Abstract
Background
In light of rapid population ageing across Europe, maintaining a high level of wellbeing in old age is a priority for social policy. Research on macro-level influences on wellbeing in the older population is rare, especially regarding heterogeneous effects within different groups, such as persons with and without health limitations.
Objective
The purpose of this study is to shed light on the following questions: Is the regional availability of care infrastructure crucial for the wellbeing in later life? If so, does the relevance of care infrastructure differ depending on an individual’s health status?
Methods
Data were drawn from wave 6 of the Survey of Health, Ageing and Retirement in Europe (SHARE) matched with data on the number of long-term care (LTC) beds on the regional level. We estimated multilevel regression models, including a cross-level interaction between individual health needs and regional LTC beds.
Results
Our analyses show that the number of LTC beds is related to the wellbeing, as measured by overall life satisfaction, in the population aged 50 + years. The association is more pronounced for individuals with health limitations who might be in need of such infrastructure.
Conclusions
Communities and local governments should ensure the necessary infrastructure for older individuals in need of care and help across different regions. The availability of formal care services may be perceived a “safety net” and thus improve wellbeing, but future studies need to investigate the underlying mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Research on wellbeing has mainly investigated its determinants on the individual level, showing that age, gender, social network characteristics, socioeconomic conditions and especially health account for a substantial amount of inter-individual variation in wellbeing (Bonini, 2008). Apart from individual differences there are considerable national differences in wellbeing (Helliwell et al., 2020). Empirical studies have shown that the economic situation, social welfare, the degree of individualism, democracy and freedom affect a nation’s wellbeing (Jorm & Ryan, 2014). Moreover, social infrastructure and healthcare services are related to wellbeing in the overall population (Davern et al., 2017). Regarding the older population, research on macro-level influences on wellbeing is rare. This is a major shortcoming as individual needs regarding public infrastructure and services change across the life course. Older persons are the fastest growing population group in Europe. In 2018, already around 20% of the population were 65 years or older and the share of older adults is expected to rise in the following decades (Eurostat, 2019), so that ensuring living conditions that allow older adults to maintain a high wellbeing is an important task for social policy. Moreover, most of the existing studies compare wellbeing across countries or welfare regimes, although living conditions, including social infrastructure and healthcare services, strongly vary within countries and differ between regions (Wagner & Brandt, 2018). In later life when experiencing health declines and limitations in daily living regional availability of care services is likely to become a central determinant for the wellbeing of older adults.
Based on multilevel regression models with data from the Survey of Health, Ageing and Retirement in Europe (SHARE) this study investigates regional inequalities in the wellbeing of the population aged 50 + in 96 European regions. Apart from several determinants of wellbeing at the individual level, including age, gender, socioeconomic conditions, family relations and health status, we investigate the role of regional long-term care (LTC) infrastructure. This indicator of social infrastructure is potentially especially relevant as substantial share of the older population suffers from health limitations and thus likely be dependent on professional care services one day. A well-developed care infrastructure may be thus perceived a “safety net” in case of (expected) care dependency and thus improve older age wellbeing. Following studies on regional influences on caregiver wellbeing (e.g., Wagner & Brandt, 2018) and transferring results to the overall older population, this study tests if the association between care infrastructure and wellbeing is more pronounced for individuals with health limitations, as they may be more in need of such services than their healthier counterparts.
The following sections provide an overview on prior research on the determinants of wellbeing. We then describe the data and methods used. After presenting the empirical results, we discuss our findings and draw conclusions for social policy in Europe’s ageing societies.
2 Determinants of Wellbeing: Concepts and Empirical Findings
Wellbeing is an umbrella term used to describe the subjective evaluation of a person’s life. According to Diener (1994), there are three important characteristics of wellbeing. “First, it is subjective – it resides within the experience of the individual. Second, it is not just the absence of negative factors, but also includes positive measures. Third, it includes a global measurement rather than only a narrow assessment of one life domain” (p.106).
