Abstract
Previous observational and randomized studies suggested potential benefit of therapeutic anticoagulation during hospitalization, but this treatment remains controversial. As of June 30th 2021, steroids is the standard treatment of COVID patients. We aimed to investigate the association of prophylactic and therapeutic anticoagulation with mortality for patients with COVID-19 who were treated with steroids. We retrospectively reviewed the medical records of 2533 patients discharged between March 1st, 2020 and March 30th, 2021, with laboratory-confirmed COVID-19 in the Mount Sinai Health System and treated with steroids. We evaluated the effect of therapeutic versus prophylactic anticoagulation on the outcomes using propensity score analyses. Subgroup analyses were conducted by stratification of patients by endotracheal intubation. Among the 2533 eligible patients, 465 (18.4%) received therapeutic anticoagulation. After 1:1 propensity score matching (N = 383 pairs), in-hospital mortality was similar between those with therapeutic versus prophylactic anticoagulation (36.0% versus 30.0%, P = 0.091). In-hospital mortality regardless of endotracheal intubation were not significantly different between the two groups. Therapeutic anticoagulation was not associated with reduced or increased risk of in-hospital mortality in patients with COVID-19 treated with steroids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
We investigated 2533 COVID-19 patients treated with steroids.
-
We evaluated the effect of therapeutic versus prophylactic anticoagulation.
-
After adjustments, in-hospital mortality was similar (36.0% versus 30.0%, P = 0.091).
-
Therapeutic anticoagulation was not associated with better or worse mortality.
Introduction
Previous observational and randomized studies suggested potential benefit of therapeutic anticoagulation during hospitalization, but this treatment remains controversial [1, 2]. As of June 30th 2021, steroids are the standard treatment of COVID-19 patients to reduce inflammation and cytokine storm associated with COVID-19 [3,4,5]. Initially, therapeutic anticoagulation seems to be preferred because COVID-19 causes inflammation and thrombosis, however, steroids were not frequently used in the initial phase of pandemic [6]. Therefore, we hypothesized that the results might be different if we selected patients who have been treated with steroid for COVID-19 and patients who needs steroids for other underlying diseases. Herein, we aimed to investigate the association of prophylactic and therapeutic anticoagulation with mortality for patients with COVID-19 who were treated with steroids.
Methods
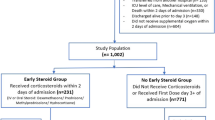
This retrospective study was conducted by review of the electronic medical records for 9965 patients with laboratory confirmed COVID-19 hospitalized in the Mount Sinai Health system between March 1st 2020 and March 30th 2021 [7,8,9,10]. Identification of COVID-19 was based on a nasopharyngeal swab, which was tested using a polymerase chain reaction. For the purpose of this study (examine the effectiveness of therapeutic versus prophylactic anticoagulation among patients on steroids), we limited our cohort to patients who were treated with steroids within 2 days of admission (n = 3984). We showed patients’ baseline characteristics and in-hospital outcomes who were not treated with steroids in supplemental Table 1. Steroids were defined as treatment with systemic betamethasone, dexamethasone, hydrocortisone, prednisone, prednisolone, and methylprednisolone. We excluded patients age < 18 years old (n = 9) and those who were transferred to other facilities (n = 86). Then, we excluded 517 patients who were discharged within two days of admission (dead or alive) to mitigate the selection bias. We also limited the analysis to patients who received therapeutic or prophylactic anticoagulation within 2 days of admission to investigate the initial treatment choice for COVID-19 patients (n = 3110). Moreover we excluded patients with both prophylactic and therapeutic anticoagulation within 2 days of admission (n = 343). Finally, we excluded patients with atrial fibrillation (n = 207) and acute venous thromboembolism during hospitalization (n = 27) since these patients needed therapeutic anticoagulation unrelated to COVID treatment, resulting in the final cohort of 2533 patients. Therapeutic anticoagulation was defined as apixaban, dabigatran, rivaroxaban (excluding 2.5 mg as prevention of atherosclerotic cardiovascular events) [11], edoxaban, warfarin, and enoxaparin (as therapeutic dose), intravenous continuous unfractionated heparin, and argatroban. Prophylactic anticoagulation was defined as subcutaneous heparin or enoxaparin in prophylactic dose.
