Abstract
Under-five mortality is known to be the result of a wide variety of inputs, among which the availability of maternal and child health services. However, their coverage and distribution, in low- and middle-income countries, continue to remain inadequate and characterized by significant inequalities. The main aim of this study is to investigate the causes of inequality in accessing the basic maternal and newborn healthcare services in Bangladesh. To this end, we use nationally representative cross-sectional data from the Bangladesh Demographic and Health Survey (BDHS), 2014. Our study builds on the Human Opportunity Index (HOI), developed at the World Bank (in World development report: Equity and development, World Bank, Washington, 2006), which measures the total contribution of individual socioeconomic and demographic circumstances to inequality of opportunity in accessing basic services. Our findings reveal that a mother’s education, wealth index and place of residence, are closely associated with access to basic maternal and newborn healthcare services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Key messages
-
Under-five mortality is known to be the result of a wide variety of inputs, among which the availability of maternal and child health services.
-
Maternal and child health services coverage in low- and middle-income countries is still relatively poor especially for disadvantaged groups.
-
Our study builds on the Human Opportunity Index (HOI), developed at the World Bank (2006), and measures the total contribution of individual socioeconomic and demographic circumstances to inequality of opportunity in accessing maternal and newborn healthcare basic services.
-
Our findings show that mother’s education, wealth index and place of residence are closely associated with access to basic maternal and newborn healthcare services.
-
Even though Bangladesh has made substantial progress over the last decades regarding maternal and child health indicators, the inequality of opportunity, as well as the average coverage, demonstrate that there are still significant gaps in ensuring equitable access to maternal and newborn healthcare services.
1 Introduction
According to the most recent estimates by the World Health Organization, in 2019, 5.2 million children under five years died, mostly from preventable and treatable causes (WHO, 2019). In the Sub-Saharan African and central and Southern Asian regions, under-five mortality continues to be a critical issue and substantial inequalities between sub-groups of the population still exist within countries (United Nations Inter-Agency Group for Child Mortality—UNIGME, 2018). Under-five mortality is known to be the result of a wide variety of inputs, among which the availability of maternal and child health services, whose coverage in low- and middle-income countries are still relatively poor especially for disadvantaged groups (Hanmer et al., 2003).
The main aim of this study is to investigate the inequality of opportunity in accessing basic maternal and newborn healthcare services in Bangladesh. Although in Bangladesh there has been a significant decline in the child and neonatal mortality rates over the last decades, appropriate measures are still required to meet the targets set by Sustainable Development Goal (SDG) (Rajia et al., 2019); inequality still persists especially owing to difficulties in accessing basic healthcare services due to cultural and economic barriers that negatively impact maternal and child health.
Bangladesh is a developing country in Southeast Asia sharing borders with India and Myanmar. Since 1972, the country has made remarkable progress in terms of economic development: Gross National Income (GNI) per capita rose from $100 to $1480 in 2017 (World Bank, 2017). The country has been characterized by fast urbanization over the last decades with 37.41% of the population living in the urban centers of the country in 2019 (Statista, 2020). The high population density, coupled with high urbanization rates, has created an important challenge on existing infrastructure capacities of urban centers to provide adequate living standards. The issue of Rohingya refugees from Myanmar adds further strain on the infrastructure services.
The country is ranked 7th on the climate risk index in the world: the settlements suffer from frequent flooding, which severely impacts the agricultural and other livelihood activities, leading to economic instability, food insecurity and often results in migration in the country.
Bangladesh has made substantial progress over the last decades regarding maternal and child level health indicators. Between 1990 and 2018, the neonatal mortality dropped from 63 to 17 per 1000 live births (UNIGME, 2019). The under-five mortality rate decreased from 144 per 1000 live births in 1990 to 30 per 1000 live births in 2018 (UNIGME, 2019). Nevertheless, the burden of the neonatal and under-five mortality continues to remain an important concern.
The country has a rather low per capita healthcare expenditure, namely about 3.35% of its GDP (Mahmudur, 2018). Socio-economic and geographic inequalities act as barriers for children and mothers to receive adequate healthcare (Jensen & Stewart, 2003; Rubayet et al., 2012). The use of traditional healthcare practices, such as the reliance on a traditional birth attendant, still dominates in the country especially in rural areas of Bangladesh, where most births take place at home.Footnote 1 Improving awareness and adequate access to healthcare services for mothers and children remain a concrete issue in order to achieve the targets related to the SDG 3 (Good Health and Well-Being). SDG 3.2.1 for Bangladesh aims at reducing the under-five mortality rate to 25 per 1000 live births by 2030 and SDG 3.2.2 at reducing the neonatal mortality rate to 12 per 1000 live births (SDG Tracker, 2020).
Healthcare in Bangladesh is provided by both public and private organizations. The healthcare system is based on a decentralized structure with a three-tier setup of primary healthcare services with Upzala Health Complexes (UHC) at sub-district level, Union Health and Family Welfare Centres (UHFWC) at the Union (collection of few villages) level, and Community Clinics (CC) at the village level.Footnote 2 These are backed by the District Hospitals providing secondary level care and the tertiary hospitals of various kind in large urban centres. The private facilities are usually concentrated in urban areas of the country, where the treatment costs are generally higher and not affordable by the disadvantaged segments of the society. The government-based facilities provide subsidized rates or free treatment for a certain marginalized section of the society, but the majority of treatments are characterized by out-of-pocket expenditure. The government run facilities face the challenge of the lack of infrastructure, lack of skilled professionals, poor service delivery and low-quality care due to inadequate financing (Islam & Biswas, 2014; Osman & Bennett, 2018).
Despite economic progress, which has characterized Bangladesh, the country continues to suffer from several development challenges such as high poverty, climate change related disasters, unplanned urbanization and internal displacement. The most socio-economic vulnerable groups continue to face difficulties in accessing basic healthcare services (Hamid et al., 2015).
