Abstract
Purpose
Acid–base derangement has been poorly described in patients with coronavirus disease 2019 (COVID-19). Considering the high prevalence of pneumonia and kidneys injury in COVID-19, frequent acid–base alterations are expected in patients admitted with SARS-Cov-2 infection. The study aimed to assess the prevalence of acid–base disorders in symptomatic patients with a diagnosis of COVID-19.
Methods
The retrospective study enrolled COVID-19 patients hospitalized at the University Hospital of Modena from 4 March to 20 June 2020. Baseline arterial blood gas (ABG) analysis was collected in 211 patients. In subjects with multiple ABG analysis, we selected only the first measurement. A pH of less than 7.37 was categorized as acidemia and a pH of more than 7.43 was categorized as alkalemia.
Results
ABG analyses revealed a low arterial partial pressure of oxygen (PO2, 70.2 ± 25.1 mmHg), oxygen saturation (SO2, 92%) and a mild reduction of PO2/FiO2 ratio (231 ± 129). Acid–base alterations were found in 79.7% of the patient. Metabolic alkalosis (33.6%) was the main alteration followed by respiratory alkalosis (30.3%), combined alkalosis (9.4%), respiratory acidosis (3.3%), metabolic acidosis (2.8%) and other compensated acid–base disturbances (3.6%). All six patients with metabolic acidosis died at the end of the follow-up.
Conclusion
Variations of pH occurred in the majority (79.7%) of patients admitted with COVID-19. The patients experienced all the type of acid–base disorders, notably metabolic and respiratory alkalosis were the most common alterations in this group of patients.
Similar content being viewed by others
Introduction
Acid–base disorders are common in severely ill patients and reflect the severity of the underlying pathologic process. Most cases of acid–base alterations are mild and rarely symptomatic and have a low tendency to impair organ homeostasis. Conversely, severe alterations of acid–base balance may have severe multiorgan consequences [1]. The incidence and effects of acid–base derangement in COVID-19 patients have been poorly evaluated until now [2]. Tropism of the virus for the lungs and kidneys may theoretically lead to frequent acid–base alterations due to pneumonia and kidney injury [3, 4], respectively.
Disruption of the cell-entry virus receptor—angiotensin-converting enzyme (ACE) II—is thought to be one of the leading causes of SARS-CoV-2 human pathogenicity. Theoretically, it should lead to the overactivation of the renin–angiotensin–aldosterone system mediated by an excess of angiotensin II [5, 6]. As a result, high levels of serum aldosterone may induce metabolic alkalosis through hydrogen ion loss from renal tubular cells [7, 8]. For all these reasons, a large number of acid–base disorders, principally of respiratory origin were expected in patients with symptoms of COVID-19. To verify this research question, we investigated the distribution of acid–base disorders in a cohort of symptomatic patients with a diagnosis of COVID-19.
Materials and methods
We retrospectively collected data from electronic charts of all COVID-19 patients hospitalized at the University Hospital of Modena from 4 March to 20 June 2020.
Diagnosis of COVID-19 was performed on nasal/oropharyngeal swabs according to the World Health Organization (WHO) guidelines [9] in all patients who were admitted for symptoms of COVID-19. Arterial blood gas (ABG) analysis was required to monitor pulmonary gas exchange and acid–base status. A pH of less than 7.37 was categorized as acidemia and a pH of more than 7.42 was categorized as alkalemia [10, 11].
Overall, 236 patients underwent 477 ABG analysis during the first 48 h from admission. After selection for inclusion criteria (age > 18 years and completeness of ABG analysis data), 211 patients were included in the study population. In patients with multiple ABG analyses, we selected only the first measurement. Often ABG analysis was provided after first aid. Supportive therapy consisted of oxygen therapy in dyspnoeic patients with low oxygen saturation and intravenous therapy in patients with low blood pressure.
Baseline characteristics were described using mean and standard deviation (SD), or frequencies, where appropriate. The chi-squared and one-way ANOVA followed by Turkey’s post hoc test were used to compare categorical and continuous variables between groups.
Results
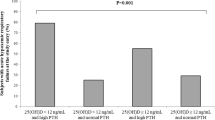
The estimated mean age of the population was 64.7 ± 15.3 years with a high predominance of males (71.6%) (Table 1). Half of the population referred dyspnea, and 61.4% had cough at physical examination. Most patients (82.6%) were on oxygen therapy when ABG analysis was performed. Overall, ABG analyses revealed pulmonary involvement manifesting with a low arterial partial pressure of oxygen (PO2, 70.2 ± 25.1 mmHg), oxygen saturation (SO2, 92%) and a mild reduction of PO2/FiO2 ratio (231 ± 129). Acid–base disturbance was found in 79.7% of the patients, and contrary to our expectation, metabolic alkalosis (33.6%) was the main alteration followed by respiratory alkalosis (30.3%), combined alkalosis (9.4%), respiratory acidosis (3.3%), metabolic acidosis (2.8%) and other compensated acid–base disturbances (3.6%) (Fig. 1). ANOVA revealed statistically significant differences in age, sex, serum level of K+, Na+, bicarbonate, creatinine, PCO2, PO2/FiO2 ratio, CKD, symptoms (caught, diarrhea), SOFA score and fatality rate among groups. Data on diuretic prescription and amount of prescribed IV fluids are reported in Supplementary Table 1.
