Abstract
Purpose
An outbreak of a novel respiratory disease due to coronavirus species was emerged in 2019 and named as Coronavirus Disease-2019 (COVID-19). Clinical and immunological factors affecting the course of COVID-19 in kidney transplant recipients (KTR) are not well-known.
Methods
In this prospective observational study, we presented 20 KTR with COVID-19 pnemonia and examined the factors predicting the severity of COVID-19. A total of 10 KTR without COVID-19 was used as control group. Lymphocyte subsets were determined by flow cytometry. In 13/20 patients, immunophenotyping was repeated 1 week later.
Results
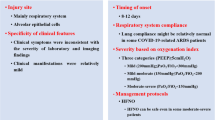
Mean age of the patients was 50 ± 9 years. Patients were classified as mild–moderate (oxygen saturation: SO2 > 90%) and severe disease groups (SO2 ≤ 90%). Serum albumin and hemoglobin were lower and CRP, fibrinogen and peak d-dimer were higher in severe group. Peak CRP was inversely associated with nadir SO2 (r = − 0.68, p = 0.001). Neutrophil/lymphocyte ratio was higher in severe group (p = 0.01). CD3 + and CD4 + cells were lower and NK cell percentage (CD16 + 56 +) was higher in severe group. Percentage of spontaneously activated CD8 cells (CD8 + CD69 +) was higher in severe group. In comparison of KTR with and without COVID-19, CD8 + cells were lower but NK cell percentage was higher in KTR with COVID-19.
Conclusion
In this pilot study, increased NK cells, activated CD8 + cells and decreased CD3 + and CD4 + cells were associated with severity of COVID-19 in KTR. Peripheral immunophenotyping of lymphocyte subtypes may provide prognostic information about the clinical course of COVID-19 in KTR.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An outbreak of a novel respiratory disease due to coronavirus species has been described in China in December 2019. This virus was named as “severe acute respiratory syndrome coronavirus-2” (SARS-CoV-2) and associated disease was named as Coronavirus Disease 2019 (COVID-19) [1, 2]. COVID-19 spreaded rapidly worldwide and on March 2020, World Health Organization (WHO) declared this viral outbreak as pandemic. COVID-19 caused high rates of hospitalization and intensive care unit (ICU) admissions overwhelming the healthcare systems of the most countries [3].
Kidney transplant recipients (KTR) receive immunosuppressive treatment to prevent rejection. The possible effects of immunosuppression on this novel virus and the disease course of COVID-19 in KTR are currently not well-known. In this study, we present the clinical course of 20 KTR with COVID-19 pneumonia and examined the immunological factors predicting the severity of COVID-19.
Materials and methods
In this prospective observational study, 20 KTR with COVID-19 pneumonia were enrolled from two transplant centers of Memorial Healthcare group (Memorial Şişli and Memorial Hizmet Hospitals). Baseline demographic data were presented in (Tables 1, 2). Mean age of the patients was 50 ± 9 years and most of the patients were male (15/20: 75%). Median transplantation duration was 75 (30–112) months. All patients had living-donor transplantation.
Primary cause of end-stage renal disease were as follows: diabetes mellitus (DM) in three patients (15%), glomerulonephritis in seven patients (10%), amyloidosis in two patients (10%), hypertension in two patient (10%), autosomal dominant polycystic kidney disease in one patient (5%), retroperitoneal fibrosis in one patient (5%), and unknown in nine patients (45%). Most patients (85%) had comorbid diseases. Comorbid diseases were as follows: hypertension (10; 50%), ischemic heart disease (6; 30%), diabetes mellitus (3; 15%), chronic obstructive pulmonary disease (COPD) (2; 10%), ankylosing spondylitis (2;10%), amyloidosis (2;10%), cerebrovascular accident (1; 5%), Hodgkin lymphoma (1; 5%), gout (2; 10%) and Behçet’s disease (1; 5%).
Symptoms of the patients at admission to hospital were as follows: cough (18; 90%), fever (14; 70%), dyspnea (6; 30%), fatigue (5; 25%), diarrhea (3; 15%) and anosmia (1; 5%). All of the patients were hospitalized. Demographic, clinical and biochemical data were recorded. COVID-19 treatments and modification of immunosuppressive drugs were also recorded.
