Abstract
Purpose
Brazil is the third country globally in dialysis patients. Little is known about the impact of the type of health insurance on the outcome of these patients after COVID-19.
Methods
We analyzed comorbidities, sociodemographic factors, and dialysis-related parameters from a retrospective cohort study of 1866 Brazilian chronic hemodialysis patients with COVID-19 from Feb 2020–July 2021. We evaluated the influence of health insurance (private vs. public) on the intensive care unit admission and 90 day fatality risk.
Results
From 1866 hemodialysis patients, 455 (24%) were admitted to the intensive care unit, and 350 (19%) died. The mean age was 57.5 years, 88% had public health insurance. Crude case-fatality rate was not different between groups (private vs. public risk ratio 1.11; 95% CI 0.82–1.52, p = 0.498). In fully adjusted multivariate models, patients with private health insurance did not have a higher chance to be admitted to an intensive care unit (odds ratio 0.97; 95% CI 0.63–1.50, p = 0.888), but they presented a lower death risk (hazard ratio 0.56; 95% CI 0.37–0.85, p = 0.006).
Conclusion
The type of health insurance did not influence the access of hemodialysis patients with COVID-19 to an intensive care unit, but patients with private health insurance had a lower mortality risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since February 3rd, 2020, when Brazil recognized COVID-19 as an emergency public health problem, 20 million Brazilians have been infected with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and nearly 575,000 have died by August 2021 [1], one of the worst counts in Latin America. Chronic kidney disease (CKD) has been associated with a higher risk of mortality after COVID-19, and both disorders share similar risk factors for poor outcomes [2,3,4]. In Brazil, where 80% of hemodialysis patients depend on the public health system to fund their treatment [5, 6], little is known about the outcomes of patients on chronic hemodialysis with COVID-19 and with private health care compared to those with public health insurance.
Similar to other countries [7, 8], according to data from the Brazilian Ministry of Health, which includes 67,180 hospitalized cases of COVID-19, 65% had ≥ 50 years of age, 57.5% were male, 66% had cardiovascular disease, and 54.5% had diabetes [2]. Much of these comorbidities and sociodemographic characteristics are present in patients on chronic dialysis [3, 5, 6], who, irrespective of the COVID-19, have a higher mortality rate than those without CKD [9]. Considering that severe forms of COVID-19 are common in hemodialysis patients [4, 6, 10,11,12], a well-structured health care system for these patients would be fundamental. Since 1993, a unified health system (Sistema Único de Saúde, SUS) implemented in Brazil allows universal and free access to health resources [13]. The private health system serves about 28.5% of the Brazilian population [14]. Approximately 25% of the people with private health insurance pay for it out of their pocket, while around 75% have their care totally or partially paid for by their employer [15]. Although Brazil has a unified and universal health system, chronic underfunding of health worsened after the economic austerity measures imposed by the government in 2016, limiting the growth of public expenditure until 2036 [13]. Considering that the municipalities are responsible for part of the public health expenditure, there is an important socio-economic gap between the richest and the poorest Brazilian cities concerning the distribution of health resources, accentuating inequality in the population’s health care [13, 14], as in other developing countries [16]. This situation can impact the care of patients with chronic diseases and limit local hospital assistance for those with a severe form of COVID-19.
It is estimated that 30% of patients hospitalized for COVID-19 require intensive care units (ICU) [2]. Although both the SUS and the private health system have increased the number of ICU beds in all regions of Brazil [17], it remains unknown if the type of health care insurance (private or public) influences the outcomes of hemodialysis patients with COVID-19. This study aimed to analyze the impact of the health insurance modality on the ICU access and 90 day mortality of chronic hemodialysis patients with this disorder.
