Abstract
Heparin-induced thrombocytopenia (HIT) is a clinicopathologic syndrome initiated by heparin exposure and characterized by thrombocytopenia and paradoxical thrombophilia. HIT is mediated by the formation of antibodies against the platelet factor 4/heparin complex, which leads to platelet activation, thrombin generation, and potentially fatal thrombotic sequelae. The clinical presentation of HIT is variable and can be easily overlooked. Although a number of functional and antigen-based immunoassays have been developed to detect the presence of HIT antibodies, initial diagnosis is often based on recognition of thrombocytopenia in the appropriate clinical context and later confirmed with immunologic testing. Given the serious clinical consequences of HIT, immediate cessation of heparin products and administration of non-heparin anticoagulants are crucial components of treatment. We provide a review of the clinical syndrome and practical summary of treatment recommendations from the most recent 2012 American College of Chest Physicians evidence-based guidelines for the treatment and prevention of HIT.
Similar content being viewed by others
Introduction
Heparin-induced thrombocytopenia (HIT) is an adverse drug reaction with potentially fatal thromboembolic complications. The term HIT was first used in the medical literature in 1969 to describe a patient with pulmonary embolism who developed severe thrombocytopenia after receiving heparin [1]. It is now known that this syndrome can be classified into two categories: type I and type II. Type I HIT typically manifests as a decrease in platelet count within the first 2 days after heparin initiation with normalization despite continued heparin use. This form of HIT, which can occur in up to 10–30 % of patients treated with heparin [2], is clinically insignificant and appears to be due to a direct effect of heparin on platelet activation leading to platelet aggregation and, consequently, thrombocytopenia [3]. In contrast, the more serious form, type II HIT is an immune-mediated disorder in which antibodies form against the platelet factor 4 (PF4)/heparin complex. Binding of these antibodies to PF4/heparin complexes on the platelet surface leads to additional platelet activation, further release of PF4, and amplification of the coagulation process, culminating in sustained thrombin generation and risk of thrombosis. Type II HIT is also known as heparin-induced thrombocytopenia and thrombosis (HITT) and white clot syndrome due to platelet-rich arterial thrombosis that may occur with this disorder [4, 5]. Although anti-PF4/heparin antibodies are present in nearly all patients clinically diagnosed with type II HIT, not all antibodies may be pathogenic and/or not all patients may be susceptible to developing HIT, as anti-PF4/heparin antibodies have also been found in patients with heparin exposure without clinical manifestations of HIT [6–8]. Conversely, thrombocytopenia, which commonly occurs outside of the context of HIT, may not be a benign finding, as decreased platelets have been associated with greater in-hospital mortality in a variety of inpatient clinical settings [9].
In February 2012, the American College of Chest Physicians (ACCP) published the 9th edition of evidence-based clinical practice guidelines for the treatment and prevention of HIT [10]. In this article, we provide a brief review of this syndrome and summarize the most recent practice guidelines regarding HIT treatment and management. Per the recommendation grading system used in the ACCP guidelines, Grade 1 indicates that the benefits of a treatment strategy clearly do or do not outweigh the risks, burdens, and costs. Grade 2 is weaker and reserved for strategies in which the relative magnitude of benefits, risks, and costs are more uncertain. Level A recommendations are based on high-quality studies [e.g., multi-center, randomized clinical trials (RCTs) with consistent results]; level B indicates intermediate-quality data (e.g., RCTs with discordant results or with methodologic weaknesses); and level C recommendations are made from data considered to be the lowest quality (e.g., from observational studies or from generalization of results of an RCT conducted in 1 patient population to another similar group that did not participate in the original trial).
Incidence and risk factors
The incidence of immune-mediated HIT depends on the population studied (Table 1), and development of the clinical syndrome has been associated with several risk factors (Table 2). Patients exposed to heparin for more than 4 days have a greater frequency of HIT, with estimates ranging from 0.2 to 5.0 % [11–15] and a reported overall rate of 2.6 % in 1 meta-analysis [11]. In comparison, the incidence of type II HIT in patients receiving unfractionated heparin (UFH) for less than 4 days from 1 large study was 0.2 % [15]. A meta-analysis of randomized and prospective data has shown the incidence of type II HIT to be significantly higher after exposure to UFH versus low-molecular-weight heparin (LMWH) (2.6 vs. 0.2 %) [11], while prospective studies have demonstrated a relative risk (RR) of 5.3 (95 % confidence interval [CI] 2.8–9.9) for developing HIT after treatment with UFH compared with LMWH [16]. Surgical patients are also more likely to develop HIT than medical patients (RR 3.2; 95 % CI 2.0–5.4) [16]. Although antibodies against PF4/heparin may develop in as many as 20–50 % of patients undergoing cardiac surgery versus 3.2–7.5 % of patients undergoing orthopedic surgery, among those with antibodies, the probability of developing HIT is higher among orthopedic than cardiac surgery patients (odds ratio [OR] 21; 95 % CI 2.2–962.8; p = 0.001) [17]. Other factors associated with increased risk of HIT include bovine versus porcine source of heparin [18], intravenous versus subcutaneous route of administration [19], and female versus male sex [16].