This global measurement of life satisfaction, also referred to by the term hedonic wellbeing, is typically measured through cognitive scales of life satisfaction or by the presence of positive affect or the absence of negative affect (Steptoe et al., 2015). While some scholars criticise that wellbeing is not more than the subjective perception of one’s life or psychological functioning, others argue that wellbeing reflects the objective conditions and the broader environment (Ng & Fisher, 2013) and consider wellbeing even as a key measure of societal progress that should complement the economic indicators that guide policy decisions (Diener & Seligman, 2018).
There are several explanations for inter-individual variation in wellbeing, ranging from a genetic predisposition for happiness (Bartels, 2015) to psychological theories concerned with personality traits (Lucas, 2018). In addition, sociological research stresses social inequalities in the resources for wellbeing, emphasising not only the role of socio-economic inequalities but also societal characteristics, such as national economic wellbeing and welfare state provision (Jorm & Ryan, 2014). The following paragraphs briefly review the state of research on individual and macro-level determinants of wellbeing.
2.1 Individual-Level Determinants of Wellbeing
Early research suggested the existence of an individual average baseline of wellbeing (“set point”) that is mainly determined by a person’s temperament. While wellbeing is relatively stable over time (Eid & Diener, 2004), individual “set points” can change under certain conditions – most likely if life changes dramatically (Diener et al., 2006). Align with this, longitudinal studies document long-lasting decreases of wellbeing following widowhood, divorce and job loss (Luhmann et al., 2012) or the onset of disability (Lucas, 2007). Besides stressful life events, there are also social structural inequalities in wellbeing. A meta-analysis showed that women report significantly lower wellbeing than men, but gender differences diminish when controlling for inequalities in social networks, health and socioeconomic conditions (Pinquart & Sörensen, 2001), and all of them are central determinants of wellbeing.
Social networks have received considerable attention in wellbeing research (cf. Diener & Ryan, 2002). Supportive relationships are both correlates and antecedents of high wellbeing. Especially living in a partnership has been shown to have an impact of wellbeing in later life (Margelisch et al., 2017). In contrast, widowhood, social isolation and loneliness are linked to an increase in depressive symptoms and reduced wellbeing (Gariépy et al., 2016; Schmitz, 2021). Moreover, socioeconomic conditions affect wellbeing. Financial resources can both directly (through access to monetary means) and indirectly (through being able to rely on a range of social resources) affect wellbeing. On average, wealthier persons are slightly happier than the average and especially persons living in poverty are frequently dissatisfied with their life (Pinquart & Sörensen, 2000). While it has been suggested that income gets less relevant once basic needs are met (Graham, 2011 for an overview), empirical studies show that the link between wealth and wellbeing holds up to very high levels of income (e.g. Killingsworth 2021). The association between education and wellbeing has been studied less extensively. While some studies show a positive association between high education and wellbeing (e.g., Powdthavee et al., 2015; Ferrer-i-Carbonell, 2005), also negative associations have been documented (e.g. Clark & Oswald 1996), which may be due to unrealistic expectations towards personal life circumstances of highly educated individuals (Kristoffersen, 2018).
Apart from psychosocial and socioeconomic factors, physical as well as mental health play a crucial role for wellbeing (Brandmaier et al., 2017; Martinez-Martin et al., 2012; Stanga et al., 2019). While the presence of chronic health conditions and functional limitations leads to a decrease in wellbeing (Gana et al., 2013), high levels of wellbeing also seem to protect from ill-health, probably due to neuroendocrine processes (Siapush et al., 2008; Steptoe et al., 2015). Poor health affects wellbeing not only because of pain and other symptoms that go along with diseases, but also because of reduced functional abilities (cf. the overview in Backe et al., 2018). It has been suggested that the relationship between functional limitations and wellbeing is bidirectional, but there are also longitudinal studies showing that functional limitations proceed declines in wellbeing (Chen et al., 2012).
