Abstract
Objective
To study the agreement of questionnaire-based assessment with voiding diary for differentiating primary mono-symptomatic nocturnal enuresis from voiding disorder in children.
Method
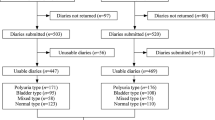
Children 5–12 years old with bedwetting after exclusion of secondary enuresis were enrolled and parents filled a clinical management tool (CMT) questionnaire and a 48-hours voiding diary. Point prevalence and agreement of classification as primary mono-symptomatic nocturnal enuresis or voiding disorder were compared.
Results
Of 1276 children screened, 143 (11.2%) reported enuresis. Of 100 (82 males) children finally analyzed, constipation and positive family history occurred in 14% and 37%, respectively. Questionnaire-based assessment and voiding diary identified 65% and 71%, respectively as voiding disorder [Cohen’s kappa 0.542 (95%CI: 0.367–0.717)]. Discordance of classification was noted in 20%. Voiding diary identified additional 7% cases of voiding disorder.
Conclusion
While CMT and voiding diary have moderate agreement, voiding diary should be used for cases screened negative by a questionnaire-based tool.
Similar content being viewed by others
References
Austin PF, Bauer SB, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the Standardization Committee of the International Children’s Continence Society. J Urol. 2014;191:1863–65.e13.
VandeWalle J, Rittig S, Bauer S, et al. Practical consensus guidelines for the management of enuresis. Eur J Pediatr. 2012;171:971–83.
Kajiwara M, Kato M, Mutaguchi K, et al. Overactive bladder in children should be strictly differentiated from mono-symptomatic nocturnal enuresis. Urol Int. 2008;80:57–61.
Kanitkar M, Ramamurthy HR. Bed wetting — Silent suffering: An approach to enuresis and voiding disorders in children. Indian J Pediatr. 2013;80:750–53.
Dogan HS, Akpinar B, Gurocak S, et al. Non-invasive evaluation of voiding function in asymptomatic primary school children. Pediatr Nephrol. 2008;23:1115–22.
Farhat W, McLorie GA, O’Reilly S, et al. Reliability of the pediatric dysfunctional voiding symptom score in monitoring response to behavioral modification. Can J Urol. 2001;8: 1401–5.
Farhat W, Bägli DJ, Capolicchio G, et al. The dysfunctional voiding scoring system: Quantitative standardization of dysfunctional voiding symptoms in children. J Urol. 2000;164:1011–5.
Ku JH, Jeong IG, Lim DJ, et al. Voiding diary for the evaluation of urinary incontinence and lower urinary tract symptoms: Prospective assessment of patient compliance and burden. Neurourol Urodyn. 2004;23:331–5.
Shoukri MM, Asyali MH, Donner A. Sample size requirements for the design of reliability study: Review and new results. Stats Method Med Res. 2004;13:1–21.
Eapen V, Mabrouk AM. Prevalence and correlates of nocturnal enuresis in the United Arab Emirates. Saudi Med J. 2003;24: 49–51.
Barroso U Jr, Nova T, Dultra A, et al. Comparative analysis of the symptomatology of children with lower urinary tract dysfunction in relation to objective data. Int Braz J Urol. 2006;32:70–6.
Kwak KW, Park KH. Clinical inconsistency of lower urinary tract symptoms between questionnaire and bladder diary in children with nocturnal enuresis J Urol. 2008;180:1085–9.
De Gennaro M, Niero M, Capitanucci ML, et al. Validity of the international consultation on incontinence questionnaire-pediatric lower urinary tract symptoms: A screening questionnaire for children. J Urol. 2010;184:1662–7.
Akbal C, Sahan A, Sener TE, et al. Diagnostic value of the pediatric lower urinary tract symptom score in children with overactive bladder. World J Urol. 2014;32:201.
McGrath KH, Caldwell PH, Jones MP. The frequency of constipation in children with nocturnal enuresis: A comparison with parental reporting. J Paediatr Child Health. 2008;44:19–27.
Funding
Funding: None
Author information
Authors and Affiliations
Contributions
Contributors: MK: conceptualization of study, drafting, finalization and approval of manuscript; SS: case recruitment, initial evaluation, literature review, manuscript drafting and approval: SKP: clinical assessment, analysis, drafting and approval of manuscript. All authors approved the final version of manuscript, and are accountable for all aspects related to the study.
Corresponding author
Ethics declarations
Ethics clearance: nstitutional ethics committee, Base Hospital Delhi Cantt; No. 139/2013 dated August 17, 2013.
Competing interest: None stated.
Additional information
Disclaimer: The work reported is those of the individual authors and in no way reflect the official position of the Directorate General Armed Forces Medical Services of India or Ministry of Defence.
Rights and permissions
About this article
Cite this article
Sajith, S., Patnaik, S.K. & Kanitkar, M. Comparison of a Voiding Diary With Clinical Management Tool As an Outpatient Screening Tool for Childhood Functional Voiding Disorders. Indian Pediatr 58, 1147–1150 (2021). https://doi.org/10.1007/s13312-021-2397-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-021-2397-x