Biochemical tests
Biochemical analyses such as creatinine, C-reactive protein (CRP), procalcitonin, d-dimer, fibrinogen, complete blood count were performed several times during the follow-up of patients. Peak and nadir values of these tests were determined and analyzed.
Baseline and modification of immunosuppressive treatments
Baseline maintenance immunosuppressive treatment was composed of tacrolimus (TAC) + mycophenolate mofetil (MMF) + deltacortril (DC) in 11 patients (55%), TAC + mycopenolic acid (MPA) + DC in seven patients (35%), cyclosporine (CSA) + MPA + DC in one patient (5%) and MMF + DC in one patient (5%). At admission to hospital, anti-metabolite treatments (MMF/MPA) were withdrawn from all patients. Prednisolone dose was doubled and patients received 10 mg of prednisolone. Blood TAC and CSA levels were measured every day and doses of these drugs were reduced to keep the target blood trough levels at 5–7 ng/mL for TAC and 50–75 ng/mL for CSA.
Diagnosis of COVID-19
SARS-CoV-2 real time reverse transcription polymerase chain reaction (RT-PCR) test of naso/oropharyngeal samples and thorax computed tomography have been performed to all patients. The diagnosis of COVID-19 pneumonia has been established based on [1] PCR positivity for SARS-CoV-2 (Covid-19 RT-qPCR Wuhan- RdRp- Qiagen Rotorgene RT-PCR) and [2] typical thorax CT and clinical findings. Out of 20 patients, 13 patients were SARS-CoV-2-RT-PCR positive. Diagnosis of COVID-19 was established in seven patients based on typical thorax CT and clinical findings. All of the patients had SARS-CoV-2 pneumonia. Radiological features of the pneumonia were presented in Table 1.
Definition of mild–moderate and severe patient groups
Patients were grouped as severe (oxygen saturation ≤ 90%, n:10) and mild–moderate COVID-19 pneumonia (oxygen saturation > 90%, n:10) according to the nadir oxygen saturation at room air during the course of the disease [4].
Treatment of COVID-19
All patients received hydroxychloroquine (HCQ) (loading dose: 2 × 400 mg, maintenance dose: 2 × 200 mg) and most patients (n:13,%65) received azithromycin (2 × 250 mg). Since HCQ, azithromycin and calcineurin inhibitors are known to prolong QT interval, ECG was performed to all patients on admission to hospital and ECG was checked every 3 days. In case of a prolongation of corrected QT (> 500 ms), HCQ and azithromycin were withdrawn. Treatments were established according to COVID-19 protocols of the Turkish Ministry of Health including HCQ and antiviral drugs, namely LPV/rv and favipravir. Accordingly, first choice of antiviral treatment was usually LPV/rv (200/50 mg tb, 2 × 2 tab/day). If the patients did not respond to treatment with LPV/r and O2 saturation dropped below 90%, favipravir (loading dose: 2 × 1600 mg, maintenance dose: 2 × 600 mg) was started. Two patients received convalescent immune plasma.
All patients received antibiotics (ceftriaxone 2 g/day for 5 days) to prevent and treat bacterial super-infection. All patients also received low-molecular weight heparin (enoxaparin) in prophylactic doses. Two patients were already on warfarin treatment because of their comorbid diseases.
Other treatments
A total of six patients (30%) was on angiotensin converting enzyme inhibitor (ACEI) and angiotensin receptor blocker (ARB) treatments. Five patients were on ramipril and one patient was on losartan treatments. Four patients were on colchicine treatment indicated by their comorbid diseases such as AA amyloidosis and gout. Colchicine treatment was continued during the hospitalization period.
Definition of acute kidney injury (AKI)
AKI was defined by the following criteria determined by KDIGO guidelines: increase in serum creatinine ≥ 0.3 mg/dL or increase in serum creatinine more than 1.5 times from the baseline creatinine levels [5].
