Abstract
Background
Thromboembolism (TE) after lung transplantation (LTX) is associated with increased morbidity and mortality. The aim of this study is to analyze the incidence and outcome of venous and arterial thromboembolic complications and to identify independent risk factors.
Patients and methods
We retrospectively analyzed the medical records of 221 patients who underwent LTX at our institution between 2002 and 2021. Statistical analysis was performed using SPSS and GraphPad software.
Results
74 LTX recipients (33%) developed TE. The 30-days incidence and 12-months incidence were 12% and 23%, respectively. Nearly half of the patients (48%) developed pulmonary embolism, 10% ischemic stroke. Arterial hypertension (p = 0.006), a body mass index (BMI) > 30 (p = 0.006) and diabetes mellitus (p = 0.041) were independent predictors for TE. Moreover, a BMI of > 25 at the time of transplantation was associated with an increased risk for TE (43% vs. 32%, p = 0.035). At the time of LTX, 65% of the patients were older than 55 years. An age > 55 years also correlated with the incidence of TE (p = 0.037) and these patients had reduced overall post-transplant survival when the event occurred within the first postoperative year (59% vs. 72%, p = 0.028).
Conclusions
The incidence of TE after LTX is high, especially in lung transplant recipients with a BMI > 25 and an age > 55 years as well as cardiovascular risk factors closely associated with the metabolic syndrome. As these patients comprise a growing recipient fraction, intensified research should focus on the risks and benefits of regular screening or a prolonged TE prophylaxis in these patients.
Trial registration number DKRS: 00021501.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Highlights
-
The incidence of arterial and venous thromboembolism after lung transplantation is high, notably in recipients with a BMI > 25 and an age > 55 years.
-
Moreover, cardiovascular risk factors closely associated with the metabolic syndrome are independent risk factors for venous thromboembolism.
-
Intensified research should focus on the risks and benefits of regular screening or a prolonged thromboembolism prophylaxis in patients at risk, especially in the first postoperative year.
Introduction
Lung transplantation is the most efficient treatment option for selected patients with end stage chronic lung disease [1], such as idiopathic pulmonary fibrosis or chronic obstructive pulmonary disease (COPD) [1]. Although the median survival rates have improved over the last decade, chronic lung allograft dysfunction (CLAD)—the hallmark of chronic lung allograft rejection—is responsible for a 5-years survival of only 55% [2]. It occurs in about half of the patients within 5 years after transplantation and up to now, there is no effective treatment available.
Since the introduction of the Lung Allocation Score (LAS) in 2005, the recipient population has changed, and older patients with age-related comorbidities are now more likely to receive an organ [3]. According to the 2013 report of the Registry of the International Society for Heart and Lung Transplantation, the median age at the time of LTX has gradually increased from 45 to 55 years over the preceding decade [4]. This implies the need to adjust to a growing fraction of patients of more than 60 or even 65 years of age with a higher risk of morbidity and mortality after lung transplantation [5].
Aside from postoperative infections, lung transplant recipients may experience cardiovascular complications, such as thromboembolism [6,7,8]. Thromboembolism (TE) is a well-known complication after surgery and the level of risk mainly depends on the surgery performed [9]. Acute pulmonary embolism is the most dangerous form of venous TE and can be fatal if left untreated [10]. It is associated with cardiac arrhythmia and right ventricular dysfunction and has an overall mortality rate of up to 10% [10, 11]. The reported incidence of thromboembolic complications after LTX is considered higher compared to other cardiothoracic surgeries [12] but varies widely between studies (6–44%) [6, 8, 13,14,15]. In our study, as in most of the others, only clinical symptoms prompted further investigation, so thromboembolic events might have been missed. This is supported by studies that implemented a regular screening protocol, where a higher incidence of TE was reported compared to studies without such a protocol [12]. Solid organ transplantation itself is recognized as an independent risk factor for thromboembolic events [16]. There are several underlying factors promoting TE: the surgical trauma itself induces inflammation leading to a prothrombotic state, immobilisation und fluid imbalance results in decreased venous flow. Side effects from immunosuppressive medication such as calcineurin inhibitors or corticosteroids, which impair glucose tolerance and induce post-transplant diabetes [17] further enhance the risk to develop thrombosis. Moreover, bacterial and viral infections have been shown to increase the risk for thrombotic events [9, 12, 18]. With increasing age, a growing number of patients develop traits of the metabolic syndrome, a heterogeneous clinical entity which includes the co-occurrence of overweight, impaired glucose tolerance, dyslipidaemia and hypertension leading to cardiovascular disease and diabetes mellitus [19, 20]. Two additional components underlined by the conference paper on the definition of the metabolic syndrome of the American Heart Association are a proinflammatory and a prothrombotic state [21]. A growing understanding is that venous TE is a chronic process which shares similar risk factors and pathophysiology, e.g., endothelial dysfunction, with atherothrombosis and coronary artery disease [9, 22]. Thus, a higher age at the time of transplantation, often accompanied by metabolic and cardiovascular comorbidity, makes a growing fraction of the lung transplant recipients particularly vulnerable to thromboembolic complications.
