Abstract
Anticoagulation therapy is standard for conditions like atrial fibrillation, venous thromboembolism, and valvular heart disease, yet it is unclear if there are ethnoracial disparities in its quality and delivery in the United States. For this scoping review, electronic databases were searched for publications between January 1, 2011 – March 30, 2022. Eligible studies included all study designs, any setting within the United States, patients prescribed anticoagulation for any indication, outcomes reported for ≥ 2 distinct ethnoracial groups. The following four research questions were explored: Do ethnoracial differences exist in 1) access to guideline-based anticoagulation therapy, 2) quality of anticoagulation therapy management, 3) clinical outcomes related to anticoagulation care, 4) humanistic/educational outcomes related to anticoagulation therapy. A total of 5374 studies were screened, 570 studies received full-text review, and 96 studies were analyzed. The largest mapped focus was patients’ access to guideline-based anticoagulation therapy (88/96 articles, 91.7%). Seventy-eight articles made statistical outcomes comparisons among ethnoracial groups. Across all four research questions, 79 articles demonstrated favorable outcomes for White patients compared to non-White patients, 38 articles showed no difference between White and non-White groups, and 8 favored non-White groups (the total exceeds the 78 articles with statistical outcomes as many articles reported multiple outcomes). Disparities disadvantaging non-White patients were most pronounced in access to guideline-based anticoagulation therapy (43/66 articles analyzed) and quality of anticoagulation management (19/21 articles analyzed). Although treatment guidelines do not differentiate anticoagulant therapy by ethnoracial group, this scoping review found consistently favorable outcomes for White patients over non-White patients in the domains of access to anticoagulation therapy for guideline-based indications and quality of anticoagulation therapy management. No differences among groups were noted in clinical outcomes, and very few studies assessed humanistic or educational outcomes.
Graphical Abstract
Scoping Review: Differences in quality of United States anticoagulation care delivery by ethnoracial group. AF = atrial fibrillation; AMS = anticoagulation management service; DOACs = direct oral anticoagulants; INR = international normalized ratio; PSM = patient self-management; PST = patient self-testing

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well-established that in the United States (US) ethnoracial disparities exist in various aspects of health care. Specifically, persons identifying with an ethnoracial minority group may have more challenging access to health care, worse clinical outcomes, and higher dissatisfaction with care compared to White persons [1,2,3,4,5]. There are differences by ethnoracial group in the prevalence of the three most common indications for which anticoagulants are prescribed, stroke prevention in atrial fibrillation (AF), treatment of venous thromboembolism (VTE), and valvular heart disease [6,7,8,9,10,11,12,13,14,15,16,17]. Specifically, VTE is most prevalent in Black patients compared to White and Asian patients, whereas AF is most prevalent in White patients compared to Black, Asian, and Hispanic patients [9, 10, 15]. Calcific heart valve disease has the most relevance to the US population, and epidemiologic data has shown that aortic stenosis is more prevalent in White patients compared to Black, Asian, and Hispanic patients [17]. Despite these epidemiologic differences, there is no evidence to suggest there should be any difference in treatment strategies across ethnoracial patient groups.
While studies have demonstrated genotypic differences that may result in different warfarin dose requirements[18], and early studies may indicate genotypic differences in direct oral anticoagulant (DOAC) response [19], no US-based labeling or guidelines recommend a difference in prescription or delivery of anticoagulation care based on race or ethnicity. However, it is unclear if there are in fact differences in the type and quality of anticoagulation therapy, which is standard of care for each of these conditions [20,21,22,23,24]. Anticoagulants remain in the top three classes of drugs causing adverse drug events (primarily bleeding) in the United States, according to the 2014 National Action Plan for Adverse Drug Event Prevention. One of the goals of the National Action Plan was to identify patient populations at higher risk for these adverse drug events to inform the development of targeted harm reduction strategies [25]. If ethnoracial minority patients are receiving sub-optimal anticoagulation therapy in certain measurable areas of anticoagulation quality, it is vital to highlight the areas of disparity so that these can be explored and care optimized. Anticoagulation providers often have high frequency contact with their patients and can be a reliable connection between disproportionately affected patients and a system in need of change. Systematic reviews of ethnoracial disparities in AF and VTE have been conducted. The AF review assessed AF prevalence among racial groups as well as differences in symptoms and management, including stroke prevention with warfarin or DOACs [9]. The VTE review specifically assessed VTE prevalence and racial differences in COVID-19 and did report the use of any prophylactic anticoagulation, but this was not part of the analysis [26]. No review of racial disparities in quality of anticoagulation therapy was found in search results conducted prior to protocol.
In this study we aimed to identify any potential ethnoracial disparities in anticoagulation care quality in the US. The decision to limit the study to a US population was based on our observation that the US has a unique history of interactions between racial and ethnic groups that may not necessarily be reflected by studies conducted in other countries. Additionally, health care delivery systems vary widely across the world, and we wanted to include the data most relevant to the potential racial disparities existing in the US health care system. The term “race” was used to identify a group of people with shared physical characteristics believed to be of common ancestry whereas the term “ethnicity” refers to a group of people with shared cultural traditions [27]. We recognize these terms may be far more complex. In order to encompass both the physical and cultural aspects of a patient’s identity we have chosen to use the term “ethnoracial” for this study [27]. Highlighting existing differences will serve as a stimulus for institutions and clinicians to assess current services, implement quality improvement measures, and inform future research efforts to deliver optimal anticoagulation care for all patients. The scoping review protocol was registered December 22, 2021 to Open Science Framework, https://doi.org/10.17605/OSF.IO/9SE7H [28].
Methods
We conducted this scoping review with guidance from the 2020 version of the JBI Manual for Evidence Synthesis and organized to Arksey's five stages: 1) identifying the research question, 2) identifying relevant studies, 3) study selection, 4) charting the data and 5) collating, summarizing and reporting the results [29, 30]. For transparency and reproducibility, we followed the PRISMA-ScR and PRISMA-S reporting guidelines in reporting our results [31]. We used Covidence (Veritas Health Innovation,) an online systematic reviewing platform to screen and select studies. Citation management and duplicate detection and removal was accomplished with EndNote, version 19 (Clarivate Analytics.) Data was charted from our selected studies using REDCap, an electronic data capture tool hosted at the University of Utah [32].