The main aim of this study is to investigate the causes of inequality in accessing the basic maternal and newborn healthcare services in Bangladesh. To this end, we use nationally representative cross-sectional data from the Bangladesh Demographic and Health Survey (BDHS), 2014. Specifically, our study focuses on four maternal and newborn health services: births taking place at a hospital facility; births being attended by a skilled professional; whether the child received any vaccination and postnatal checkup (within 2 months after delivery). Our study builds on the Human Opportunity Index (HOI) developed at the World Bank (2006) which measures how socioeconomic and demographic circumstances affect inequality of opportunity in accessing basic services (Barros et al., 2012). We also break down the inequality by circumstances using Shapley’s decomposition method. This method indicates the contribution of each circumstance variable to the total inequality of opportunity. Compared to other measures of inequality in healthcare access, the HOI presents the advantage of combining the availability of an opportunity ( i.e. the coverage rate) over the population with a measure of how equitably the opportunity is distributed among population groups with different characteristics (i.e. circumstances). Decompositions are used to assess the contribution of each individual circumstance to inequality of opportunity.
Several studies have been carried out to measure inequality in accessing child and maternal healthcare services in relation to social and economic determinants (see for instance Collin et al., 2007; Nazmul & Tarana, 2008; Amin et al., 2010; Anwar et al., 2015; Chowdhury et al., 2017; Singh et al.,; 2017). However, to the best our knowledge, none of these studies have focused on Bangladesh and used the HOI index and Shapley’s decomposition. Our analysis aims to shed light on these aspects, especially on the circumstances that may influence maternal and child healthcare access.
2 Literature Review
As mentioned, under-five mortality remains a major challenge to the health systems of low-income countries. Maternal and newborn healthcare services (such as hospital deliveries, skilled attendance at birth, postnatal care and child immunization) can contribute to the reduction of the under-five mortality rate but they are often only accessible to the better-off and the poor-rich gap continues to persist. Many studies, focused on developing countries, have documented the differentials in the uptake of such services, which may be influenced by circumstances such as the family's economic status and other socio-geographic indicators such as education and urban–rural residence.
Singh’s analysis (2011) on the HOI relied on the Indian National Health Family survey data for 1993 and 2006 to measure inequality in immunization and nutrition among Indian children. As for indicators of immunization, he used whether a child has received vaccines for tuberculosis, diphtheria, whooping cough, tetanus, polio and measles. As indicators of nutrition, he applied the criteria of underweight by analyzing weight for age. The circumstance variables employed in the study were caste of the household head, religion, child gender, place of residence, wealth quintiles, average parental education and number of siblings. The results indicate that there are high levels of inequality for both immunization and nutrition with substantial geographic variations.
The study by Amara and Jemmali (2017) examined inequality of opportunity in maternal and newborn health services and child nutrition in Tunisia using the Multiple Indicator Cluster Survey data for 2011–2012 and HOI index. Among the indicators of maternal and newborn health services, they included antenatal care, births taking place at health facilities, births being attended by a skilled health professional, the child having postnatal check-up, health examination and regular immunizations within one year after birth, as well as access to safe water and access to toilets. Nutrition comprised indicators of stunting, wasting, underweight and whether the mother has had blood tests during her pregnancy status. As for circumstance variables, the authors referred to regions and place of residence (urban or rural), number of children under age of five, household composition, age of household head, gender of household head and mother’s education. The study found low levels of inequality, and with further Shapley’s decomposition, the authors found that the mother’s education, wealth and place of residence are key factors causing inequalities among the Tunisian children.
Sanoussi (2017) analyzed the inequality of opportunities in accessing maternal and child health care in Togo for 1998 and 2013. They computed the HOI using five indicators of access to healthcare and one composite indicator of access to adequate care for children. The indicators were based on antenatal visits, vital signs measurements during pregnancy, whether the birth was attended by a skilled professional, the place of birth (type of health facility) and whether the child received any vaccination. Based on the aforementioned indicators, a composite indicator for access to maternal and child health care was developed which takes the value one if all the conditions for adequate healthcare are met. Concerning the circumstance indicators, they considered the mother’s education, father’s education, mother’s occupation, father’s occupation, household’s wealth, gender of the child, gender of household head, number of children in the household, region and place of residence (urban or rural). They did not provide any decomposition of the HOI; their findings, however, showed that inequalities in accessing adequate care in Togo increased over time.
Saidi and Hamdaoui (2017) examined inequality of opportunities among children in Tunisia on healthcare access and health status using the/a Multiple Indicator Cluster Survey for 2012. The study computed HOI for health service utilization and nutrition indicators. For health service utilization, indicators for prenatal care, testing of blood samples and postnatal care were considered. For nutritional status, indicators were weight for age, length for age and weight for height. The circumstance variables selected were gender, residence, region, mother’s education and annual family income. With the use of Shapley’s decomposition method, the study found that the mother’s education, wealth and geographic factors are the key factors in determining child development outcomes.
Tsawe and Susuman (2020) analyzed the HOI in the use and access to maternal and reproductive healthcare using the Sierra Leone Demographic and Health Survey data for 2008 and 2013. The dependent variables included in this study were antenatal care visits, skilled antenatal care providers, births delivered in a facility, births assisted by a skilled birth attendant and the use of any method of contraception. The circumstance variables used in the study were maternal age, maternal education and marital status, media saturation, household wealth, number of living children and number of household members, region and place of residence. The study concluded that between 2008 and 2013, the HOI improved access to maternal and reproductive healthcare. Overall, the authors found that inequalities declined over time and while employing Shapley’s decomposition method they found that household wealth status, maternal education and place of residence are the most important factors contributing to the inequality.
3 Methods
3.1 Data and Sample Design
This study uses data from the Bangladesh Demographic and Health Survey (BDHS) 2014. The dataset represents the seventh DHS undertaken in Bangladesh. The survey was implemented from June to mid-November 2014, under the National Institute of Population Research and Training (NIPORT) of the Ministry of Health and Family Welfare and provides information on demographic status, family planning, maternal, child health and healthcare access to basic services.
The BDHS is one of the most comprehensive sources of data available at a household level covering various indicators related to access and use of healthcare services with reported indicators for both mothers and children, along with demographic and household characteristics, and is thus well-suited to this kind of study. The survey is representative of the entire population of the country covering all the seven administrative regions, namely Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur and Sylhet.