Clinical manifestations
Thrombocytopenia is the primary manifestation of HIT, but both the degree and onset of decrease in platelet count can be variable. Type I, or non-immune-mediated HIT, is often characterized by a drop in platelet count within 1–4 days of heparin exposure, with a nadir level of 100,000/μL, spontaneous normalization despite continued heparin administration, and no other clinical sequelae (Table 2). In contrast, type II HIT occurs 5–10 days after initiation of heparin therapy; this timing is consistent with the development of pathologic antibodies which typically form 5 to 8 days after exposure [20]. Platelet counts drop more significantly with immune-mediated HIT, with a median nadir of ~60,000/μL [21]. However, platelet counts with type II HIT are typically >20,000/μL, making spontaneous bleeding rare. Early onset of immune-mediated HIT prior to 5 days after heparin exposure may occur in patients treated with heparin in the prior 1–3 months due to persistent anti-PF4/heparin antibodies. Conversely, cases of delayed-onset HIT occurring a median of 14 days after heparin exposure have been reported and may be due to heparin-independent anti-PF4 antibody platelet activation [22, 23]. Use of the term “HIT” will be used henceforth to refer to type II, immune-mediated HIT.
Thrombosis is the main contributor to morbidity and mortality associated with HIT, and HIT is fatal in an estimated 5–10 % of patients, typically due to thrombotic events [10]. Thrombosis can accompany thrombocytopenia in 30–60 % of patients [24] and may even precede thrombocytopenia in up to 25 % of patients with HIT [25]. Although thrombosis can occur in any vascular bed, venous thrombosis is more common than arterial thrombosis and often presents as deep venous thrombosis or pulmonary embolism [26, 27]. Thrombosis also often occurs at sites of catheter insertion [28]. Two populations in which arterial thromboses may be more common include cardiac and vascular surgery patients [29, 30]. HIT-related thrombosis may present atypically, for example, as bilateral adrenal hemorrhage secondary to adrenal vein thrombosis, skin necrosis at sites of heparin injection, or venous limb gangrene [2, 31]. Importantly, subclinical thrombosis can also occur; the incidence from a single-center study among patients thought to have isolated HIT (without thrombosis) was reported to be ~50 % [32].
Screening
There is no consensus for platelet count monitoring as part of screening for early detection of HIT, but results of such testing may be helpful in calculating pretest probability of HIT. Recommendations for frequency of platelet count monitoring vary according to the estimated risk of HIT and depend on both the population in question and type of heparin therapy considered. In 2002, the College of American Pathologists put forth the following ungraded recommendations: platelet counts should be monitored at least every 2 days from postoperative days 4 through 10 in high-risk patients (2–5 %), i.e., postoperative orthopedic, cardiac, and vascular surgical patients receiving therapeutic doses of UFH for at least 5 days [33]. Patients at lower risk of HIT (0.5 %), such as orthopedic patients receiving LMWH postoperatively, should have 1 or 2 platelet counts checked between postoperative days 5 and 10. Finally, platelet counts should not be monitored in medical or obstetrical patients receiving LMWH, as these populations are at low risk of HIT (<0.2 %). Despite the availability of these guidelines, subsequent studies showed low compliance rates with these recommendations [34, 35].
Recent 2012 practice guidelines from the ACCP for the treatment of HIT include recommendations for platelet count monitoring for patients with a minimum heparin exposure of at least 4 days [10]. These guidelines advocate as a Grade 2C recommendation platelet count monitoring every 2–3 days from days 4 through 14 or until cessation of heparin, whichever occurs first, in patients with >1 % risk of HIT (i.e., all cardiac surgery patients and any postoperative patient without recent heparin exposure treated with therapeutic- or prophylactic-dose UFH; Table 1). In contrast, patients in whom the risk of HIT is considered <1 % (i.e., medical and obstetrical patients, and non-cardiac surgery postoperative patients receiving LMWH or heparin flushes) should not have platelet counts routinely monitored (Grade 2C). Although not a formal recommendation, patients who have had previous exposure to heparin within the past 100 days, however, are suggested to have a baseline platelet count drawn prior to starting heparin or LMWH, and a follow up level drawn 24 h after the initiation of treatment, if possible. Platelet counts should also be drawn after an acute systemic reaction within 30 min of a bolus of intravenous heparin, though this again is not a formal ACCP recommendation. It should be noted that although the ACCP guidelines do include specific recommendations for platelet count monitoring, the risk–benefit ratio of these practices is uncertain, and hence, these recommendations were not based upon consensus agreement (e.g., >20 % of participants voted against inclusion of each of these recommendations) [10].
Diagnosis
The diagnosis of HIT, a clinicopathologic syndrome, relies on clinical assessment as well as laboratory evaluation. HIT should be suspected in the setting of absolute thrombocytopenia (platelet count <150,000/μL) as well as relative thrombocytopenia (drop in platelet count of at least 50 % from baseline value). However, the diagnosis of HIT should also be considered in the setting of skin necrosis at heparin injection sites, new or progressive thrombosis while receiving a heparin product, and acute systemic anaphylactoid reactions after heparin bolus administration. Given the variable pattern of presentation of thrombocytopenia and multiple other causes of thrombocytopenia, especially in populations at risk for development of HIT, this syndrome can easily remain undetected. The significant associated morbidity and mortality, however, warrant vigilance in monitoring for and early suspicion of HIT.
To aid in the diagnosis of HIT, a pretest clinical score called the “4Ts” was developed and validated (Table 3) [36–39]. A score is calculated based on the following four categories: degree of thrombocytopenia, timing of decrease in platelet count, clinical sequelae such as thrombosis, and presence of other etiologies of thrombocytopenia. Compared with the presence of HIT antibodies detected by ELISA immunoassay, patients with low 4Ts scores (0–3) have a low probability of HIT (0–1.6 %), while intermediate (4–5) or high (6–8) scores are associated with serologic diagnosis of HIT (7.9–28.6 and 21.4–100 %, respectively) [39]. These data suggest that the pretest clinical score may be useful in identifying those in whom laboratory studies are worth pursuing.