The mechanisms responsible for the association between functional limitations, one of the most prevalent health conditions in later life (Schmitz & Lazarevič, 2020), and wellbeing have been rarely studied. Backe and colleagues (2018) suggest that sense of mastery, i.e. whether a person feels able to influence important outcomes in his/her life, plays an important role. A pronounced sense of mastery may lead a more effective mobilisation of personal coping resources and support from the social network. Support from the network – in turn – reduces the negative impact of disability on mental health (Jang et al., 2002). Thus, informal support from the personal network buffers against the detrimental effects of functional limitations on wellbeing. If the same holds for professional services that provide help and care to older persons has not been studied yet.
Another recurrent interest of research are wellbeing trajectories with age/over the life course. In line with “set point” theory, wellbeing typically increases or at least does not decrease up to very old age. Significant declines only occur towards the end of life (Mroczek & Spiro, 2005), a life phase when several of the afore mentioned risk factors (e.g., widowhood, physical illness) occur frequently. However, age-related declines in wellbeing are much more pronounced in poorer countries relative to wealthy countries (Deaton, 2008). Thus, one can conclude that growing older is not necessarily a source of unhappiness, but that the societal context plays a role in mitigating age-associated risks for well-being, such as health limitations and care dependency, as we will argue in the following.
2.2 National and Regional-Level Determinants of Wellbeing
Nations across the globe differ with respect to the average level of wellbeing (Helliwell et al., 2020). According to Need Fulfilment Theory (Tay & Diener, 2011), wellbeing depends on a person’s fulfilment of physical and psychological needs, which societal systems or conditions can either hinder or promote. Veenhoven & Erhardt (1995) suggested a “Livability Theory”, arguing that some societies allow for a higher quality of life as they have characteristics that are universally desirable for humans. These needs might be differentiated into basic needs (food and shelter), safety and security needs, social needs (social support and love), respect needs (feeling respected and pride in activities) and autonomy needs (mastery, self-direction and autonomy; Tay & Diener, 2011). Empirical support for this theory comes from studies showing that societies with hunger, conflict, corruption, and war are less happy than the ones with sufficient material resources and stable democratic governments (see the systematic literature review on predictors of national differences in wellbeing by Jorm & Ryan, 2014).
Most studies on cross-country variation in wellbeing focus on the economic wellbeing of nations. Generally, increases in income are associated with increases in wellbeing on the macro-level. However, it is not clear if the benefits of economic growth also apply to high-income countries. Some scholars argue that national income only matters as long as it enables persons to fulfil their basic needs and there might be less gains in wellbeing if these meets are already met, which is similar to the suspected declining marginal utility at the individual level. Another argument is that economic growth in high-income countries is only associated to wellbeing if it allows people to pursue meaningful goals and if it improves the quality of working life (cf. the overview in Jorm & Ryan, 2014).
It is likely that not only the economic situation improves wellbeing, but that – with increasing GDP – also social welfare develops, including social infrastructure and health care services. Research focussing on concrete indicators for social infrastructure or healthcare and its relation to wellbeing is very rare, especially regarding inequalities in wellbeing at the subnational level. A notable exception is a study by Davern and colleagues (2017) that analyses the association between social infrastructure and wellbeing in 31 local government areas within urban metropolitan Melbourne, Australia. The authors applied a broad definition of social infrastructure, including community centres, culture and leisure, childcare services, schools, education, health and social services, as well as sports and recreation. Their analyses show that both accessibility and a mix of social infrastructure were associated with higher wellbeing.