Isolation of white blood cells and immunophenotyping
Peripheral blood white blood cells (WBC) of all participants were isolated from their hemogram tubes with EDTA taken for their routine tests by using erythrocyte lysing solution (155 mM NH4Cl; 10 mM KHCO3; 0,1 mM EDTA; pH:7.3). The following fluorochrome labeled monoclonal antibodies (mAb) and isotype-matched controls were used for two–three color phenotypic analysis: anti-IgG1, anti-IgG2a, anti-CD45, anti-CD3; anti-CD4; anti-CD8; anti-CD16; anti-CD56; anti-CD19; anti-HLA-DR; anti-CD69, (Becton&Dickinson Corp, San Jose, CA, USA). Cells were acquired and analyzed using CellQuest software on a FACS scan flow cytometer (Becton Dickinson Inc, San Jose, CA, USA). Lymphocytes were gated according to their forward and side scatter characteristics and their specific CD markers. Markers were evaluated as percentages. In 13 of 20 patients, peripheral lymphocyte subset analysis was repeated 1 week later. A total of 10 KTR without COVID-19 was used as control group.
Statistical analysis
Continuous variables were presented as mean ± SD or median-IQR. Mann–Whitney U test was used to compare non-parametric data. Normality of distribution was tested by Shapiro–Wilk test. Normally distributed parameters were compared using Student’s t test. χ2 test was used for categorical variables. Paired samples T test and Wilcoxon-signed ranks tests were used to compare repeated parameters. Statistical significance was defined as p < 0.05. Statistical analyses were performed by SPSS (ver 16.0).
The study was approved by Marmara University Ethics Committee (No: 08.05.2020/09.2020.541). Informed consent was obtained from all participants before the study.
Results
Baseline demographic and clinical parameters were presented in Table 1. Accordingly, mean O2 saturation at room air was 92 ± 3% at admission to hospital and 97 ± 2% at discharge from the hospital. Mean nadir O2 saturation during follow-up was 89 ± 8%. During follow-up of patients, none of the patients died. Only two patients were admitted to ICU and one of these patients was intubated who had a previous history of COPD. Comparison of mild–moderate and severe COVID-19 patients was presented in Table 2. Accordingly, age and transplantation vintage were not different between the groups. Hospitalization duration was found to be significantly higher in severe COVID-19 group as expected. Serum albumin, hemoglobin and lymphocyte levels were significantly lower in severe COVID-19 group compared to mild group. Serum CRP, fibrinogen and peak D-dimer levels were significantly higher in severe COVID-19 group. Furthermore, peak serum CRP levels were significantly inversely associated with nadir SO2 levels (r = − 0.68, p = 0.001) (Fig. 1). Also serum CRP level at admission was significantly associated with the initial S02 (r = − 0.50, p = 0.022).
Male patients were significantly younger than female patients (48 ± 8 vs. 58 ± 7 years, p = 0.019). Disease severity was observed to be similar in gender groups (severe COVID-19 frequency 53% in males, 40% in females, p = 0.60).
A total of four patients were on colchicium for the treatmentof AA amylodiosis and gout. Baseline and maximum serum CRP levels were not different between patients with and without colchicum treatment [56 (9–143) vs. 45 (16–75), p = 0.73 and 84 (13–154) vs. 76 (26–173), p = 0.66, respectively]. Oxygen saturations were similar between the groups. Two out of four patients on colchicum treatment had severe COVID-19 (50%) compared to 8/16 patients in non-colchicum group (50%).
Although blood tacrolimus trough levels were closely followed up and reduction or temporary cessation of tacrolimus treatments were performed, blood tacrolimus levels were significantly higher in patients on LPV/rv treatment [9.6 (8.22–21.31) vs. 6.1 (4.85–8.42), p = 0.008].
Patients with ACEI/ARB treatment were less likely to have severe COVID-19 (1/6, 16%) compared to patients without ACEI/ARB treatment (9/14, 64%) (likelihood ratio = 0.04). Time on transplantation (115 (99–136) vs. 54 (11–84) months, p = 0.009) and lymphocyte counts at admission (1515 (1140–1787) vs. 525 (475–755)/µL, p = 0.001) and nadir lymphocyte counts (1170 (1087–1487 vs. 461 (285–537)/µL, p = 0.0001) were found to be significantly higher in ACEI/ARB groups. Furthermore CRP at admission [19.5 (4.72–32.37) vs. 67.5 (35.25–105) mg/L, p = 0.012] and peak CRP levels [26.25 (10.42–47.47) vs. 144 (64.5–184.5) mg/L, p = 0.012] were significantly lower in patients on ACEI/ARB treatment.