Materials and methods
Study design
This is a retrospective cohort observational study with data collection performed through filling out a form available online for dialysis clinics affiliated with the Brazilian Society of Nephrology (BSN). All dialysis clinics in the country were invited to participate in the study utilizing various means of communication. Those whose managers accepted participating filled out individual patient information and sent it electronically to the research coordinating center. Adult patients (> 18 years) with kidney failure undergoing kidney replacement therapy through hemodialysis for at least three months were selected. The analysis interval included patients diagnosed since the beginning of the country’s pandemic (Feb 26th, 2020) until Jul 23rd, 2021. As an inclusion criterion, the patients should have had a diagnosis of COVID-19 by laboratory examination, either by RT-PCR or serology. The Research Ethics Committee of the Federal University of the State of São Paulo approved the study under registration number 39988220.0.1001.5505.
Data collection
Data were provided by the participating outpatient dialysis centers of the country using the patients’ medical records to fill an electronic form. Collected information included sociodemographic characteristics (age, gender, race, and region of Brazil), previous comorbidities, dialysis vintage, and vascular access. Concerning COVID-19, the confirmatory diagnosis tool, symptoms, hospitalization, ICU admission, and mortality were registered. The form accessed by the clinics for completion is available online (http://censo-sbn.org.br/reglgCovid19). In case of doubts, a BSN Registry investigator contacted the clinic for data validation.
Statistical analysis
Qualitative variables are initially described by their frequency and percentage or mean and standard deviation for quantitative variables. The Kolmogorov–Smirnov test assessed the normality of data distribution. Case-fatality rate and rate ratio (RR) to death were calculated per 1000 person-days. A survival curve analysis in relation to the health care status to the outcome was presented by the Kaplan–Meier method, and the log rank test verified any difference. We used a chi-square test and Student’s t test to compare frequencies or means of the secondary variables in relation to the primary exposure (private or public health insurance). If not on a causal pathway, variables associated with the primary exposure and risk factors to the outcome were considered potential confounders. Multivariate explanatory models were proposed to verify the association between the type of health plan and access to intensive care or the occurrence of death after COVID-19 diagnosis. Initially, we used the Mantel–Haenszel stratification to evaluate confounders and any effect modification in the association between the type of health plan and access to intensive care units. Continuous variables (body mass index, BMI, and age) were split by tertiles to keep a balance for each category group and avoid data sparsity in the analysis. All variables with a known confounder effect in the exposure or with an effect modification greater than 10% to the outcome in the Mantel–Haenszel method were included in the multivariate logistic regression analysis. Models were constructed progressively, including variable categories (sociodemographic, variables associated with hemodialysis, and comorbidities). Subsequently, we investigated the influence of the type of health insurance (private or public) on death within 90 days after the diagnosis of COVID-19. As the SARS-CoV-2 vaccination roll-out for dialysis patients in Brazil was in May 2021, encompassing less than 12% of the subjects’ enrollment period, we decided not to include patients’ vaccination status in the analysis. Crude and adjusted hazard ratios for each covariate were calculated. Similarly, all variables with a known confounder effect in the exposure or with an effect modification greater than 10% to the outcome in the bi-variate analysis were included in the final multivariate model by Cox regression analysis in a progressively way by variable categories (sociodemographic, variables associated with hemodialysis, comorbidities, most prevalent symptoms related to COVID-19, and need for hospital admission). For both analyses, logistic regression and Cox regression, the likelihood test evaluated any interaction factor for the principal exposure variable with the other variables. Substantial effect modification was just considered when significant effect by subgroups was found. For multivariate analysis, the linear effects for categorical variables age and BMI by tercile and region were verified through a departure test from linear trend. The proportional hazard assumption in the Cox regression analysis was confirmed by Nelson Aalen plots and by a formal test of proportionality. All data were analyzed using STATA/IC 15.1 software.