In later life, the individual needs regarding social infrastructure may change. Compared to younger age, services that secure an adequate care when experiencing health declines and limitations in daily living could become more relevant for wellbeing. Prior studies have focussed on the relevance of care infrastructure, as measured by the provision of long-term care services (LTC), for informal caregivers – i.e. persons who provide care to dependent family members or friends. By comparing 18 European countries, Verbakel (2014) found that differences in the wellbeing between caregivers and non-caregivers were less pronounced in countries with more formal LTC services, while Floridi and colleagues (2022) showed substantial gender differences in the wellbeing outcomes of different care arrangements in care regimes across Europe. These results indicate that professional support and the possibility of outsourcing care to professional caregivers may relieve the individual burden and thus lead to a higher wellbeing of informal caregivers, at least in some care contexts. In line with that, Wagner & Brandt (2018) showed that the negative impact of caregiving on wellbeing was less pronounced when state-supported LTC services are more readily available at the regional level.
In sum, these studies show that the availability of LTC services is related to the wellbeing of caregivers. We do not know if these associations are also present in the general older population. However, a substantial share of older individuals suffers from health limitations and could be dependent on professional care services one day. A well-developed care infrastructure may be perceived a “safety net” in case of (expected) care dependency and thus improve the wellbeing in old age. Thus, it is likely that the regional care infrastructure does not only affect the wellbeing of individuals who provide care to their dependent relatives as Wagner & Brandt (2018) have shown, but also for the wellbeing of older adults with health limitations who may be in need of such services.
2.3 Aims of this Study
The purpose of this study is to shed light on the following questions: Is care infrastructure crucial for the wellbeing of older adults? If so, does the relevance of care infrastructure differ depending on an individual’s health status? We hypothesize that care infrastructure not only matters for caregivers, as has been shown in previous studies, but also for the general older population. We assume that the association between care infrastructure and wellbeing is more pronounced for individuals with health limitations, as they may be more in need of such services relative to their counterparts without health limitations.
Our study extends previous research in several ways. First, we focus on the general older population, a group that prior research on regional-level influences on wellbeing did rarely consider. Second, we examine whether there are heterogeneous effects of care infrastructure depending on individual needs by comparing individuals with and without health limitations. Third, by using regional-level information, we are able to provide more nuanced analyses as compared to previous studies that compare countries or welfare state regimes.
3 Data and Methods
3.1 Share
Data were drawn from wave 6 (collected in 2015) of SHARE, a multidisciplinary panel study that started in 2004 with representative samples of the population aged 50 + across Europe and Israel (Börsch-Supan et al., 2013; SHARE Team, 2019). In our analyses, we include data from 35,451 respondents from 96 European regions.
We match the data from SHARE with regional data on the care infrastructure on the regional level using the NUTS (Nomenclature of Territorial Units for Statistics) classification.Footnote 1 The NUTS-2 regions differ considerably in terms of population size, ranging from regions with 80,000 inhabitants to regions with 3,000,000 inhabitants. Depending on the population size, not all countries have every level of division. For instance, Luxembourg simultaneously represents the NUTS-1 and NUTS-2 level (Eurostat, 2022; Destatis, 2022).
The data on NUTS-2 level was retrieved from Eurostat (2021) dating from the year 2015, the year the SHARE-data has been collected. Additional regional data were drawn from the national statistical offices in Switzerland (Federal Statistical Office Switzerland, 2021) and Denmark (Statistics Denmark, 2021).
The sample was restricted to respondents for whom data linkage with regional information was possible.Footnote 2 This restricted the original sample from 65,164 to 50,456. Furthermore, we excluded respondents with missing information on one of the variables of interest on the individual- or regional-level. Finally, data from 35,451 respondents from 96 regions located in twelve countries were included (Northern Europe: Sweden, Denmark; Eastern Europe: Czech Republic, Poland, Estonia, Croatia; Southern Europe: Spain, Italy, Greece; Western Europe: Austria, Luxembourg, and Switzerland).
We performed sensitivity analyses with regard to the selectivity of the sample due to the exclusion of respondents and regions with missing information. Various checks (dummy coding, imputations; results available upon request) did not lead to any substantial differences in the models and our specific and general conclusions.