AKI developed in five patients (25%) during the course of hospitalization. Peak serum CRP [71 (19–168) vs. 82 (26–165) mg/L, p = 0.86] and nadir lymphocyte counts [500 (381–885) vs. 520 (350–1170) /µL, p = 0.73] were not different between the patients with and without AKI. Median blood tacrolimus levels were also not different between these two groups [8.45 (2.7–8.7) vs. 8.5 (5.95–12.3) ng/mL, p = 0.37]. AKI was observed in three of 10 patients with severe COVID-19 (30%), meanwhile AKI developed in two of ten patients with mild COVID-19 (20%). AKI seemed not to be related to severity of COVID-19. ACEI/ARB use was also not associated with AKI; AKI occurred in only one patient using ACEI/ARB (16%), and in four patients not using these drugs (28%) (Chi-squared p value: 0.57). Serum creatinine levels returned to basal values in all these patients at the end of the follow-up period (1.66 ± 0.65 vs. 1.64 ± 0.57, p = 0.91). Since all patients recovered in terms of kidney function, kidney biopsy was not performed to determine the cause of AKI.
New-onset proteinuria occurred in seven patients (35%) during the course of the disease. Five of the patients (71%) with new-onset proteinuria had severe COVID-19, however, no significant relationship could be found between new-onset proteinuria and severity of COVID-19 (Chi-squared p value = 0.13). No association was present between patients with AKI and new-onset proteinuria; only one patient with AKI has new-onset proteinuria and only one patient with new-onset proteinuria had AKI during the follow-up. In five of the seven patients (71%), proteinuria disappeared after the recovery.
Immunophenotyping and lymphocyte subsets
Comparison of lymphocyte subsets between severe and mild–moderate COVID-19 groups was presented in Table 3. Accordingly, in severe COVID-19 group, lymphocyte ratio was found to be lower and granulocyte ratio was higher compared to mild–moderate COVID-19 group. Neutrophil/lymphocyte ratio was also higher in KTR with severe COVID-19 pneumonia compared to mild–moderate group (p = 0.01). CD3 + cell percentage was significantly lower. NK cell percentage (CD16 + 56 +) was found to be higher in severe COVID-19 group (Fig. 2). CD4 + cell percentages were lower in severe COVID-19 group compared to mild–moderated COVID-19 group. Although CD8 + cell percentages were similar between the groups, percentage of spontaneously activated CD8 cells (CD8 + CD69 +) was significantly higher in severe COVID-19 group (Fig. 3a). Spontaneously activated CD4 cell percentage (CD4 + CD69 +) tended to be higher in severe group (p = 0.06) (Fig. 3b).
We also examined the change of lymphocyte subsets at baseline and 1 week after the admission (Table 4). Accordingly, CD4 + CD69 + and CD8 + CD69 + cell percentages were observed to significantly decrease during the COVID-19 course. NK cell percentage (CD16 + 56 +) had tendency to decrease (from 20.67 ± 12.21 to 12.32 ± 5.49%, p = 0.08).
Comparison of immunophenotyping parameters between KTR with and without COVID-19 pneumonia was presented in Table 5. CD8 + cell percentage was significantly lower but NK cell percentage was significantly higher in KTR patients with COVID-19. CD3 + cell percentage tended to be lower in KTR patients with COVID-19.
Discussion
In this study, we present the clinical course of 20 KTR with COVID-19 pneumonia and examined the immunological factors predicting the severity of COVID-19. In contrary to several reports from US, Italy and Spain for KTR, outcome of our patients was relatively good with no loss of patients. In China, in general population, overall case fatality rate was reported to be around 1.4–2%. However, it may be lower as less than 1% in the absence of comorbidities [6, 7]. The presence of comorbidities such as hypertension, diabetes, coronary heart disease was associated with a higher risk of death [8]. Immunosuppression due to transplantation was a feared condition which was thought to cause very high rates of mortality which was extrapolated from the clinical experiences from other known viral infections in this patient population. In a study from Spain, in solid organ transplantation, case fatality rate of COVID-19 was 27% [9]. In a case-series from US, which included 15 KRT patients with COVID-19, four patients (27%) needed intubation and mechanical ventilation and two patients died due to ARDS [10]. In another study from US, 36 KTR with COVID-19 was included. A total of 11 patients (39%) needed mechanical ventilation and 10 patients died (28%) [11]. In a case series form Italy which included 20 KTR with COVID-19, five patients died (25%) [12]. In these previous case series of KTR with COVID-19, patients were significantly older than our patients. For example, median age of case series from Spain was 71 ± 12 years [9]. Furthermore, deceased patients in these studies were even more older; mean ages of deceased patients were 74 ± 5, 74 ± 4 and 64 ± 6 years, respectively [9, 10, 12]. In our study, mean age of our patients was 50 ± 9 and our oldest patient was 64 years of age. We thought that main reason of the difference of outcomes between the studies might be the younger age of our patients. Other possible explanations of why our patients had more favorable outcomes compared to literature might be genetic differences in immune system and different vaccination policies in countries such as BCG vaccination which might decrease the COVID-19-associated morbidity and mortality by the way of trained immunity [13, 14].