Results
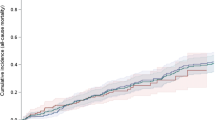
From the whole sample (n = 1903), crucial missing data were identified in 4 cases (2 for the type of health care and 2 for the type of dialysis method). In addition, we excluded five people under 18 years old (0.3%) and 28 on peritoneal dialysis (1.5%), resulting in 1866 patients on hemodialysis with COVID-19, from 68 dialysis centers, for the analysis. The average age was 57.5 ± 15.2 years, 59% were male, 12.2% had private health care, 24.4% were admitted to an ICU, and 18.8% died. Of the 1866 patients studied, 1320 (91.8%) had COVID-19 diagnosis before the SARS-COV-2 vaccination roll-out in Brazil (public health care proportion before vs after SARS-COV0-2 vaccination, 87.5 vs. 91.5%, p = 0.147). The percentage of deaths was similar before and after SARS-COV-2 vaccine implementation in the country (19.0 vs. 16%, respectively, p = 0.424), and was independent of the type of health care (before vaccination: 18 vs. 21% for those with public or private health care, respectively, p = 0.412; after vaccination, the corresponding percentages were: 17 vs. 8%, respectively, p = 0.378). The crude case-fatality rate for patients with public health care was 3.95 per 1000 person-days (95% CI 3.52–4.42), while for patients with private health care was 4.40 per 1000 person-days (95% CI 3.29–5.87). The crude case-fatality rate was not different between groups (private vs. public: RR 1.11; 95% CI 0.82–1.52, p = 0.498). The cumulative survival of COVID-19 hemodialysis patients, factored by type of health insurance (log rank test, p = 0.458) is in Fig. 1.
The distribution of other studied variables concerning the health care status is in Table 1. Patients with private health insurance were more frequently in the older age category (≥ 75 years old) and white, had higher BMI and lower hemodialysis vintage, and most were derived from the Southeast. They used less arteriovenous fistula as HD access than those with public health care (64 vs. 75%, respectively), and had a higher frequency of diabetes, previous myocardial infarction and/or stroke, and some COVID-19 clinical findings (dyspnea, and fatigue/malaise). Hospital and ICU admissions were more common in patients with private health insurance (55 vs. 37%, and 33 vs. 23%, respectively).
Health care status and ICU admission
The crude and adjusted odds ratios of ICU admission after stratifying for potential confounders and other variables of interest are in the supplementary Table 1. Patients with private health care showed a 61% higher chance of being admitted to an ICU than those with public health care (crude OR 1.61; 95% CI 1.19–2.18). The summarized odds ratio indicated a confounding effect to the association studied after adjusting for age and BMI tertile groups, region, time on hemodialysis, type of vascular access, diabetes, and previous stroke history. An interaction effect was not found for all confounders and the health care plan status after comparing the log-likelihoods obtained in each model excluding and including the interaction parameters by logistic regression analysis. An explanatory logistic regression model of the health care plan status for admission in ICU considering all identified confounder variables and others with potential confounding effect is presented in the Table 2. The presence of a private health care plan was only significantly associated with a greater chance of admission to the ICU when factors related to hemodialysis treatment or previous comorbidities did not enter into the models (model 1). After adjusting for all variables in the final model, the presence of private health care was not significantly associated with ICU admission (OR 0.97; 95% CI 0.63–1.50, p = 0.888). When considering hospital admission as the outcome, after adjusting for the same confounder variables, the presence of a private health plan did not increase the chance of admission (OR 1.25; 95% 0.82–1.90; p = 0.292).
Health care status and death
Table 3 shows crude and adjusted hazard ratios of death after stratifying for potential confounder variables and other variables of interest. The presence of private health care was not associated with death in patients on hemodialysis after COVID-19 infection compared to those with public health care (crude HR 1.12, 95% CI 0.82–1.53). Although the presence of private health care was not significantly associated with an increased risk of death, this effect was slightly confounded by other variables such as age, BMI, region, hemodialysis vintage, and diabetes (Table 3). However, when considering the main exposure adjusted for the need for hospitalization, the presence of private health care showed a protective effect to death after adjustment for hospital admission (adjusted HR 0.73; 95% CI 0.53–1.00, p = 0.047) and a trend toward protection after adjusting for ICU admission (adjusted HR 0.75; 0.55–1.02, p = 0.07). In multivariate analysis (Table 4), private health care was associated with lower fatality than public health care adjusting for all potential confounders and for hospital and ICU admission (HR 0.56; 0.37–0.85, p = 0.006; model 4).