All six patients who experienced metabolic acidosis died after 7 ± 5.6 days from admission. Half of the subjected died of acute respiratory distress syndrome and half of septic shock. Patients with metabolic acidosis had an increased value of serum creatinine and a higher SOFA score compared to patients showing a normal pH. Metabolic acidosis was primarily due to kidney impairment. A mild elevation of blood lactate levels (2.4 mmol/l) contributed to the development of metabolic acidosis in a single patient. Mean serum creatinine measured 4.5 ± 4.5 mg/dl. Notably, 33.3% of patients were on hemodialysis, 33.3% developed COVID-19-associated acute kidney injury and 33.3% had a GFR < 60 ml/min.
Discussion
The analysis of our data reported for the first time the spectrum of acid–base alterations in patients with COVID-19. Pneumonia is the main manifestation of this disease and is virtually diagnosed in all hospitalized subjects with COVID-19. It generally manifests with bilateral ground-glass opacities associated with or without consolidations [12]. Extensive pneumonia is a potentially serious infectious disease because it impairs respiratory gas exchange and induces a change in minute ventilation. Acid–base disturbances of respiratory origin were, therefore, an expected complication in our COVID-19 population. Surprisingly, metabolic alkalosis (33.6%) was the primary alteration. The etiology of this disorder was difficult to trace in our cohort of patients. Dehydration due to fever, dyspnea and loss of appetite appeared to be the most plausible hypothesis, although no statistically significant differences were detected in mean arterial pressure, Na+, body temperature, pulmonary gas exchange and diuretic therapy compared to the normal group. Furthermore, even the hypothesis of SARS-CoV-2-mediated hyperactivation of RAAS remained unexplored in our study owing to the lack of serum aldosterone levels. On the other hand, the causes of acid–base disorders of respiratory origin were easily tracked in each group. Notably, respiratory alkalosis was caused by hypoxia-induced hyperventilation (PO2 = 70.1 ± 32.9 mmHg), whereas respiratory acidosis developed in patients with hypercapnic respiratory failure (PCO2 = 62.2 ± 13.4 mmHg).
The analysis of our data reported that metabolic acidosis occurred in subjects with varying degrees of renal impairment, and a higher baseline SOFA compared to patients with normal pH. They showed a death-fatality rate of 100% at the end of the follow-up. Ammonia excretion impairment and decreased tubular reabsorption of bicarbonate [13] were supposed to be the leading causes of metabolic acidosis in this group of patients. Metabolic acidosis—acute or chronic—is a serious medical condition, associated with high morbidity and poor outcome in CKD [17] and non-CKD subjects [18]. This acid–base disorder causes notable adverse effects on organ homeostasis, especially on the cardiovascular system [14, 15], where acidosis reduces cardiac contractility, cardiac output and induces arterial vasodilation [16].
Generalization of these results is limited by the retrospective nature of the study, the small number of patients and a lack of a control group. Larger studies without the change of a selection bias are therefore necessary to confirm the distribution of acid–base disturbances in patients with COVID-19 and verify the potential association between metabolic acidosis and death risk in this subset of patients.
In conclusion, patients admitted to the hospital for symptoms of COVID-19 had a high rate of acid–base disorders. They experienced all kinds of acid–base alterations. Metabolic and respiratory alkalosis were the most common acid–base disorders in this group of patients.
Data availability
Data are available upon adeguate request.