Lymphopenia and neutrophilia are common manifestations of COVID-19 which was observed in up to 63% of patients in general population [15]. They have been found to be associated with the severity of COVID-19 pneumonia [16]. Neutrophil–lymphocyte ratio (NLR) may be a better combined indicator of the disease severity. In a study by Liu et al., patients with NLR ≥ 3.13 were found to be associated with severe illness and the need for ICU admission [17]. In consistent with the literature, in the present study, lymphocyte count was lower and granulocyte count was higher in severe COVID-19 group compared to mild–moderate COVID-19 group. Thus NLR was also significantly higher in severe COVID-19 pneumonia in parallel to previous reports.
Universal response to viral infections includes the activation of both innate (NK cells) and adaptive immunity (CD4 + and CD8 + T cells) [18]. Thus immune profile seems to be directly associated with the outcome of patients with COVID-19. We examined and compared the immunophenotyping profiles of KTR with mild–moderate and severe COVID-19 pneumonia. Furthermore, we also investigated the differences of lymphocyte subsets in KTR with and without COVID-19 pneumonia. In the context of COVID-19 disease, T cell profile was investigated in a few studies. In most of the studies performed in patients with COVID-19 in non-transplant population, a marked reduction of CD4 + cells and CD8 + cells was observed [19, 20]. In a study by Li et al. [21], deceased COVID-19 patients had lower CD3 + , CD4 + , and CD8 + T cells. In another study, CD3 + and CD4 + T cell percentages were found to be significantly lower in severe COVID-19 patients compared to mild patients [22]. Studies that examined T cell subsets in transplant patients are even more scarce. In a case report, immunophenotyping was performed in two transplant patients (a KTR and bone marrow transplant recipient) and it showed low counts of T cells [23]. In a case series from US, 79% of patients had lymphopenia, 68% had low CD3 cell counts, 71% had low CD4 cell counts, and 29% had low CD8 cell counts [11]. In consistent with these results in the literature, CD8 + cell percentage was significantly lower in KTR with COVID-19 pneumonia compared to KTR without COVID-19 in our study. Furthermore, CD3 + and CD8 cell percentage were found to be significantly lower in severe COVID-19 group as compared to mild/moderate disease. CD4 + cell percentage tended to be lower in severe COVID-19 group. One of the most important proposed mechanism responsible for reduction of T lymphocytes is initial hyperfunctioning of lymphocytes with subsequent exhaustion and senescence of these cells [24]. Although T cells are decreased, their expression of activation markers such as CD69, CD38, CD44, and HLA-DR are reported to be increased [25]. Furthermore, degree of activation may be an indicator of severity of the COVID-19. In a study, activation markers such as HLA-DR and CD45RO on CD4 + and CD8 + T cells were found to be higher in severe patients compared with mild patients [22]. Importantly, in our study, we studied the activation marker, CD69 on T cells. Spontaneously activated CD8 cells namely CD8 + CD69 + cell percentage were significantly higher in severe COVID-19 group. Also, spontaneously activated CD4 cell percentage (CD4 + CD69 +) tended to be higher in severe group (p = 0.06). Furthermore, activation of CD4 + and CD8 + cells (CD4 + CD69 + and CD8 + CD69 +) was decreased within 1 week in course of COVID-19. These findings may support the hypothesis of activation induced T cell apoptosis and exhaustion. HLA-DR expression is known to be another activation marker of T cells. In a study, there was no significant difference in activated total T cells (CD3 + HLADR +) and activated cytotoxic T cells (CD3 + CD8 + HLA − DR +) in mild and severe COVID-19 patients [26]. Similar to this study, we also found no difference in terms of CD3 + HLA-DR + between mild–moderate and severe group. Furthermore, CD3 + HLA-DR + cell percentage did not change during the course of disease.