Discussion
In this large observational study, having private health care was not associated with a higher chance of being admitted to an intensive care unit after COVID-19 infection in patients on chronic hemodialysis compared to those with public health care. However, having private health care was associated with lower lethality after adjustment for confounder variables. As far as we know, this is the first study to assess the impact of the type of health care insurance on the outcome of patients on hemodialysis with COVID-19 in Brazil.
Studies have shown that patients on maintenance hemodialysis may present a higher incidence and higher risk of death due to COVID-19 than the general population [18,19,20,21]. A meta-analysis of more than 396,000 patients on chronic hemodialysis found a COVID-19 incidence of 7.7% (95% CI 5.0–10.9%) and a mortality rate of 22.4% (95% CI 17.9–27.1%) [21]. Regarding the severity of infection by COVID-19 in this population, between 28.6% and 82.5% required hospitalization and about 6.6% to 28.6% intensive care [21,22,23,24]. A high hospitalization rate was also observed in our study, with a quarter of the sample requiring intensive care. Part of this more significant need for intensive care compared to the general population may be associated with the presence of a higher number of comorbidities such as diabetes and cardiovascular diseases [18, 25] and impaired immune response [26, 27].
Notably, in the present study, patients on hemodialysis funded by private health insurance had a higher background of factors associated with higher mortality risk (age, diabetes, previous myocardial infarction, and stroke) than those with public health care. This unfavorable background can differ between public and private health care patients from that in developed countries with more structured public health care systems and fewer inequalities [28,29,30]. In high-income countries where there is better primary care assistance available, other chronic diseases may be better treated, impacting the comorbidities profile among those who initiate dialysis and are eligible to access public primary care assistance versus those who need to pay out of pocket or do not qualify for public health care [28, 31, 32]. Considering the limitations of the Brazilian public health system to promote equality of the assistance for all regions of the country, many older people look for private health care to deal with their chronic conditions. This can justify the unfavorable background of comorbidities found in our study for those with private health care. Although lower kidney replacement therapy access and higher mortality in hemodialysis patients have been associated with lower income [33, 34], and private health insurance can be associated with higher income [15], our study focused on patients that needed urgent hospital assistance due to severe COVID-19 infection. In this circumstance, the quality of hospital care can be a pivotal factor impacting the survival of patients with severe pulmonary infection [35].
A well-structured health system, with resources and professionals trained to care for patients with greater severity and risk of complications by COVID-19, is vital for reducing the number of deaths [36]. In the present study, patients with private insurance had more chance of being admitted to the intensive care unit in a non-adjusted analysis. However, this association was no longer present after adjustment for other comorbidities and confounding factors related to worse outcomes on hemodialysis, even when considering hospital admission as an outcome, in a sub-analysis (data not shown). Brazil is the largest and most populous country in South America. Despite the SUS having advanced primary care in all country regions, there is still much inequality between the regions’ secondary and tertiary care levels [13, 17]. The distribution of intensive care beds and ICU physicians per inhabitant in public and private health systems was markedly unbalanced among the country regions before the epidemic [17]. One of the Brazilian government's responses to the epidemic was a significant increase in intensive care beds in all country regions, which reached twofold in more deprived places [17]. We believe that such an increase, particularly in public hospitals, may have contributed to the absence of differences in the adjusted chance of ICU admission between patients with public or private health insurance.
