Abstract
Patients diagnosed with lymphoma or multiple myeloma are at elevated risk of venous thromboembolism (VTE). Optimum risk stratification and effective thromboprophylaxis can only be achieved through the development of a multiple-specific risk score that successfully captures all aspects of the heterogeneous prothrombotic environment existing in these patients. Our aim was to identify risk factors for thrombosis and suggest an improved tool combining clinical data, thrombo-inflammatory biomarkers and genetic (Thrombo inCode® test) variables for predicting thrombotic risk in patients with lymphoma and multiple myeloma. A prospective longitudinal study was conducted on newly-diagnosed lymphoma and multiple myeloma patients who presented at our institution between February 2020 and January 2021. The study included 47 patients with lymphoma and 16 patients with multiple myeloma. We performed a follow-up of 1 year or until September 2021. The incidence of venous thrombosis and associated risk factors were analysed, including the genetic Thrombo inCode® test. Khorana and ThroLy scores for lymphoma patients and IMPEDE VTE score for myeloma patients were calculated. At a median follow-up of 9.1 months, VTE incidence was 9.5% (6/63), with 4 and 2 patients with lymphoma and myeloma who developed the events, respectively. Univariate analysis showed that the incidence of thrombosis was significantly higher in patients with ECOG ≥ 2 and prior immobility. Median factor VIII levels were significantly higher in patients with thrombosis (with increased values in all of them). Moreover, there was a trend in genetic variant rs5985 (factor XIII) as a protective factor, and a trend to higher thrombotic risk in patients with factor V Leiden, rs2232698 variant (serpinA10), low total protein S activity, elevated D-dimer, aggressive lymphoma and treatment with dexamethasone. The results of our study demonstrate promise for the potential use of widely accessible markers to increase precision in risk prediction for VTE in patients with lymphoma and multiple myeloma, particularly ECOG ≥ 2, immobility and higher factor VIII levels, as well as lymphoma aggressiveness, treatment with dexamethasone and the haemostatic biomarkers D-dimer and total protein S activity. Additionally, genetic variants factor V Leiden, serpinA10 rs2232698 and factor XIII-A Val34Leu warrant further investigation for use in the research setting.
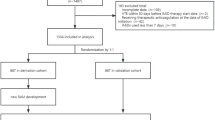
Graphical Abstract

Similar content being viewed by others
Introduction
Patients with cancer have a 4–eightfold greater risk of experiencing VTE compared to the general population [1], being the second cause of death in cancer patients. It also causes worsened patients’ morbidity, a delay in planification of systemic therapies and an increase of health-care costs [2]. Patients are exposed to a higher risk of thrombotic complications during the first months after cancer diagnosis and start of antineoplastic therapy [1, 3]. The incidence of VTE varies according to patient-related, disease-related and treatment-related factors [2], with an estimated heritability of about 60% [4]. In lymphoma, the rate of thrombosis ranges from 1.5% up to 59.5%. The basis of this variability probably lies in the heterogeneity of aggressiveness, tumour burden and location of the different types of lymphomas, with a demonstrated higher risk in patients with aggressive non-Hodgkin lymphoma (NHL) than in those with indolent NHL or Hodgkin lymphoma (HL) [1]. The incidence of thrombosis in patients diagnosed with multiple myeloma (MM) is 8.7 per 1000 person-years [5], with a greater risk in patients treated with immunomodulatory agents (IMiDs), especially in combination with dexamethasone or anthracyclines [6].
Thromboembolic complications can be prevented by primary thromboprophylaxis, which is included as a recommendation in guidelines for VTE management in cancer patients. However, pharmacological thromboprophylaxis increases the risk of haemorrhage, especially in certain populations (e.g. patients with thrombocytopenia). In ambulatory patients, it is recommended to be cautious and to identify patients who are at higher risk by using risk assessment models (RAMs), so that thromboprophylaxis is justified in certain cases [7]. The most consolidated predictive model in cancer patients is Khorana score, which is mainly focused on solid tumours [8]. More recently, other clinical RAMs have been proposed in hematological patients, such as ThroLy [9] in lymphoma and IMPEDE VTE [10] in MM. However, it remains unclear whether these RAMs should be generally recommended for identification of patients who are at major risk of thrombosis [7]. In order to approach this unmet need, novel scores including clinical and genetic variables have been developed and have shown promising results. These scores are TiC-Onco [11] and ONCOTHROMB [12] for patients with solid tumours, and TiC-LYMPHO [13] for lymphoma patients.
In the present work, we hypothesized that a personalized approach to the thrombotic risk based on the inclusion of genetic and acquired thrombophilia parameters in predictive scores could better identify those patients diagnosed with lymphoma or MM who would benefit most from thromboprophylaxis. The aim of this study was to analyse the incidence of venous thrombosis in a real-world cohort of lymphoma and MM patients and to identify clinical, laboratory or genetic variables that could potentially increase their thrombotic risk. Our results suggest that a new risk score that includes a combination of clinical, prothrombotic biomarkers and genetic (Thrombo inCode®- TiC) variables could be developed in order to better predict which patients should receive primary thromboprophylaxis.