Clinical trials in general -, urologic -, and orthopaedic surgery have shown that the incidence of venous postoperative TE can be significantly reduced by interventions like early mobilization and adequate pharmacologic thrombosis prophylaxis to a range of 1.1–10.6% [9, 23]. While TE in general is associated with increased morbidity and hospital length of stay as well as reduced overall survival [24], there is limited data regarding the optimal management of these patients.
The aim of this study is to analyse the incidence of arterial and venous thromboembolic events in our lung transplanted patient cohort and identify independent risk factors. Furthermore, we make an attempt to discuss a regular screening during follow-up for patients at risk and the potential need for a personalised prophylaxis regime after surgery for a growing number of our patients.
Methods
Design and study population
We performed a retrospective single centre analysis of patients who underwent LTX at the Department of Thoracic Surgery, Medical Centre—University of Freiburg between March 2003 and June 2021. A total of 221 patients were identified (115 males and 106 females). Patients with combined transplantations, such as heart–lung transplantations, were excluded.
All patients underwent regular clinical follow-ups, including bronchoscopy, blood values, and lung function analysis. Data were collected by checking electronic medical records, discharge reports and autopsy reports.
The study was approved by the Medical Centre—University of Freiburg’s local ethics committee and conducted in accordance with the guideline proposed in the Declaration of Helsinki. A waiver of consent was granted due to the retrospective nature of the study and the associated minimal risk. It is registered at the German Registry for Clinical Trials (DRKS) under the trial registration number 00021501.
Follow-up schedule after lung transplantation
In the first year after the lung transplantation, clinical examination, lung function test and surveillance bronchoscopies with bronchoalveolar lavage and lung biopsies are scheduled for 1, 2, 3, 4, 6, and 12 months. From the second postoperative year on, patients are seen every 3 months for clinical examination, lab and lung function testing (Supplemental Fig. 2). In case of conspicuous results, such as infection or an otherwise not explainable decline in lung function, further testing/imaging/bronchoscopy to rule out/confirm CLAD is performed. If clinical symptoms for TE are present, further testing as described under the “definitions” section is initiated.
Immunosuppression medication levels as well as blood and kidney parameters were initially checked weekly after discharge and once stable, the interval was extended to every 4 weeks (Table 1).
Definitions
We defined TE as the main event. TE includes every event attributed to either thrombotic arterial occlusion (e.g., myocardial infarction, stroke) and venous thrombosis or embolism as listed in Table 2. Thromboembolism was detected mostly by clinical symptoms during regular follow-ups in the transplant outpatient centre. Since asymptomatic patients were not routinely screened, some events might have been missed, especially after the first postoperative year. The diagnosis was established by ultrasound. In case of suspected pulmonary embolism ventilation/perfusion scintigraphy or CT angiography were performed. Diagnostic measures for other venous and arterial events were initiated as appropriate upon clinical presentation. If a patient suffered from multiple thromboembolic events, they were listed separately, each counting as one event. However, for the calculation of survival and risk factors, patients were divided into 2 groups, one with and the other without thromboembolic events. Thromboembolic events that occurred before transplantation were excluded.
The body mass index (BMI) was used to define if patients are underweight (BMI < 18.5), of normal weight (18.5–24.9), overweight (25.0–29.9) or obese (BMI > 30.0).