Literature searching
An information specialist developed and translated search strategies for the online databases using a combination of keywords and controlled subject headings unique to each database along with team feedback. Peer review of the strategies was conducted by library colleagues using the PRESS guidelines. [33] Electronic databases searched included Medline (Ovid) 2011–2022, Embase (embase.com) 2011–2022, CINAHL Complete (Ebscohost) 2011–2022, Sociological Abstracts (ProQuest) 2011–2022, International Pharmaceutical Abstracts (Ovid) 2011–2022, Scopus (scopus.org) 2011–2022 and Web of Science Core Collection (Clarivate Analytics) 2011–2022. Limits included a date range from January 1, 2011 to March 30—April 19, 2022, as not all database results were exported on the same day. See Supplemental File 1 for detailed search strategies. A search of grey literature was not conducted due to time and resource constraints.
Study Selection
For inclusion, each study required two votes by independent reviewers for screening of titles and abstracts followed by full-text review. A third reviewer provided the deciding vote. Data extraction was performed by two independent reviewers, and consensus on any discrepancies was reached via discussion between the reviewers. The data form was piloted by two team members using sentinel articles prior to data extraction.
Eligible studies included all types of study designs in any setting with a population of patients of any age or gender located within the US who were prescribed anticoagulant therapy for any indication, published between January 1, 2011 – March 30, 2022 in order to capture contemporary and clinically relevant practices.
We defined the following research questions for this scoping review as described in Table 1.
Studies must have reported any of these anticoagulation care delivery outcomes for at least 2 distinct racial or ethnic groups. We excluded genotyping studies and non-English language articles at full text review, as we had no funding for translation services. In checking references of included studies, no additional studies met inclusion criteria. In accordance with scoping review methodology, no quality assessment of included studies was conducted as our goal was to rapidly map the literature. As this is a scoping review of the literature, no aggregate or pooled analysis was performed; however, for ease of interpretation, when assessing for the directionality of the outcomes in the various studies, we categorized studies into Favoring White Group, Favoring Non-White Group, and No Differences Among Ethnoracial Groups. If studies had mixed outcomes of favoring one group for one outcome and no difference for another, then the study was categorized with the favoring group.
Results
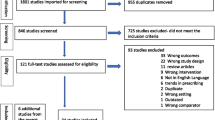
A PRISMA flow diagram in Fig. 1 depicts search results, exclusions, and inclusions. The search strategies retrieved 6900 results with 1526 duplicates removed. Following title and abstract screening of 5374 references, 570 articles received full-text review. The most common reason for the exclusion of 474 studies was that outcomes were not reported for two distinct ethnoracial groups (171 studies). Ninety-six studies underwent data extraction.
Study characteristics-overall
Fifty of the 96 studies were published between 2011 and 2018 (an average of 6.25 articles per year that compared outcomes between two ethnoracial groups) and 43 of 96 studies were published in the years 2019–2021 (average 14.3 articles per year; 2022 excluded here because only 4 months of data was captured) (Fig. 2). Most studies analyzed an outpatient population (65.6%) for an indication of stroke prevention in AF (67.7%) in patients taking warfarin (71.9%) or DOACs (49.0%). Study population size was heterogenous, ranging from a study size of 24 patients to over 1.3 million patients (median 5,238 patients) in the 69 studies that reported population size by racial group. When stratified by size, 60.9% of the articles in the scoping review (42 articles) represented < 10,000 patients (Table 2).
Study characteristics-by ethnoracial group
There were 50 studies (52.1%) where race or ethnicity was either mentioned in the title or objective of the article, with 24 of these published over the 7-year period 2011–2018 and 26 published over the 3-year period 2019 to first quarter 2022. The method for reporting race or ethnicity was unclear or unspecified in most studies (77.1%) and 16 articles (16.7%) utilized self-reporting of race or ethnicity. Most studies analyzed White or Caucasian racial groups (94.8%), followed by Black or African-American (80.2%), and many studies grouped all other racial groups into an “Other” category (41.7%) (Fig. 3).
White patients accounted for a median 77% of study populations, Black patients 9.5%, Hispanic/Latino patients 6.2%, “Other” racial groups 5.3%, and Asian patients 2.5%.
Study outcomes-overall
Of the 4 research questions, most studies included in this review analyzed patients’ access to guideline-based anticoagulation therapy (88/96 articles, 91.7%), clinical outcomes (42/96 articles, 43.8%), or quality of anticoagulation management (24/96 articles, 25.0%), while very few addressed humanistic or educational outcomes (5/96 articles, 5.2%) (Fig. 4). Many studies addressed multiple outcomes within the single study.
Seventy-eight of the 96 included studies provided statistical comparisons between ethnoracial groups, and these data are presented below.
Outcomes for research question 1: Do ethnoracial differences exist in access to guideline-based anticoagulation therapy?
Anticoagulation for a guideline-based indication
This question focused on patients who had an indication for anticoagulation actually receiving an anticoagulant, specifically AF and VTE prophylaxis (based on risk stratification) and acute VTE. The majority of the AF studies (25/34 studies) demonstrated White patients receiving anticoagulation at significantly higher rates compared to non-White patients [36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60], while the six VTE studies largely demonstrated no difference among ethnoracial groups [61,62,63,64,65,66].
DOACs as first-line therapy for AF or VTE
Eighteen individual studies statistically assessed the outcome of DOAC as first-line therapy (compared to warfarin) for AF (15 studies), VTE treatment (2 studies), or both indications (1 study). Twelve of the 15 AF studies showed a significantly higher proportion of White patients received DOACs as first-line therapy compared to non-White patients [36, 40,41,42,43,44,45,46, 54, 55, 67, 68]. Of those 12, 9 specifically compared White patients to Black patients. Both VTE treatment studies and the study that assessed both AF and VTE indications showed significantly higher DOAC prescribing rates for White patients compared to Black patients [69,70,71].
Anticoagulant therapy adherence/persistence
The eight studies that addressed anticoagulation therapy adherence/persistence showed variability in outcome directionality by ethnoracial group: 5 no difference [41, 72,73,74,75], 2 showed better treatment adherence/persistence for White patients compared to Black patients[76] or non-White patients [77], and one showed better treatment adherence/persistence for White patients compared to Hispanic patients, but no difference in White versus Black patients [78].
Figure 5 summarizes the outcome directionality for Research Question 1 regarding access to guideline-based anticoagulation therapy. Overall, the areas of disparity identified included anticoagulation for atrial fibrillation and preferential use of DOAC therapy for AF and VTE treatment.
Research question 2: Do ethnoracial differences exist in the quality of anticoagulation therapy management?