Methods
Study design and participants
This is a prospective, longitudinal study that includes patients over 18 years of age diagnosed with lymphoma (based on the World Health Organization 2016 classification) [14] or MM (based on the 2014 International Myeloma Working Group updated criteria [15]) between February 2020 and June 2021. Follow-up was performed during the next 12 months following cancer diagnosis or until September 2021. For the analysis, lymphomas were classified according to the histological diagnosis and NHL were grouped according to their clinical aggressiveness into indolent and aggressive. Aggressive lymphomas included diffuse large B-cell lymphoma, high grade B-cell lymphoma, mantle cell lymphoma, T-cell lymphomas and follicular lymphomas grade 3B. Indolent lymphomas included marginal zone lymphoma, lymphoplasmacytic lymphoma and follicular lymphoma grade 1-3A. Patients diagnosed with monoclonal gammopathy of undetermined significance, chronic lymphocytic leukemia/small lymphocytic lymphoma or cutaneous lymphomas with no systemic manifestation were excluded.
This study was approved by the local ethics committee and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its latter amendments. Informed consent was obtained from all patients before inclusion in the study.
Follow-up and diagnosis of thromboembolic events
VTE symptoms were evaluated at baseline and regular follow-up visits throughout the first year. Apart from routine visits, the electronic health record was reviewed at 3, 6 and 12 months from disease diagnosis. Research team analysed all emergent visits and hospital admissions. When a thrombotic episode occurred, this was appropriately registered.
There was no routine screening for VTE. Objective imaging methods were performed to confirm or exclude the diagnosis only when a patient developed symptoms of VTE. Duplex ultrasound was applied for diagnosis of deep vein thrombosis (DVT), and spiral computed tomography scan was applied for diagnosis of pulmonary embolism (PE).
Sample genotyping
DNA was obtained from blood samples extracted at the time of diagnosis. These were genotyped using the Thrombo inCode kit (Gen inCode), a real-time PCR method that analyses 12 single nucleotide polymorphisms (SNPs) known to be associated to VTE (Table S1 in Supplementary Material) [4]. A score related to thrombosis probability was calculated through TiC test, based on clinical and genetic variables.
Prothrombotic biomarkers
At the time of cancer diagnosis, blood samples were obtained in order to analyse the laboratory parameters, including blood cell counts and D-dimer, fibrinogen and inflammatory markers values (C reactive protein – CRP, lactate dehydrogenase – LDH, albumin). Acquired/ Plasmatic thrombophilia testing consisted of: lupus anticoagulant, anticardiolipin IgG and IgM antibodies, levels of coagulation factors VIII (FVIII) and XII, activity levels of natural anticoagulant proteins (protein S, protein C and antithrombin III) and free protein S levels. Patients who developed a thrombotic event at the same time of cancer diagnosis were excluded for analysis of plasmatic thrombophilia. Later on, samples were extracted at 3, 6 and 12 months from diagnosis, with fibrinogen and D dimer testing. Moreover, in patients who developed venous thrombosis, blood cell counts, D dimer and fibrinogen were measured at this time.
Clinical risk factors
Data for demographic and clinical variables that could potentially be associated with VTE were extracted at diagnosis, based in previous studies concerning lymphoma and MM patients [9, 10, 13, 16]. These included patient characteristics (age, sex, race, personal or family history of thrombosis, body mass index (BMI), ECOG performance status, comorbidities, recent (< 6 weeks) immobility period, hospitalization in the last 12 weeks, acute infection, rheumatologic disorder, baseline antithrombotic therapy and type of drug used), lymphoma characteristics (histological type, stage, bulky disease, mediastinal or central nervous system – CNS – involvement, extranodal disease and B symptoms) and multiple myeloma characteristics (paraprotein secretion and type of protein involved, International Scoring System (ISS) stage and pelvic, hip or femur fracture). In this study, race was classified as White, Black, American Indian/ Alaska Native or Asian Pacific Islander according to SEER Race Recode [17]. Treatment variables were also recorded at diagnosis and updated during follow-up: use of recombinant erythropoietin (EPO), steroids (type of drug and dosage), anthracyclines, cyclophosphamide, lenalidomide, bortezomib or central venous catheter (CVC) (mainly peripherally-inserted central venous catheter (PICC) in our series).
Performance of predictive scores
At the time of diagnosis, Khorana algorithm was performed for patients with lymphoma, and ThroLy score was tested in the same subpopulation after 1 cycle of antineoplastic therapy. In patients with MM, IMPEDE VTE was performed at cancer diagnosis. Patients who developed a thrombotic event at the same time of cancer diagnosis were excluded for this analysis.