The BDHS used four Questionnaires, each one specifically regarding the household, women, men and the community. The indicators employed in this study were taken from the Women’s Questionnaire which covers the topic of maternal and newborn health. The original sample comprised 7886 observations. Questions related to the basic maternal and newborn healthcare services were reported for surviving children only, hence, we removed from the sample the observations where children did not survive (319 observations, about 4% of the original sample).Footnote 3 Questions related to place of delivery and skilled professional attendance at birth were reported for birth taking place preceding three years of the survey for surviving children; hence, we included in our sample only women who had at least one live birth three years preceding the survey (i.e., we removed from the sample 3.3013 observations, about 38% of the original sample).Footnote 4 Since postnatal care for children were reported for the last live birth for the mother in the three years preceding the survey, the sample was further reduced (we removed from the sample 186 observations, about 2% of the original sample). After correcting for the missing values for the variables included in our model, the final sample includes 4.308 observations.Footnote 5
3.2 Defining Opportunities
In this study, the dependent variables (opportunities) are indicators of maternal and newborn healthcare services access, namely: births taking place at a health facility, whether the birth was attended by a skilled professional, whether the child received any vaccination and postnatal checkup (within 2 months after the birth). All indicators are dummy variables. The same indicators have been widely used in previous studies (see, for instance, Sanoussi, 2017; Amara & Jemmali, 2017; Tsawe & Susuman, 2020).
-
(i)
Births taking place at a health facility. Births taking place in a hospital or at a health facility is considered one of the most effective measures to reduce maternal mortality and increase chances for children to survive and enjoy a healthy life (Yesuf et al., 2014). An institutional delivery can better handle complications during delivery and provides a safe environment in ensuring proper health for both the mother and child. Essential newborn care (delayed bath until 72 h of birth; breastfeeding in one hour after birth; drying and wrapping of the newborn within 5 min of birth; application of antiseptic to umbilical cord, etc.) is one of the most fundamental and crucial procedures for neonatal survival (Singh et al., 2017). An institutionalized delivery provides a greater probability for a child to receive all the recommended essential newborn healthcare in a proper manner.
In our study, the responses were categorized as institutionalized deliveries or birth reported at a health facility against the birth taking place at the respondent’s home. As stated above, we constructed a dummy variable which takes a value 1 for births taking place in a health institution such as a hospital/health facility and otherwise 0.
-
(ii)
Births Attended by Skilled Professionals. Births attended by a skilled professional is another key indicator associated with reductions in mortality and morbidity rate for both mothers and the newborn. Trained and accredited professionals are better equipped to deal with the delivery and to better address the complexities involved in both the mother’s and child’s health. A child being delivered by a skilled professional has a higher probability of being born healthy and receiving appropriate care. According to Haider et al. (2018), whose analysis was conducted using data from BDHS 2014, unskilled birth attendants tend to perform less essential newborn care practices compared to skilled birth attendant. It is thus imperative that birth attendants should have proper skills, education and knowledge for delivery that can play a pivotal role in a child’s survival.
Responses involving categories with qualified doctors; nurse/midwife/paramedic; community skilled birth attendant; medical assistant; community healthcare provider and trained traditional birth attendant were considered as skilled professionals for delivery. Whereas responses with a family welfare visitor, an untrained traditional birth attendant, unqualified doctors, friends/neighbors, relatives, no one at all and others, were coded as unskilled birth attendance. This indicator was constructed again as a dummy variable with value 1 for birth being attended by a skilled professional and otherwise 0.
-
(iii)
Whether the child received any vaccination. Vaccination represents one of the most important public health interventions to reduce child deaths from vaccine-preventable diseases. The government of Bangladesh initiated the Expanded Program on Immunization (EPI) in Bangladesh in 1979, with the support of Unicef and WHO. Thanks to EPI, the country has seen a rise in the coverage of immunization services, which include vaccinations against tuberculosis, diphtheria, tetanus, pertussis, poliomyelitis and measles in children less than a year old. The intervention helped the country to achieve a polio-free status in 2001, eradication of neonatal tetanus in 2008 and the highest vaccination coverage rate in comparison with other South Asian countries. Although Bangladesh has had a successful history of immunization and is able to achieve high vaccination coverage against vaccine-preventable diseases, it remains among the top 10 countries with the highest childhood mortality globally (Liu et al., 2015). Immunization coverage suffers from important geographical disparities related to supply-side factors (such as the distance of health facilities and vaccination centers, fragile communication systems in some remote areas) and demand-side factors (religious conservativeness, lower level of literacy that reduces knowledge about the benefits of vaccination for children) that contribute to incomplete vaccination of children (Uddin et al., 2016).
In Bangladesh, immunizations are routinely recorded on a vaccination card. For each child, mothers were asked whether they had the vaccination card and, if so, to show the card to the interviewer. If the mother was able to show the vaccination card, the dates of vaccinations were transferred from the card to the survey questionnaire. If the vaccination card was not available, mothers were asked to recall whether the child had received each vaccine (National Institute of Population Research and Training – NIPORT, 2016; ICF, 2013). Hence, immunization was coded again as a dummy response, with value 1 if respondents were able to show the vaccination card or reported that the child had received each vaccine and 0 otherwise.
-
(iv)
Postnatal checkup for child (within 2 months after birth) The majority of neonatal deaths happen during childbirth or during the postnatal period (WHO, 2022). The postnatal period, as defined by the WHO, concerns the first six weeks after the birth, which are considered a critical time frame for survival and overall development of health indicators for the child. Postnatal care provides an opportunity to check for early on signs of illness. It can help in preventing complications in the newborn related to meningitis, diarrhea, sepsis and pneumonia (Singh et al., 2017).
Again, the variable takes value 1 if a child accessed a postnatal checkup within the first 2 months after his/her birth and 0 otherwise.
3.2.1 Defining Circumstances
Based on the existing literature which employed HOI, a set of circumstances were selected which are also described in Table 1:
-
(i)
Child gender In developing countries, gender still plays a prominent role in access to basic services (Hoyos & Narayan, 2011). It is a critical indicator in assessing the inequality of access to healthcare services for children among Bangladesh and is included as an indicator of circumstance in accordance with the previous literature which relies on HOI.
-
(ii)
Household head gender In developing countries, the head of the household is responsible for the provision of and access to basic services. The indicator will help in representing the inequalities arising due to the gender of household head based on bargaining power and decision making for access to healthcare services for the children.