A total of 21 studies assessed quality of anticoagulation therapy management: Warfarin time in therapeutic range (TTR)/INR (International Normalized Ratio) control 12 studies, appropriate anticoagulant dosing 3 studies, enrollment in an anticoagulation management service 5 studies, and PST/PSM one study.
In statistical comparisons of INR control in warfarin patients, all 12 studies (7 assessed mean or median TTR, 5 assessed other measures of INR control such as days spent above/below range, gaps in INR monitoring) showed White patients had favorable INR control compared to non-White patients (most comparisons included Black patients) [41, 75, 79,80,81,82,83,84,85,86,87]. Enrollment in an anticoagulation management service was statistically compared among ethnoracial groups in 5 studies, and this opportunity favored White patients compared to other racial groups in four of the five [41, 82, 86, 88]. Two of the three studies that statistically analyzed appropriate anticoagulant dosing showed a higher rate of appropriate DOAC dosing in White patients compared to non-White patients [41, 89], and the third showed no difference among ethnoracial groups for enoxaparin dosing in the emergency department [90]. The one study assessing access to PST/PSM showed that more White patients used PST compared to Black or Hispanic patients[91] (Fig. 5).
Research question 3: Do ethnoracial differences exist in the clinical outcomes related to anticoagulation care?
Articles assessing clinical outcomes among ethnoracial groups primarily assessed bleeding (15 articles) or thrombosis (9 articles) outcomes, and 8 articles assessing anticoagulation related hospitalization or mortality. One article addressed a net clinical outcome including major bleeding, stroke or systemic embolism, and death from any cause. This was included in the bleeding outcomes category so that it was not double-counted in the other two outcome categories. Additional details about the 24 unique studies that statistically assessed clinical outcomes including the study design, population size, ethnoracial groups studied, anticoagulants used, and statistical outcomes measured can be found in Supplementary Tables 1 and 2.
Sixteen studies statistically assessed bleeding outcomes of varying definitions (major bleeding 13 studies, clinically relevant non-major bleeding 3 studies, any bleeding 3 studies, bleeding otherwise defined 3 studies). Six studies demonstrated no difference in bleeding outcomes by ethnoracial group [55, 92,93,94,95,96]9 reported that White patients had lower rates of bleeding compared to Black or Asian patients,[53, 80, 83, 85, 97,98,99,100,101]. In the remaining study, Asian patients had a more favorable net clinical outcome compared to non-Asian patients [102].
Nine studies statistically assessed thrombosis outcomes among ethnoracial groups, including stroke/systemic embolism (5 studies), recurrent VTE (3 studies), or any thrombosis (1 study). The stroke outcomes by racial group were heterogeneous, with 3 studies showing better outcomes for White patients compared to Black patients[103,104,105] and two studies showing no difference in outcomes when White patients were compared to Non-White patients [55, 95]. In three of the four VTE studies there were no differences in outcomes by ethnoracial group [61, 93, 96], and in one study White patients had more favorable outcomes compared to Black patients [106].
Nine studies assessed anticoagulation-related hospitalizations or mortality by ethnoracial group. Outcomes were mixed, as four studies showed no difference in hospitalizations or mortality among ethnoracial groups,[89, 95, 96, 107], three studies showed White patients had a lower rate of hospitalizations[85, 105] or mortality[104, 105] Another study showed lower rate of mortality or hospice after intracranial hemorrhage in Black and Other race patients [108].(Fig. 5).
Research question 4: Do ethnoracial differences exist in the humanistic/educational outcomes related to anticoagulation therapy?
The five studies reporting this category of outcomes were heterogeneous. Of the two studies assessing anticoagulation knowledge, one showed no difference by ethnoracial group [109], and the other favored the non-White group in appropriately estimating bleeding risk [110]. One study assessed an atrial fibrillation quality of life score at 2-year follow-up after AF diagnosis and found the outcomes favored White patients [79]. Another study assessed satisfaction with VTE care and found no difference among ethnoracial groups [111]. A third study found no difference in the percentage of racial groups having a cost conversation when initiating DOAC therapy (78% Whites, 72.2% non-Whites)[112] (Fig. 5).
Overall outcome directionality for all four research questions is shown in Fig. 6. A total of 79 articles demonstrated favorable outcomes for White patients compared to non-White patients, 38 articles showed no difference between White and non-White groups, and 8 articles had outcomes favoring non-White groups (the total exceeds the 78 articles with statistical outcomes as many articles reported multiple outcomes). The biggest areas of disparity between White and non-White groups are access to guideline-based anticoagulation therapy and quality of anticoagulation therapy management. Clinical outcomes relating to anticoagulation care had the least difference among ethnoracial groups. Relatively few studies assessed potential ethnoracial disparities in humanistic and educational outcomes.
Discussion
This scoping review assessing ethnoracial differences in the quality of anticoagulation care and its delivery to patients in the United States encompassed eleven full years of literature and resulted in the inclusion of 96 studies, 78 of which contained statistical outcomes comparisons among ethnoracial groups. The most common reason for study exclusion was that outcomes were not reported for at least two distinct ethnoracial groups. We observed that beginning in 2019 and following the racial unrest of 2020, the density of articles addressing ethnoracial disparities in anticoagulation care more than doubled. During the entire study period, half of studies had race or ethnicity as the focus or objective of the paper, but this was largely driven by articles published after 2019.
Only 16% of included articles documented self-reporting of racial identity, with most of the remainder using an unspecified method for documenting racial identity. It is likely that many studies utilize demographic information extracted from an electronic medical record (EMR), but it is often unclear if that is truly self-reported race. A second element this scoping review identified was that many studies analyzed two or three ethnoracial groups and then categorized all others into a heterogenous “Other” category. For example, frequently studies would categorize patients as White, Black, and “Other.” It is unclear whether those in a racial category labeled as “Other” had an unknown or missing racial identity in the EMR, or intentionally chose not to disclose. It is also likely that study investigators decided to classify ethnoracial groups with lower population sizes into a miscellaneous category. There were few studies (15%) that specifically assessed patients identifying as Native American/Alaska Native, Native Hawaiian/Pacific Islander, and multiracial. While Hispanic/Latino is an ethnicity, most studies categorized it as a separate “race” category. Of the 37 studies that analyzed “Asian” patient populations, none specifically defined “Asian” beyond that. The US Census Bureau defines “Asian” race as a person having origins of the Far East, Southeast Asia, or the Indian subcontinent [113]. This broad definition encompasses many different ethnicities which could represent variability in health outcomes if better defined and more frequently analyzed. These may be opportunities for EMR systems to improve transparency for how race, ethnicity, and language preference are captured and for those designing research studies to be thoughtful and intentional about analyzing the ethnoracial identities of the study population, perhaps in alignment with the minimum 5 racial categories utilized by the US Census Bureau, the National Institutes of Health, and the Office of Management and Budget (White, Black, American Indian/Alaska Native, Asian, Native Hawaiian/Pacific Islander, with permission for a “some other race” category and the option to select multiple races) [113]. Since 2017 Clinicaltrials.gov has required the reporting of race/ethnicity if collected, and there is good compliance with this requirement, but less so in publication of the work [114].