Statistical analysis
Continuous variables were recorded as median (interquartile range) and categorical variables as proportions. Univariate association between either clinical, laboratory or genetic variables and thrombosis was determined by T-test or Mann–Whitney U test for continuous variables and X2 or Fisher tests for categorical variables. The correlation between two continuous variables was analysed with Pearson’s r or Spearman rank correlation coefficients. For categorical variable D-dimer, ROC (Receiver Operating Characteristic) curves were used to select the cut-point that maximizes sensitivity and specificity (D-dimer 1.22 mg/L). Multiple comparisons between paired continuous variables were performed with paired T-test or Wilcoxon signed-rank test, and Holm method was used for p value correction. All reported p values were 2-sided and were considered significant at the 5% significance level. The statistical analysis was performed using IBM SPSS Statistics software (version 25.00) (IBM Corp., Armonk, NY, USA) [18]. The score derived from the TiC test was calculated by multivariate logistic regression analysis of clinical and genetic variables, using the Thrombo inCode kit application [19].
Results
Patients characteristics
The study population included 47 (74.6%) patients diagnosed with lymphoma and 16 (25.4%) patients diagnosed with MM. The median patient age was 64 years (interquartile range (IQR), 51–72 years), with 36 (57.1%) men. Patients’ race distribution was: 62 White and 1 American Indian. Twenty-two (34.9%) patients were on antithrombotic therapy at baseline: 15 (23.8%) were on anticoagulant drugs, one of them on a therapeutic dose, 4 (6.3%) were on antiplatelet drugs and 3 (4.8%) were on both. The most common reason for antithrombotic therapy was the initiation of lenalidomide in 8 (36.4%) patients, all of whom were diagnosed with MM. Among patients diagnosed with lymphoma, the majority (87.2%) had NHL, with 41 cases, and the majority of these were high-grade NHL (70.7%). Ann-Arbor stage was ≥ 3 in 30 (63.8%) patients and no CNS involvement was observed. Among patients diagnosed with MM, the majority had ISS III (62.5%) and 7 (43.8%) had IgG isotype. Other characteristics of the population with and without VTE are shown in Table 1 and Tables S2 and S3 in Supplementary Material.
Thromboembolic events
At a median follow-up of 9.1 months (IQR 5.1–12), 6 (9.5%) patients developed VTE (Fig. 1), of which 4 had been diagnosed with lymphoma and 2 with myeloma. To date, after 3 years since the first patient was included, no other thrombotic episodes have appeared. In the majority of patients (5/6), thrombosis occurred during the first 3 months since cancer diagnosis, with a median time to thrombosis of 36 days (IQR 4–92). Two of the 6 patients experienced the event before the start of antineoplastic therapy. Detailed description of VTE episodes is shown in Table 2. Regarding laboratory markers, a majority of the patients had elevated fibrinogen (3/5) and D-dimer (3/4) values at the time of the episode, with a median of 443 mg/dL (IQR 366–512) and 0.51 mg/L (0.49–3.04), respectively.
The median duration of full-dose anticoagulation was 6.4 months (IQR 6.1–6.5). At this time, the majority (5/6) discontinued anticoagulation due to non-active cancer.
Genetic analysis (Thrombo inCode®)
The TiC tool showed that median calculated genetic score was higher in the patients who developed VTE (1.86; IQR 0.70–8.30) than in those who did not (1.38; IQR 0.54–3.09); p = 0.470. The most frequent genetic variants were mutations in FXII (36.5%) and FXIII (31.7%) genes and presence of A1 haplotype (30.2%). FVL and SERPINA10 mutations were more prevalent in VTE patients compared to non-VTE patients. The heterozygous or homozygous mutated forms in FXIII gene were more frequent in patients who did not develop thrombosis than in those with events; none of the 16 patients who had the heterozygous mutation developed thrombosis (Table 1).
Other risk factors for thromboembolism
Regarding haemostatic biomarkers, FVIII > 200% and low total PS activity were the most common abnormalities in the plasmatic thrombophilia study (60.7% and 36.1% of the population, respectively). In patients with thrombosis, elevated FVIII was present in 5 out of 5 cases, and reduced PS activity was present in 3 out of 5 cases (Table 1). Median FVIII levels were significantly higher in patients who developed VTE (393%; IQR 246–344) compared to those who did not (211%; IQR 157–241); p = 0.01. (Fig. 2). In addition, median total PS activity was lower in patients who developed VTE (55%; IQR 43–86) compared to those without VTE (82%; IQR 62–106); p = 0.096. There was a strong significant correlation between median total PS activity and median free PS (r = 0.787; p < 0.001). However, median free PS was not reduced in patients with thrombosis (91%; IQR 68–96) compared to those without events (86%; IQR 69–110); p = 0.577.
