Abstract
Objective
This study was organized to form a symptom scale for diagnosis and assessment of urinary and bowel symptoms in children with dysfunctional elimination syndrome (DES).
Methods
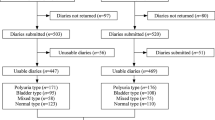
The study group included 81 children presented to our clinic with symptoms of DES like enuresis, abnormal voiding, urinary tract infection and urgency, between January 2003 and February 2004. Age matched 102 children with no history of urological complaints were randomly recruited from a public school as control group. Children with isolated, mono-symptomatic nocturnal enuresis were not taken to the study. All children and parents were requested to fill a 35-item questionnaire related to symptoms of DES. After statistical analysis, questions from the initial form that had a P-value <0.05 and an area under curve (AUC) value >0.6 were selected to form a final scale.
Results
The mean ages for study and control groups were 8.7 ± 2.5 and 8.3 ± 2.2 years, respectively (P = 0.236). The final scale was composed of 15 questions. The cut-off score for the presence of DES was determined as 7.5 (sensitivity 85.2%, specificity 93.1%, AUC value = 0.943) for the total population. When only the male population were concerned the cut-off score was 4.5 (sensitivity 93.8%, specificity 78%, AUC value = 0.913) while the cut-off score for the female population was 7.5␣(sensitivity 87.7%, specificity 94.2%, AUC value = 0.953).
Conclusion
Providing objective assessment of symptom severity, formation of a validated scoring system for children with DES might be a good tool for diagnosis, confirmation of treatment results and follow up. It might also be useful for screening purposes.
Similar content being viewed by others
References
Koff SA, Jayanthi VR (2002) Non-neurogenic lower urinary tract dysfunction. In: Walsch PC (eds) Campbell’s Urology, 8th edn. Saunders Company, Philadelphia, USA, pp 2262–2263
Rushton HG (1995) Wetting and functional voiding disorders. Urol Clin North Am 22(1):75–93
Snodgrass W (1991) Relationship of voiding dysfunction to urinary tract infection and vesicoureteral reflux in children. Urol 38(4):341–344
Koff SA, Wagner TT, Jayanthi VR (1998) The relationship among dysfunctional elimination syndromes, primary vesicoureteral reflux and urinary␣tract infections in children. J Urol 160:1019–1022
Norgaard JP, Van Gool JD, Hjalmas K, Djurhuus JC, Hellström AL (1998) Standardization and definitions in lower urinary tract dysfunction in children. International Children’s Continence Society. Br J Urol Suppl 3:1–16
Hoebeke P, Van Laecke E, Van Camp C, Raes A, Van De Walle J (2001) One thousand video-urodynamic studies in children with non-neurogenic bladder sphincter dysfunction. BJU Int 87:575–580
Porter T, Weerasinghe N, Malone PS (1995) Modification of therapy based on videourodynamics in neurologically normal children: Southhampton 1988–1993. Br J Urol 76:779–781
Schewe J, Brands FH, Pannek J (2002) Voiding dysfunction in children: role of urodynamic studies. Urol Int 69:297–301
O’Leary MP, Sant GR, Fowler FJ et al (1997) The interstitial cystitis symptom index and problem index. Urol 49(5A Suppl):58–63
Barry MJ, Fowler FJ, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK (1992) The American urological association symptom index for benign prostatic hyperplasia. The measurement committee of the American urological association. J Urol 148:1549–1557
Farhat W, Bagli DJ, Capolicchio G, O’Reilly S, Merguerian PA, Khoury A, McLorie GA (2000) The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children. J Urol 164:1011–1015
Akbal C, Genç Y, Burgu B, Özden E, Tekgül S (2005) Dysfunctional voiding and incontinence scoring system: quantitative evaluation of incontinence symptoms in pediatric population. J Urol 173:969–973
Koff SA (1992) Relationship between dysfunctional voiding and reflux. J Urol 148(5 pt 2):1703–1705
Homsy YL (1994) Dysfunctional voiding syndromes and vesicoureteral reflux. Pediatr Nephrol 8:116–121
Allen TD, Bright TC (1978) Urodynamic patterns in children with dysfunctional voiding problems. J Urol 119:247–249
McGuire EJ, Savastano JA (1984) Urodynamic studies in enuresis and the nonneurogenic neurogenic bladder. J Urol 132:299–302
Mayo ME, Burns MW (1990) Urodynamic studies in children who wet. Br J Urol 65:641–645
Passerini-Glazel G, Cisternino A, Camuffo MC, Ferrarese P, Aragona F, Artibani W (1992) Videourodynamic studies of minor voiding dysfunctions in children: an overview of 13 years experience. Scand J Urol Nephrol Suppl 141:70–84
Ollendick TH, King NJ, Frary RB (1989) Fears in children and adolescents: reliability and generalizability across gender, age and nationality. Behav Res Ther 27:19–26
Hagglof B, Andren O, Bergstrom E, Marklund L, Wendelius M (1997) Self-esteem before and after treatment in children with nocturnal enuresis and urinary incontinence. Scand J Urol Nephrol Suppl 183:79–82
Nijman RJ (2000) Classification and treatment of functional incontinence in children. BJU Int 85(Suppl 3):37–42
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A
Questionnaire for Dysfunctional Elimination Syndrome
Date:
Name-surname:
Sex:
Age:
Telephone number:
Address:
Part-1 (Questions for the Child)
Urgency Symptoms (During the last 3–6 months)
These questions will help us to understand the problems related to your complaints. Please think about your toilet habits during the last 3–6 months, and choose the best answer that fits to your habits.
Appendix B
Final symptom scale for children with dysfunctional elimination syndrome
Rights and permissions
About this article
Cite this article
Tokgöz, H., Tan, M.Ö., Şen, İ. et al. Assessment of urinary symptoms in children with dysfunctional elimination syndrome. Int Urol Nephrol 39, 425–436 (2007). https://doi.org/10.1007/s11255-006-9062-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-006-9062-0