However, just increasing the physical structure to admit more patients with a severe condition of COVID-19 may not have entirely corrected chronic problems of inequalities in health care in Brazil. In a study on sepsis enrolling 21 ICUs in Brazil, the authors found a lower mortality rate in patients admitted to private than public ICUs, even after adjusting for age, severity at admission, and other comorbidities [35]. In addition, the standardized expenditure cost on patient care was lower in public hospitals than in private hospitals in this study on sepsis [35]. Another factor that may have impacted hospitalized patients with COVID-19 was the lack of adequately trained healthcare professionals. Many physicians, nurses, and physiotherapists working in ICU were not board-certified by the specialty [37, 38]. Moreover, it is also likely that better equipment, effective and expensive drugs were more available in private than public services. Thus, considering that the most deaths occurred within the first 20 days of hospital admission, our study’s higher mortality risk in patients admitted to public ICU may reflect these long-standing inequalities that surfaced during the epidemic.
The present study has some limitations. It is not possible to rule out a differential misclassification for some comorbidities, such as chronic obstructive pulmonary disease (COPD) and alcohol abuse, since the answers to these questions were based on data already available in the medical records of each hemodialysis center. Even so, smoking status was used as a proxy measure for COPD. Furthermore, although several comorbidities were included in the analyses, we were not able to include inflammatory tests and the extension of the pulmonary involvement at ICU admission. It was assumed that patients with private health insurance were admitted to private hospitals when needed considering that they hardly use public services. We may not have assessed all confounder factors as inherent to observational studies, and some residual bias may have persisted. For instance, individual income could not be included in the analysis. The anti-SARS-Cov-2 vaccination roll-out in Brazil was at the end of the patients’ recruitment period, and only a small percentage of our sample received it, hindering a more detailed analysis on this aspect. Also, as the vaccines were freely distributed to the population under the coordination of the Ministry of Health, one can assure that public and private health care patients have had equal access to them. Finally, although this is the largest COVID-19 database on hemodialysis patients in Brazil, with balanced participation among several country regions, there was lower participation of dialysis centers from the North region. Thus, it is impossible to rule out some selection bias that could enhance the differences found since this region has more significant inequalities, although with a lower proportion of dialysis patients.
This study suggests that hemodialysis patients with Covid-19 who have private health insurance have a lower risk of death than patients with public assistance. Nonetheless, the chance of hospitalization and admission to ICU was not different between groups. Although more notable in low- and middle-income countries, inequalities in health care assistance may have been amplified during this pandemic in most countries. In Brazil, where about 80% of hemodialysis patients depend on public funding (6), our findings reinforce the need for further studies assessing the socio-economic aspects and the quality of hospital care involved in the assistance of these patients.