Thrombosis prophylaxis and ICU management
The standard pharmacological thrombosis prophylaxis consisted of 40 mg enoxaparin or 5000 IE unfractionated heparin every 12 h in intensive care unit (ICU) and 4500 IE tinzaparin in intermediate care unit (IMC) every 24 h. This regimen was initiated in ICU as soon as possible after ruling out postoperative active bleeding. Additionally, medical compression bandages were used in ICU and medical compression stockings in IMC and regular wards until discharge. Generally, patients discharged from the hospital did not receive further thrombosis prophylaxis in accordance with the current guidelines. Patients with the indication for therapeutic anticoagulation, e.g., atrial fibrillation or pulmonary embolism, received unfractionated heparin or enoxaparin in therapeutic doses while being at the hospital. Therapeutic anticoagulation therapy was continued after the patients were discharged. After an arterial thromboembolic event patients were placed on aspirin therapy in accordance with current guidelines. Physical therapy was available to all patients starting from the first postoperative day in ICU.
Intravenous as well as intraarterial catheters were removed as soon as possible at the discretion of the treating physician in ICU or IMC.
Statistical analysis
The Kaplan–Meier-Method was used to estimate overall survival and the log rank test was used for comparison of survival curves of patients with and without TE. To evaluate connections between different parameters the Fischer’s exact test, the Chi-squared test and the Mann–Whitney U test were used when appropriate. Univariate and multivariate logistic regression models were used to select independent predictors of TE and survival in our cohort. All tests were two-tailed. A p-value < 0.05 was considered statistically significant. All statistical analyses were conducted using SPSS software (Version 27, IBM Corporation, New York, NY, USA) and GraphPad Prism (Version 9, GraphPad Software, San Diego, CA 92108, USA).
Results
Overall, 221 patients (115 male, 106 female) underwent LTX at our institution between March 2002 and June 2021. 196 (89%) patients underwent a double lung transplantation, 25 (11%) patients a single lung transplantation. 68 (31%) patients underwent LTX before implementation of the lung allocation score (LAS)—based distribution system at the end of 2011. From 2012 until 2021, another 153 transplantations (69%) were performed. At the time of data analysis, 146 patients (66) were still alive. The 1-year-, 5-years- and 10-years-survival-rate in our patient collective is 80%, 66% and 59% respectively (Fig. 1a).
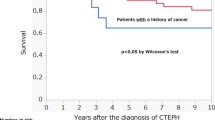
a Overall post-transplant survival. Kaplan–Meier Analysis of survival after lung tranplantation. 1 month: 89%, 6 months: 82%, 1 year: 80%, 5 years: 66% and10 years 59%. b overall survival and survival after thromboembolic events within the first month after LTX. Log rank t test p = 0.027. Survival after lung tranplantation. Thromboembolic event in the first month (1 year: 74%, 3 years: 60%, 5 years: 30% and 10 years: 30%) vs. no thromboembolic event in the first month (1 year: 81%, 3 years: 75%, 5 years: 70% and 10 years: 61%). c overall survival and survival after thromboembolic events within the first year after LTX of patients ≥ 55 years. Long rank t test p = 0.028. Survival after lung tranplantation. Thromboembolic event in the first year (1 year: 82%, 3 years: 67%, 5 years: 45% and 10 years: 37%) vs. no thromboembolic event in the first year (1 year: 85%, 3 years: 78%, 5 years: 72% and 10 years: 66%) in patients ≥ 55 years of age
The average waiting time for a transplantation was 14 months (range 2 days to 11 years). The main underlying pulmonary diseases leading to LTX were idiopathic fibrosis (38%), or chronic obstructive pulmonary disease (COPD) (35%). Concomitant cardiovascular diseases, e.g., arterial hypertension (29%) or one-vessel coronary artery disease (17%), as well as diabetes mellitus (18%), were present in a substantial fraction of the patients (Table 3). Patients transplanted after 2011 were more often aged > 55 years compared to patients that underwent surgery before the implementation of the LAS score (72% vs. 49%, p < 0.001). Overall, 143 patients (65%) were over 55 years old, and 96 patients (43%) were aged 60 years or older at the time of transplantation (Table 1).
We identified 74 patients (33%) who experienced at least one thromboembolic event after lung transplantation. Most of the events (68%) took place within the first postoperative year, whereas 35% already occurred within the first postoperative month (Table 1). 34 patients (15%) developed pulmonary embolism and 23 patients (10%) were diagnosed with ischemic stroke. Hemiparesis or hypaesthesia persisted in 11 patients (4.8%) of the latter group. Most pulmonary embolisms occurred during the first year (53%) while the majority of strokes took place in the first month (57%). However, approximately 1/3 of all thromboembolic events were diagnosed after the first postoperative year (Table 1).