We reviewed patients’ electronic medical records and extracted demographics, comorbidities, vital signs, laboratory data, and clinical outcomes. Patients were stratified into two groups, those with therapeutic or prophylactic anticoagulation. Comorbidities were characterized based on the ICD 10 codes. All vital signs and blood tests were recorded at the time of admission. The primary outcome of interest was the in-hospital mortality. Secondary outcomes are acute kidney injury, liver injury, hemoglobin drop, transfusion of red blood cell. Hemoglobin drop was defined as hemoglobin decline by more than 3 g/dL and acute kidney injury was defined as any increase of creatinine by more than 0.3 mg/dL or to more than 1.5 times baseline [12]. Liver injury was defined as ALT more than 5 × upper normal limit (46 U/L).
Continuous variables are presented as mean ± standard deviation or median [interquartile range] depending on the data distribution, and categorical variables were expressed as percentages. Differences in baseline characteristics between groups were evaluated, using the χ2 test for categorical variables, and t-test or Wilcoxon test for continuous variables. We performed 1:1 match using the nearest neighbor with a caliper equal to 0.2 of the standard deviation of the logit of the propensity score [13]. The following variables were used to estimate propensity score: age, sex, asthma, chronic obstructive pulmonary disease, obstructive sleep apnea, obesity, hypertension, diabetes mellitus, cancer, atrial fibrillation, coronary artery disease, heart failure, estimated glomerular filtration rate (eGFR), blood urea nitrogen, white blood cell count, and hemoglobin, vital signs, tocilizumab, remdesivir, and treatment with convalescent plasma [5, 9, 14, 15]. The Modification of Diet in Renal Disease equation was used to estimate eGFR [12, 16].
In addition, as a sensitivity analysis, we performed inverse probability treatment weighted (IPTW) analysis to estimate the association of anticoagulation with in-hospital mortality. We imputed missing data using mice package (R software) and repeated propensity score matched and IPTW analysis.
We compared the in-hospital mortality between the propensity-score-matched patients with therapeutic versus prophylactic anticoagulation in the following subgroups: patients on endotracheal intubation, patients who did not have endotracheal intubation; patients were matched by re-estimated propensity score in each subgroup.
All statistical analyses were performed using R (version 3.6.2, R Foundation for Statistical Computing, Vienna, Austria). P-values < 0.05 considered statistically significant.
Results
Among the 2533 eligible patients, 465 (18.4%) received therapeutic anticoagulation. The patients with therapeutic anticoagulation were older and had more comorbidities (Table 1) as compared to patients with prophylactic anticoagulation. Notably, patients with therapeutic anticoagulation strategies had higher d-dimer at admission than those with prophylactic anticoagulation. Table 2 showed crude in-hospital outcomes. Patients on therapeutic anticoagulation had lower in-hospital mortality compared to those who were not treated with prophylactic anticoagulation. They also experienced higher AKI and liver injury, hemoglobin drop > 3 g/dL, and transfusion (Table 2).
After matching by propensity score (N = 383 in each group), baseline characteristics and in-hospital treatments were well balanced, with standardized differences of < 0.10 (Table 1). In-hospital mortality was not significantly different between patients with therapeutic anticoagulation and those with prophylactic anticoagulation (Table 2). In addition, ICU admission, endotracheal intubation, acute kidney injury, liver injury, hemoglobin drop > 3 g/dL, and transfusion were not significantly different. Furthermore, IPTW and multiple imputation for missing data did not change the result (therapeutic versus prophylactic; odds ratio [95% confidential interval] 1.06 [0.81–1.39], P = 0.67]; 1.07 [0.77–1.50], P = 0.68, respectively).
Subgroup analyses are shown in Table 3. Patients with therapeutic anticoagulation did not have significantly different in-hospital mortality compared to those with prophylactic anticoagulation in the subgroup of patients with or without endotracheal intubation (Table 3).
Discussion
In this study, we could not reveal the survival benefit of therapeutic anticoagulation over prophylactic anticoagulation. Previous observational data demonstrated no significant different mortality between these treatments [1] and our data validated the results among patients with the current standard treatment of steroids. Although COVID-19 triggers hypercoagulable state, therapeutic anticoagulation was not proven to reduce in-hospital mortality with the treatment by steroids.
Thromboembolism due to COVID-19 related coagulopathy is the major complication [17,18,19,20,21,22,23,24,25]. Herein, in the early phase of pandemic, therapeutic dose of anticoagulation was associated with a decreased risk of mortality [1, 6]. However, given the data in the early phase of pandemic, the use of steroids were not clear. Steroids were proven to be effective to decrease the risk of death due to COVID-19 since they reduce cytokine storm [3,4,5]. Our study showed that no benefit was observed in therapeutic anticoagulation over prophylactic anticoagulation for COVID-19 patients with steroids, which could be interpreted that steroid and prophylactic anticoagulation is usually enough to treat COVID-19 patients.