NK cells are the most important cells of the immune system during acute viral infections [27]. However there are controversial findings in literature about the NK-cell levels during the course of COVID-19. In several studies, NK cells were reported to be reduced in COVID-19 patients, and furthermore, low NK cell counts were associated with the severity of the disease [28,29,30]. Similarly, in a study that made a single-cell atlas of the peripheral immune response in non-transplant patients with severe COVID-19, NK cells were found to be depleted [31]. However in analysis of BALF transcriptome, NK cells were found to be increased in COVID-19 patients, compared to healthy controls [32]. Similarly, in another study, NK cell percentages increased in severe COVID-19 patients [22]. In consistent with these results, NK cell percentages (CD16 + 56 +) were found to be higher in severe COVID-19 group compared to mild–moderate group in our study. When we compare KTR with or without COVID-19, we observed that NK cell percentage was increased in KTR patients with COVID-19 pneumonia. Increased NK-cells in KTR patients with COVID-19 may suggest that a similar pattern of NK-cell response to viral infections in general population is valid for also KTR with COVID-19.
Exaggerated inflammatory response and cytokine storm seem to be the most important factors in severe COVID-19 patients leading to high mortality rates. In our study, serum CRP levels were found to be directly associated with the severity of COVID-19. Peak serum CRP levels were also significantly inversely associated with the nadir SO2 levels suggesting a direct role of inflammation in the pathophysiology of respiratory failure.
Optimal modification of maintenance immunosuppressive treatments of KTR during the course of COVID-19 is not well-known and there is no consensus on this topic. In everyday clinical practice, during the treatment of severe opportunistic infections, a reduction or discontinuation of immunosuppressive treatment is a common strategy which is frequently associated with faster recovery [33, 34]. In our clinics, antimetabolites (MMF/MPA) were withdrawn from all KTR, prednisolone dose was doubled and CNI doses were reduced. However, these modifications vary between the clinics. Similar modifications in parallel to our adjustments have been described in the literature [10]. In some guidelines, total withdrawal of CNIs was recommended in severe COVID-19 patients [35]. However, an analysis of protein–protein interactions between SARS-CoV and human proteins showed that cyclophilin molecules and FK506-binding proteins interacted with SARS-CoV proteins [36]. Furthermore, in in-vitro studies, tacrolimus was demonstrated to decrease SARS-CoV replication which suggested that CNIs might have inhibitory effects on SARS-CoV-2 replication [37]. Therefore, continuing CNIs might be useful in KTR with COVID-19 infection. Increased inflammation is known to be associated with COVID-19 associated mortality. Abrupt and major decline in immunosuppressive treatments may result in exacerbation of inflammatory responses and poor clinical outcomes [38]. Another concern in reduction of immunosuppressive treatment is the risk of acute rejection. Impaired graft function is a comorbidity which can lead to poor outcomes in KTR with COVID-19. For that reason, we recommend continuing CNI treatment in reduced doses in KTR with mild/moderate COVID-19 in early stages.
AKI is an important complication of COVID-19 infections which causes increased mortality rates. In general population, AKI was reported to occur with a frequency of 0.5% to 15% during the course of COVID-19. In critically ill patients with COVID-19, rate of AKI increased up to 29% [6, 39]. In a case series from UK, AKI was reported to occur at a rate of 57% in KTR with COVID-19 [40]. In another case series from US, AKI frequency was reported to be 40% during the course of COVID-19 [10]. Etiology of AKI may be various including direct viral effects on kidneys as well as CNI overdose, sepsis, increased inflammation, cytokine storm, hypotension and acute rejection [10, 41]. In our study, AKI developed in five patients (25%) during the course of hospitalization, however, all patients recovered to baseline renal functions at the end of the follow-up period. Furthermore, AKI was not found to be related to the severity of COVID-19. ACEI/ARB use and blood tacrolimus levels were not associated with AKI.