Thromboembolic events within the first postoperative month were associated with reduced survival after transplantation (56% vs. 68%, p = 0.027) (Fig. 1b). Notably, patients over 55 years of age at the time of transplantation, which comprise 65% of our cohort, had not only an increased incidence of thromboembolic events in the first postoperative month (p = 0,025), but also a reduced survival rate when they experienced at least one event within the first year (59% vs. 72%, p = 0,028) (Fig. 1c). In accordance with that, a recipient age of > 55 years correlated with the incidence of TE (p = 0.037) (Table 3). Moreover, arterial hypertension (p = 0.004), peripheral artery disease (p = 0.019) and diabetes mellitus (p = 0.017) were independent predictors for TE (Table 4). These factors are closely related to the metabolic syndrome, and fittingly, a body mass index (BMI) of > 25 at the time of transplantation also contributed significantly to the risk for TE (p = 0.035) (Tables 3 and 4). Particularly venous TE correlated with the above-mentioned factors with few exceptions when arterial TE was more predominant (Tables 3 and 4). While several independent risk factors for TE could be identified, they had no effect on long-term survival (Table 5).
At the time of transplantation, about half of patients (51%) had a normal weight with a BMI between 18.5 and 24.9 kg/m2 (Supplementary Fig. 1). In our cohort, 36 (32%) patients of normal weight had a thromboembolic event and 42% of them were diagnosed with pulmonary embolism. The incidence of pulmonary embolism further increased to 61% in patients with a BMI of > 25. In contrast, only 5 (15%) underweight patients were diagnosed with TE and none of them had pulmonary embolism. This indicates that specifically the occurrence of pulmonary embolism was closely related to the patients’ weight (p < 0.001).
Discussion
Incidence and timing of TE
We found a 30-day and 12-month incidence of TE of 12% and 23% respectively in our lung transplant recipients. Overall, about one third of them had at least one thromboembolic event during the postoperative course. Current evidence indicates that the incidence of venous TE after LTX is higher [6] compared to other cardiothoracic surgeries, but varies between studies (8%–43%) [6, 12, 13, 24, 25]. A possible explanation is that the lung transplant cohorts are heterogeneous due to different underlying diseases and preexisting conditions. Moreover, there are also differences in screening protocols and thrombosis prophylaxis regimes as well as in time schedules of follow-up appointments between institutions. Notably, many cases of TE occur during hospital stay despite the use of thrombosis prophylaxis. It is widely accepted that pharmacologic prophylaxis with unfractionated heparin and low molecular weight heparin should be monitored with appropriate tests such as anti-factor-Xa-activity, for example. This may help to tailor individual doses for every patient. Although most thromboembolic events in our cohort took place in the first postoperative year, about one third was detected later than that. It can only be assumed that with a structured screening in place, the incidence would be even higher. In accordance with this, a high risk for recurrence was shown in a study by Prandoni et al., who followed a cohort of 1626 consecutive patients with venous TE in Padua, Italy for up to 10 years and found a high rate of recurrent events: 11% after 1 year, 20% after 3 years, 29% after 5 years, and 40% after 10 years [26].
Risk factors and distribution of TE
We identified both, arterial and venous thromboembolic events. Both share common risk factors [27], which can be found in an increasing fraction for TE in our cohort. Although they share similar risk factors, they are different diseases and, in our cohort, venous events are more common than the arterial ones. Interestingly, most of the risk factors seem to be statistically relevant for venous TE which makes a prolonged thrombosis prophylaxis even more relevant.
We had a surprisingly high number of patients suffering from stroke, not only in the first month after surgery but also after the first postoperative year. Transplantation surgery itself along with the above-mentioned risk factors have been described to play a role in the early cases of those occurring within 30 days [28]. The later ones, however, may be a combined result of preexisting condition and e.g. the immunosuppression or other factors in the aftermath of the transplantation. Patients with newly diagnosed atrial fibrillation after surgery were placed on anticoagulation therapy according to current guidelines, and there is no statistically significant increase in the incidence of stroke in these patients (Table 3). We may, however, have missed some cases of atrial fibrillation if it occurred later or only paroxysmal and without symptoms.