3.2 Variables
3.2.1 Dependent Variable
Wellbeing was measured by the question: „On a scale from 0 to 10 where 0 means completely dissatisfied and 10 means completely satisfied, how satisfied are you with your life?“ Life satisfaction as an indicator of hedonic wellbeing is widely used in research on quality of life (Steptoe et al., 2015).
3.2.2 Predictors on the Individual-Level
As predictors of wellbeing on the individual-level, we accounted for gender and age, family situation, socio-economic conditions, and health status. Regarding the respondent´s family situation, we included marital status, parenthood and also caregiving to a person living inside or outside the household. To account for the socio-economic situation, we included educational attainment, the subjective evaluation of the household’s financial resources and employment status. Regarding health, we accounted for the number of chronic diseases and limitations in daily activities because of health. Table 1 presents information on the operationalization and coding of the variables.
3.2.3 Predictors on the Regional-Level
Care infrastructure, our main regional-level variable of interest, was measured by the number of institutionalized LTC beds in nursing homes or residential care facilities per 100 inhabitants aged 65 years or older by NUTS-2-region in 2015. As a control variable, we included the economic wealth as measured by the Gross Domestic Product (GDP) in Euro per capita at current market prices in 2015.
3.3 Statistical Analysis
We estimated linear Ordinary-Least-Squares (OLS) models with individuals (level 1) nested in NUTS-2-regions (level 2), which are clustered in countries (level 3). The model is a random-intercept multilevel model (Maas & Hox, 2004) with individual and regional variables. It includes a cross-level interaction between individual´s functional health status (level 1) and the regional availability of care beds (level 2) to test if care infrastructure is more relevant for the wellbeing of older adults with functional impairments.
Prior multilevel analyses of macro-level influences on wellbeing typically operate with country data, but care infrastructure varies a lot by region and the reachability of services is what matters for individual wellbeing (see also Wagner & Brandt, 2018).
4 Results
4.1 Descriptive Results
The mean life satisfaction in the total SHARE-sample amounted to 7.7 on a scale from 0 (completely dissatisfied) to 10 (completely satisfied), meaning that the majority of the older Europeans is quite satisfied with their life in general (Table 2). Two thirds of the sample were women. The mean age was 67.3 years. 55% of the sample were living in a rural area. Regarding family situation, most respondents were married or living in a relationship (70.2%) and had at least one child (90.6%) and around 11% provided care to a person living inside the household. With respect to the socioeconomic conditions, the majority of older Europeans had a middle or low educational attainment (40.2%, resp. 39.0%), whereas the proportion of highly educated individuals was around 21%. Most of the respondents were financially well off, but 26% reported some difficulties and another 13% reported great difficulties in making ends meet. The majority of the sample was still in the workforce (76.3%). Health limitations were quite frequent. On average, older Europeans reported 1.7 chronic conditions and almost half of the respondents (44.7%) considered themselves limited in daily activities due to health problems.
Source: Survey of Health, Ageing and Retirement in Europe (SHARE), wave 6, own calculations. Standard deviation for arithmetic means in brackets.
4.1.1 Regional Availability of Care Beds
There is huge regional variation in the availability of care infrastructure across Europe (Table 3). The number of LTC beds per 100 inhabitants aged 65 years and over was generally higher in the countries of Northern, Central and Western Europe, whereas it was lower in Eastern and especially Southern Europe. However, there are also notable examples (see Czech Republic, Estonia and Spain). Besides cross-country differences, there are also differences within countries when comparing the NUTS-2-regions. One region in Italy, for example, provided almost no LTC beds (0.3 beds per 100 older inhabitants), whereas another Italian region supplied 4.4 LTC beds per 100 older inhabitants. Pronounced regional differences can also be observed in all of the other countries with the exception of Greece, where the availability of LTC beds is generally low. The Europeans regions also differ with respect to the economic resources as measured by GDP per capita. The wealthiest countries are located in Northern, Central and Western Europe with Switzerland ranging on top. In contrast and not surprisingly, the Southern and especially Eastern European countries are among the poorest nations.