References
Kaplan LJ, Frangos S (2005) Clinical review: acid–base abnormalities in the intensive care unit—part II. Crit Care 9:198–203. https://doi.org/10.1186/cc2912
Chhetri S, Khamis F, Pandak N et al (2020) A fatal case of COVID-19 due to metabolic acidosis following dysregulate inflammatory response (cytokine storm). IDCases 21:e00829. https://doi.org/10.1016/j.idcr.2020.e00829
Ronco C, Reis T, Husain-Syed F (2020) Management of acute kidney injury in patients with COVID-19. Lancet Respir Med 8:738–742. https://doi.org/10.1016/S2213-2600(20)30229-0
Zhu N, Zhang D, Wang W et al (2020) A Novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med. https://doi.org/10.1056/NEJMoa2001017
Alfano G, Guaraldi G, Fontana F et al (2020) The role of the renin-angiotensin system in severe acute respiratory syndrome-CoV-2 infection. Blood Purif. https://doi.org/10.1159/000507914
Ni W, Yang X, Yang D et al (2020) Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care 24:422. https://doi.org/10.1186/s13054-020-03120-0
Kassirer JP, London AM, Goldman DM, Schwartz WB (1970) On the pathogenesis of metabolic alkalosis in hyperaldosteronism. Am J Med 49:306–315. https://doi.org/10.1016/S0002-9343(70)80021-3
Wagner CA (2014) Effect of Mineralocorticoids on acid-base balance. Nephron Physiol 128:26–34. https://doi.org/10.1159/000368266
Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases. https://www.who.int/publications-detail-redirect/10665-331501. Accessed 19 Aug 2020
Castro D, Keenaghan M (2020) Arterial blood gas. In: StatPearls. StatPearls Publishing, Treasure Island (FL)
Abramowitz MK (2014) Acid-base balance and physical function. Clin J Am Soc Nephrol CJASN 9:2030–2032. https://doi.org/10.2215/CJN.10371014
Bertolino L, Vitrone M, Durante-Mangoni E (2020) Does this patient have COVID-19? A practical guide for the internist. Intern Emerg Med 15:791–800. https://doi.org/10.1007/s11739-020-02377-1
Kovesdy CP (2014) Metabolic acidosis as a possible cause of CKD: What should clinicians do? Am J Kidney Dis Off J Natl Kidney Found 64:481–483. https://doi.org/10.1053/j.ajkd.2014.08.005
Raikou VD (2016) Metabolic acidosis status and mortality in patients on the end stage of renal disease. J Transl Intern Med 4:170–177. https://doi.org/10.1515/jtim-2016-0036
Jung B, Rimmele T, Le Goff C et al (2011) Severe metabolic or mixed acidemia on intensive care unit admission: incidence, prognosis and administration of buffer therapy. A prospective, multiple-center study. Crit Care Lond Engl 15:R238. https://doi.org/10.1186/cc10487
Mitchell JH, Wildenthal K, Johnson RL (1972) The effects of acid-base disturbances on cardiovascular and pulmonary function. Kidney Int 1:375–389. https://doi.org/10.1038/ki.1972.48
Raphael KL, Zhang Y, Wei G et al (2013) Serum bicarbonate and mortality in adults in NHANES III. Nephrol Dial Transplant 28:1207–1213. https://doi.org/10.1093/ndt/gfs609
Gauthier PM, Szerlip HM (2002) Metabolic acidosis in the intensive care unit. Crit Care Clin 18(289–308):vi. https://doi.org/10.1016/s0749-0704(01)00012-4
Acknowledgements
Special thanks to all healthcare workers that have been involved in the care of COVID-19 patients. Modena Covid-19 Working Group (MoCo19) includes: Cristina Mussini, Giovanni Guaraldi, Erica Bacca, Andrea Bedini, Vanni Borghi, Giulia Burastero, Federica Carli, Giacomo Ciusa, Luca Corradi, Gianluca Cuomo, Margherita Digaetano, Giovanni Dolci, Matteo Faltoni, Riccardo Fantini, Giacomo Franceschi, Erica Franceschini, Vittorio Iadisernia, Damiano Larné, Marianna Menozzi, Marianna Meschiari, Jovana Milic, Gabriella Orlando, Francesco Pellegrino, Alessandro Raimondi, Carlotta Rogati, Antonella Santoro, Roberto Tonelli, Marco Tutone, Sara Volpi, and Dina Yaacoub (Infectious Diseases Clinics, University Hospital, via del Pozzo 71, 41124 Modena, Italy); Gianni Cappelli, Riccardo Magistroni, Gaetano Alfano, Annachiara Ferrari, Francesco Fontana, Ballestri Marco, Giacomo Mori, Roberto Pulizzi, Elisabetta Ascione, Marco Leonelli, Francesca Facchini, Francesca Damiano (Nephrology Dialysis and Transplant Unit, University Hospital of Modena, Modena, Italy); Massimo Girardis, Alberto Andreotti, Emanuela Biagioni, Filippo Bondi, Stefano Busani, Giovanni Chierego, Marzia Scotti, and Lucia Serio (Department of Anesthesia and Intensive Care, University Hospital, via del Pozzo 71, 41124 Modena, Italy); Andrea Cossarizza, Caterina Bellinazzi, Rebecca Borella, Sara De Biasi, Anna De Gaetano, Lucia Fidanza, Lara Gibellini, Anna Iannone, Domenico Lo Tartaro, Marco Mattioli, Milena Nasi, Annamaria Paolini, and Marcello Pinti (Chair of Pathology and Immunology, University of Modena and Reggio Emilia, Via Campi, 287, 41125 Modena, Italy).
Author information
Authors and Affiliations
Consortia
Contributions
Conception GA, AF. Analysis and interpretation of data: GA, AF. Drafting FF, GM, FG, AF,SG, GL, EA, SC, MB, RM. Intellectual Contribution: MDG, MM, MM, JM, BA, EF, GC,CM. Revising the article: GC, JM, GG. Approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Ethical approval
“Comitato Etico dell’Area Vasta Emilia Nord” of the “Azienda Ospedaliero-Universitaria di Modena” appoved this study (protocol number: AOU 0013376/20). This study complies with the guidelines for human studies and includes evidence that the research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Consent to participate
Not applicable because of the risk of virus spread with objects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Modena Covid-19 Working Group (MoCo19) are listed in acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Alfano, G., Fontana, F., Mori, G. et al. Acid base disorders in patients with COVID-19. Int Urol Nephrol 54, 405–410 (2022). https://doi.org/10.1007/s11255-021-02855-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02855-1