We examined the proportion of ethnoracial groups represented for each of the disease states in the studies included in this scoping review, relative to disease state prevalence and found a discrepancy. For AF, prevalence in White patients was 11.3%, in Black patients 6.6%, and in Hispanic patients 7.8% [15]. However, the representation in AF studies in this review were 74% White, 13% Black, and 8% Hispanic. Assessing VTE incidence by race is more difficult, as studies have shown regional and time variation, with Black patients typically having a higher incidence compared to other ethnoracial groups [16]. In this review, however, of the studies assessing VTE treatment or prophylaxis, only 16% of the patient population identified as Black, whereas 70% identified as White. There were only 3 studies that assessed a valvular heart disease population, making ethnoracial group representation difficult to assess.
The majority of studies captured in this review analyzed patients in the outpatient setting, for the anticoagulation indication of stroke prevention in AF, taking either warfarin or DOAC. Few studies involved the acute care setting or injectable anticoagulants, representing an area for future study of potential ethnoracial disparities.
Overall, the majority of studies in this scoping review addressed ethnoracial disparities in patients’ access to guideline-based anticoagulation therapy, clinical outcomes related to anticoagulation care, and quality of anticoagulation management. A research gap identified was more study is needed to assess gaps in educational outcomes such as anticoagulation and disease state knowledge, shared decision-making willingness and capability, and humanistic outcomes such as quality of life or satisfaction with anticoagulation therapy.
In analyzing the first research question regarding ethnoracial differences in access to guideline-based anticoagulation therapy, the majority of studies addressed use of any anticoagulation for stroke prevention in AF in patients above a threshold risk score and the preferential use of DOACs as first-line therapy instead of warfarin for AF. In both categories, patients in a non-White ethnoracial group (particularly Black patients) received recommended therapy less often than patients identified as White. It is unclear why this is the case. It could be on the patient, provider, and/or system level. It is possible that some studies more successfully adjusted for covariates than others. Sites or settings with systematic processes like order sets or clinical decision support systems in place for standard prescribing may be more successful in equitably prescribing indicated therapies. In one large study in the Veterans Affairs population of AF patients, even after adjusting for numerous variables that included clinical, demographic, socioeconomic, prescriber, and geographic site factors, DOAC prescribing remained lower in Asian and Black patients when compared with White patients. The authors in that study postulate that non-White populations may be less receptive to novel therapies due to historical mistrust of the health care system or have reduced access to education about the latest treatments, and they give the example of direct-to-consumer advertising [42]. It has also previously been demonstrated that prescribing of oral anticoagulation and particularly DOACs is lower in non-White patients [41]. These are difficult to capture as standard covariates, which is why further study is needed. We examined the publication dates for both access categories to see if perhaps there was a lack of contemporary data skewing the outcomes. However, for both anticoagulation for a guideline-based indication and DOACs as first-line therapy, the majority of articles came from the time period 2019–2021 (24 of 40 articles, and 15 of 18 articles, respectively), well after guideline updates preferentially recommended DOACs [34, 35]. Also, there were relatively few studies addressing guideline-based therapy for VTE treatment and prophylaxis, making assessment of disparities difficult. Regarding access, it is well established that race and ethnicity often determine a patient’s socioeconomic status and that low socioeconomic status and its correlates (e.g., reduced education, income, and healthcare access) are associated with poorer health outcomes [115]. However, at each level of income or education, Black patients experience worse health outcomes than Whites [116]. So, low socioeconomic status does not fully explain poorer health outcomes for non-White individuals.
After examining access to appropriate and preferred anticoagulation therapy, the second research question of this scoping review examined potential ethnoracial disparities in the quality of anticoagulation therapy management. INR control measures such as time in therapeutic INR range are a surrogate measure of both thrombotic and bleeding outcomes and frequently used as a way to assess quality of warfarin therapy. The studies identified in this review showed clear disparity between White and non-White patient groups (especially Black patients), however all twelve studies comparing TTR among ethnoracial groups were published prior to 2019. This could be due to the decline in warfarin prescribing relative to increases in DOAC prescribing [117,118,119], but there remain patient populations that require or choose warfarin, so this marker of anticoagulation control remains relevant and requires continued reassessment. There were relatively few studies assessing other markers of anticoagulation management quality such as anticoagulation management service enrollment, appropriate DOAC dosing, and access to quality improvement strategies like PST or PSM. Few studies assessed educational outcomes, yet this may have relevance to the above anticoagulation care quality question. For those patients who remain on warfarin, dietary Vitamin K consistency is an example of a key educational point that links directly to INR control. It is unclear if there are disparities in this type of education among ethnoracial groups that may have more far-reaching effects.
Of note, clinical outcomes related to anticoagulant therapy seemed to have the fewest areas of disparity, although the number of articles was small. This suggests that if patients have access to high quality anticoagulation therapy, there is a promising sign that optimal clinical outcomes can be achieved for all ethnoracial groups.
There are some limitations of this scoping review that warrant consideration. First, we chose fairly broad inclusion criteria (all anticoagulants, all study types) because a review of this type had never been performed before. This resulted in a relatively large number of included articles for a scoping review. Second, there is likely a high degree of heterogeneity among patient populations and outcomes definitions. However, as this is a scoping review with the goal to present an overview of the literature and not report on composite outcomes, a risk of bias assessment was not performed. Third is our decision to group patients into White and non-White groups for assessment of outcome directionality. In doing so, we may have missed subtle differences in outcomes between various non-White ethnoracial groups. Fourth, in our main search we included all studies that reported outcomes, but due to scope, we only reported outcome directionality for studies that statistically compared outcomes between ethnoracial groups. Finally, due to the large number of studies that required review and analysis, this was a lengthy undertaking and we are certain that additional studies have been published since the closure of our search period.