Perioperative ECMO support itself did not increase the risk for TE in our cohort, however, this may be due to the large time span of observation and the fact that 30-days-mortality in patients on ECMO support as ‘bridge to transplant’ was much higher in the earlier years compared to the last decade.
There are some reports describing thrombi arising from the surgical suture lines, which is a possible, although rare source for TE [29, 30]. The venous and pulmonary arterial anastomoses are checked for patency and flow pattern intra- and, if needed, also postoperatively by transesophageal echography. Moreover, a precise suture technique with an endothelium-to-endothelium junction to occlude the muscle from the blood-contacting surfaces is employed for the venous cuff anastomoses [29]. All patients are checked for an atrial septum defect before transplantation and occlusion therapy is initiated for patients at need.
As described in previous studies, weight plays an important role in the incidence of thromboembolic events [31,32,33]. In our cohort, almost half of the patients with a BMI > 25 had a thromboembolic event during the postoperative course, most of them within the first year after transplantation. In recent years, our patients who initially presented with a BMI > 30 had to reduce weight before transplantation as this reduces not only the risk for TE and other cardiovascular complications but also for the development of primary graft dysfunction [32].
Prophylaxis and treatment of venous and arterial TE
All patients at our center received thrombosis prophylaxis and regular physiotherapy with the goal of ambulation starting from ICU until the day of discharge. Furthermore, all patients with TE were prescribed anticoagulation therapy or antiplatelet drugs according to current guidelines. Pre-existing antiplatelet therapy was not interrupted for transplantation and pre-existing anticoagulation therapy was continued as soon as possible after surgery with low molecular weight heparin in therapeutic doses. Patients with atrial fibrillation known prior to LTX were on anticoagulation therapy and none of them suffered postoperative stroke.
Gastrointestinal bleeding occurred in 6 (3%) patients on anticoagulation after transplantation, while no other major bleeding events were recorded. However, individual risks for bleeding complications need to be taken into consideration when thinking about a prolonged thrombosis prophylaxis for a certain amount of time to reduce the incidence of TE for patients at risk.
Limitations of the study
A limiting factor of this retrospective single-centre study is that it covers a period of nearly 20 years and thus our findings may not apply to all lung transplant recipients. Moreover, due to the absence of clinical signs, we might have missed some cases of TE or complications thereof in our patient cohort. This is especially true for events that occurred after the first postoperative year. That said, a strength of the study is that one single protocol regarding postoperative management and TE prophylaxis applied to all patients at the respective time of transplantation, despite the arguably long follow-up time. The latter, however, allowed us to detect the events that occurred years after transplantation.
Conclusions
About 2/3 of all TE events occur in the first postoperative year, therefore an extended thrombosis prophylaxis for lung transplant patients with risk factors for TE such as age of more than 55 years, cardiovascular risk factors or diabetes mellitus, seems beneficial, particularly within the first year after surgery. However, whether this reduces the incidence of TE, or whether therapeutic anticoagulation is beneficial for selected patients for a certain amount of time after LTX needs to be analysed in randomised controlled studies. Considering the individual risk of the patient, also with regards to potential bleeding complications, is essential when making a decision.
In any case, it is very important to be aware of the increased risk of TE and to improve early detection, particularly in patients with pre-existing or new-onset cardiovascular comorbidity. The implementation of a regular screening, possibly integrated in the follow-up schedule at the outpatient transplant centre, as described for example by Zheng et al. [12] or Jorge et al [34], seems to be of great value and should be subject to further investigation.
Data availability
The dataset generated during and/or analysed during the current study is available from the corresponding author on reasonable request.