4.1.2 Multivariate Results
To determine whether regional care infrastructure is related to the wellbeing of older Europeans and whether the relevance of care infrastructure is dependent on the individual functional health status, we estimated several multilevel regression Models (Table 4). The empty Model 1 shows how much of the variation in life satisfaction can be attributed to the different levels of analysis as measured by the intraclass correlation (ICC). The variance in life satisfaction that could be attributed to the country level (ICC country) was 10%. The ICC at the region-within-country level (ICC country in region) was 11%. The decrease of the ICC in Model 2 and Model 3 shows how much of the unexplained variance at the country and regional level is reduced by the inclusion of variables on the individual- and regional-level.
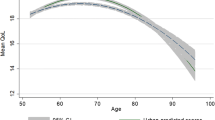
Model 2 shows that factors on both the individual and the regional-level characteristics are related to the wellbeing of older Europeans. Looking at the individual-level predictors, we find that women reported a higher life satisfaction relative to their male counterparts, although the effect size of gender differences is rather small. We also find an increase in life satisfaction with age, whereby the negative effect of age squared indicates that as people get older the effect of age is turning around. Having children was also positively related to life satisfaction, as well as a higher educational attainment and participation in working life compared to those who are retired or permanently sick. In contrast, being single / divorced or widowed, as well as giving care for a person living inside the household were negatively associated with life satisfaction. The same held for problems in making ends meet. Further, we found that health problems are significantly correlated with life satisfaction. With every additional chronic disease, life satisfaction decreased. Furthermore, being limited in activities because of health was negatively associated with life satisfaction.
With regard to the regional-level characteristics, we found that the number of LTC beds was significantly associated to wellbeing in older Europeans. With every additional LTC bed per 100 persons aged 65 years and older, life satisfaction increases by about 0.04 units. In contrast, GDP per capita as an indicator of the regional economic situation was not related to life satisfaction. As a first conclusion, it can be stated that care infrastructure is related to the wellbeing of older Europeans. Model 3 tests if the care infrastructure matters especially for the wellbeing of those who are limited in health and thus may be in greater need of such services. This hypothesis was supported by the significantly positive interaction term between health limitations (measured at the individual level) and LTC beds (measured at the regional level).
5 Discussion
In light of rapid population ageing across European countries, ensuring living conditions that allow for a high level of wellbeing until old age should be a priority for social policy makers. This paper uses data from a representative sample of adults aged 50 + years in order to investigate both individual and regional-level determinants of wellbeing in terms of general life satisfaction in older age. Regarding the determinants of wellbeing on the individual level, our analysis shows that several groups bear a higher risk for a low wellbeing. First, we observed that individuals with low education and few financial resources reported a significantly lower wellbeing as compared to their better-off counterparts. Socioeconomic inequalities in physical health, as measured by functional limitations (von dem Knesebeck et al., 2017), or more generic indicators such as self-rated health (Schmitz & Pförtner, 2017), have been documented in numerous studies. According to our analyses, socioeconomic inequalities are not only present in physical health, but also with respect to life satisfaction, which is considered another important indicator of successful ageing (Rowe & Kahn, 1997).
Second, our analyses indicate that family circumstances are related to wellbeing in later life, as individuals living in a relationship and those who have children are, on average, more satisfied with their life. The importance of social ties and social participation for wellbeing in later life has also been shown in previous studies (Huxhold et al., 2020; Tomini et al., 2016). While social connectedness is an important resource for wellbeing, research has also shown that a better initial wellbeing leads to broader social networks (Schwartz & Litwin, 2019).
Third, we observe inequalities in wellbeing depending on the individual health status. As expected, people with chronic diseases and those who were limited in activities because of health problems reported lower levels of wellbeing. This result is in line with numerous previous studies on the importance of physical health for wellbeing and mental health (Backe et al., 2018; Chen et al., 2012; Schmitz & Brandt, 2019). Thus, living conditions that allow for healthy ageing are urgently needed. Besides of adequate healthcare services, this implies a wide range of policy areas, as it is not primarily the health system that keeps people healthy, but rather the social conditions under which people live and work (Bambra et al., 2005; Marmot, 2005).