In line with the 2014 National Action Plan for Adverse Drug Event Prevention’s goal of identifying patient populations at higher risk of adverse drug events, this scoping review highlights several areas where quality of anticoagulation care can be optimized for all patients. Future research opportunities in ethnoracial differences in the quality of anticoagulation care are summarized in Table 3. While the scoping review focused exclusively on the evaluation of peer-reviewed manuscripts, the heterogeneity of terminology and methodologies identified in the published papers may have implications for national health policy relating to the quality and safety of care (e.g.the Medicare Quality Payment Program) [120]. To accurately and reliably quantify important disparities in AC-related care and support effective improvement initiatives, attention and effort will need to be invested across the full continuum of quality measure development [121], measure endorsement [122], measure selection, and status assignment within value-based payment programs (e.g., required/optional, measure weighting) [123]. The findings of the scoping review may be of utility to such efforts, and the development and implementation of suitable quality measures will likely be of value to future research efforts in this important therapeutic area.
Conclusions
Treatment guidelines do not recommend differentiating anticoagulant therapy by ethnoracial group, yet this scoping review of the literature demonstrates consistent directionality in favor of White patients over non-White patients in the domains of access to anticoagulation therapy for guideline-based indications, prescription of preferred anticoagulation therapies, and quality of anticoagulation therapy management. These data should serve as a stimulus for an assessment of current services, implementation of quality improvement measures, and inform future research to make anticoagulation care quality more equitable.
Data Availability
Data are available on request from the corresponding author.
References
Wheeler SM, Bryant AS (2017) Racial and Ethnic Disparities in Health and Health Care. Obstet Gynecol Clin North Am 44(1):1–11
Manuel JI (2018) Racial/Ethnic and Gender Disparities in Health Care Use and Access. Health Serv Res 53(3):1407–1429
Nadeem MF, Kaiser LR (2022) Disparities in Health Care Delivery Systems. Thorac Surg Clin 32(1):13–21
Wallace J et al (2021) Changes in Racial and Ethnic Disparities in Access to Care and Health Among US Adults at Age 65 Years. JAMA Intern Med 181(9):1207–1215
Churchwell K et al (2020) Call to Action: Structural Racism as a Fundamental Driver of Health Disparities: A Presidential Advisory From the American Heart Association. Circulation 142(24):e454–e468
Gomez SE et al (2023) Racial, ethnic, and sex disparities in atrial fibrillation management: rate and rhythm control. J Interv Card Electrophysiol 66(5):1279–1290
Tamirisa KP et al (2021) Racial and Ethnic Differences in the Management of Atrial Fibrillation. CJC Open 3(12 Suppl):S137–S148
Eberly LA et al (2021) Racial/Ethnic and Socioeconomic Disparities in Management of Incident Paroxysmal Atrial Fibrillation. JAMA Netw Open 4(2):e210247
Ugowe FE, Jackson LR, Thomas KL (2018) Racial and ethnic differences in the prevalence, management, and outcomes in patients with atrial fibrillation: A systematic review. Heart Rhythm 15(9):1337–1345
Xu Y, Siegal DM, Anand SS (2021) Ethnoracial variations in venous thrombosis: Implications for management, and a call to action. J Thromb Haemost 19(1):30–40
Erinne I et al (2021) Racial disparities in the treatment of aortic stenosis: Has transcatheter aortic valve replacement bridged the gap? Catheter Cardiovasc Interv 98(1):148–156
Ali A et al (2022) Racial and Ethnic Disparities in the Use of Transcatheter Aortic Valve Replacement in the State of Connecticut. Cardiovasc Revasc Med 37:7–12
Pienta MJ et al (2023) Racial disparities in mitral valve surgery: A statewide analysis. J Thorac Cardiovasc Surg 165(5):1815-1823.e8
Alkhouli M et al (2019) Racial Disparities in the Utilization and Outcomes of Structural Heart Disease Interventions in the United States. J Am Heart Assoc 8(15):e012125
Heckbert SR et al (2020) Differences by Race/Ethnicity in the Prevalence of Clinically Detected and Monitor-Detected Atrial Fibrillation: MESA. Circ Arrhythm Electrophysiol 13(1):e007698
Zakai NA et al (2014) Racial and regional differences in venous thromboembolism in the United States in 3 cohorts. Circulation 129(14):1502–1509
Lamprea-Montealegre JA et al (2021) Valvular Heart Disease in Relation to Race and Ethnicity: JACC Focus Seminar 4/9. J Am Coll Cardiol 78(24):2493–2504
Tamargo J et al (2022) Racial and ethnic differences in pharmacotherapy to prevent coronary artery disease and thrombotic events. Eur Heart J Cardiovasc Pharmacother 8(7):738–751
Kanuri SH, Kreutz RP (2019) Pharmacogenomics of Novel Direct Oral Anticoagulants: Newly Identified Genes and Genetic Variants. J Pers Med 9(1):7
Craig TJ, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland CJ Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie LK, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW (2019) Circulation 140 (2):e125–e151. https://doi.org/10.1161/CIR.000000000000066
Ortel TL et al (2020) American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism. Blood Adv 4(19):4693–4738
Stevens SM et al (2021) Antithrombotic Therapy for VTE Disease: Second Update of the CHEST Guideline and Expert Panel Report. Chest 160(6):e545–e608
Schünemann HJ et al (2018) American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv 2(22):3198–3225
Otto CM et al (2021) 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 143(5):e72–e227
National Action Plan for Adverse Drug Event Prevention (2014) Office of Disease Prevention and Health Promotion. US Department of Health and Human Services, Washington, DC
Bhakta S et al (2022) A systematic review and meta-analysis of racial disparities in deep vein thrombosis and pulmonary embolism events in patients hospitalized with coronavirus disease 2019. J Vasc Surg Venous Lymphat Disord 10(4):939-944.e3