Multiple laboratory assays are available to diagnose HIT and are broadly classified into functional and antigen-based assays. Two standard reference functional assays are the 14C-serotonin release assay (SRA), which has high sensitivity and specificity (both >95 %) when performed at experienced centers [33, 40], and the heparin-induced platelet aggregation assay, which is specific (>90 %) but not sensitive [41]. Due to limited ability of many clinical laboratories to perform these functional tests, a commercially-available ELISA immunoassay that detects antibodies against the PF4/heparin complex is often used instead. The ELISA is a sensitive antigen-based assay (>90 %) and has a high negative predictive value (95 %) but low specificity, and hence, can be falsely positive, detecting non-pathogenic antibodies in patients without clinical evidence of HIT [40]. More recently, commercial antigen assays that can provide test results faster than the ELISA have become available [36, 42, 43]. However, due to wide availability but low diagnostic specificity of antigen-based studies as a class, the antigen assay is best reserved for use as a screening test that can rule out the diagnosis of HIT if negative, whereas weakly positive (indeterminate) tests or positive tests in patients with low pretest probability both require confirmation with a functional assay [10, 33]. Importantly, studies have found a correlation with the strength of the ELISA reaction, measured in optical density units (OD), and likelihood of clinical HIT [44, 45]. Based on these observations, some have suggested that a combination of >1.0 OD on an ELISA with at least intermediate pretest 4Ts probability of HIT may be as accurate as the standard SRA, though this strategy has not been validated [10].
An important distinction must be made between true HIT and an adverse reaction to heparin contaminants. In 2007 and 2008, hundreds of individuals experienced immediate and heterogeneous reactions to heparin consisting of gastrointestinal distress, cardiac arrhythmias, pharyngeal edema, dizziness, flushing, and hypotension, among other symptoms and signs; such reactions also resulted in a significant number of deaths [46]. Ultimately, these reactions were linked to the presence of several oversulfated heparin by-products, including oversulfated chondrotin sulfate, leading to a voluntary recall of multiple lots of heparin by the drug’s manufacturer [47–50]. While the contaminated heparin was found to complex with PF4 and induce platelet aggregation as well as activate the immune complement system, the mechanistic pathways are unlike those associated with true HIT [51]. The pathogenic sequence of platelet aggregation in HIT is complex and requires the precise association of UFH and PF4 to form linear, multimolecular antigen clusters to which anti-PF4/heparin antibodies then bind, form large immune complexes, and cross-link platelet activation receptors [52–54]. The immunogenicity of PF4/heparin complexes in HIT is also influenced by complex size, abundance, and stability. Given the requirement for anti-PF4/heparin antibody presence in true HIT and overlapping clinical manifestations of HIT and allergies to heparin contamination, serologic tests are necessary to distinguish the two conditions; the ELISA or SRA will be positive in the former but not the latter. Awareness of heparin contamination, associated adverse reactions, and differentiation from true HIT is especially important in light of current availability of generic heparin products.
Treatment
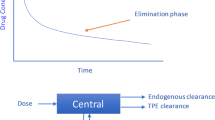
Delays in the availability of diagnostic test results often necessitate initiation of treatment for HIT based on clinical assessment alone. The first step in treatment of HIT is immediate removal of heparin exposure, including heparin flushes and heparin-coated catheters, and inclusion of heparin as an allergy in the patient’s record. In addition to heparin cessation, patients with either HIT with thrombosis or isolated HIT (type II HIT without thrombosis) require further treatment with an alternative anticoagulant; the 30-day risk for subsequent thrombosis with isolated HIT after heparin cessation has been estimated to be as high as 55.5 % [55]. In light of the sustained thrombus propagation that occurs with HIT, current treatment is focused on reduction of thrombin generation via direct thrombin inhibition (e.g., argatroban, lepirudin, bivalirudin) or indirect factor Xa inhibition (e.g., danaparoid, fondaparinux) (Table 4).
While both direct thrombin inhibitors (DTIs) and factor Xa inhibitors have been used to treat patients with HIT, direct comparisons of agents through randomized clinical trials are generally lacking. Recommendations are thus based mainly on historical controlled studies. For patients with HITT, ACCP guidelines recommend use of lepirudin, argatroban, and danaparoid (no longer available in the U.S.) over continuation of heparin products or use of vitamin K antagonist (VKA) therapy (Grade 1C) or other non-heparin anticoagulants (Grade 2C). Patients with HIT with thrombosis and renal insufficiency should be treated with argatroban (Grade 2C), as lepirudin and danaparoid are renally-cleared. In these patients, the ACCP suggests omission of the initial argatroban bolus and initiation of intravenous infusion at ≤2 μg/kg/min. The starting infusion dose in patients with heart failure, multiple organ failure, anasarca, or who are post-cardiac surgery is between 0.5 and 1.2 μg/kg/min, with dosing adjustments every 2 h targeting an activated partial thromboplastin time of 1.5–3 × the patient’s baseline level. Similarly, ACCP recommendations for patients with isolated HIT are for treatment with lepirudin, argatroban, or danaparoid over continuation of heparin products or use of VKA (Grade 1C) or other non-heparin anticoagulants (Grade 2C).
