Abstract
Background
In autosomal dominant polycystic kidney disease (ADPKD) it is frequently found a reduction in urinary citrate of unknown origin. It has been suggested that it could be a marker of acid retention in chronic kidney disease. Our aim was to compare urinary citrate in ADPKD with other nephropathies and to show its relation with serum bicarbonate.
Methods
We determined urinary citrate in patients with several nephropathies and varied renal function. We included 291 patients, 119 with glomerular diseases, 116 with ADPKD, 21 with other nephropathies, and 35 patients with normal renal function.
Results
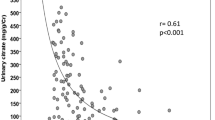
Urinary citrate was higher in women and in patients with normal renal function. ADPKD patients showed similar values of urinary citrate to patients with glomerular diseases and with other nephropathies. We observed a progressive reduction in urinary citrate with renal impairment, in a comparable way among patients with ADPKD and glomerular diseases. We did not observe a relationship with serum bicarbonate. Serum uric acid levels were significantly higher in patients with glomerular diseases than in ADPKD patients, even after correction with the degree of renal function.
Conclusions
Hypocitraturia is not specific of ADPKD but it is also present in all tested nephropathies and is related with renal impairment and not with serum bicarbonate. It could be interesting to study urinary citrate as a marker of renal function and as a prognostic factor.




Similar content being viewed by others
References
Nishiura JL, Neves RFCA, Eloi SRM, Cintra SMLF, Ajzen SA, Heilberg IP (2009) Evaluation of nephrolithiasis in autosomal dominant polycystic kidney disease patients. Clin J Am Soc Nephrol 4:838–844
Torres VE, Wilson DM, Hattery RR, Segura JW (1993) Renal stone disease in autosomal dominant polycystic kidney disease. Am J Kidney Dis 22(4):513–519
Torres VE, Erickson SB, Smith LH, Wilson DM, Hattery RR, Segura JW (1988) The association of nephrolithiasis and autosomal dominant polycystic kidney disease. Am J Kidney Dis 11(4):318–325
Ogborn MR, Sareen S, Prychitko J, Buist R, Peeling J (1997) Altered organic anion and osmolyte content and excretion in rat polycystic kidney disease: an NMR study. Am J Physiol 272:F63–F69
Borrego Utiel FJ, Herrera Contreras I, Merino García E, Camacho Reina MV, Moriana Domínguez C, Ocaña Pérez E (2021) Urinary citrate as a marker of renal function in patients with autosomal dominant polycystic kidney disease. Int Urol Nephrol. https://doi.org/10.1007/s11255-021-02953-0
Hamm LL (1990) Renal handling of citrate. Kidney Int 38:728–735
Baruch SB, Burich RL, Eun CK, King VF (1975) Renal metabolism of citrate. Med Clin N Am 59:569–582
Unwin RJ, Capasso G, Shirley DG (2004) An overview of divalent cation and citrate handling by the kidney. Nephrol Physiol 98:15–20
Hering-Smith KS, Mao W, Schiro FR, Coleman-Barnett J, Pajor AM, Hamm LL (2014) Localization of the calcium regulated citrate transport process in proximal tubule cells. Urolithiasis 42(3):209–2019
Mandel EI, Taylor EN, Curhan GC (2013) Dietary and lifestyle factors and medical conditions associated with urinary citrate excretion. Clin J Am Soc Nephrol 8(6):901–908
Zuckerman JM, Assimos DG (2009) Hypocitraturia: pathophysiology and medical management. Rev Urol 11(3):134–144
Forni Ogna V, Blanchard A, Vargas-Poussou R, Ogna A, Baron S, Bertocchio JP et al (2017) Signification of distal urinary acidification defects in hypocitraturic patients. PLoS ONE 12(5):e0177329. https://doi.org/10.1371/journal.pone.0177329
Sakhaee K, Alpern R, Jacobson HR, Pak CY (1991) Contrasting effects of various potassium salts on renal citrate excretion. J Clin Endocrinol Metab 72(2):396–400
Skolarikos A, Straub M, Knoll Th, Sarica K, Seitz Ch, Petrik A, Turk Ch (2015) Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. Eur Urol 67(4):750–763
Goraya N, Simoni J, Sager LN, Madias NE, Wesson DE (2019) Urine citrate excretion as a marker of acid retention in patients with chronic kidney disease without overt metabolic acidosis. Kidney Int 95(5):1190–1196
Marangella M, Vitale C, Manganaro M, Cosseddu D, Martini C, Petrarulo M, Linari F (1991) Renal handling of citrate in chronic renal insufficiency. Nephron 57(4):439–443
Moellering H, Gruber W (1966) Determination of citrate with citrate lyase. Anal Biochem 17(3):369–376