Corbie-Smith G et al (2008) Conceptualizing race in research. J Natl Med Assoc 100(10):1235–1243
Vazquez SR, Yates NYY, McFarland MM (2022). Differences in anticoagulant care delivery according to ethnoracial group in the United States: a scoping review protocol. Open Sci Fram osf.io/eydsa. https://doi.org/10.17605/OSF.IO/9SE7H
Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H (2020) Joanna briggs institute reviewer's manual. Aromataris E, Munn Z (eds). Publisher: Joanna briggs institute. Chapter: chapter 11: scoping reviews
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8(1):19–32
Rethlefsen ML et al (2021) PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev 10(1):39
Harris PA et al (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381
McGowan J et al (2016) PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol 75:40–46
Kearon C et al (2016) Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 149(2):315–352
Lip GYH et al (2018) Antithrombotic Therapy for Atrial Fibrillation: CHEST Guideline and Expert Panel Report. Chest 154(5):1121–1201
al Taii, H. and S. Al-Kindi, Racial disparities in prescriptions of oral anticoagulants among patients with atrial fibrillation., in 24th International Atrial Fibrillation Symposium (2019) Boston. MA, USA
Bhave PD et al (2015) Race- and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Heart Rhythm 12(7):1406–1412
Chapman SA et al (2017) Adherence to treatment guidelines: the association between stroke risk stratified comparing CHADS. BMC Health Serv Res 17(1):127
Chen Q et al (2021) Prevalence and the factors associated with oral anticoagulant use among nursing home residents. J Clin Pharm Ther 46(6):1714–1728
Deitelzweig S et al (2020) Utilization of anticoagulants and predictors of treatment among hospitalized patients with atrial fibrillation in the USA. J Med Econ 23(12):1389–1400
Essien UR et al (2018) Association of Race/Ethnicity With Oral Anticoagulant Use in Patients With Atrial Fibrillation: Findings From the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation II. JAMA Cardiol 3(12):1174–1182
Essien UR et al (2021) Disparities in Anticoagulant Therapy Initiation for Incident Atrial Fibrillation by Race/Ethnicity Among Patients in the Veterans Health Administration System. JAMA Netw Open 4(7):e2114234
Essien UR, Kim N, Hausmann LR, Mor MK, Good C, Gellad WF, Fine MJ (2020) Abstract: racial and ethnic disparities in anticoagulant choice for atrial fibrillation in the veterans health administration: results from the reach-af study. J Gen Int Med J 35(1):S250–251
Essien UR et al (2022) Association of Race and Ethnicity and Anticoagulation in Patients With Atrial Fibrillation Dually Enrolled in Veterans Health Administration and Medicare: Effects of Medicare Part D on Prescribing Disparities. Circ Cardiovasc Qual Outcomes 15(2):e008389
Essien UR et al (2020) Race/Ethnicity and Sex-Related Differences in Direct Oral Anticoagulant Initiation in Newly Diagnosed Atrial Fibrillation: A Retrospective Study of Medicare Data. J Natl Med Assoc 112(1):103–108
Fohtung RB, Novak E, Rich MW (2017) Effect of New Oral Anticoagulants on Prescribing Practices for Atrial Fibrillation in Older Adults. J Am Geriatr Soc 65(11):2405–2412
Lewis WR et al (2011) Improvement in use of anticoagulation therapy in patients with ischemic stroke: results from Get With The Guidelines-Stroke. Am Heart J 162(4):692-699.e2
Martin Diaz C et al (2021) Anticoagulation After Ischemic Stroke or Transient Ischemic Attack (TIA) in the Time of Direct Oral Anticoagulation (DOAC) and Thrombectomy. Cureus 13(8):e17392
Mentias A et al (2021) Racial and Sex Disparities in Anticoagulation After Electrical Cardioversion for Atrial Fibrillation and Flutter. J Am Heart Assoc 10(17):e021674
Obi CA et al (2022) Examination of anticoagulation prescription among elderly patients with atrial fibrillation after in-hospital fall. J Thromb Thrombolysis 53(3):683–689
Piccini JP et al (2019) Adherence to Guideline-Directed Stroke Prevention Therapy for Atrial Fibrillation Is Achievable. Circulation 139(12):1497–1506
Raji MA et al (2013) National utilization patterns of warfarin use in older patients with atrial fibrillation: a population-based study of Medicare Part D beneficiaries. Ann Pharmacother 47(1):35–42
Schwartz SM et al (2019) Discriminative Ability of CHA. Am J Cardiol 123(12):1949–1954
Shahid I et al (2021) Meta-Analysis of Racial Disparity in Utilization of Oral Anticoagulation for Stroke Prevention in Atrial Fibrillation. Am J Cardiol 153:147–149
Tedla YG et al (2020) Racial Disparity in the Prescription of Anticoagulants and Risk of Stroke and Bleeding in Atrial Fibrillation Patients. J Stroke Cerebrovasc Dis 29(5):104718
Thomas KL et al (2013) Racial differences in the prevalence and outcomes of atrial fibrillation among patients hospitalized with heart failure. J Am Heart Assoc 2(5):e000200
Waddy SP et al (2020) Racial/Ethnic Disparities in Atrial Fibrillation Treatment and Outcomes among Dialysis Patients in the United States. J Am Soc Nephrol 31(3):637–649
Wetmore JB et al (2019) Relation of Race, Apparent Disability, and Stroke Risk With Warfarin Prescribing for Atrial Fibrillation in Patients Receiving Maintenance Hemodialysis. Am J Cardiol 123(4):598–604
Winkelmayer WC et al (2012) Prevalence of atrial fibrillation and warfarin use in older patients receiving hemodialysis. J Nephrol 25(3):341–353
Zahuranec DB et al (2017) Stroke Quality Measures in Mexican Americans and Non-Hispanic Whites. J Health Dispar Res Pract 10(1):111–123
Addo-Tabiri NO et al (2020) Black Patients Experience Highest Rates of Cancer-associated Venous Thromboembolism. Am J Clin Oncol 43(2):94–100
Freeman AH et al (2016) Venous thromboembolism following minimally invasive surgery among women with endometrial cancer. Gynecol Oncol 142(2):267–272
Friedman AM et al (2013) Underuse of postcesarean thromboembolism prophylaxis. Obstet Gynecol 122(6):1197–1204
Lau BD et al (2015) Eliminating Health Care Disparities With Mandatory Clinical Decision Support: The Venous Thromboembolism (VTE) Example. Med Care 53(1):18–24