Furthermore, D-dimer and fibrinogen had high values more frequently in VTE group than in non-VTE patients (Table 1). We found that the median D-dimer concentration was slightly higher in patients who experienced VTE (1.96 mg/L; IQR 1.16–3.72) compared to those who did not (0.65 mg/L; IQR 0.39–2.03); p = 0.139. Fibrinogen levels were also slightly higher in the VTE group (median 473 mg/dL; IQR 317–556) compared to the non-VTE group (median 371 mg/dL; IQR 324–471); p = 0.332. Finally, patients with thrombosis exhibited abnormal results in values of platelets, CRP and albumin more frequently than non-VTE patients (Table 1).
Comparison of coagulation parameters at diagnosis and during follow-up showed significant differences between baseline D-dimer and D-dimer at 3, 6 and 12 months of follow-up (Table S4 in Supplementary Material). Other comparisons of coagulation parameters during follow-up did not show interesting results (data not shown).
Univariate regression analysis demonstrated that patients with an impaired performance status, measured by an ECOG ≥ 2, experienced VTE at a significantly higher frequency than patients with ECOG < 2 (Fig. 3). In the same way, patients with immobility in the 6 weeks prior to cancer diagnosis had thrombosis more frequently than the other patients (30% vs. 5.7%; p = 0.046).
Other clinical variables showed a tendency towards an increase in thrombotic risk, such as an older age, female sex or BMI ≥ 30 kg/m2 (Table 1). All of the patients diagnosed with lymphoma who developed thrombosis had aggressive NHL (100% vs. 67.6% for those without VTE) and Bulky disease was more frequent in thrombosis group than in non-VTE one (50% vs. 18.6%) (Table S2 in Supplementary Material). Regarding treatment characteristics in the whole population, more patients in the VTE group had a permanent CVC (50% vs. 29.6%) or received steroids (100% vs. 83.3%), especially dexamethasone, anthracyclines (75% vs. 59.3%) or cyclophosphamide (100% vs. 68.5%). On the contrary, antithrombotic prophylaxis was not associated with a lower VTE incidence compared to patients with no thromboprophylaxis (9.8% vs. 9.1%) (Table 1). In the same way, patients diagnosed with MM who received lenalidomide-based therapies did not show a higher risk of VTE compared to those who received other treatments (data not shown).
Finally, the RAMs analysed (Khorana, ThroLy and IMPEDE VTE) did not manage to adequately predict thrombotic risk in our population (Table S5 in Supplementary Material).
Discussion
An integrated evaluation of multiple risk factors is likely to be the standard for multifactorial diseases such as cancer-associated thrombosis (CAT). To the best of our knowledge, our study is the first to conduct a prospective and comprehensive study of several clinical, thrombo‐inflammatory, and genetic variables associated with VTE to identify lymphoma and MM patients at risk for CAT. Our findings show the risk contribution of two clinical risk factors, namely ECOG ≥ 2 and immobility in the 6 weeks prior to the diagnosis of malignancy, as well as increased levels of FVIII. The presence of a low total PS activity and two genetic variants, namely factor V Leiden and rs2232698 (serpinA10), showed a tendency to a higher incidence of thrombosis. Interestingly, the genetic variant rs5985 (factor XIII) was found to have a slight protective effect against thrombosis. Our study introduces new variables which have the potential to improve the accuracy of thrombosis risk models and guide thromboprophylaxis in lymphoma and MM patients.
The incidence of VTE in the present population at 9 months of follow-up was 8.5% and 12.5% in patients diagnosed with lymphoma and MM, respectively; these figures are consistent with the range reported in a recent review for the same follow-up period (20). This finding supports the observation that the highest incidence of VTE occurs within the first 3 months after cancer diagnosis [9, 20, 21], which can be attributed to the higher tumour burden and initiation of antineoplastic treatment [3, 9]. Notably, all VTE events among patients with lymphoma occurred in patients diagnosed with aggressive lymphomas, as previously reported [22]. This suggests that the lymphoma aggressiveness is a major factor contributing to the risk of VTE.
Corresponding to several previous findings [9, 23,24,25,26], clinical RAMs (Khorana and ThroLy scores in lymphoma, and IMPEDE VTE in MM) have not demonstrated satisfactory thrombotic prediction performance in our patients with lymphoma and MM. One possible explanation to this could be the high rate of antithrombotic prophylaxis in our patients. Despite the lack of association between thromboprophylaxis and VTE in our population, we cannot firmly conclude that thromboprophylaxis had no influence in preventing thrombosis and in the prediction performed by the RAMs. Therefore, optimum risk stratification can only be achieved through the development of a lymphoma and MM-specific risk score that can successfully capture all aspects of the heterogeneous prothrombotic environment that exists in these patients.