-
(iii)
The number of children under the age of five in the household This variable may influence a mother’s ability to afford the costs of healthcare services access due to a higher need of care that characterizes this age category. Indeed, the profile of total healthcare expenditure by age is J-shaped: expenditure for newborns is high and decreases with age until the age of 15, it increases only slightly until the age of 45, and it becomes higher at an increasing rate later (Gabriele et al., 2006).
-
(iv)
Mother’s education This variable has been widely used in the literature based on opportunity approaches, the mother’s’ education being the proxy for circumstance in almost all the contributions. A mother’s’ educational attainment has been categorized as “no education”, “primary”, “secondary” and “higher”. No education refers to her not having any formal education, with primary defined as completing grade 5, secondary as completing grade 10 and higher defined as attaining more than grade 10.
-
(v)
Mother’s occupation A mother’s occupation can be considered an indicator of her relative bargaining power in the family, that may influence her ability in accessing healthcare services. Together with the mother’s education, this variable may also capture the effect of the socioeconomic status of a woman on maternal and child health services. Occupational status was defined as employed/unemployed.
-
(vi)
Household wealth As an indicator of household wealth, we employed the wealth index included in the BDHS which is a composite measure of a household's cumulative living standard calculated though the principle component analysis method by assigning weights to the household assets (ownership of land, vehicles, appliances, etc.) and household characteristics (type of material used for floor, roof, etc.) (Filmer & Pritchett, 2001). Based on the scores generated by each household, the sample is divided in quintiles. The index comprises five categories: (i) Poorest, (ii) Poorer, (iii) Middle, (iv) Richer and (v) Richest.
-
(vii)
Place of residence This concerns a binary variable that indicated whether the community where the household is located is of urban or rural nature. Several studies have reported a negative impact of living in rural areas on healthcare utilization. Rural areas in Bangladesh are characterized by a lower concentration of health facilities and infrastructures; the distances to health care facilities and the poor condition of roads to arrive at the point of delivery may lead to a decrease in the access to healthcare services (O’Donnell, 2007; Murawski & Church, 2009; Bakshi et al., 2015).
-
(viii)
Region of residence of the household. Regions refer to the administrative divisions in Bangladesh, namely: Barisal, Chittagong, Dhaka, Khulna, Rajshahi, Rangpur and Sylhet.
3.3 HOI Approach
The Human Opportunity Index (HOI) comprises two main components: C the average coverage rate of the access to basic maternal and newborn healthcare services. The Dissimilarity Index (D-index) that measures the dissimilarity in access to basic maternal and newborn healthcare services for groups defined by circumstance characteristics (e.g. gender, wealth index, place of residence, etc.) compared with the overall coverage rate C of the population as a whole (de Barros et al., 2009). The D-index ranges from 0 to 1. A D-Index equal to 0 implies that access to basic maternal and newborn healthcare services is the same among the general population no matter one’s particular circumstance; by contrast, a D-index of 1 indicates that a group is completely excluded from the access. When the access to basic maternal and newborn healthcare services are equally distributed among the society the value of the D-index would be equal to 0 (Juárez & Soloaga, 2014; Singh, 2011).
Access to basic maternal and newborn healthcare services are defined as dichotomous outcome variables. Hence, for each type of care (i.e., birth taking place at a health facility, whether the birth was attended by a skilled professional, whether the child received any vaccination and postnatal checkup), we estimate the conditional likelihoods by specifying a binary function between access to care and circumstance variables using a logistic regression model. Then, we estimated the predicted probability of access to care (opportunity) by the i'th individual that is explained by the circumstance variables:
where here \(\widehat{p}\) i denotes the predicted probability for access to healthcare services, m denotes the number of criteria for the circumstances \({x}_{ik}\) (k = 1,…, m); \(\widehat{\beta }\) k are the parameters to be estimated. The coverage rate C for access to healthcare services could be calculated as follows:
where, wi represents the population weight associated to the specific opportunity.
The degree of inequality of opportunity that is explained by the individual’s circumstances is measured by the D-index. Based on the approach of de Barros et al. (2009), D is given as follows:
Thus, the Human Opportunity Index HOI for access to care is shown in the Eq. (4):
HOI is a composite index of two factors: the level or coverage (C) and (1-D) that can be interpreted as equity of opportunity. The policymakers’ objective should be to maximize HOI, which can be achieved either by enhancing the percentage of individuals who have access to the opportunities or by promoting a more equitable distribution of the opportunities or by increasing both coverage and equity. The HOI index ranges between 0 and 1: a higher value of the index means a higher coverage rate of opportunity, while lower inequality through the dissimilarity index.
3.3.1 Shapley Decomposition
After estimating the level of equality of opportunity proxied by the HOI, we assess the marginal contribution of each circumstance variable to inequality in maternal and child health healthcare access using the Shapley decomposition procedure proposed by Shorrocks (2013). The Shapley decomposition consists of estimating the marginal effect in the HOI of each inequality contributor (circumstance) in a specified sequence of elimination (Betti & Lemmi, 2008; Shorrocks, 2013).Footnote 6
Following de Barros et al. (2009), the dissimilarity index depends on the set of the circumstances and its value increases adding more circumstances. For example, if there are two circumstance variables A1 and A2, then D-index (A1, A2) > D-index (A1) and opposite for HOI. According to the Shapley decomposition method, from the set of circumstance variables, each circumstance variable is removed one after the other in a sequence, to measure the marginal effect of the removed variable on the dissimilarity index (Saidi & Hamdaoui, 2017). The new or changed value of the dissimilarity index provides the magnitude of the impact that a particular circumstance has over the overall value of the inequality index.
Let ‘N’ be denoted by the total number of circumstance variables that are present. Let ‘n’ represent the number of circumstance variables selected out of total circumstances N. Let ‘S’ represent the subset of N that does not include a particular circumstance, say ‘T’. Then D(S) denotes the subset without T circumstance, while D (S \(\cup\){T}) denotes the subset that includes the circumstance T, where D represents the dissimilarity index for the opportunity of access to healthcare for the given circumstances. Thus, the inequality for a particular circumstance (T) is given as follows in Eq. (5).