The ACCP guidelines for treatment of HIT also include recommendations for use of platelet transfusions and VKA therapy. Unlike other immune-mediated thrombocytopenic conditions (i.e., immune thrombocytopenic purpura), spontaneous bleeding with HIT is uncommon. Further, platelet transfusions have been reported to increase the risk of thrombosis in HIT patients [56]. Thus, platelet transfusions are only recommended in patients with bleeding or as a prophylactic measure in patients undergoing an invasive procedure with high risk of bleeding (Grade 2C). Regarding VKA therapy, which is typically used for longer-term anticoagulation, initial treatment of HIT should not include this agent as its use may exacerbate hypercoagulability due to faster depletion of protein C than prothrombin [57]. As thrombocytopenia in HIT reflects an ongoing prothrombotic, consumptive state, ACCP guidelines advocate both waiting to start VKA in patients with strongly suspected or confirmed HIT until platelets have recovered (≥150,000/μL) and starting VKA at low doses (maximum of 5 mg warfarin or 6 mg phenprocoumon) as Grade IC recommendations. Moreover, patients in whom VKA has already been initiated at the time of diagnosis of HIT should have their VKA reversed with vitamin K (Grade 2C).
Evidence for duration of treatment of HIT with DTIs, factor Xa inhibitors, or VKA is lacking. However, some data suggest that early discontinuation of thrombin or factor Xa inhibition may increase risk of thrombosis [58]. Consequently, in patients with confirmed HIT, the non-heparin anticoagulant should be overlapped with VKA for at least 5 days and until the international normalized ratio (INR) is within therapeutic range, and a therapeutic INR should be confirmed after resolution of effects of the non-heparin anticoagulant (Grade 1C). Although the duration of VKA therapy in HIT patients has not been well studied, HIT is considered to be a reversible etiology of a hypercoagulable state. As such, the ACCP has put forth a statement but not a formal recommendation suggesting a 3-month duration of VKA or alternative anticoagulant for patients with HITT versus 4 weeks of therapy for patients with isolated HIT.
Special populations
There are certain patient populations in whom management of acute (thrombocytopenic, antibody-positive) or subacute (recovered platelets, antibody-positive) HIT may not be straightforward. Patients undergoing cardiac surgery typically receive significant exposure to heparin, which is used to maintain patency of the cardiopulmonary bypass equipment. Strategies for performing cardiac surgery in HIT patients include substitution with non-heparin anticoagulants, such as bivalirudin, argatroban, or lepirudin, or use of heparin in conjunction with antiplatelet agents, such as glycoprotein IIb/IIIa inhibitors, to reduce platelet activation [10]. However, of these agents, bivalirudin is the only one for which non-randomized data exist supporting use during cardiac surgery in HIT patients [59, 60]. Although the ACCP recommends delay of cardiac surgery, if possible, until both resolution of HIT and absence of HIT antibodies (Grade 2C), in urgent situations, patients with acute or subacute HIT should undergo cardiac surgery with bivalirudin instead of other non-heparin anticoagulants or heparin combined with antiplatelet agents (Grade 2C). In contrast, short-term use of heparin is recommended in patients with a history of HIT but negative antibody status undergoing cardiac surgery (Grade 2C). This is based on 3 observations: (1) HIT antibodies are transient, (2) patients with a history of HIT but who are HIT antibody negative require at least 4 days of heparin exposure for sensitization and do not have a stronger immune response on re-exposure, and (3) patients who have developed HIT within 24 h of re-exposure (“rapid-onset HIT”) have residual HIT antibodies [10]. Thus, in patients with a history of HIT but no detectable HIT antibodies, short-term re-exposure to heparin for <4 days, such as for cardiac surgery, may be possible without triggering another episode of HIT (Table 5).
Another procedure during which heparin is typically used is percutaneous coronary intervention (PCI). Patients undergoing PCI are at high risk for both bleeding and thrombotic complications, and selection of an appropriate procedural antithrombotic agent in the setting of HIT can be particularly challenging. Despite extensive investigations of DTIs and factor Xa inhibitors for use during PCI, these therapies have not been well studied in the context of HIT and have not been directly compared with one another. A pooled analysis of over 19,000 patients from 5 RCTs comparing bivalirudin with heparin plus glycoprotein IIb/IIIa inhibitor during PCI found a similar risk of ischemic outcomes (OR 1.07; 95 % CI 0.96–1.19) but lower risk of major bleeding (OR 0.55; 95 % CI 0.44–0.69) with use of bivalirudin [61], and bivalirudin was similarly associated with high procedural success (98 %) and low bleeding risk (2 %) in a small prospective cohort study of HIT patients undergoing PCI [62]. Data for use of argatroban during PCI in HIT patients is from a secondary analysis of prospective, historical controlled trials and similarly showed high clinical success (98 %) and low incidence of major bleeding (1 %), although the proportion of patients with laboratory-confirmed HIT in this study is uncertain [63]. Data for use of lepirudin in PCI patients with HIT is limited to a single small prospective cohort study that showed an acceptable clinical success rate (92 %) but high incidence of major bleeding (8 %) [64]. After considering the available data, ACCP recommendations for patients with acute or subacute HIT requiring PCI are for treatment with intraprocedural bivalirudin (Grade 2B) or argatroban (Grade 2C).
Although not part of the ACCP practice guidelines, others have suggested that in certain circumstances, consideration of patient risk for acute coronary syndrome (ACS) be taken into account when planning an anticoagulant strategy for PCI in patients with non-acute HIT [65]. Accordingly, clinicians may want to delay PCI in patients with recent HIT (onset >30 days, resolved thrombocytopenia; positive HIT antibody without prior thrombocytopenia; or prior HIT but antibody titer unknown) who are undergoing elective PCI and at low risk of ACS. In this algorithm, once patients have had at least 125 days since most recent heparin exposure or have undetectable HIT antibodies by immunoassay, PCI can be performed safely with heparin. The ACCP recognizes that this approach theoretically parallels their recommendations for patients undergoing non-urgent cardiac surgery and could be applied to patients with a history of HIT requiring PCI. However, ACCP recommendations for non-heparin anticoagulation for PCI in patients with prior HIT, regardless of antibody status, are still for bivalirudin (Grade 2B) or argatroban (Grade 2C). Continued avoidance of re-exposure to heparin is suggested because there is a risk for recurrent sensitization to heparin if the same patient then undergoes cardiac surgery with heparin and because, unlike the case for bivalirudin use during cardiac surgery, experience with bivalirudin in PCI has been favorable [10].