Among the strengths of this study is the comprehensive analysis of 12 genetic variants that have been previously identified in genome-wide analysis as being associated with VTE in both the general population and patients with solid tumours [4, 11, 12]. Consistent with the findings of previous studies conducted in patients with solid tumours [11], our study also found that patients with lymphoma and MM who had two specific genetic variants (factor V Leiden and SERPINA10 variants) had a higher incidence of VTE. In line with our results, factor V Leiden has previously demonstrated to confer a higher thrombotic risk in oncological patients, having a synergistic interaction with cancer [27]. The prothrombotic mechanism of this variant is explained by the conformational change in the binding site between factor V and activated PC (aPC), increasing resistance of activated factors V and VIII to degradation by aPC ([28]. Moreover, cancer could additionally increase thrombotic risk, by generating an acquired resistance to aPC [29].
Regarding SERPINA10 mutation, a threefold risk of developing VTE has been demonstrated in a prior investigation [30]. The proposed mechanism for this is the impaired function of SERPINA10 molecule as potent inhibitor of activated factors X and XI [30, 31].
Our study supports the findings of a meta-analysis [32], and suggests that the FXIII-A Val34Leu mutation, which is present in approximately 25% of European Caucasians, provides a slight protective effect against VTE. The proposed mechanism for this effect is interesting. In plasmas with normal fibrinogen levels, the Leu34 allele produces clots with thinner fibers and decreased permeability, whereas in plasmas with high fibrinogen, it produces clots with thicker fibers, and increased permeability and susceptibility to fibrinolysis [33]. These observations indicate that both FXIII genotype and plasma fibrinogen concentration should be considered when calculating thrombosis risk in population studies.
Emerging evidence suggests that there are cancer-type-specific haemostatic biomarkers of VTE [34,35,36]. Our analysis revealed that lymphoma and MM patients with VTE had higher levels of D-dimer and FVIII, as well as a lower total PS activity, overall suggesting a predominantly thrombotic state. Moreover, we have observed that almost 80% of our patients displayed one of these hypercoagulation abnormalities. This subset of patients did indeed exhibit a higher rate of thrombosis.
These findings are in accordance with a recent review on the pathophysiological mechanisms underpinning thrombosis in untreated lymphoma and leukemia patients with active disease, which concluded that these patients appear to display a hypercoagulable phenotype including significant elevations in FVIII and D-dimer levels and reduced protein S levels. The etiology of these haemostatic abnormalities is unclear, with possible causative mechanisms including a combination of chronic endothelial activation and dysfunction, increased bone marrow angiogenesis, and disturbances in the VWF/ADAMTS‐13 axis [37]. Other potential contributors to the hypercoagulable profile seen in lymphoma and MM patients include elevations in fibrinogen levels. However, the relative effect and overall contribution of this abnormality towards VTE occurrence in lymphoma and MM patients has not yet been fully determined [38, 39]. The use of these haemostatic biomarkers for prediction of VTE in patients with lymphoma and MM warrants further investigation in prospective trials [40, 41].
Importantly, in our study, an impaired performance status measured by an ECOG ≥ 2 and a period of immobility in the 6 weeks prior to malignancy diagnosis were significantly associated to VTE. Similarly, several studies reported an ECOG > 1 or bed rest for more than 3 days as risk factors for thrombosis in patients with lymphoma or MM [9, 13, 42, 43]. A potential explanation for this is that a reduction of the daily activity, with partial or complete immobilization, could promote the deceleration of blood flow in the venous bed [42]. Other clinical factors that in our investigation showed a tendency to higher thrombotic risk (bulky disease in lymphoma patients and treatment with dexamethasone) have already been associated to an increased thrombotic risk in prior publications from lymphoma and MM populations [10, 42, 44].
We acknowledge limitations of our study. We recognize that this is a pilot study with a small number of patients, and due to this, a proportional low number of thrombotic episodes. As a consequence, we could not manage to perform a multivariate analysis to confirm the associations found or other associations between the risk factors included and thrombosis. The difficulty in the comparison of our results with respect to other works is possibly derived from the small size of our cohort. Moreover, haemostatic biomarkers have important limitations for clinical implementation as of their low specificity.
Conclusion
From the aforementioned data, adjunctive clinical risk factors, biomolecular markers, and genetic variants assessment could all ameliorate VTE prediction, while the introduction of novel computational analyses could help with gaining knowledge from available datasets to obtain accurate and precise personalized risk estimates in lymphoma and MM patients. Our data indicate that prediction of VTE in lymphoma and MM patients may be more accurate if a limited set of genetic predictors (FV rs6025, serpinA10 rs2232698 and FXIII-A Val34Leu), clinical predictors (ECOG, immobilization, the aggressiveness of the neoplasia and treatment with dexamethasone), and haemostatic biomarkers (D-dimer, FVIII and total PS activity) are included in a new risk score, which could contribute to personalized, risk-stratified patient management in the future. The results could change clinical practice and have an important impact in national health systems.