Owodunni OP et al (2020) Using electronic health record system triggers to target delivery of a patient-centered intervention to improve venous thromboembolism prevention for hospitalized patients: Is there a differential effect by race? PLoS ONE 15(1):e0227339
Shah S et al (2021) Implementation of an Anticoagulation Practice Guideline for COVID-19 via a Clinical Decision Support System in a Large Academic Health System and Its Evaluation: Observational Study. JMIR Med Inform 9(11):e30743
Steinberg BA et al (2013) Early adoption of dabigatran and its dosing in US patients with atrial fibrillation: results from the outcomes registry for better informed treatment of atrial fibrillation. J Am Heart Assoc 2(6):e000535
Vaughan Sarrazin MS et al (2014) Bleeding rates in Veterans Affairs patients with atrial fibrillation who switch from warfarin to dabigatran. Am J Med 127(12):1179–1185
Nathan AS et al (2019) Racial, Ethnic, and Socioeconomic Inequities in the Prescription of Direct Oral Anticoagulants in Patients With Venous Thromboembolism in the United States. Circ Cardiovasc Qual Outcomes 12(4):e005600
Singh BP, Sitlinger A, Saber I, Thames E, Beckman M, Reyes N, Schulteis RD, Ortel T (2016) Direct oral anticoagulant usage in the treatment of venous thromboembolism across racial groups in Durham County, NC. J Gen Int Med 31:S191–S192
Schaefer JK et al (2017) Sociodemographic factors in patients continuing warfarin vs those transitioning to direct oral anticoagulants. Blood Adv 1(26):2536–2540
Lank RJ et al (2019) Ethnic Differences in 90-Day Poststroke Medication Adherence. Stroke 50(6):1519–1524
O'Brien EC, Holmes ND, Thomas L, Fonarow GC, Kowey PR, Ansell JE, Mahaffey KW, Gersh BJ, Peterson ED, Piccini JP, Hylek EM (2018) J Am Heart Assoc 7(12):e006391
Singh RR et al (2016) Adherence to Anticoagulant Therapy in Pediatric Patients Hospitalized With Pulmonary Embolism or Deep Vein Thrombosis: A Retrospective Cohort Study. Clin Appl Thromb Hemost 22(3):260–264
Yong C, Xu XY, Than C, Ullal A, Schmitt S, Azarbal F, Heidenreich P, Turakhia M (2013) Abstract 14134: racial disparities in warfarin time in INR therapeutic range in patients with atrial fibrillation: Findings from the TREAT-AF Study. Circul 128(22). https://www.ahajournals.org/doi/10.1161/circ.128.suppl_22.A14134
Chen N, Brooks MM, Hernandez I (2020) Latent Classes of Adherence to Oral Anticoagulation Therapy Among Patients With a New Diagnosis of Atrial Fibrillation. JAMA Netw Open 3(2):e1921357
Pham Nguyen TP et al (2003) Does hospitalization for thromboembolism improve oral anticoagulant adherence in patients with atrial fibrillation? J Am Pharm Assoc 60(6):986-992.e2
Patel AA et al (2013) Persistence of warfarin therapy for residents in long-term care who have atrial fibrillation. Clin Ther 35(11):1794–1804
Golwala H et al (2016) Racial/ethnic differences in atrial fibrillation symptoms, treatment patterns, and outcomes: Insights from Outcomes Registry for Better Informed Treatment for Atrial Fibrillation Registry. Am Heart J 174:29–36
Limdi NA et al (2017) Quality of anticoagulation control and hemorrhage risk among African American and European American warfarin users. Pharmacogenet Genomics 27(10):347–355
Lip GY et al (2016) Determinants of Time in Therapeutic Range in Patients Receiving Oral Anticoagulants (A Substudy of IMPACT). Am J Cardiol 118(11):1680–1684
Rao SR et al (2015) Explaining racial disparities in anticoagulation control: results from a study of patients at the Veterans Administration. Am J Med Qual 30(3):214–222
Thigpen JL, Yah Q, Beasley M, Limdi NA (2012) Abstract: racial differences in anticoagulation control and risk of hemorrhage among warfarin users. Pharmacoth 32(10):E189
Yong C et al (2016) Racial Differences in Quality of Anticoagulation Therapy for Atrial Fibrillation (from the TREAT-AF Study). Am J Cardiol 117(1):61–68
Moffett BS, Kim S, Bomgaars LR (2013) Readmissions for warfarin-related bleeding in pediatric patients after hospital discharge. Pediatr Blood Cancer 60(9):1503–1506
Rose AJ et al (2013) Gaps in monitoring during oral anticoagulation: insights into care transitions, monitoring barriers, and medication nonadherence. Chest 143(3):751–757
Mahle WT et al (2011) Management of warfarin in children with heart disease. Pediatr Cardiol 32(8):1115–1119
Meade M et al (2011) Impact of health disparities on staff workload in pharmacist-managed anticoagulation clinics. Am J Health Syst Pharm 68(15):1430–1435
Aguilar F et al (2021) Off-label direct oral anticoagulants dosing in atrial fibrillation and venous thromboembolism is associated with higher mortality. Expert Rev Cardiovasc Ther 19(12):1119–1126
Jellinek-Cohen SP, Li M, Husk G (2018) Enoxaparin dosing errors in the emergency department. World J Emerg Med 9(3):195–202
Triller DM et al (2015) Trends in Warfarin Monitoring Practices Among New York Medicare Beneficiaries, 2006–2011. J Community Health 40(5):845–854
Akhtar T et al (2020) Factors associated with bleeding events in patients on rivaroxaban for non-valvular atrial fibrillation: A real-world experience. Int J Cardiol 320:78–82
Cires-Drouet RS et al (2022) Prevalence and clinical outcomes of hospitalized patients with upper extremity deep vein thrombosis. J Vasc Surg Venous Lymphat Disord 10(1):102–110
Doucette K et al (2020) Efficacy and Safety of Direct-Acting Oral Anticoagulants (DOACs) in the Overweight and Obese. Adv Hematol 2020:3890706
Gu K et al (2021) Racial disparities among Asian Americans with atrial fibrillation: An analysis from the NCDR® PINNACLE Registry. Int J Cardiol 329:209–216
Yamashita Y et al (2018) Asian patients versus non-Asian patients in the efficacy and safety of direct oral anticoagulants relative to vitamin K antagonist for venous thromboembolism: A systemic review and meta-analysis. Thromb Res 166:37–42
Di Nisio M et al (2016) Risk of major bleeding in patients with venous thromboembolism treated with rivaroxaban or with heparin and vitamin K antagonists. Thromb Haemost 115(2):424–432
Hernandez I et al (2015) Risk of bleeding with dabigatran in atrial fibrillation. JAMA Intern Med 175(1):18–24