Martinez CA, Górriz JL, Bover J, de la Segura MJ, Cebollada J, Escalada J, Esmatjes E, Fácila L et al (2014) Documento de consenso para la detección y manejo de la enfermedad renal crónica. Nefrologia 34(2):243–262
Torres VE, Keith DS, Offord KP, Kon SP, Wilson DM (1994) Renal ammonia in autosomal dominant polycystic kidney disease. Kidney Int 45:1745–1753
Fabris A, Lupo A, Bernich P, Abaterusso C, Marchionna N, Nouvenne A, Gambaro G (2010) Long-term treatment with potassium citrate and renal stones in medullary sponge kidney. Clin J Am Soc Nephrol 5(9):1663–1668
Goraya N, Simoni J, Sager LN, Mamun A, Madias NE, Wesson DE (2019) Urine citrate excretion identifies changes in acid retention as eGFR declines in patients with chronic kidney disease. Am J Renal Physiol. https://doi.org/10.1152/ajprenal.00044.2019
Han M, Park HC, Kim H, Jo HA, Huh H, Jang JY et al (2014) Hyperuricemia and deterioration of renal function in autosomal dominant polycystic kidney disease. BMC Nephrol 15:63. https://doi.org/10.1186/1471-2369-15-63
Helal I, McFann K, Reed B, Yan X, Schrier RW, Fick-Brosnahan GM (2013) Serum uric acid, kidney volume and progression in autosomal-dominant polycystic kidney disease. Nephrol Dial Transpl 28:380–385
Torres-Sánchez MJ, Ávila-Barranco E, de la Esteban RRJ, Fernández-Castillo R, Esteban MA, Carrero JJ, García-Valverde M, Bravo-Soto JA, en representación del Grupo para el Estudio de la Enfermedad Poliquística Autosómica Dominante (GEEPAD) (2016) Relación entre función y volumen renal en lapoliquistosis renal autosómica dominante: estudio transversal. Rev Clin Esp 216(2):62–67
Kaehny WD, Tangel DJ, Johnson AM, Kimberling WJ, Schrier RW, Gabow PA (1990) Uric acid handling in autosomal dominant polycystic kidney disease with normal filtration rates. Am J Med 89(1):49–52
Helal I, Reed B, McFann K, Yan XD, Fick-Brosnahan GM, Cadnapaphornchai M, Schrier RW (2011) Glomerular hyperfiltration and renal progression in children with autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol 6(10):2439–2443
Nashar K, Fried LF (2012) Hyperuricemia and the progression of chronic kidney disease: is uric acid a marker or an independent risk factor? Adv Chronic Kidney Dis 19(6):386–391
Bose B, Badve SV, Hiremath SS, Boudville N, Brown FG, Cass A et al (2014) Effects of uric acid-lowering therapy on renal outcomes: a systematic review and meta-analysis. Nephrol Dial Transpl 29:406–441
Johnson RJ, Nakagawa T, Jalal D, Sanchez-Lozada LG, Kang DH, Ritz E (2013) Uric acid and chronic kidney disease: which is chasing which? Nephrol Dial Transpl 28(9):2221–2228
Caliskan Y, Ozluk Y, Celik D, Oztop N, Aksoy A, Ucar AS, Yazici H, Kilicaslan I, Sever MS (2016) The clinical significance of uric acid and complement activation in the progression of IgA nephropathy. Kidney Blood Press Res 41(2):148–157
Myllymäki J, Honkanen T, Syrjänen J, Helin H, Rantala I, Pasternack A, Mustonen J (2005) Uric acid correlates with the severity of histopathological parameters in IgA nephropathy. Nephrol Dial Transpl 20(1):89–95
Ruan Y, Hong F, Wu J, Lin M, Wang C, Lian F, Cao F, Yang G, Gao M (2018) Clinicopathological characteristics, role of immunosuppressive therapy and progression in IgA nephropathy with hyperuricemia. Kidney Blood Press Res 43(4):1131–1140
Moriyama T, Itabashi M, Takei T, Kataoka H, Sato M, Shimizu A, Iwabuchi Y, Nishida M, Uchida K, Nitta K (2015) High uric acid level is a risk factor for progression of IgA nephropathy with chronic kidney disease stage G3a. J Nephrol 28(4):451–456
Author information
Authors and Affiliations
Contributions
Research idea and study design: FJBU; data acquisition: FJBU, IHC, EMG, CMD, MJGC; data analysis/interpretation: FJBU, IHC, EOP; statistical analysis: FJBU. Each author contributed important intellectual content during manuscript drafting or revision. All authors aproved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest to declare. We have not received any financial support for this research. We declare that the results presented in this paper have not been published previously in whole or part, except in abstract format.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Borrego Utiel, F., Herrera Contreras, I., Merino García, E. et al. Hypocitraturia is present when renal function is impaired in diverse nephropathies and is not related with serum bicarbonate levels. Int Urol Nephrol 54, 1261–1269 (2022). https://doi.org/10.1007/s11255-021-02992-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02992-7