR et al (2013) Unilateral renal denervation improves autonomic balance in conscious rabbits with chronic heart failure. Am J Physiol Regul Integr Comp Physiol 305:R886-892
Townsend RR, Mahfoud F, Kandzari DE et al (2017) Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 390:2160–2170
Fujita M, Hayashi I, Yamashina S et al (2005) Angiotensin type 1a receptor signaling-dependent induction of vascular endothelial growth factor in stroma is relevant to tumor-associated angiogenesis and tumor growth. Carcinogenesis 26:271–279
Acknowledgements
We thank colleagues of cardiology for the professional guidance.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
XW: conceptualization; methodology; software; visualization; writing—original draft; XZ: methodology; review and editing; CJ and GL: investigation; software; XL and HG: supervision; validation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. The abstract part of the paper were previously reported in the “abstracts communication” of the AUA annual meeting.
Ethical approval
All the procedure of this study was approved by the Medical Ethics Committee of the Affiliated Drum Tower Hospital of Nanjing University Medical School (Number: 2020–090-0) and were in accordance with the Helsinki Declaration.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, X., Zhao, X., Ji, C. et al. Effect of extensive artery isolation during robotic-assisted partial nephrectomy on blood pressure of patients with poorly controlled hypertension: a preliminary study. Int Urol Nephrol 55, 29–36 (2023). https://doi.org/10.1007/s11255-022-03384-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03384-1