Anticoagulant treatment of several other special populations should also be specifically addressed. Unlike patients undergoing cardiac surgery or PCI, patients with a history of HIT and a new thrombosis (unrelated to HIT) will require long-term anticoagulation. Longer re-exposure to heparin has been associated with higher likelihood of re-formation of HIT antibodies and possible development of clinical HIT [66]. Avoidance of heparin exposure in these patients is thus paramount. If renal function is normal, patients with history of HIT and acute thrombosis unrelated to HIT should be treated with full therapeutic-dose fondaparinux until transition to VKA has been accomplished (Grade 2C). In pregnant patients with HIT, however, fondaparinux is not the first-line agent, as it crosses the placenta. Pregnant patients with acute or subacute HIT should be treated with danaparoid (Grade 2C). In spite of the fact that the highest level of evidence for danaparoid use in this patient population comes from a retrospective case series, this drug does not cross the placenta. If danaparoid is not available, lepirudin or fondaparinux can be used instead (Grade 2C), although this recommendation is based on limited data from case reports [67–70]. Finally, based on limited prospective and pharmacokinetic data [71–73], the ACCP recommends that patients with acute or subacute HIT requiring renal replacement therapy (RRT) be treated with argatroban or danaparoid (Grade 2C). When RRT will be ongoing or if catheter locking is necessary, regional citrate should be used instead of heparin or LMWH (Grade 2C).
Conclusions and future directions
HIT is a serious adverse drug reaction with potentially fatal consequences. Due to wide variability in the clinical presentation and availability of laboratory testing, diagnosis of this syndrome can be difficult. Treatment of thrombosis associated with HIT can also pose a challenge. Despite the availability of a number of non-heparin anticoagulant therapeutic options, very little high-quality data supporting use of these agents in patients with HIT exist. Furthermore, newer oral DTI and factor Xa inhibitor therapies are currently being used to treat other conditions and have potential applications for management of HIT. Studies evaluating the safety and efficacy of newer antithrombotic treatments, as well as those in current use, are needed to inform contemporary treatment of this important condition.
References
Natelson EA, Lynch EC, Alfrey CP Jr, Gross JB (1969) Heparin-induced thrombocytopenia. An unexpected response to treatment of consumption coagulopathy. Ann Intern Med 71:1121–1125
Jang IK, Hursting MJ (2005) When heparins promote thrombosis: review of heparin-induced thrombocytopenia. Circulation 111:2671–2683. doi:10.1161/CIRCULATIONAHA.104.518563
Chong BH (2003) Heparin-induced thrombocytopenia. J Thromb Haemost 1:1471–1478
Warkentin TE, Greinacher A, Koster A, Lincoff AM (2008) Treatment and prevention of heparin-induced thrombocytopenia: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th edition). Chest 133:340S–380S. doi:10.1378/chest.08-0677
Warkentin TE (2004) An overview of the heparin-induced thrombocytopenia syndrome. Semin Thromb Hemost 30:273–283. doi:10.1055/s-2004-831039
Arepally GM, Ortel TL (2006) Clinical practice. Heparin-induced thrombocytopenia. N Engl J Med 355:809–817. doi:10.1056/NEJMcp052967
Lindhoff-Last E, Eichler P, Stein M, Plagemann J, Gerdsen F, Wagner R, Ehrly AM, Bauersachs R (2000) A prospective study on the incidence and clinical relevance of heparin-induced antibodies in patients after vascular surgery. Thromb Res 97:387–393
Foo SY, Everett BM, Yeh RW, Criss D, Laposata M, Van Cott EM, Jang IK (2006) Prevalence of heparin-induced thrombocytopenia in patients undergoing cardiac catheterization. Am Heart J 152(290):e291–e297. doi:10.1016/j.ahj.2006.04.028
Lopes RD, Ohman EM, Granger CB, Honeycutt EF, Anstrom KJ, Berger PB, Crespo EM, Oliveira GB, Moll S, Moliterno DJ, Abrams CS, Becker RC (2009) Six-month follow-up of patients with in-hospital thrombocytopenia during heparin-based anticoagulation [from the Complications After Thrombocytopenia Caused by Heparin (CATCH) registry]. Am J Cardiol 104:1285–1291. doi:10.1016/j.amjcard.2009.06.045
Linkins LA, Dans AL, Moores LK, Bona R, Davidson BL, Schulman S, Crowther M (2012) Treatment and prevention of heparin-induced thrombocytopenia: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e495S–e530S. doi:10.1378/chest.11-2303
Martel N, Lee J, Wells PS (2005) Risk for heparin-induced thrombocytopenia with unfractionated and low-molecular-weight heparin thromboprophylaxis: a meta-analysis. Blood 106:2710–2715. doi:10.1182/blood-2005-04-1546