The contribution of T is given as follows:
where the total sum of contributions of all circumstance variables should add up to 100% or 1.
All estimations are carried out with STATA 17. For details on the computational issues (using STATA) we refer to Azevedo et al. (2010) and Suarez (2013).
4 Results
This section is divided into two sub-sections. In the first sub-section, we provide the descriptive statistics and estimates of the coverage rate, D-Index and HOI for maternal and child health services. We estimate the indices for all Bangladesh divisions and for rural and urban areas. In the second sub-section, we provide the Shapley decomposition of the D-Index that provides estimates of the contribution of each circumstance to overall inequality of opportunity and discuss the results.
4.1 Descriptive Statistics, Estimates of the Coverage Rate, D-Index and HOI
Access to appropriate healthcare, especially hospital deliveries and skilled attendance at birth, is closely associated with substantial reductions in mortality and morbidity for both mothers and newborns (Starrs, 2006). According to our descriptive statistics, included in Table 2, few women use health facilities for births and skilled care providers. In our sample, 35% of women gave birth with a skilled care provider and 39% of women reported having given birth at a health institution. Our statistics show that, compared to skilled birthing and institutional delivery service utilization, the access to postnatal checkups and children immunization are relatively higher: 64% of respondents reported to have accessed postnatal checkups and 94% to children immunization.
The descriptive statistics for the circumstance variables are included in Table 3. It is worth noting that the percentage of women without any formal education and with primary education is quite high, while those with a higher level of education are relatively low (around 10% of the sample). In our sample, around 75% of women are unemployed and around 73% live in a rural areas.
Table 4 shows the level of coverage of healthcare services across circumstance variables. For both births taking place at a health facility and births attended by skilled professional indicators, the level of coverage is particularly low among women with no education and among those who belong to the lowest (first and second) wealth quintiles.
Table 5 shows the logit marginal effects for the basic maternal and newborn healthcare services.
A mother’s education, the economic background of the family, the number of children in the household and living in an urban area, all appear to be the most important predictors for accessing maternal and newborn healthcare services.Footnote 7
Based on the predicted probability from the logit model, we estimate inequality of opportunity. Table 6 shows Coverage, D-Index and HOI for the healthcare outcome variables. We also carried out an analysis for place of residence (urban vs. rural area) and for regions.
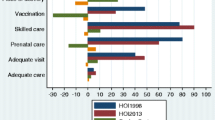
Starting from births taking place at a hospital, we find that the overall coverage rate for Bangladesh is 38.91%. The D-index for the country is equal to 24.69% (see also Fig. 1).
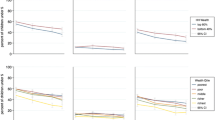
The D- index shows the largest variation between the urban areas and rural areas compared to other services. We also find that there is wide regional variation in terms of coverage and inequality of opportunity. Khulna has the highest coverage of 54.80% with the lowest inequality of 8.69% (see Fig. 2). The region of Barisal presents the highest level of inequality: D-index equal to 32.03%. The region of Sylhet presents the lowest level of coverage, equal to 24.09%, accompanied by the second highest level of inequality: D-index equal to 29.11%.
Despite the increase in rates of facility delivery, home birth is still the norm. Given that the health system in rural Bangladesh is not configured to provide skilled delivery care at home, there is a continued reliance on informal healthcare providers, such as traditional birth attendants (TBAs) especially in rural areas. Rural areas continue to be characterized by a shortage of healthcare professionals and healthcare facilities, thereby increasing their dependency on TBAs which ultimately results in lower access to institutional deliveries that remain relatively very low. In 2009, the government launched the Revitalization of Community Healthcare initiatives to tackle the problem for the rural areas with a community engagement program focused on capacity building for the community clinics in rural areas and by raising awareness for the utilization of primary healthcare in order to reduce maternal and neonatal mortality (Yaya et al., 2017).
Concerning births attended by skilled professionals, our results show that the overall coverage rate for the country is 34.72%, while the D-index is equal to 24.68% (see Fig. 1) with quite a large variation between rural and urban areas: D- index of 15.84% rural areas against a D- index of 10.38% in the urban areas (see Table 6). There is also a large variation across divisions within the country with Sylhet which presents the lowest coverage (equal to 22.97%) and the highest D- index (equal to 30.73%) (see Fig. 3). Despite public information campaigns to raise awareness, training of traditional birth attendants, training of new community based skilled birth attendants and healthcare voucher programs to raise demands for utilization of healthcare services for delivery, the proportion of births attended by skilled professionals in Bangladesh has remained relatively low again especially in rural areas and in some regions (Saha & Odjidja, 2017).
Bangladesh has made significant gains in childhood vaccination coverage. Vaccination presents the lowest level of access inequality compared to the other maternal and new born healthcare services. The overall coverage rate for children immunization is equal to 94.09% and the D-index is approximately 1.49%, the lowest among the healthcare services considered in our study (see Fig. 1). Despite the success, full immunization coverage varies across the country. For instance, immunization coverage is the highest in Dhaka (95.99%) while the lowest coverage is observed in the Sylhet region (85.82%). Figure 4 shows the region wise ranking.
Finally, we find that the overall coverage rate for postnatal checkup for child in Bangladesh is 64.03% (see Fig. 1). The inequality index for rural (2.59%) and urban areas (1.96%) are relatively low (see Table 6). The region of Sylhet presents again the lowest coverage (49.88%) with the D-index equal to 3.96%. While the region of Barisal presents the highest level of inequality accounting for a D-index equal to 7.27%. Figure 5 shows the region-wise ranking.
In 2007, the Ministry of Health and Family Welfare of the Government of Bangladesh implemented the Maternal Health Voucher Scheme, a specialized form of a demand-side financing program to reduce financial, geographical and institutional barriers to access maternal healthcare services for the poorest. Eligible women (identified based on household income and land ownership criterion) were provided with vouchers for various services along with the postnatal care visit within six weeks of delivery. The evaluation of the program resulted in improved postnatal visits among the poor. This success led the Maternal Health Voucher Scheme to be integrated into the government’s main health program known as Health, Population and Nutrition Sector Development Program (HPNSDP) 2011–2016 (Ministry of Health and Family Welfare, 2015).