Innate immunity is the first line of defense against viral infections. A component of SARS-CoV, namely Viroporin E is known to activate the NLRP3 inflammasome [42]. Colchicine blocks NLRP3 inflammasome assembly leading to decreased cytokine secretion including IL-1b and IL-6 [43]. In a clinical observation from Italy, colchicine was started to a KTR with severe COVID-19. During follow-up, plasma IL-6 levels decreased and respiratory parameters improved. In another KTR patient, colchicine decreased plasma IL-6 levels promptly. We continued colchicine treatment in four patients during the hospitalization period. There was no difference in inflammation parameters (serum CRP) and oxygen saturations in patients receiving colchicum compared to patients who were not on colchicum. Further studies investigating the effectivity of colchicine in COVID-19 are needed.
Relatively small sample size may be regarded as a limitation of this study.
In this pilot study, we presented clinical features and lymphocyte profiles of 20 KTR with COVID-19 pneumonia. Increased CRP, neutrophil/lymphocyte ratio, d-dimer and fibrinogen levels were associated with severe COVID-19 pneumonia. Furthermore, increased percentage of NK cell and spontaneously activated CD8 + cell (CD8 + CD69 +) and decreased percentage of CD3 + and CD4 + cells predicted the severity of the disease. Peripheral immunophenotyping of lymphocyte subtypes may provide prognostic information about the clinical course of COVID-19 in KTR.
Availability of data and material
Data may be provided on request from the corresponding author.
Code availability
Not applicable.
References
Coronavirus disease 2019. https://who.int/emergencies/diseases/novel-coronavirus-2019. (Accessed 3 Aug 2020)
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. https://doi.org/10.1001/jama.2020.2648
Grasselli G, Pesenti A, Cecconi M (2020) Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. https://doi.org/10.1001/jama.2020.4031
https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1. (Accessed 11 May 2021)
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int 2(Suppl 1):138
Guan WJ, Ni ZY, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. https://doi.org/10.1056/NEJMoa2002032
Li Q, Guan X, Wu P et al (2020) Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. https://doi.org/10.1056/NEJMoa2001316
Zhou F, Yu T, Du R et al (2020) Clinical course and risk factors formortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054–1062
Fernández-Ruiz M, Andrés A, Loinaz C et al (2020) COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant 20(7):1849–1858
Columbia University Kidney Transplant Program (2020) Early description of coronavirus 2019 disease in kidney transplant recipients in New York. J Am Soc Nephrol 31(6):1150–1156
Akalin E, Azzi Y, Bartash R et al (2020) Covid-19 and kidney transplantation. N Engl J Med 382(25):2475–2477
Alberici F, Delbarba E, Manenti C et al (2020) A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int 97(6):1083–1088
Ozdemir C, Kucuksezer UC, Tamay Z (2020) Is BCG vaccination effecting the spread and severity of COVID-19. Allergy 75:1815–1819
Gursel M, Gursel I (2020) Is global BCG vaccination-induced trained immunity relevant to the progression of the SARS-CoV-2 pandemic? Allergy 75:1815–1819
Naicker S, Yang CW, Hwang SJ et al (2020) The novel coronavirus 2019 epidemic and kidneys. Kidney Int 97(5):824–828
Wu F, Zhao S, Yu B et al (2020) A new coronavirus associated with human respiratory disease in China. Nature 579:265–269
Liu J, Liu Y, Xiang P et al (2020) Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J Transl Med 18:206
Jung MC, Pape GR (2002) Immunology of hepatitis B infection. Lancet Infect Dis 2:43–50
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395:497–506
Xu Z, Shi L, Wang Y et al (2020) Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 8:420–422
Li D, Chen Y, Liu H et al (2020) Immune dysfunction leads to mortality and organ injury in patients with COVID-19 in China: insights from ERS-COVID-19 study. Signal Transduct Target Ther 5:62
Wang F, Hou H, Luo Y et al (2020) The laboratory tests and host immunity of COVID-19 patients with different severity of illness. JCI Insight 5(10):e137799