Warkentin TE, Levine MN, Hirsh J, Horsewood P, Roberts RS, Gent M, Kelton JG (1995) Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med 332:1330–1335. doi:10.1056/NEJM199505183322003
Harbrecht U, Bastians B, Kredteck A, Hanfland P, Klockgether T, Pohl C (2004) Heparin-induced thrombocytopenia in neurologic disease treated with unfractionated heparin. Neurology 62:657–659
Girolami B, Prandoni P, Stefani PM, Tanduo C, Sabbion P, Eichler P, Ramon R, Baggio G, Fabris F, Girolami A (2003) The incidence of heparin-induced thrombocytopenia in hospitalized medical patients treated with subcutaneous unfractionated heparin: a prospective cohort study. Blood 101:2955–2959. doi:10.1182/blood-2002-07-2201
Smythe MA, Koerber JM, Mattson JC (2007) The incidence of recognized heparin-induced thrombocytopenia in a large, tertiary care teaching hospital. Chest 131:1644–1649. doi:10.1378/chest.06-2109
Warkentin TE, Sheppard JA, Sigouin CS, Kohlmann T, Eichler P, Greinacher A (2006) Gender imbalance and risk factor interactions in heparin-induced thrombocytopenia. Blood 108:2937–2941. doi:10.1182/blood-2005-11-012450
Warkentin TE, Sheppard JA, Horsewood P, Simpson PJ, Moore JC, Kelton JG (2000) Impact of the patient population on the risk for heparin-induced thrombocytopenia. Blood 96:1703–1708
Francis JL, Palmer GJ 3rd, Moroose R, Drexler A (2003) Comparison of bovine and porcine heparin in heparin antibody formation after cardiac surgery. Ann Thorac Surg 75:17–22
Ban-Hoefen M, Francis C (2009) Heparin induced thrombocytopenia and thrombosis in a tertiary care hospital. Thromb Res 124:189–192. doi:10.1016/j.thromres.2009.01.006
Warkentin TE, Kelton JG (2001) Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med 344:1286–1292. doi:10.1056/NEJM200104263441704
Warkentin TE (1998) Clinical presentation of heparin-induced thrombocytopenia. Semin Hematol 35:9–16
Warkentin TE, Makris M, Jay RM, Kelton JG (2008) A spontaneous prothrombotic disorder resembling heparin-induced thrombocytopenia. AmJ Med 121:632–636. doi:10.1016/j.amjmed.2008.03.012
Rice L, Attisha WK, Drexler A, Francis JL (2002) Delayed-onset heparin-induced thrombocytopenia. Ann Intern Med 136:210–215
Greinacher A, Farner B, Kroll H, Kohlmann T, Warkentin TE, Eichler P (2005) Clinical features of heparin-induced thrombocytopenia including risk factors for thrombosis. A retrospective analysis of 408 patients. Thromb Haemost 94:132–135. doi:10.1267/THRO05010132
Lubenow N, Warkentin TE, Greinacher A, Wessel A, Sloane DA, Krahn EL, Magnani HN (2006) Results of a systematic evaluation of treatment outcomes for heparin-induced thrombocytopenia in patients receiving danaparoid, ancrod, and/or coumarin explain the rapid shift in clinical practice during the 1990s. Thromb Res 117:507–515. doi:10.1016/j.thromres.2005.04.011
Lewis BE, Wallis DE, Berkowitz SD, Matthai WH, Fareed J, Walenga JM, Bartholomew J, Sham R, Lerner RG, Zeigler ZR, Rustagi PK, Jang IK, Rifkin SD, Moran J, Hursting MJ, Kelton JG (2001) Argatroban anticoagulant therapy in patients with heparin-induced thrombocytopenia. Circulation 103:1838–1843
Wallis DE, Workman DL, Lewis BE, Steen L, Pifarre R, Moran JF (1999) Failure of early heparin cessation as treatment for heparin-induced thrombocytopenia. Am J Med 106:629–635
Hong AP, Cook DJ, Sigouin CS, Warkentin TE (2003) Central venous catheters and upper-extremity deep-vein thrombosis complicating immune heparin-induced thrombocytopenia. Blood 101:3049–3051. doi:10.1182/blood-2002-05-1448
Warkentin TE, Greinacher A (2003) Heparin-induced thrombocytopenia and cardiac surgery. Ann Thorac Surg 76:638–648
Gruel Y, Pouplard C, Nguyen P, Borg JY, Derlon A, Juhan-Vague I, Regnault V, Samama M (2003) Biological and clinical features of low-molecular-weight heparin-induced thrombocytopenia. Br J Haematol 121:786–792
Warkentin TE, Roberts RS, Hirsh J, Kelton JG (2005) Heparin-induced skin lesions and other unusual sequelae of the heparin-induced thrombocytopenia syndrome: a nested cohort study. Chest 127:1857–1861. doi:10.1378/chest.127.5.1857
Tardy B, Tardy-Poncet B, Fournel P, Venet C, Jospe R, Dacosta A (1999) Lower limb veins should be systematically explored in patients with isolated heparin-induced thrombocytopenia. Thromb Haemost 82:1199–1200
Warkentin TE (2002) Platelet count monitoring and laboratory testing for heparin-induced thrombocytopenia. Arch Pathol Lab Med 126:1415–1423. doi:10.1043/0003-9985(2002)126<1415:PCMALT>2.0.CO;2
ten Berg MJ, van den Bemt PM, Huisman A, Schobben AF, Egberts TC, van Solinge WW (2009) Compliance with platelet count monitoring recommendations and management of possible heparin-induced thrombocytopenia in hospitalized patients receiving low-molecular-weight heparin. Ann Pharmacother 43:1405–1412. doi:10.1345/aph.1L646