4.2 Decomposition Results
We also decompose inequality of opportunity using the Shapley value method to find the contribution of individual circumstances. The Shapley decomposition gives percentage contributions of various circumstances to the D-Index. Knowledge about relative contributions is particularly relevant as it enables policymakers to take appropriate measures and concentrate on the largest contributors to reducing inequality of opportunity. The decomposition of the D-index by circumstances is shown in Table 7.
According to the previous literature, Shapley’s decomposition reveals that the family’s welfare (measured through the wealth index) is the most significant contribution to inequality in accessing basic maternal and newborn healthcare services. We also find that the wealth index, mother’s educational level and place of residence (urban/rural) are among the most important contributors to inequality of opportunity. The empirical results show that regional differences contribute in particular to inequality of opportunity in vaccinations.
It is evident from Table 7 that the family’s economic background accounts for the highest contribution to inequality of opportunity in all the maternal and newborn healthcare services. For births taking place at a health facility, births being attended by a skilled professional, postnatal checkups of child and vaccinations, wealth classes contribute to 43.32%, 43.98%, 43.44% and 27.04% of inequality of opportunity respectively.
The second important contributor to inequality of opportunity is the mothers’ educational level. The percentage contribution of a mother’s education to inequality of opportunity is relatively high for all the maternal and newborn healthcare services considered in this study. Looking at each healthcare services, the marginal contribution is higher for births taking place at a health facility and being attended by a skilled professional which accounts for 28.16% and 27.34% of the inequality respectively. A mother’s education in postnatal checkup for the child also shows a contribution of 23.78%. Similarly, for vaccinations, it shows a substantial contribution of 23.24%, which is the lowest among the healthcare services. Concerning vaccinations, it can also be noted that the difference in the contributions of mother’s education and family's economic background is quite low compared to other services. Table 7 shows that the contribution of wealth classes is 27.04%, whereas the education of the mother contributes 23.24% to inequality of opportunity.
The place of residence too appears to be a significant contributor to explaining inequalities for all the healthcare opportunities. There exists a huge difference in the inequality index for urban and rural areas with rural areas always having a higher inequality for all the healthcare opportunities, except for vaccinations. Rural areas tend to suffer from the challenge of the availability of healthcare infrastructure. However, for vaccinations, the place of residence is not as high as compared to other healthcare opportunities with a contribution of 8.40%. For other healthcare opportunities, the place of residence explains between 15 and 20% of inequalities approximately.
Number of children in household (under five) also captures a significant contribution to explaining the inequality of opportunity. For a child receiving vaccination, it is one of the major drivers with large proportion among the circumstance variable that explains the inequality with 20.74%. For the remaining healthcare opportunities, it explains between 4 to 6% of inequality approximately.
According to our decomposition results, mother's occupation is not one of the most important contributors to the inequality of opportunity (less than 5%) with highest being for postnatal checkup for the child for which it accounts for 5.11% of the inequality.
The contribution of regions in explaining inequality for access to healthcare is relatively low. Interestingly, it is one of the significant drivers in explaining inequalities in vaccination with a contribution of 15.44% among the circumstance variables. For postnatal checkup of the child, region explains 2.03% inequality and contributes to less than 2% of the remaining healthcare opportunities inequality.
Gender of household head does not capture a significant contribution toward the inequality of opportunity. Specifically, it explains less than 1% of inequality for births taking place at a hospital, being attended by a skilled professional and postnatal checkup for the child. For children receiving vaccination, it shows a slightly higher contribution of 1.25%.
Finally, gender of child contribution is quite low (less than 1%) among all healthcare opportunities except for vaccination which explains 3.45% of inequality.
5 Discussion
The main aim of this study is to investigate the causes of inequality in accessing the basic maternal and newborn healthcare services in Bangladesh and underline the main drivers of inequality in accessing these services for effective coverage and targeted interventions in the country.
Our results show that maternal education, family wealth and place of residence are the key identifiers responsible for the low healthcare access opportunity in the country. Coverage and opportunities are lower in the rural areas due to the lack of health infrastructure, health professionals and awareness. Specific efforts should be made to provide basic maternal healthcare services to women of lower socio-economic status, especially those living in rural areas where poverty is more prevalent (Cummings et al., 2019). Education levels and wealth are positively associated with the utilization of basic maternal and newborn healthcare services and hence economic and educational improvement of the poor mothers would have a positive effect on reducing the prevalent inequalities.
The region-wise analysis of the index and decomposition helped identify the priority areas for interventions for each region. According to our results, Sylhet exhibits the lowest coverage in all services and the highest D-Index rankings for birth being attended by a skilled professional and a substantial level of inequality in other services in comparison to other regions. The population in Sylhet is less literate, more conservative and faces sociocultural barriers to accessing healthcare services. Geographic barriers also affect the Sylhet division, which mostly covers a remote hilly and riverine area, and healthcare access tends to be more complex. The region is far below in terms of coverage of healthcare and thus should be prioritized for interventions related to access to maternal and newborn healthcare services. While the region of Barisal exhibits the highest D-Index ranking for birth taking place at a health facility, vaccinations and postnatal checkups. Thus in this region, interventions should be targeted in addressing the main causes of inequality.
6 Concluding Remarks
Even though Bangladesh has made substantial progress over the last decades regarding maternal and child health indicators, the inequality of opportunity, as well as the average coverage, demonstrate that there are still significant gaps in ensuring equitable access to maternal and newborn healthcare services. These results point to the need for further efforts by the government of this country to implement policies taking them into account in order to ensure equitable access to healthcare opportunities. Continuous and targeted interventions are required which demands collaboration from both public and private health providers along with effective community participation. Access to basic healthcare services among mothers and children may potentially impact the under-five mortality and improve child health status in Bangladesh. There exists a need to strike a true balance between knowledge building and collaboration among various development sectors to match the vision and implementation in the healthcare sector in Bangladesh in order to achieve progress.