References
Brazil (2021) Painel coronavírus. https://covid.saude.gov.br/. Accessed 24 Aug 2021
de Souza WM, Buss LF, Candido DDS, Carrera JP, Li S, Zarebski AE, Pereira RHM, Prete CA Jr, de Souza-Santos AA, Parag KV, Belotti M, Vincenti-Gonzalez MF, Messina J, da Silva Sales FC, Andrade PDS, Nascimento VH, Ghilardi F, Abade L, Gutierrez B, Kraemer MUG, Braga CKV, Aguiar RS, Alexander N, Mayaud P, Brady OJ, Marcilio I, Gouveia N, Li G, Tami A, de Oliveira SB, Porto VBG, Ganem F, de Almeida WAF, Fantinato F, Macario EM, de Oliveira WK, Nogueira ML, Pybus OG, Wu CH, Croda J, Sabino EC, Faria NR (2020) Epidemiological and clinical characteristics of the COVID-19 epidemic in Brazil. Nat Hum Behav 4(8):856–865. https://doi.org/10.1038/s41562-020-0928-4
Prichard SS (2000) Comorbidities and their impact on outcome in patients withend-stage renal disease. Kidney Int 57:S100–S104
Khatri M, Charytan DM, Parnia S, Petrilli CM, Michael J, Liu D, Tatapudi V, Jones S, Benstein J, Horwitz LI (2021) Outcomes among hospitalized chronic kidney disease patients with COVID-19. Kidney 360 2:1107–1114
Neves P, Sesso RCC, Thome FS, Lugon JR, Nasicmento MM (2020) Brazilian dialysis census: analysis of data from the 2009–2018 decade. J Bras Nefrol 42(2):191–200. https://doi.org/10.1590/2175-8239-JBN-2019-0234
Sesso R, Lugon JR (2020) Global dialysis perspective: Brazil. Kidney 360 1:216–219
Huang D, Lian X, Song F, Ma H, Lian Z, Liang Y, Qin T, Chen W, Wang S (2020) Clinical features of severe patients infected with 2019 novel coronavirus: a systematic review and meta-analysis. Ann Transl Med 8(9):576. https://doi.org/10.21037/atm-20-2124
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
USRDS (2019) United States Renal Data System. 2019 USRDS Annual Data Report: Epidemiology of kidney disease in the United States. https://www.usrds.org/annual-data-report/. Accessed 28 Aug 2021
Vergara A, Molina-Van den Bosch M, Toapanta N, Villegas A, Sanchez-Camara L, Sequera P, Manrique J, Shabaka A, Aragoncillo I, Ruiz MC, Benito S, Sanchez E, Soler MJ (2021) The impact of age on mortality in chronic haemodialysis popu-lation with COVID-19. J Clin Med. https://doi.org/10.3390/jcm10143022
Wu J, Li J, Zhu G, Zhang Y, Bi Z, Yu Y, Huang B, Fu S, Tan Y, Sun J, Li X (2020) Clinical features of maintenance hemodialysis patients with 2019 novel coronavirus-infected pneumonia in Wuhan. China Clin J Am Soc Nephrol 15(8):1139–1145. https://doi.org/10.2215/CJN.04160320
Lugon JR, Neves PDMdM, Pio-Abreu A, Nascimento MMd, Sesso R (2020) Evaluation of central venous catheter and other risk factors for mortality in chronic hemodialysis patients with COVID-19 in Brazil. Int Urol Nephrol. https://doi.org/10.1007/s11255-021-02920-9
Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, de Souza Noronha KVM, Rocha R, Macinko J, Hone T, Tasca R, Giovanella L, Malik AM, Werneck H, Fachini LA, Atun R (2019) Brazil’s unified health system: the first 30 years and prospects for the future. Lancet 394(10195):345–356. https://doi.org/10.1016/S0140-6736(19)31243-7
Júnior PRBdS, Szwarcwald ClL, Damacena GN, Stopa SR, Vieira MLcFaP, Almeida WdSd, Oliveira MMd, Sardinha LMV, Macário EM (2021) Health insurance coverage in Brazil: analyzing data from the National Health Survey, 2013 and 2019. Cien Saude Colet 26:2529–2541. https://doi.org/10.1590/1413-81232021266.1.43532020
Malta DC, Stopa SR, Pereira CA, Szwarcwald CL, Oliveira M, Reis ACd (2017) Private health care coverage in the Brazilian population, according to the 2013 Brazilian National Health Survey. Cien Saude Colet 22(1):179–190