Rogers BA, Cowie AS (2010) The monitoring of heparin induced thrombocytopenia following surgery: an audit and international survey. J Perioper Pract 20:66–69
Denys B, Stove V, Philippe J, Devreese K (2008) A clinical-laboratory approach contributing to a rapid and reliable diagnosis of heparin-induced thrombocytopenia. Thromb Res 123:137–145. doi:10.1016/j.thromres.2008.04.020
Bryant A, Low J, Austin S, Joseph JE (2008) Timely diagnosis and management of heparin-induced thrombocytopenia in a frequent request, low incidence single centre using clinical 4T’s score and particle gel immunoassay. Br J Haematol 143:721–726. doi:10.1111/j.1365-2141.2008.07401.x
Warkentin TE, Linkins LA (2010) Non-necrotizing heparin-induced skin lesions and the 4T’s score. J Thromb Haemost 8:1483–1485. doi:10.1111/j.1538-7836.2010.03880.x
Lo GK, Juhl D, Warkentin TE, Sigouin CS, Eichler P, Greinacher A (2006) Evaluation of pretest clinical score (4 T’s) for the diagnosis of heparin-induced thrombocytopenia in two clinical settings. J Thromb Haemost 4:759–765. doi:10.1111/j.1538-7836.2006.01787.x
Napolitano LM, Warkentin TE, Almahameed A, Nasraway SA (2006) Heparin-induced thrombocytopenia in the critical care setting: diagnosis and management. Crit Care Med 34:2898–2911. doi:10.1097/01.CCM.0000248723.18068.90
Chong BH, Burgess J, Ismail F (1993) The clinical usefulness of the platelet aggregation test for the diagnosis of heparin-induced thrombocytopenia. Thromb Haemost 69:344–350
Bakchoul T, Giptner A, Najaoui A, Bein G, Santoso S, Sachs UJ (2009) Prospective evaluation of PF4/heparin immunoassays for the diagnosis of heparin-induced thrombocytopenia. J Thromb Haemost 7:1260–1265. doi:10.1111/j.1538-7836.2009.03465.x
Warkentin TE, Sheppard JI, Moore JC, Sigouin CS, Kelton JG (2008) Quantitative interpretation of optical density measurements using PF4-dependent enzyme-immunoassays. J Thromb Haemost 6:1304–1312. doi:10.1111/j.1538-7836.2008.03025.x
Altuntas F, Matevosyan K, Burner J, Shen YM, Sarode R (2008) Higher optical density of an antigen assay predicts thrombosis in patients with heparin-induced thrombocytopenia. EurJ Haematol 80:429–435. doi:10.1111/j.1600-0609.2008.01035.x
Zwicker JI, Uhl L, Huang WY, Shaz BH, Bauer KA (2004) Thrombosis and ELISA optical density values in hospitalized patients with heparin-induced thrombocytopenia. J Thromb Haemost 2:2133–2137. doi:10.1111/j.1538-7836.2004.01039.x
Ramacciotti E, Wahi R, Messmore HL (2008) Contaminated heparin preparations, severe adverse events and the contact system. Clin Appl Thromb Hemost 14:489–491. doi:10.1177/1076029608324291
Hoppensteadt DA, Wahi R, Adiguzel C, Iqbal O, Ramacciotti E, Bick RL, Messmore HL, Bansal V, Fareed J (2008) Contaminant in the recalled unfractionated heparin preparations: where is the problem? Clin Appl Thromb Hemost 14:261–266. doi:10.1177/1076029608317932
Kishimoto TK, Viswanathan K, Ganguly T, Elankumaran S, Smith S, Pelzer K, Lansing JC, Sriranganathan N, Zhao G, Galcheva-Gargova Z, Al-Hakim A, Bailey GS, Fraser B, Roy S, Rogers-Cotrone T, Buhse L, Whary M, Fox J, Nasr M, Dal Pan GJ, Shriver Z, Langer RS, Venkataraman G, Austen KF, Woodcock J, Sasisekharan R (2008) Contaminated heparin associated with adverse clinical events and activation of the contact system. N Engl J Med 358:2457–2467. doi:10.1056/NEJMoa0803200
Guerrini M, Beccati D, Shriver Z, Naggi A, Viswanathan K, Bisio A, Capila I, Lansing JC, Guglieri S, Fraser B, Al-Hakim A, Gunay NS, Zhang Z, Robinson L, Buhse L, Nasr M, Woodcock J, Langer R, Venkataraman G, Linhardt RJ, Casu B, Torri G, Sasisekharan R (2008) Oversulfated chondroitin sulfate is a contaminant in heparin associated with adverse clinical events. Nat Biotechnol 26:669–675. doi:10.1038/nbt1407
Pan J, Qian Y, Zhou X, Pazandak A, Frazier SB, Weiser P, Lu H, Zhang L (2010) Oversulfated chondroitin sulfate is not the sole contaminant in heparin. Nat Biotechnol 28:203–207. doi:10.1038/nbt0310-203 author reply 207-211
Yi Q, Jing P, Xiaodong Z, Weiser P, Hong L, Shih FF, Porche-Sorbet R, Eby C, Lijuan Z (2010) Heparin and oversulfated heparin byproduct induce thrombin generation through contact system activation in plasma of patients with HIT. Clin Appl Thromb Hemost 16:251–260. doi:10.1177/1076029610362072
Greinacher A (2009) Heparin-induced thrombocytopenia. J Thromb Haemost 7:9–12. doi:10.1111/j.1538-7836.2009.03385.x
Suvarna S, Espinasse B, Qi R, Lubica R, Poncz M, Cines DB, Wiesner MR, Arepally GM (2007) Determinants of PF4/heparin immunogenicity. Blood 110:4253–4260. doi:10.1182/blood-2007-08-105098
Greinacher A, Potzsch B, Amiral J, Dummel V, Eichner A, Mueller-Eckhardt C (1994) Heparin-associated thrombocytopenia: isolation of the antibody and characterization of a multimolecular PF4-heparin complex as the major antigen. Thromb Haemost 71:247–251