Our study presents the following limitations. Our results are descriptive and based on correlation analysis and not on causal effects. Therefore, they should be taken as potential lines of exploration only. The cross-sectional design of this study involves the evaluation of the characteristics of the individuals and their opportunities at the same point in time making it impossible to disentangle the temporal sequencing of circumstances and opportunities and failing to take the dynamic nature of these phenomena into account. In order to sort out these temporal sequences, long-term studies are needed. However, data of this type are rarely available for developing countries such as Bangladesh. Despite the limitations of the cross-sectional data that do not allow to explore the underlying causal mechanisms that link circumstances and opportunities, we used BDHS data since it collects a wide range of objective and self-reported data with a strong focus on indicators of reproductive health, maternal and child health and healthcare access with high response rates and high national coverage.
Notes
Although Bangladesh has made significant progress in reducing maternal and child mortality in the last decades, childbirth assisted by skilled attendants has not increased as much as expected. In rural areas, professionally trained staff are often in short supply and there is a tendency for women to rely on traditional birth attendants for delivery.
The Upazila, which replaced the oldest institution called Thana, is an administrative subdistrict in Bangladesh. UHCs are primary healthcare centers and the first point of referral.
One of the limitations of our study concerns the fact that the omission of women whose children did not survive from the sample might bias the results toward a more favorable equality of opportunity outcome if children did not survive because of lack of access to services.
In case of multiple births, BDHS, collects data on basic maternal and newborn healthcare services access with reference to the youngest of the multiple births. Twins accounted for 0.75% of the original sample only. We removed twins from the analysis.
To make the sample data representative of the entire population sample weights were employed. The sample weights used in the analysis are those provided in the BDHS dataset.
When different categorical variables represent a single circumstance, we remove them simultaneously as a group. For instance, there are four dummy variables indicating the mother’s education. In the regression analysis, we include three dummy variables as explanatory variables with secondary education as reference category. In various iterations for the decomposition analysis, we simultaneously include or remove all the educational levels from the regression. This process gives the contribution of the mother’s education to total inequality of opportunity. We carry out the same process for the other circumstances that are represented by more than one binary variable.
According to our results the economic background of the family, measured through the wealth index quintiles, does not affect the probability of accessing vaccinations. Actually, this is not surprising since the most important childhood vaccines, in Bangladesh, are made available by the government free of cost under the Expanded Program on Immunization (EPI). Sex of the child, sex of head of household, the mother’s occupation, place of residence were found to be non-significant factors in determining whether or not a child had received full vaccination.
References
Amara, M., & Jemmali, H. (2017). On the decomposition and dynamics of inequality of opportunities: A special focus on early childhood health and nutrition in Tunisia. In Economic Research Forum Working Paper 1093. Giza: Economic Research Forum.
Amin, R., Shah, N. M., & Becker, S. (2010). Socioeconomic factors differentiating maternal and child health-seeking behavior in rural Bangladesh: A cross-sectional analysis. International Journal for Equity in Health, 9, 9.
Anwar, I., Nababan, H. Y., Mostari, S., Rahman, A., & Khan, J. A. M. (2015). Trends and inequities in use of maternal health care services in Bangladesh, 1991–2011. PLoS ONE, 10, e0120309.
Azevedo, J. P., Franco, S., Rubiano, E., & Hoyos, A. (2010). HOI: Stata module to compute Human Opportunity Index. In Statistical Software Components S457191, Boston College Department of Economics.
Bakshi, R. K., Mallick, D., & Ulubaşoğlu, M. A. (2015). Social capital and hygiene practices among the extreme poor in rural Bangladesh. The Journal of Development Studies, 51(12), 1603–1618.
Betti, G., & Lemmi, A. (2008). Advances on income inequality and concentration measures. Taylor & Francis Ltd: Routledge.
Barros, R. P., Molinas Vega, J. R., Chanduvi, J., Giugale, M., & Hasan, A. (2012). Do our children have a chance? A human opportunity report for Latin America and the Caribbean. Washington: World Bank.
Chowdhury, A. H., Hanifi, S. M. A., Mia, M. N., & Bhuiya, A. (2017). Socioeconomic inequalities in under-five mortality in rural Bangladesh: Evidence from seven national surveys spreading over 20 years. International Journal for Equity in Health, 16, 197.
Collin, S. M., Anwar, I., & Ronsmans, C. (2007). A decade of inequality in maternity care : Antenatal care, professional attendance at delivery and caesarean section in Bangladesh (1991–2004). International Journal for Equity in Health, 9, 1–9.
Cummings, S., Seferiadis, A. A., Maas, J., Bunders, J. F. G., & Zweekhorst, M. B. M. (2019). Knowledge, social capital, and grassroots development: Insights from Rural Bangladesh. The Journal of Development Studies, 55, 161–176.
de Barros, P. R., Ferreira, F. H. G., Molinas, V. R., de Barros, R. P., & Chanduvi, S. J. (2009). Measuring inequality of opportunities in Latin America and the Caribbean. Washington: World Bank.
Filmer, D., & Pritchett, L. H. (2001). Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of India. Demography, 38(1), 115–132.
Gabriele, S. Cislaghi, C., Costantini, F. (2006) Demographic Factors and Health Expenditure Profiles by Age: The Case of Italy. ENEPRI Research Reports No. 18.
Haider, M. R., Rahman, M. M., Islam, F., & Khan, M. M. (2018). Are trained delivery assistants better than non-trained personnel in practicing essential newborn care in home deliveries? Evidence from a nationally representative survey in Bangladesh. International Health, 10, 302–309.
Hamid, S. A., Ahsan, S. M., Begum, A., & Asif, C. A. A. (2015). Inequity in formal health care use: Evidence from rural Bangladesh. Journal of International Development, 27, 36–54.
Hanmer, L., Lensink, R., & White, H. (2003). Infant and child mortality in developing countries: Analysing the data for robust determinants. Journal of Development Studies, 40, 101–118.
Hoyos, A., & Narayan, A. (2011). Inequality of Opportunities Among Children: How much does gender matter. Washington: World Bank.
ICF. (2013). Demographic and health surveys standard recode Manual for DHS6. Rockville: The Demographic and Health Surveys Program.
Islam, A., & Biswas, T. (2014). Health System in Bangladesh: Challenges and Opportunities Health system in Bangladesh: Challenges and opportunities. American Journal of Health Research, 6, 366–374.
Jensen, E. R., & Stewart, J. F. (2003). Health facility characteristics and the decision to seek care. Journal of Development Studies, 40, 79–100.