References
Bos S, Vos R, Van Raemdonck DE, Verleden GM (2020) Survival in adult lung transplantation: where are we in 2020? Curr Opin Organ Transplant 25(3):268–273. https://doi.org/10.1097/MOT.0000000000000753
Young KA, Dilling DF (2019) The future of lung transplantation. Chest 155(3):465–473. https://doi.org/10.1016/j.chest.2018.08.1036
Kanade R, Mohanka M, Bollineni S et al (2021) Characteristics and outcomes among patients with early venous thromboembolic events after lung transplant. Transpl Proc 53(1):303–310. https://doi.org/10.1016/j.transproceed.2020.08.013
Yusen RD, Christie JD, Edwards LB et al (2013) The registry of the international society for heart and lung transplantation: thirtieth adult lung and heart-lung transplant report–2013; focus theme: age. J Heart Lung Transplant 32(10):965–978. https://doi.org/10.1016/j.healun.2013.08.007
Mosher CL, Weber JM, Frankel CW, Neely ML, Palmer SM (2021) Risk factors for mortality in lung transplant recipients aged >/=65 years: a retrospective cohort study of 5815 patients in the scientific registry of transplant recipients. J Heart Lung Transplant 40(1):42–55. https://doi.org/10.1016/j.healun.2020.10.009
Kahan ES, Petersen G, Gaughan JP, Criner GJ (2007) High incidence of venous thromboembolic events in lung transplant recipients. J Heart Lung Transplant 26(4):339–344. https://doi.org/10.1016/j.healun.2007.01.009
Parsa SA, Khaheshi I, Dousti A, Naghashzadeh F, Ataeinia B (2016) ST-elevation myocardial infarction 33 days after lung transplant in a patient with non-significant CAD before transplantation: a case report. J Clin Diagn Res 10(5):OD23–OD24. https://doi.org/10.7860/JCDR/2016/18830.7800
Ribeiro Neto ML, Budev M, Culver DA et al (2018) Venous thromboembolism after adult lung transplantation: a frequent event associated with lower survival. Transplantation 102(4):681–687. https://doi.org/10.1097/TP.0000000000001977
Stavrou EX, Schmaier AH (2014) Chapter 15—Venous and arterial thrombosis. In: Willis MS, Homeister JW, Stone JR (eds) Cellular and molecular pathobiology of cardiovascular disease. Academic Press, Cambridge, pp 277–296
Huisman MV, Barco S, Cannegieter SC et al (2018) Pulmonary embolism. Nat Rev Dis Primers 4:18028. https://doi.org/10.1038/nrdp.2018.28
Essien EO, Rali P, Mathai SC (2019) Pulmonary Embolism. Med Clin North Am 103(3):549–564. https://doi.org/10.1016/j.mcna.2018.12.013
Zheng M, Yousef I, Mamary AJ et al (2021) Venous thromboembolism in lung transplant recipients real world experience from a high volume center. J Heart Lung Transplant 40(10):1145–1152. https://doi.org/10.1016/j.healun.2021.07.010
Izbicki G, Bairey O, Shitrit D, Lahav J, Kramer MR (2006) Increased thromboembolic events after lung transplantation. Chest 129(2):412–416. https://doi.org/10.1378/chest.129.2.412
Kristensen AW, Mortensen J (2017) Berg RM pulmonary thromboembolism as a complication of lung transplantation. Clin Transplant. https://doi.org/10.1111/ctr.12922
Smith PJ, Stonerock GL, Ingle KK et al (2018) Neurological sequelae and clinical outcomes after lung transplantation. Transplant Direct 4(4):e353. https://doi.org/10.1097/TXD.0000000000000766
Garcia-Ortega A, Lopez-Reyes R, Anguera G et al (2021) Venous thromboembolism in solid-organ transplant recipients: findings from the RIETE registry. Thromb Res 201:131–138. https://doi.org/10.1016/j.thromres.2021.02.022
Jindal RM, Sidner RA, Milgrom ML (1997) Post-transplant diabetes mellitus the role of immunosuppression. Drug Saf 16(4):242–257. https://doi.org/10.2165/00002018-199716040-00002
Biyik I, Akturk IF, Yalcin AA, Celik O, Oner E (2015) Immunosuppressive therapy induced coronary vasospasm and acute myocardial infarction in a patient undergoing new renal transplantation. Postepy Kardiol Interwencyjnej 11(2):141–145. https://doi.org/10.5114/pwki.2015.52288
Alessi MC, Juhan-Vague I (2008) Metabolic syndrome, haemostasis and thrombosis. Thromb Haemost 99(6):995–1000. https://doi.org/10.1160/TH07-11-0682
Wenger U, Cottini SR, Noll G et al (2013) Pretransplant dyslipidaemia determines outcome in lung transplant recipients. Lipids Health Dis 12(1):53. https://doi.org/10.1186/1476-511x-12-53