Huang J, Lin H, Wu Y et al (2020) COVID-19 in posttransplant patients—report of 2 cases. Am J Transplant 20(7):1879–1881
McLane LM, Abdel-Hakeem MS, Wherry EJ (2019) CD8 T cell exhaustion during chronic viral infection and cancer. Annu Rev Immunol 37:457–495
Zhou Y, Fu B, Zheng X et al (2020) Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl Sci Rev. https://doi.org/10.1093/nsr/nwaa041
Qin C, Zhou L, Hu Z et al (2020) Dysregulation of immune response in patients with COVID-19 in Wuhan China. Clin Infect Dis 71(15):762–768
Marquardt N, Ivarsson MA, Blom K et al (2015) The human NK cell response to yellow fever virus 17D is primarily governed by nk cell differentiation independently of NK cell education. J Immunol 195(7):3262–3272
Song CY, Xu J, He J et al (2020) COVID-19 early warning score: a multi-parameter screening tool to identify highly suspected patients. medrXiv. https://doi.org/10.1101/2020.03.05.20031906
Yu L, Tong Y, Shen G et al (2020) Immunodepletion with hypoxemia: a potential high risk subtype of coronavirus disease 2019. medrXiv. https://doi.org/10.1101/2020.03.03.20030650
Zheng M, Gao Y, Wang G et al (2020) Functional exhaustion of antiviral lymphocytes in COVID-19 patients. Cell Mol Immunol 17:533–535
Wilk AJ, Rustagi A, Zhao NQ et al (2020) A single-cell atlas of the peripheral immune response in patients with severe COVID-19. Nat Med 26(7):1070–1076
Liao M, Liu Y, Yuan J et al (2020) The landscape of lung bronchoalveolar immune cells in COVID-19 revealed by single cell RNA sequencing. medrXiv. https://doi.org/10.1101/2020.02.23.20026690
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group (2009) KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant 9(Suppl 3):S1–S155
Kumar D, Michaels MG, Morris MI et al (2010) Outcomes from pandemic influenza A H1N1 infection in recipients of solid-organ transplants: a multicentre cohort study. Lancet Infect Dis 10(8):521–526
DESCARTES expert opinion regarding the management of immunosuppressive medication forkidney transplant patients during the COVID-19 pandemic. European Renal Association – European Dialysis and Transplant Association, 2020. https://era-edta.org/en/wp-content/uploads/2020/04/Expert-opinion-on-ISD-in-Covid-19.pdf. (Accessed 3 Aug 2020)
Pfefferle S, Schöpf J, Kögl M et al (2011) The SARS-coronavirus-host interactome: identification of cyclophilins as target for pan-coronavirus inhibitors. PLoS Pathog 7:e1002331
Carbajo-Lozoya J, Müller MA, Kallies S et al (2012) Replication of human coronaviruses SARS-CoV, HCoVNL63 and HCoV-229E is inhibited by the drug FK506. Virus Res 165:112–117
Gandolfini I, Delsante M, Fiaccadori E et al (2020) COVID-19 in kidney transplant recipients. Am J Transplant 00:1–8
Yang X, Yu Y, Xu J et al (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8(5):475–481
Banerjee D, Popoola J, Shah S et al (2020) COVID-19 infection in kidney transplant recipients. Kidney Int 97(6):1076–1082
Fishman JA (2020) The immunocompromised transplant recipient and SARS-CoV-2 infection. J Am Soc Nephrol 31(6):1147–1149
Nieto-Torres JL, Verdiá-Báguena C, Jimenez-Guardeño JM et al (2015) Severe acute respiratory syndrome coronavirus E protein transports calcium ions and activates the NLRP3 inflammasome. Virology 485:330–339
Nidorf SM, Thompson PL (2019) Why colchicine should be considered for secondary prevention of atherosclerosis: an overview. Clin Ther 41(1):41–48
Funding
This study was supported by Memorial Healthcare Group, Turkey.
Author information
Authors and Affiliations
Contributions
AO: Participated in the writing of the paper and performance of the research. NA, SA, NDB, FS, EED:: Participated in the performance of the research. HY: Participated in the writing of the paper. AY: Participated in research design and data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Ethical approval
The study was approved by Marmara University Ethics Committee (No:08.05.2020/09.2020.541).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ozkok, A., Alpay, N., Alan, S. et al. Immunological parameters associated with the severity of COVID-19 pneumonia in kidney transplant recipients. Int Urol Nephrol 54, 1105–1116 (2022). https://doi.org/10.1007/s11255-021-02947-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02947-y