Juárez, F. W. C., & Soloaga, I. (2014). Estimating ex-ante inequality of opportunity. The Stata Journal, 14, 830–846.
Liu, L., Oza, S., Hogan, D., et al. (2015). Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: An updated systematic analysis. Lancet, 385, 430–440.
Mahmudur, R. A. (2018). A review on child and maternal health status of Bangladesh. Chrismed J. Health Res., 5, 1–7.
Ministry of Health and Family Welfare. (2015). Health, population and nutrition sector development program (HPNSDP).
Murawski, L., & Church, R. L. (2009). Improving accessibility to rural health services: The maximal covering network improvement problem. Socio-Economic Planning Sciences, 43, 101–110.
Nazmul, M., & Tarana, H. Æ. (2008). Maternal education and child healthcare in Bangladesh. Maternal and Child Health Journal, 12, 43–51.
National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. (2016). Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh, and Rockville, Maryland: NIPORT, Mitra and Associates, and ICF International.
O’Donnell, O. (2007). Access to health care in developing countries: Breaking down demand side barriers. Cadernos De Saúde Pública, 23, 2820–2834.
Osman, F. A., & Bennett, S. (2018). Political economy and quality of primary health service in rural Bangladesh and the United States of America: A comparative analysis. Journal of International Development, 30, 818–836.
Rajia, S., Sabiruzzaman, M., Islam, M. K., Hossain, M. G., & Lestrel, P. E. (2019). Trends and future of maternal and child health in Bangladesh. PloS one, 14(3), e0211875.
Rubayet, S., Shahidullah, M., Hossain, A., Corbett, E., Moran, A. C., Mannan, I., Matin, Z., Wall, S. N., Pfitzer, A., Mannan, I., & Syed, U. (2012). Bangladesh newborn change and future analysis Group. Newborn survival in Bangladesh: A decade of change and future implications. Health Policy and Planning, 27(Suppl 3 iii), 40–56.
Saha, M., & Odjidja, E. N. (2017). Access to a Skilled Birth Attendant in Bangladesh: What we know and what health system framework can teach us. Health Systems Policy Research, 4(4), 66.
Saidi, A., & Hamdaoui, M. (2017). On measuring and decomposing inequality of opportunity in access to health services among Tunisian children: A new approach for public policy. Health and Quality of Life Outcomes, 15, 213. https://doi.org/10.1186/s12955-017-0777-7
Sanoussi, Y. (2017). Measurement and analysis of inequality of opportunity in access of maternal and child health care in Togo. BMC Health Services Research. https://doi.org/10.1186/s12913-017-2647-8
SDG Tracker: Bangladesh. (2020). Retrieved from http://www.sdg.gov.bd/page/indicator-wise/5/428/3/0#1 accessed on May 22, 2020.
Shorrocks, A. F. (2013). Decomposition procedures for distributional analysis: A unified framework based on the Shapley value. Journal of Economic Inequality, 11, 99–126.
Singh, A. (2011). Inequality of opportunity in Indian Children: the case of immunization and nutrition. Population Research and Policy Review, 30, 861–883.
Singh, K., Brodish, P., Chowdhury, M. E., Biswas, T. K., Kim, E. T., Godwin, C., & Moran, A. (2017). Postnatal care for newborns in Bangladesh: The importance of health-related factors and location. Journal of Global Health, 7(2), 020507.
Starrs, A. (2006). Safe motherhood initiative: 20 years and counting. Lancet, 368, 1130–1132.
Suarez, A. H. (2013). HOISHAPLEY: Stata module to perform Shapley Decomposition of the Human Opportunity Index”, Statistical Software Components S457618, Boston College Department of Economics.
Statista—The Statistics Portal. “Bangladesh: Urbanization from 2009 to 2019”. Retrieved November, 17, 2020, from https://www.statista.com/statistics/455782/urbanization-in-bangladesh/
Tsawe, M., & Susuman, A. S. (2020). Examining inequality of opportunity in the use of maternal and reproductive health interventions in Sierra Leone. Journal of Public Health, 42(2), 254–261.
Uddin, M. J., Shamsuzzaman, M., Horng, L., et al. (2016). Use of mobile phones for improving vaccination coverage among children living in rural hard-to-reach areas and urban streets of Bangladesh. Vaccine, 34, 276–283.
UN Inter–agency Group for Child Mortality (UNIGME). (2018) Child Mortality Estimates 2018. New York: United Nations Children’s Fund.
UN Inter–agency Group for Child Mortality (UNIGME) (2019). Child Mortality Estimates 2019. New York: United Nations Children’s Fund.
Yaya, S., Bishwajit, G., & Ekholuenetale, M. (2017). Factors associated with the utilization of institutional delivery services in Bangladesh. PLoS ONE, 12(2), e0171573.
Yesuf, E. A., Kerie, M. W., & Calderon-Margalit, R. (2014). Birth in a health facility–inequalities among the Ethiopian women: results from repeated national surveys. PloS one, 9(4), e95439.
World Bank. (2006). World development report: Equity and development. Washington: World Bank.
World Bank. (2017). Country Snapshot—Bangladesh, an overview of the World Bank group’s work in Bangladesh, 2010 (October). Retrieved from http://www.worldbank.org/en/country/bangladesh accessed on 20 May, 2020.
World Health Statistics 2019: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2019. License: CC BY-NC-SA 3.0 IGO.
World Health Organization. (2022). WHO recommendations on maternal and newborn care for a positive postnatal experience: executive summary.
Acknowledgements
We are grateful to Elenka Brenna, Stephen Conway, Enico Di Bella, Filomena Maggino, Anna Marenzi, Marcello Montefiori for their helpful comments on previous drafts of this paper. The views expressed in this article are purely those of the authors and may not in any circumstances be regarded as stating an official position of the European Commission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Ethical Approval
This study does not require ethical approval since it involves information freely available in the public domain and the analysis of the data relies on open source database.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Di Novi, C., Thakare, H. Inequality of Opportunity in Accessing Maternal and Newborn Healthcare Services: Evidence from the Bangladesh Demographic and Health Survey. Soc Indic Res 164, 1505–1529 (2022). https://doi.org/10.1007/s11205-022-03004-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-022-03004-6