Grundy SM, Brewer HB Jr, Cleeman JI et al (2004) Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation 109(3):433–438. https://doi.org/10.1161/01.CIR.0000111245.75752.C6
Goldhaber SZ (2012) Venous thromboembolism: epidemiology and magnitude of the problem. Best Pract Res Clin Haematol 25(3):235–242. https://doi.org/10.1016/j.beha.2012.06.007
Collins R, Scrimgeour A, Yusuf S (1988) Peto R reduction in fatal pulmonary embolism and venous thrombosis by perioperative administration of subcutaneous heparin. Overview of results of randomized trials in general, orthopedic, and urologic surgery. N Engl J Med 318(18):1162–1173. https://doi.org/10.1056/NEJM198805053181805
Aboagye JK, Hayanga JWA, Lau BD et al (2018) Venous thromboembolism in patients hospitalized for lung transplantation. Ann Thorac Surg 105(4):1071–1076. https://doi.org/10.1016/j.athoracsur.2017.10.041
Saez-Gimenez B, Berastegui C, Loor K et al (2015) Deep vein thrombosis and pulmonary embolism after solid organ transplantation: an unresolved problem. Transplant Rev (Orlando) 29(2):85–92. https://doi.org/10.1016/j.trre.2014.12.005
Prandoni P, Noventa F, Ghirarduzzi A et al (2007) The risk of recurrent venous thromboembolism after discontinuing anticoagulation in patients with acute proximal deep vein thrombosis or pulmonary embolism. A prospective cohort study in 1626 patients. Haematologica 92(2):199–205. https://doi.org/10.3324/haematol.10516
Prandoni P (2007) Links between arterial and venous disease. J Intern Med 262(3):341–350. https://doi.org/10.1111/j.1365-2796.2007.01815.x
Shigemura N, Sclabassi RJ, Bhama JK et al (2013) Early major neurologic complications after lung transplantation: incidence, risk factors, and outcome. Transplantation 95(6):866–871. https://doi.org/10.1097/TP.0b013e318280b359
Griffith BP, Magee MJ, Gonzalez IF et al (1994) Anastomotic pitfalls in lung transplantation. J Thorac Cardiovasc Surg 107(3):743–754. https://doi.org/10.1016/s0022-5223(94)70330-2
Soetanto V, Grewal US, Mehta AC et al (2022) Early postoperative complications in lung transplant recipients. Indian J Thorac Cardiovasc Surg 38(Suppl 2):260–270. https://doi.org/10.1007/s12055-021-01178-1
Severinsen MT, Kristensen SR, Johnsen SP, Dethlefsen C, Tjonneland A, Overvad K (2009) Anthropometry, body fat, and venous thromboembolism: a Danish follow-up study. Circulation 120(19):1850–1857. https://doi.org/10.1161/CIRCULATIONAHA.109.863241
Upala S, Panichsillapakit T, Wijarnpreecha K, Jaruvongvanich V, Sanguankeo A (2016) Underweight and obesity increase the risk of mortality after lung transplantation: a systematic review and meta-analysis. Transpl Int 29(3):285–296. https://doi.org/10.1111/tri.12721
Schwann TA, Kistler L, Engoren MC, Habib RH (2010) Incidence and predictors of postoperative deep vein thrombosis in cardiac surgery in the era of aggressive thromboprophylaxis. Ann Thorac Surg 90(3):760–766. https://doi.org/10.1016/j.athoracsur.2010.03.117. ((discussion 766-8))
Jorge A, Sanchez PG, Hayanga JWA et al (2020) Routine deep vein thrombosis screening after lung transplantation: incidence and risk factors. J Thorac Cardiovasc Surg 159(3):1142–1150. https://doi.org/10.1016/j.jtcvs.2019.08.030
Acknowledgements
Supplemental Fig. 2 contains an image created with the help of BioRender.com. Open Access funding is enabled and organized by Projekt DEAL.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
IM and OS concepted the study. EDO, IH and IM collected the data. EDO and IM performed the statistical analysis and wrote the manuscript. WJ, JK, OS and BP reviewed and revised the manuscript. Part of this work was used for EDO’s M.D. thesis (Dr. med.).
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial conflict of interest or relevant disclosures related to this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
11239_2022_2748_MOESM1_ESM.svg
Supplementary file1 (SVG 71 KB)—Supplementary Fig. 1 Distribution of patients’ weight at the time of lung transplantation
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moneke, I., Ogutur, E.D., Kalbhenn, J. et al. Independent risk factors for an increased incidence of thromboembolism after lung transplantation. J Thromb Thrombolysis 55, 252–262 (2023). https://doi.org/10.1007/s11239-022-02748-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-022-02748-9