Warkentin TE, Kelton JG (1996) A 14-year study of heparin-induced thrombocytopenia. Am J Med 101:502–507
Babcock RB, Dumper CW, Scharfman WB (1976) Heparin-induced immune thrombocytopenia. N Engl J Med 295:237–241. doi:10.1056/NEJM197607292950501
Warkentin TE, Elavathil LJ, Hayward CP, Johnston MA, Russett JI, Kelton JG (1997) The pathogenesis of venous limb gangrene associated with heparin-induced thrombocytopenia. Ann Intern Med 127:804–812
Hursting MJ, Lewis BE, Macfarlane DE (2005) Transitioning from argatroban to warfarin therapy in patients with heparin-induced thrombocytopenia. Clin Appl Thromb Hemost 11:279–287
Koster A, Dyke CM, Aldea G, Smedira NG, McCarthy HL II, Aronson S, Hetzer R, Avery E, Spiess B, Lincoff AM (2007) Bivalirudin during cardiopulmonary bypass in patients with previous or acute heparin-induced thrombocytopenia and heparin antibodies: results of the CHOOSE-ON trial. Ann Thorac Surg 83:572–577. doi:10.1016/j.athoracsur.2006.09.038
Dyke CM, Aldea G, Koster A, Smedira N, Avery E, Aronson S, Spiess BD, Lincoff AM (2007) Off-pump coronary artery bypass with bivalirudin for patients with heparin-induced thrombocytopenia or antiplatelet factor four/heparin antibodies. Ann Thorac Surg 84:836–839. doi:10.1016/j.athoracsur.2007.04.007
Lee MS, Liao H, Yang T, Dhoot J, Tobis J, Fonarow G, Mahmud E (2011) Comparison of bivalirudin versus heparin plus glycoprotein IIb/IIIa inhibitors in patients undergoing an invasive strategy: a meta-analysis of randomized clinical trials. Int J Cardiol 152:369–374. doi:10.1016/j.ijcard.2010.08.007
Mahaffey KW, Lewis BE, Wildermann NM, Berkowitz SD, Oliverio RM, Turco MA, Shalev Y, Ver Lee P, Traverse JH, Rodriguez AR, Ohman EM, Harrington RA, Califf RM (2003) The anticoagulant therapy with bivalirudin to assist in the performance of percutaneous coronary intervention in patients with heparin-induced thrombocytopenia (ATBAT) study: main results. J Invasive Cardiol 15:611–616
Lewis BE, Matthai WH Jr, Cohen M, Moses JW, Hursting MJ, Leya F (2002) Argatroban anticoagulation during percutaneous coronary intervention in patients with heparin-induced thrombocytopenia. Catheter Cardiovasc Intervent 57:177–184. doi:10.1002/ccd.10276
Cochran K, DeMartini TJ, Lewis BE, J OB, Steen LH, Grassman ED, Leya F (2003) Use of lepirudin during percutaneous vascular interventions in patients with heparin-induced thrombocytopenia. J Invasive Cardiol 15:617–621
Jolicoeur EM, Wang T, Lopes RD, Ohman EM (2007) Percutaneous coronary interventions in patients with heparin-induced thrombocytopenia. Curr Cardiol Rep 9:396–405
Lubenow N, Kempf R, Eichner A, Eichler P, Carlsson LE, Greinacher A (2002) Heparin-induced thrombocytopenia: temporal pattern of thrombocytopenia in relation to initial use or reexposure to heparin. Chest 122:37–42
Mehta R, Golichowski A (2004) Treatment of heparin induced thrombocytopenia and thrombosis during the first trimester of pregnancy. J Thromb Haemost 2:1665–1666. doi:10.1111/j.1538-7836.2004.00883.x
Chapman ML, Martinez-Borges AR, Mertz HL (2008) Lepirudin for treatment of acute thrombosis during pregnancy. Obstet Gynecol 112:432–433. doi:10.1097/AOG.0b013e31817788e0
Gerhardt A, Zotz RB, Stockschlaeder M, Scharf RE (2007) Fondaparinux is an effective alternative anticoagulant in pregnant women with high risk of venous thromboembolism and intolerance to low-molecular-weight heparins and heparinoids. Thromb Haemost 97:496–497
Mazzolai L, Hohlfeld P, Spertini F, Hayoz D, Schapira M, Duchosal MA (2006) Fondaparinux is a safe alternative in case of heparin intolerance during pregnancy. Blood 108:1569–1570. doi:10.1182/blood-2006-03-009548
Link A, Girndt M, Selejan S, Mathes A, Bohm M, Rensing H (2009) Argatroban for anticoagulation in continuous renal replacement therapy. Crit Care Med 37:105–110. doi:10.1097/CCM.0b013e3181932394
Polkinghorne KR, McMahon LP, Becker GJ (2002) Pharmacokinetic studies of dalteparin (Fragmin), enoxaparin (Clexane), and danaparoid sodium (Orgaran) in stable chronic hemodialysis patients. Am J Kidney Dis 40:990–995. doi:10.1053/ajkd.2002.36331
Henny CP, ten Cate H, Surachno S, Stevens P, Buller HR, den Hartog M, ten Cate JW (1985) The effectiveness of a low molecular weight heparinoid in chronic intermittent haemodialysis. Thromb Haemost 54:460–462
Shantsila E, Lip GY, Chong BH (2009) Heparin-induced thrombocytopenia. A contemporary clinical approach to diagnosis and management. Chest 135:1651–1664. doi:10.1378/chest.08-2830
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hess, C.N., Becker, R.C., Alexander, J.H. et al. Antithrombotic therapy in heparin-induced thrombocytopenia: guidelines translated for the clinician. J Thromb Thrombolysis 34, 552–561 (2012). https://doi.org/10.1007/s11239-012-0785-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-012-0785-8