Abstract
Purpose
The use of lung ultrasound (LUS) to identify extravascular lung water has received increasing acceptance. Sonographic B-lines, discrete vertical lines that originate from the pleura, represent pulmonary edema and are correlated with the accumulation of fluid. The goal of this study was to evaluate the utility of LUS to determine the accuracy of prescribed dry weight (DW) in chronic hemodialysis (HD) patients and to ascertain the adequacy of fluid removal.
Methods
LUS was scheduled to be performed pre- and post-HD in 20 patients. The HD prescription and DW challenge were done independent of the results of the LUS. The presence of B-lines was tabulated and compared to the intradialytic ultrafiltration parameters.
Results
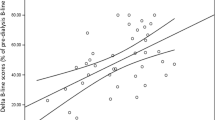
Of the 20 patients, 3 did not exhibit B-lines at the first dialysis session. In regard to the other 17 patients, B-lines disappeared in 7 patients at the end of the HD session (mean B-lines 4.2–0). One patient was 0.3 kg away from the prescribed dry weight, but the 6 patients were a mean of 1.7 kg below DW. Of the remaining 10 patients, eight decreased but did not eliminate the B-lines (mean B-lines 15.5–3.8) and were a mean of 3.8 kg below DW post-HD. Two patients who exhibited more cardiac insufficiency than initially recognized could not reach DW or eliminate the B-lines. Eight patients who had residual B-lines at the end of the first HD session had their DW re-estimated and had a second session. Two were able to eliminate the B-lines (mean 2.5–0) and reached a mean of 1.2 kg below DW. Six did not eliminate the B-lines (mean 11.5–4.2) but were able to reach a mean of 0.6 kg below DW. Correlation analysis showed a statistically significant correlation (P < 0.05) between the intradialytic percent change in B-lines and the percent change in total body weight (r = 0.40) and ultrafiltration rate (r = 0.33). Seven of 10 patients with clear chest X-rays pre-HD exhibited B-lines.
Conclusions
This study supports the hypothesis that reduction in B-lines during HD can provide accurate information regarding changes in pulmonary fluid content. Further, LUS is a valuable diagnostic tool for recognizing both the adequacy of fluid removal and the occurrence of error in the estimation of dry weight by usual clinical parameters.


Similar content being viewed by others
Abbreviations
- BIA:
-
Bioimpedance analysis
- BIS:
-
Bioimpedance spectroscopy
- BVM:
-
Blood volume monitoring
- CXR:
-
Chest X-ray
- DW:
-
Dry weight
- EDW:
-
Estimated dry weight
- ESRD:
-
End-stage renal disease
- HD:
-
Hemodialysis
- LUS:
-
Lung ultrasound
- NYHA:
-
New York heart association
- UF:
-
Ultrafiltration
References
Kalantar-Zadeh K, Regidor DL, Kovesdy CP et al (2009) Fluid retention is associated with cardiovascular mortality in patients undergoing long-term hemodialysis. Circulation 119:671–679
Wizemann V, Wabel P, Chamney P et al (2009) The mortality risk of overhydration in haemodialysis patients. Nephrol Dial Transplant 24:1574–1579
Charra B, Calemard M, Laurent G (1996) Importance of treatment time and blood pressure control in achieving long term survival on dialysis. Am J Nephrol 16:35–44
Scribner BH, Buri R, Caner JE et al (1960) The treatment of chronic uremia by means of intermittent hemodialysis: a preliminary report. Trans Am Soc Artif Intern Organs 6:114–122
Onofriescu M, Hogas S, Voroneanu L et al (2014) Bioimpedance-guided fluid management in maintenance hemodialysis: a pilot randomized controlled trial. Am J Kidney Dis 64(1):111–118
Raimann J, Liu L, Tyagi S et al (2008) A fresh look at dry weight. Hemodialysis International 12:395–405
Lichtenstein DA, Meziere GA (2008) Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 134:117–125
Jambrik Z, Monti S, Coppola V et al (2004) Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol 93:1265–1277
Agricola E, Bove T, Oppizzi M et al (2005) “Ultrasound comet tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest 127:1690–1695
Noble VE, Murray AF, Capp R et al (2014) Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest 135:1433–1439
Mallamaci F, Benedetto FA, Tripepi R et al (2010) Detection of pulmonary congestion by chest ultrasound in dialysis patients. JACC Cardiovasc Imaging 3:586–594
Kooman JP, van der Sander FM, Leunissen KM (2009) Wet or dry in dialysis–can new technologies help? Semin Dial 22:9–12
Trezzi M, Torzillo D, Ceriani E et al (2013) Lung ultrasonography for the assessment of rapid extravascular water variation: evidence from hemodialysis patients. Intern Emerg Med 8:409–415
Vitturi N, Dugo M, Soattin M et al (2014) Lung ultrasound during hemodialysis: the role in the assessment of volume status. Int Urol Nephrol 46:169–174
Torino C, Gargani L, Sicari R et al (2016) The Agreement Between Auscultation and Lung Ultrasound in Hemodialysis Patients: the LUST Study. Clin J Am Soc Nephrol 11:2005–2011
Daugirdas JT, Blake PG, Ing TS (2007) Handbook of dialysis. Lipincott Williams, Baltimore, pp 205–206
Thomson GE, Waterhouse K, McDonald HP Jr, Friedman EA (1967) Hemodialysis for chronic renal failure. Clinical observation. Arch Intern Med 120:153–167
Fuller D, Robinson B (2017) Facility practice variation to help understand the effects of public policy: insights from the dialysis outcomes and practice patterns study (DOPPS). Clin J Am Soc Nephrol 12(1):190–199
Charra B, Bergstrom J, Scribner BH (1998) Blood pressure control in dialysis patients: importance of the lag phenomenon. Am J Kidney Dis 32:720–724
Chan C, McIntyre C, Smith D et al (2009) Combining near-subject absolute and relative measures of longitudinal hydration in hemodialysis. Clin J Am Soc Nephrol 4(11):1791–1798
Steuer RR, Bell DA, Barrett LL (1999) Optical measurement of hematocrit and other biological constituents in renal therapy. Adv Ren Replace Ther 6(3):217–224
Zhu F, Sarkar S, Kaitwatcharachai C et al (2003) Methods and reproducibility of measurement of resistivity in the calf using regional bioimpedance analysis. Blood Purif 21:131–136
Siriopol D, Onofriescu M, Voroneanu L et al (2017) Dry weight assessment by combined ultrasound and bioimpedance monitoring in low cardiovascular risk hemodialysis patients: a randomized controlled trial. Int Urol Nephrol 49:143–153
Bennett BC, Vivas CA (1997) Postoperative management of the renal transplant recipient. In: Shapiro R, Simmons RL, Starzl TE (eds) Renal Transplantation. Appleton and Lange, Connecticut, pp 141–148
Acknowledgements
This study was performed with the support of our biostatistics department and our hemodialysis unit nursing staff. We wish to thank Mr. Guillaume Stoffels MA, MS. His assistance with the study design and statistical analysis was invaluable. We also thank Marlyn A. Batan RN, BSN, CNN, nurse manager of our dialysis unit for her enthusiastic efforts.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All of the authors declare that they have no conflicts of interests.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of Northwell Health and with the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Jiang, C., Patel, S., Moses, A. et al. Use of lung ultrasonography to determine the accuracy of clinically estimated dry weight in chronic hemodialysis patients. Int Urol Nephrol 49, 2223–2230 (2017). https://doi.org/10.1007/s11255-017-1709-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1709-5