Mills A (2014) Health care systems in low- and middle-income countries. N Engl J Med 370(6):552–557. https://doi.org/10.1056/NEJMra1110897
Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, Lago M, Castro MC (2021) Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health 9(6):e782–e792. https://doi.org/10.1016/S2214-109X(21)00081-4
Ng JH, Hirsch JS, Wanchoo R, Sachdeva M, Sakhiya V, Hong S, Jhaveri KD, Fishbane S, Northwell C-RC, The Northwell Nephrology C-RC (2020) Outcomes of patients with end-stage kidney disease hospitalized with COVID-19. Kidney Int 98(6):1530–1539. https://doi.org/10.1016/j.kint.2020.07.030
Puchalska-Reglińska E, Dębska-Ślizień A, Biedunkiewicz B, Tylicki P, Polewska K, Jagodziński P, Rutkowski B, Gellert R, Tylicki L (2021) Extremely high mortality rates among hemodialysis patients with COVID-19 before the era of SARS-CoV-2 vaccination: results from a large database from the North of Poland. Pol Arch Intern Med 131(7–8):643–648
De Meester J, De Bacquer D, Naesens M, Meijers B, Couttenye MM, De Vriese AS, Group NKR (2021) Incidence, characteristics, and outcome of COVID-19 in adults on kidney replacement therapy: a regionwide registry study. J Am Soc Nephrol 32(2):385–396. https://doi.org/10.1681/ASN.2020060875
Chen C-Y, Shao S-C, Chen Y-T, Hsu C-K, Hsu H-J, Lee C-C, Sun C-Y, Chen Y-C, Hung M-J, Wu I-W (2021) Incidence and clinical impacts of COVID-19 infection in patients with hemodialysis: systematic review and meta-analysis of 396,062 hemodialysis patients. Healthcare 9(47):1–14
Bahat KA, Parmaksiz E, Sert S (2020) The clinical characteristics and course of COVID-19 in hemodialysis patients. Hemodial Int 24:534–540. https://doi.org/10.1111/hdi.12861
Seidel M, Hölzer B, Appel H, Babel N, Westhoff TH, Group TCDW (2020) Impact of renal disease and comorbidities on mortality in hemodialysis patients with COVID-19: a multicenter experience from Germany. J Nephrol 33:871–874. https://doi.org/10.1007/s40620-020-00828-8
Couchoud C, Bayer F, Ayav C, Béchade C, Brunet P, Chantrel F, Frimat L, Galland R, Hourmant M, Laurain E, Lobbedez T, Mercadal L, Moranne O (2020) Low incidence of SARS-CoV-2, risk factors of mortality and the course of illness in the French national cohort of dialysis patients. Kidney Int 98:1519–1529. https://doi.org/10.1016/j.kint.2020.07.042
Pio-Abreu A, Nascimento MMd, Vieira MA, Neves PDMdM, Lugon JR, Sesso R (2020) High mortality of CKD patients on hemodialysis with Covid-19 in Brazil. J Nephrol. https://doi.org/10.1007/s40620-020-00823-z
Girndt M, Sester M, Sester U, Kaul H, Kohler H (2001) Molecular aspects of T- and B-cell function in uremia. Kidney Int Suppl 78:S206-211. https://doi.org/10.1046/j.1523-1755.2001.59780206.x
Vaziri ND, Pahl MV, Crum A, Norris K (2012) Effect of uremia on structure and function of immune system. J Ren Nutr 22(1):149–156. https://doi.org/10.1053/j.jrn.2011.10.020
Thurlow JS, Joshi M, Yan G, Norris KC, Agodoa LY, Yuan CM, Nee R (2021) Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am J Nephrol 52(2):98–107. https://doi.org/10.1159/000514550
Bello AK, Okpechi IG, Osman MA, Cho Y, Htay H, Jha V, Wainstein M, Johnson DW (2022) Epidemiology of haemodialysis outcomes. Nat Rev Nephrol. https://doi.org/10.1038/s41581-022-00542-7
Gray NA, Dent H, McDonald SP (2012) Dialysis in public and private hospitals in Queensland. Intern Med J 42(8):887–893. https://doi.org/10.1111/j.1445-5994.2012.02795.x
Postorino M, Amato C, Mancini E, Carioni P, D’Arrigo G, Di Benedetto A, Cerino F, Marino C, Vilasi A, Tripepi G, Stuard S, Capasso G, Santoro A, Zoccali C, Calabrian ED, Transplantation Registries W (2018) A comparative study of the risk profile of hemodialysis patients in a for profit network and in two regional registries of the Italian Society of Nephrology. J Nephrol 31(1):119–127. https://doi.org/10.1007/s40620-016-0372-8