Data Availability
The datasets presented in this article are not openly available because the data are part of an ongoing study at this centre.
References
Antic D, Jelicic J, Vukovic V, Nikolovski S, Mihaljevic B (2018) Venous thromboembolic events in lymphoma patients: Actual relationships between epidemiology, mechanisms, clinical profile and treatment. Blood Rev 32(2):144–158
Gervaso L, Dave H, Khorana A (2021) Venous and arterial thromboembolism in patients with cancer. JACC: CardioOncology 3(2):173–190
Bradbury CA, Craig Z, Cook G, Pawlyn C, Caims DA, Hockaday A, Paterson A, Jenner MW, Jones JR, Drayson MT, Owen RG, Kaiser MF, Gregory WM, Davies FE, Child JA, Morgan GJ, Jackson GH (2020) Thrombosis in patients with myeloma treated in the myeloma IX and myeloma XI phase 3 randomized controlled trials. Blood 136(9):1091–1104. https://doi.org/10.1182/blood.2020009029
Soria J, Morange P, Vila J, Souto J, Moyano M, Trégouët D, Mateo J, Saut N, Salas E, Elosua R (2014) Multilocus genetic risk scores for venous thromboembolism risk assessment. J Am Heart Assoc 3(5):e001060
Kristinsson SY, Fears TR, Gridley G, Turesson I, Mellqvist UH, Bjorkholm M, Landgren O (2008) Deep vein thrombosis after monoclonal gammopathy of undetermined significance and multiple myeloma. Blood 112(9):3582–3586
Boyle E, Fouquet G, Manier S, Gauthier J, Noel M, Borie C, Facon T, Elalamy I, Leleu X (2012) Immunomodulator drug-based therapy in myeloma and the occurrence of thrombosis. Expert Rev Hematol 5(6):619–629
Falanga A, Ay C, Di Nisio M, Gerotziafas G, Langer F, Lecumberri R, Mandala M, Maraveyas A, Pabinger I, Jara-Palomares L, Sinn M, Syrigos K, Young A, Jordan K, on behalf of the ESMO Guidelines Committee (2023) Venous thromboembolism in cancer patients: ESMO clinical practice guideline. Ann Oncol 34:452. https://doi.org/10.1016/j.annonc.2022.12.014
Khorana AA, Kuderer NM, Culakova E, Lyman GH, Francis CW (2008) Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 111(10):4902–4907
Antic D, Milic N, Nikolovski S, Todorovic M, Bila J, Djurdjevic P, Andjelic B, Djurasinovic V, Sretenovic A, Vukovic V, Jelicic J, Hayman S, Mihaljevic B et al (2016) Development and validation of multivariable predictive model for thromboembolic events in lymphoma patients. Am J Hematol 91(10):1014–1019
Sanfilippo K, Luo S, Wang T, Fiala M, Schoen M, Wildes T et al (2019) Predicting venous thromboembolism in multiple myeloma: development and validation of the IMPEDE VTE score. Am J Hematol 94(11):1176–1184
Muñoz Martín AJ, Ortega I, Font C, Pachón V, Castellón V, Martínez-Marín V, Salgado M, Martínez E, Calzas J, Rupérez A, Souto JC, Martín M, Salas E, Soria JM (2018) Multivariable clinical-genetic risk model for predicting venous thromboembolic events in patients with cancer. Br J Cancer 118(8):1056–1061
Muñoz A, Ay C, Grilz E, López S, Font C, Pachón V, Castellón V, Martínez-Marín V, Salgado M, Martínez E, Calzas J, Ortega L, Rupérez A, Salas E, Pabinger I, Soria JM (2023) A clinical-genetic risk score for predicting cancer-associated venous thromboembolism: A development and validation study involving two independent prospective cohorts. J Clin Oncol 41:2911
Bastos-Oreiro M, Ortiz J, Pradillo V, Salas E, Martínez-Laperche C, Muñoz A, Buño I, Díez-Martín JL, Soria JM, Pascual IC (2021) Incorporating genetic and clinical data into the prediction of thromboembolism risk in patients with lymphoma. Cancer Med 10(21):7585–7592
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Arber DA, Hasserjian RP, Le Beau MM, Orazi A, Siebert R (2017) WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (Revised 4th edition). Lyon: International Agency for Research on Cancer
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos M-V, Kumar S, Hillengass J, Kastritis E, Richardson P, Landgren O, Paiva B, Dispenzieri A, Weiss B, LeLeu X, Zweegman S, Lonial S, Rosinol L, Zamagni E, Jagannath S, Sezer O, Kristinsson SY, Caers J, Usmani SZ, Lahuerta JJ, Johnsen HE, Beksac M, Cavo M, Goldschmidt H, Terpos E, Kyle RA, Anderson KC, Durie BGM, San Miguel J (2014) International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15(12):e538
Li A, Wu Q, Luo S, Warnick G, Zakai N, Libby E et al (2019) Derivation and validation of a risk assessment model for immunomodulatory drug-associated thrombosis among patients with multiple myeloma. J Natl Compr Canc Netw 17(7):840–847