Majeed A et al (2016) Bleeding events with dabigatran or warfarin in patients with venous thromboembolism. Thromb Haemost 115(2):291–298
Hankey GJ et al (2014) Intracranial hemorrhage among patients with atrial fibrillation anticoagulated with warfarin or rivaroxaban: the rivaroxaban once daily, oral, direct factor Xa inhibition compared with vitamin K antagonism for prevention of stroke and embolism trial in atrial fibrillation. Stroke 45(5):1304–1312
Kobayashi L et al (2017) Novel oral anticoagulants and trauma: The results of a prospective American Association for the Surgery of Trauma Multi-Institutional Trial. J Trauma Acute Care Surg 82(5):827–835
Gencer B et al (2022) Edoxaban versus Warfarin in high-risk patients with atrial fibrillation: A comprehensive analysis of high-risk subgroups. Am Heart J 247:24–32
Chen N et al (2021) Joint Latent Class Analysis of Oral Anticoagulation Use and Risk of Stroke or Systemic Thromboembolism in Patients with Atrial Fibrillation. Am J Cardiovasc Drugs 21(5):573–580
Kabra R et al (2015) Effect of race on outcomes (stroke and death) in patients >65 years with atrial fibrillation. Am J Cardiol 116(2):230–235
Kim MH, Xu L, Puckrein G (2018) Patient Diversity and Population Health-Related Cardiovascular Outcomes Associated with Warfarin Use in Atrial Fibrillation: An Analysis Using Administrative Claims Data. Adv Ther 35(11):2069–2080
Abu-Zeinah G, Oromendia C, DeSancho MT (2019) Thrombotic risk factors in patients with antiphospholipid syndrome: a single center experience. J Thromb Thrombolysis 48(2):233–239
Banala SR et al (2017) Discharge or admit? Emergency department management of incidental pulmonary embolism in patients with cancer: a retrospective study. Int J Emerg Med 10(1):19
LaDuke ZJ et al (2019) Association of mortality among trauma patients taking preinjury direct oral anticoagulants versus vitamin K antagonists. Surgery 166(4):564–571
Moreland CJ et al (2013) Anticoagulation education: do patients understand potential medication-related emergencies? Jt Comm J Qual Patient Saf 39(1):22–31
Bamgbade BA et al (2021) Differences in Perceived and Predicted Bleeding Risk in Older Adults With Atrial Fibrillation: The SAGE-AF Study. J Am Heart Assoc 10(17):e019979
Webb D et al (2019) Patient Satisfaction With Venous Thromboembolism Treatment. Clin Appl Thromb Hemost 25:1076029619864663
Kamath CC et al (2021) Cost Conversations About Anticoagulation Between Patients With Atrial Fibrillation and Their Clinicians: A Secondary Analysis of a Randomized Clinical Trial. JAMA Netw Open 4(7):e2116009
U.S. Census Bureau. [cited 2023 10/20/23]; Available from: https://www.census.gov/quickfacts/fact/note/US/RHI625222#:~:text=Asian.,Japan%2C%20Korea%2C%20or%20Vietnam.
Fain KM et al (2021) Race and ethnicity reporting for clinical trials in ClinicalTrials.gov and publications. Contemp Clin Trials 101:106237
American Psychological Association Ethnic and racial minorities & socioeconomic status. 3/22/24]; Available from: https://www.apa.org/pi/ses/resources/publications/minorities#:~:text=The%20relationship%20between%20SES%2C%20race,SES%2C%20race%2C%20and%20ethnicity. Accessed 22 Mar 2024
Braveman PA et al (2010) Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health 100 Suppl 1(Suppl 1):186–96
Wheelock KM et al (2021) Clinician Trends in Prescribing Direct Oral Anticoagulants for US Medicare Beneficiaries. JAMA Netw Open 4(12):e2137288
Barnes GD et al (2015) National Trends in Ambulatory Oral Anticoagulant Use. Am J Med 128(12):1300–5.e2
Iyer GS et al (2023) Trends in the Use of Oral Anticoagulants for Adults With Venous Thromboembolism in the US, 2010–2020. JAMA Netw Open 6(3):e234059
MACRA Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). 03/19/24]; Available from: https://www.cms.gov/medicare/quality/value-based-programs/chip-reauthorization-act. Accessed 19 Mar 2024
Blueprint Measure Lifecycle Overview. 03/19/2024]; Available from: https://mmshub.cms.gov/blueprint-measure-lifecycle-overview. Accessed 19 Mar 2024
Endorsement and Maintenance (E&M) Guidebook. 3/19/24]; Available from: https://p4qm.org/sites/default/files/2023-12/Del-3-6-Endorsement-and-Maintenance-Guidebook-Final_0_0.pdf. Accessed 19 Mar 2024
Measure Implementation. 3/19/24]; Available from: https://mmshub.cms.gov/measure-lifecycle/measure-implementation/selection. Accessed 19 Mar 2024
Acknowledgements
The authors wish to acknowledge the following individuals for their work in screening articles for this scoping review: April Allen, PharmD, CACP; Allison Burnett, PharmD, PhC, CACP; Stacy Ellsworth, RN, MSN, CCRC; Danielle Jenkins, MBA, RN, BSN, CRNI; Amanda Katz, MBA; Lea Kistenmacher, Julia Mulheman, PharmD; Surhabi Palkimas, PharmD, MBA; Terri Schnurr, RN, CCRC; Deborah Siegal, MD, MSc, FRCPC; Kimberly Terry, PharmD, BCPS, BCCCP; and Terri Wiggins, MS.
The authors wish to acknowledge the support of the Anticoagulation Forum in the development of this manuscript. The Anticoagulation Forum is a non-profit organization dedicated to improving the quality of care for patients taking antithrombotic medications.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Sara Vazquez, Naomi Yates, and Mary McFarland. Data collection and analysis were performed by Sara Vazquez, Naomi Yates, Craig Beavers, and Darren Triller. The first draft of the manuscript was written by Sara Vazquez and all authors edited subsequent drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Dr. Vazquez discloses that she is a member of the Anticoagulation Forum Advisory Council and an editorial consultant for UptoDate, Inc.
Dr. Yates has no conflicts of interest to disclose.
Dr. Beavers has no conflicts of interest to disclose.
Dr. Triller has no conflicts of interest to disclose.
Ms. McFarland has no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vazquez, S.R., Yates, N.Y., Beavers, C.J. et al. Differences in quality of anticoagulation care delivery according to ethnoracial group in the United States: A scoping review. J Thromb Thrombolysis 57, 1076–1091 (2024). https://doi.org/10.1007/s11239-024-02991-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-024-02991-2