Raghavan R, Sheikh-Hamad D (2011) Descriptive analysis of undocumented residents with ESRD in a public hospital system. Dialysis Transplant 40(2):78–81
Arogundade FA, Omotoso BA, Adelakun A, Bamikefa T, Ezeugonwa R, Omosule B, Sanusi AA, Balogun RA (2020) Burden of end-stage renal disease in sub-Saharan Africa. Clin Nephrol 93(1):3–7
Marinovich S, Lavorato C, Rosa-Diez G, Bisigniano L, Fernández V, Hansen-Krogh D (2012) The lack of income is associated with reduced survival in chronic haemodialysis. Nefrologia 32(1):79–88
Conde KAP, Silva E, Silva CO, Ferreira E, Freitas FGR et al (2013) Differences in sepsis treatment and outcomes between public and private hospitals in Brazil: a multicenter observational study. PLoS ONE 8(6):e64790. https://doi.org/10.1371/journal.pone.0064790
Blumenthal D, Fowler EJ, Abrams M, Collins SR (2020) Covid-19—implications for the health care system. N Engl J Med 383(15):1483–1488. https://doi.org/10.1056/NEJMsb2021088
Soares M, Bozza FA, Angus DC, Japiassu´ AM, Viana WN, Costa R, Brauer L, Mazza BF, Correˆa TD, Nunes ALB, Lisboa T, Colombari F, Maciel AT, Azevedo LCP, Damasceno Ms, Fernandes HS, Cavalcanti AB, Brasil PEAAd, Kahn JM, Salluh JIF (2015) Organizational characteristics, outcomes, and resource use in 78 Brazilian intensive care units: the ORCHESTRA study. Intensive Care Med 41:2149-2160
Rodes CH, Dare JVL, de Araujo BC, Graciani L, Joao SMA, Germani A, Schmitt ACB (2021) The physiotherapy workforce in the Brazilian unified health care system. Hum Resour Health 19(1):101. https://doi.org/10.1186/s12960-021-00642-8
Acknowledgements
We are grateful to all Covid 19-HD Brazil investigators who contributed to this study (R.F. Manfrim, K.G. Santos, G.S. Ennes, O.D.F. Filho, M.C.A. Rios, T.L.V.Costa, J.D.S. Simões, R. Benvenutti, R.T. Belila, J.M.V. Obregón, S.M. Cunha, E.A.C.Neto, F. Araújo, A. Borborema, R.M. Gomes, A.P.H.R. Mesquita, M.M.M. Souto, M.X. Carrera, G.A.R. Neto, L.K.C. Batista, M.C.D.G. Gomes, F.S.G. Polacchini, A.L. C. Neto, A.F. Neto, R.H. Emeric, M.Z.P. Silveira, S.P. Melo, P.S. Teixeira, A.R. Salmeron, M.A.R. Tormes, F.C. Barcellos, N.F. Moreira, B. Meneghelli, A.L.F. Gouveia, L.R. Carneiro, L.F.B. Curti, C.A. Gomes, K.A. Alcântara, M.F.M. Sarro, H.N.C. Agra, M.T.I. Vannucchi, L.G.S. Oliviera, R. Rodrigues, S.M. Baltar, W.D. Silva, L.A. Miorin, A.K.C. D. Lopes, S.M. Oliveira, O.B. Junior, R.S. Humel, A. Watanabe, N. Gushi, E.A. Souza, M.A.C. Galvão, F.S. Fonseca, J.C. Guilhen, H.G. Neto, J.R.M. M. Carvalho, J.R.B. Junior, M.C. Jorge, N.Hoefelmann, S.A. Bobbio, R.R. Abrita, J. Pereira, M.E.P. Nardin, P. Sarturi, D.A. Bazhuni, E.A.L. Portioli, C.A.Caniello, P.H.Fraxino).
Funding
This study has been done without funding or support grants.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest in relation to the study performed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ricardo Sesso and Jocemir Ronaldo Lugon are both senior authors.
The members of the The Covid19-HD Brazil Investigators are listed in Acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
do Nascimento Lima, H., Nerbass, F.B., Neto, O.M.V. et al. Chronic hemodialysis patients with COVID-19 cared for by the public health system have higher mortality than those treated in private facilities: analysis of the Brazilian dialysis registry. Int Urol Nephrol 55, 449–458 (2023). https://doi.org/10.1007/s11255-022-03289-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03289-z