Race and Hispanic ethnicity changes - seer documentation [Internet]. SEER. Available from: https://seer.cancer.gov/seerstat/variables/seer/race_ethnicity/. Accessed 26 Jan 2023
IBM documentation. Available from: https://www.ibm.com/docs/en/spss-statistics/25.0.0. Accessed 26 Jan 2023
Bienvenido a SITAB [Internet]. sitab. [cited 2023Jan26]. Available from: https://sitabapp.genincode.com/sitab/Account/Login. Accessed 26 Jan 2023
Otasevic V, Mihaljevic B, Milic N, Stanisavljevic D, Vukovic V, Tomic K, Fareed J, Antic D (2022) Immune activation and inflammatory biomarkers as predictors of venous thromboembolism in lymphoma patients. Thrombosis Journal 20(1):20. https://doi.org/10.1186/s12959-022-00381-3
Brown J, Adams V (2016) Incidence and risk factors of thromboembolism with multiple myeloma in the presence of death as a competing risk: An empirical comparison of statistical methodologies. Healthcare 4(1):16
Yokoyama K (2015) Thrombosis in lymphoma patients and in myeloma patients. Keio J Med 64(3):37–43. https://doi.org/10.2302/kjm.2014-0017-re
Rupa-Matysek J, Gil L, Kaźmierczak M, Barańska M, Komarnicki M (2017) Prediction of venous thromboembolism in newly diagnosed patients treated for lymphoid malignancies: validation of the khorana risk score. Med Oncol 35(1):1
Lim SH, Woo S, Kim S, Ko YH, Kim WS, Kim SJ (2016) Cross-sectional study of patients with diffuse large B-cell lymphoma: Assessing the effect of host status, tumor burden, and inflammatory activity on venous thromboembolism. Cancer Res Treat 48(1):312–321. https://doi.org/10.4143/crt.2014.266
Rupa-Matysek J, Brzeźniakiewicz-Janus K, Gil L, Krasiński Z, Komarnicki M (2018) Evaluation of the THROLY score for the prediction of venous thromboembolism in newly diagnosed patients treated for lymphoid malignancies in clinical practice. Cancer Med 7(7):2868–2875
Kapur S, Feehan K, Mosiman S, Frankki S, Rosenstein LJ (2021) Real world validation of VTE risk models in newly diagnosed multiple myeloma in a community setting. Blood 138(Supplement 1):2971–2972
Gran OV, Smith EN, Braekkan SK, Jensvoll H, Solomon T, Hindberg K, Wilsgaard T, Rosendaal FR, Frazer KA, Hansen J (2016) Joint effects of cancer and variants in the factor 5 gene on the risk of venous thromboembolism. Haematologica 101(9):1046–1053
Vos HL (2006) Inherited defects of coagulation factor V: The thrombotic side. J Thromb Haemost 4(1):35–40
Haim N, Lanir N, Hoffman R, Haim A, Tsalik M, Brenner B (2001) Acquired activated protein C resistance is common in cancer patients and is associated with venous thromboembolism. Am J Med 110(2):91–96
Corral J, González-Conejero R, Soria JM, González-Porras JR, Pérez-Ceballos E, Lecumberri R, Roldán V, Souto JC, Miñano A, Hernández-Espinosa D, Alberca I, Fontcuberta J, Vicente V (2006) A nonsense polymorphism in the protein Z-dependent protease inhibitor increases the risk for venous thrombosis. Blood 108(1):177–183
Van de Water N, Tan T, Ashton F, O’Grady A, Day T, Browett P et al (2004) Mutations within the protein Z-dependent protease inhibitor gene are associated with venous thromboembolic disease: A new form of thrombophilia. Br J Haematol 127(2):190–194. https://doi.org/10.1111/j.1365-2141.2004.05189.x
Wells PS, Anderson JL, Scarvelis DK, Doucette SP, Gagnon F (2006) Factor XIII VAL34LEU variant is protective against venous thromboembolism: A huge review and meta-analysis. Am J Epidemiol 164(2):101–109. https://doi.org/10.1093/aje/kwj179
Lim BCB, Ariëns RAS, Carter AM, Weisel JW, Grant PJ (2003) Genetic regulation of fibrin structure and function: Complex gene-environment interactions may modulate vascular risk. The Lancet 361(9367):1424–1431
Hisada Y, Mackman N (2017) Cancer-associated pathways and biomarkers of venous thrombosis. Blood 130(13):1499–1506. https://doi.org/10.1182/blood-2017-03-743211
Pabinger I, Thaler J, Ay C (2013) Biomarkers for prediction of venous thromboembolism in cancer. Blood 122(12):2011–2018. https://doi.org/10.1182/blood-2013-04-460147
Alexander M, Burbury K (2016) A systematic review of biomarkers for the prediction of thromboembolism in lung cancer — results, practical issues and proposed strategies for future risk prediction models. Thromb Res 148:63–69. https://doi.org/10.1016/j.thromres.2016.10.020