There are several ongoing randomized trials of therapeutic anticoagulation targeting hospitalized patients with COVID-19, demonstrating conflicting results [26,27,28,29,30], which will further elucidate which anticoagulation is necessary for COVID-19 patients, especially treated with steroids. Interestingly, the recent report demonstrated no benefit of therapeutic anticoagulation for critically ill patients with COVID-19, which supported our findings [31], however, therapeutic anticoagulation was shown to be beneficial for non-critically ill patients with COVID-19 in organ support-free days, but not for survival until hospital discharge [32]. Further investigation is warranted.
Our study has several limitations. First, this is a retrospective observational study. Despite rigorous adjustments including multiple imputation for missing data and propensity score analyses, we could not exclude unmeasured confounders. Second, we do not have complete information on the indication for therapeutic anticoagulation, including history of venous thromboembolism, other thrombi, and mechanical valvular surgery.
In conclusion, prophylactic versus therapeutic anticoagulation showed similar in-hospital mortality of COVID-19 patients treated with steroids. Our data supports prophylactic anticoagulation for COVID-19 patients treated with steroids.
References
Nadkarni GN, Lala A, Bagiella E, Chang HL, Moreno PR, Pujadas E et al (2020) Anticoagulation, bleeding, mortality, and pathology in hospitalized patients with COVID-19. J Am Coll Cardiol 76(16):1815–1826
Lee A, deSancho M, Pai M et al (2020) COVID-19 and pulmonary embolism: frequently asked questions. American Society of Hematology. COVID-19 Resources Web site. Version 9.0 updated February 25, 2021. Available from https://www.hematology.org/covid-19/covid-19-and-vte-anticoagulation. Accessed 30 Jun 2021
Group WHOREAfC-TW, Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J et al (2020) Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA 324(13):1330–41
Obata R, Maeda T, Do DR, Kuno T (2020) Increased secondary infection in COVID-19 patients treated with steroids in New York City. Jpn J Infect Dis. https://doi.org/10.7883/yoken.JJID.2020.884
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y et al (2020) Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 369:m1966
Paranjpe I, Fuster V, Lala A, Russak AJ, Glicksberg BS, Levin MA et al (2020) Association of treatment dose anticoagulation with in-hospital survival among hospitalized patients with COVID-19. J Am Coll Cardiol 76(1):122–124
Kuno T, So M, Takahashi M, Egorova NN (2021) U shape association of hemoglobin level with in-hospital mortality for COVID-19 patients. J Thromb Thrombolysis. https://doi.org/10.1007/s11239-021-02516-1
So M, Kabata H, Takahashi M, Egorova NN, Kuno T (2021) The association of inhaled corticosteroid before admission and survival of patients with COVID-19. J Aerosol Med Pulm Drug Deliv. https://doi.org/10.1089/jamp.2021.0020
Kuno T, Takahashi M, Egorova NN (2021) The association between convalescent plasma treatment and survival of patients with COVID-19. J Gen Intern Med. https://doi.org/10.1007/s11606-021-06894-3
Takahashi M, Egorova NN, Kuno T (2021) COVID-19 and influenza testing in New York City. J Med Virol 93(2):698–701
Eikelboom JW, Connolly SJ, Bosch J, Dagenais GR, Hart RG, Shestakovska O et al (2017) Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med 377(14):1319–1330
Chandiramani R, Cao D, Nicolas J, Mehran R (2020) Contrast-induced acute kidney injury. Cardiovasc Interv Ther 35(3):209–217
Austin PC (2009) The relative ability of different propensity score methods to balance measured covariates between treated and untreated subjects in observational studies. Med Decis Mak 29(6):661–677
Yokoyama Y, Briasoulis A, Takagi H, Kuno T (2020) Effect of remdesivir on patients with COVID-19: a network meta-analysis of randomized control trials. Virus Res 288:198137
Maeda T, Obata R, Rizk DD, Kuno T (2020) The association of interleukin-6 value, interleukin inhibitors, and outcomes of patients with COVID-19 in New York City. J Med Virol. https://doi.org/10.1016/j.chest.2020.08.295
Acosta-Ochoa I, Bustamante-Munguira J, Mendiluce-Herrero A, Bustamante-Bustamante J, Coca-Rojo A (2019) Impact on outcomes across KDIGO-2012 AKI criteria according to baseline renal function. J Clin Med 8(9):1323
Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS (2020) Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med 8(7):681–686
Yamakawa M, Kuno T, Mikami T, Takagi H, Gronseth G (2020) Clinical characteristics of stroke with COVID-19: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis 29(12):105288
Zhang Y, Xiao M, Zhang S, Xia P, Cao W, Jiang W et al (2020) Coagulopathy and antiphospholipid antibodies in patients with covid-19. N Engl J Med 382(17):e38
Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E et al (2020) COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 75(23):2950–2973
Zhang L, Feng X, Zhang D, Jiang C, Mei H, Wang J et al (2020) Deep vein thrombosis in hospitalized patients with COVID-19 in Wuhan, China: prevalence, risk factors, and outcome. Circulation 142(2):114–128
Marginean A, Masic D, Brailovsky Y, Fareed J, Darki A (2020) Difficulties of managing submassive and massive pulmonary embolism in the era of COVID-19. JACC Case Rep 2(9):1383–1387
Spyropoulos AC, Weitz JI (2020) Hospitalized COVID-19 patients and venous thromboembolism: a perfect storm. Circulation 142(2):129–132
Piazza G, Campia U, Hurwitz S, Snyder JE, Rizzo SM, Pfeferman MB et al (2020) Registry of arterial and venous thromboembolic complications in patients with COVID-19. J Am Coll Cardiol 76(18):2060–2072
Konstantinides SV (2020) Thrombosis and thromboembolism related to COVID-19: increase the level of awareness, lower the threshold of suspicion, and keep following the guidelines. JACC Case Rep 2(9):1388–1390
Tritschler T, Mathieu ME, Skeith L, Rodger M, Middeldorp S, Brighton T et al (2020) Anticoagulant interventions in hospitalized patients with COVID-19: a scoping review of randomized controlled trials and call for international collaboration. J Thromb Haemost 18:2958
Houston BL, Lawler PR, Goligher EC, Farkouh ME, Bradbury C, Carrier M et al (2020) Anti-thrombotic therapy to ameliorate complications of COVID-19 (ATTACC): study design and methodology for an international, adaptive Bayesian randomized controlled trial. Clin Trials 17(5):491–500
Marietta M, Vandelli P, Mighali P, Vicini R, Coluccio V, D’Amico R et al (2020) Randomised controlled trial comparing efficacy and safety of high versus low low-molecular weight heparin dosages in hospitalized patients with severe COVID-19 pneumonia and coagulopathy not requiring invasive mechanical ventilation (COVID-19 HD): a structured summary of a study protocol. Trials 21(1):574
Full-dose blood thinners decreased need for life support and improved outcome in hospitalized COVID-19 patients. NIH, news release. https://www.nih.gov/news-events/news-releases/full-dose-blood-thinners-decreased-need-life-support-improved-outcome-hospitalized-covid-19-patients. Accessed 30 Jun 2021
Ryan Zarychanski, ATTACC Investigators (2021) Therapeutic anticoagulation in critically ill patients with Covid-19—preliminary report. The REMAP-CAP, ACTIV-4a. https://doi.org/10.1101/2021.03.10.21252749
Investigators R-C, Investigators AC-a, Investigators A, Goligher EC, Bradbury CA, McVerry BJ et al (2021) Therapeutic anticoagulation with heparin in critically ill patients with covid-19. N Engl J Med 385(9):777–89
Investigators A, Investigators AC-a, Investigators R-C, Lawler PR, Goligher EC, Berger JS et al (2021) Therapeutic anticoagulation with heparin in noncritically ill patients with covid-19. N Engl J Med 385(9):790–802
Funding
None.
Author information
Authors and Affiliations
Contributions
TK, MT, NE, had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis. Study concept and design: TK. Data Curation: TK, MT, NE. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: TK. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: TK, MT. Administrative, technical, or material support: NE. Study supervision: NE.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review boards of Icahn School of Medicine at Mount Sinai (#2000495) and conducted in accordance with the principles of the Declaration of Helsinki. The waiver of patients’ informed consent was also approved by the institutional review boards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kuno, T., So, M., Takahashi, M. et al. Prophylactic versus therapeutic anticoagulation for survival of patients with COVID-19 on steroid. J Thromb Thrombolysis 53, 352–358 (2022). https://doi.org/10.1007/s11239-021-02569-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02569-2