Comerford C, Glavey S, Quinn J, O’Sullivan JM (2022) The role of VWF/FVIII in thrombosis and cancer progression in multiple myeloma and other hematological malignancies. J Thromb Haemost 20(8):1766–1777
Mohren M, Jentsch-Ullrich K, Koenigsmann M, Kropf S, Schalk E, Lutze G (2015) High coagulation factor VIII and von Willebrand factor in patients with lymphoma and leukemia. Int J Hematol 103(2):189–195
Lekovic D, Miljic P, Mihaljevic B (2010) Increased risk of venous thromboembolism in patients with primary mediastinal large B-cell lymphoma. Thromb Res 126(6):477–480
Boersma RS, Hamulyak K, van Oerle R, Tuinenburg A, ten Cate-Hoek AJ, Schouten HC (2016) Biomarkers for prediction of central venous catheter related-thrombosis in patients with hematological malignancies. Clin Appl Thromb Hemost 22(8):779–784
Ay C, Vormittag R, Dunkler D, Simanek R, Chiriac A-L, Drach J, Quehenberger P, Wagner O, Zielinski C, Pabinger I (2009) D-dimer and prothrombin fragment 1 + 2 predict venous thromboembolism in patients with cancer: Results from the Vienna Cancer and thrombosis study. J Clin Oncol 27(25):4124–4129
Hohaus S, Tisi MC, Bartolomei F, Cuccaro A, Maiolo E, Alma E, D’Alò F, Bellesi S, Rossi E, De Stefano V (2018) Risk factors for venous thromboembolism in patients with lymphoma requiring hospitalization. Blood Cancer J 8(6):54
Martínez-Alfonzo I, Velasco D, Mínguez Paniagua P, Mahillo-Fernández I, Askari E, Vidal Laso R, Fernández Maqueda C, Velasco A, González-Teomiro A, Civeira-Marín M, Prieto-Pareja E, Martín-Herrero S, Calvo Villas JM, Krsnik I, Sánchez-Garcia J, Alvarez MA, Llamas Sillero MP, Serrano-López J (2022) Machine learning model defines higher risk of venous thromboembolism in young adults with multiple myeloma. Blood 140(Supplement 1):2811–2812
Dharmavaram G, Cao S, Sundaram S, Ayyappan S, Boughan K, Gallogly M et al (2020) Aggressive lymphoma subtype is a risk factor for venous thrombosis. development of lymphoma - specific venous thrombosis prediction models. Am J Hematol 95(8):918–26. https://doi.org/10.1002/ajh.25837
Sanfilippo KM (2022) Venous thromboembolism and risk stratification in hematological malignancies. Thrombosis Res 213:16. https://doi.org/10.1016/j.thromres.2022.01.008
Acknowledgements
The authors acknowledge the institutional support from GEN inCode and the financial support provided by the Fundación para la Investigación Biomédica del Hospital Universitario Príncipe de Asturias. The authors thank M.L.G. for editorial assistance.
Funding
This work was supported by the Fundación para la Investigación Biomédica del Hospital Universitario Príncipe de Asturias.
Author information
Authors and Affiliations
Contributions
Irene Sánchez, Isabel Gutiérrez and Julio García designed research and analyzed data. Irene Sánchez and Julio García wrote the initial draft of the paper. All authors participated in provision of study materials and patients, collection of data and writing/ reviewing the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors confirm that there are no relevant financial or non-financial competing interests to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Patients with lymphoma and multiple myeloma are at elevated risk of venous thromboembolic disease.
• An accurate risk stratification that captures the heterogeneous hypercoagulable state present in these patients is needed to guide individualized primary thromboprophylaxis.
• Performance status, immobilization and factor VIII levels are significantly associated to venous thrombosis in patients with lymphoma and multiple myeloma, and genome-wide genetic analysis warrants further investigation in this setting.
• A novel multivariable clinical-genetic model that includes a limited set of genetic variants, prothrombotic biomarkers and clinical variables could improve prediction of thrombotic risk in these patients.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sánchez Prieto, I., Gutiérrez Jomarrón, I., Martínez Vázquez, C. et al. Comprehensive evaluation of genetic and acquired thrombophilia markers for an individualized prediction of clinical thrombosis in patients with lymphoma and multiple myeloma. J Thromb Thrombolysis (2024). https://doi.org/10.1007/s11239-024-02977-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s11239-024-02977-0