Regarding the determinants of wellbeing on the regional-level, GDP as a measure of the regional economic development was not related to wellbeing in the older population. Previous research on national income and wellbeing provided mixed results. While several studies find an association between GDP and life satisfaction, others do not. When an association is present, it is typically more pronounced in low income countries and diminishes in countries with higher levels of national income (cf. the overview in Jorm & Ryan, 2014). We replicated our analysis also including GDP as the only regional-level indicator without accounting for the care infrastructure, but found no association to the wellbeing in Europe’s older population in any of our models.
In contrast, the regional care infrastructure was significantly related to wellbeing in the older population. This holds especially in individuals with health limitations, who might be in need of such infrastructure one day. It may be that the availability of healthcare and formal care services is perceived as a “safety net” in case of care dependency and thus improves wellbeing, but future studies are needed to investigate the causal mechanisms. However, our analysis shows that the regional care infrastructure not only matters for the wellbeing of caregivers as (perceived) alternative to private care and thus leading a greater sense of control (Wagner & Brandt, 2018), but also for the general older population and especially those persons limited in health. It is the available care infrastructure in the neighbourhood that seems to matter for individual wellbeing, more than the general wealth of a country. Communities and local governments should thus ensure the necessary infrastructure for older individuals in need of care and help across different regions, and especially in depopulating rural areas where social networks of less mobile older people are also jeopardized (Huxhold & Fiori, 2019). This infrastructure should not only include LTC beds in nursing homes, which were the focus of our analysis, but also outpatient care, as many older people themselves prefer ambulant care to LTC facilities at least when the need for care can be addressed in ambulant settings (Hajek et al., 2017).
5.1 Limitations
This study is not without limitations. First, our infrastructure analyses are restricted to the number of LTC beds in nursing homes. Cross-country comparative data on ambulant care services, which are an important complement to inpatient care services, are not available at the regional level. Second, there is also no data on the quality, but only on the availability of such care beds. Third, more nuanced regional analyses would be desirable in order to really capture the care infrastructure in the immediate living environment. Finally yet importantly, based on a cross-sectional snapshot, we cannot rule out reverse causality such as selection into different life situations based on wellbeing or assess causal macro-micro-links.
Nevertheless, our study is an important contribution to previous research on determinants of wellbeing in later life. Based on a representative data set of older adults, the analysis not only indicates that several social groups are confronted with lower levels of wellbeing, but also highlight the need for considering regional-level influences in policies that enhance wellbeing in later life. To that end, our study highlights the importance of a well-equipped care infrastructure. The analysis provides several starting points for future studies. Future studies should investigate from a longitudinal perspective whether changes in care infrastructure are related to wellbeing in later life. Furthermore, the underlying mechanisms of the association between care infrastructure and wellbeing deserve further attention.
Notes
NUTS is a geographical system that divides the territory of the European Union into hierarchical levels, which allow for cross-border statistical comparisons at various regional levels (Destatis, 2022). Within the member states of the European Union, the NUTS-classification differentiates between 92 regions at NUTS-1-level (“major socio-economic regions” encompassing between three and seven million inhabitants). NUTS-1-regions are in turn subdivided into NUTS-2 regions (“basic regions for the application of regional policies”).
Israel does not use the NUTS2-classification. Slovenia, Portugal, Belgium and France did not provide data that could be used as an indicator for the availability of care infrastructure. Therefore, respondents from these countries had to be excluded from the sample. For the German SHARE-sample, data on the NUTS-2 region were not available in the Scientific Use File due to data protection issues.
References
Backe, I. F., Patil, G. G., Nes, R. B., & Clench-Aas, J. (2018). The relationship between physical functional limitations and psychological distress: Considering a possible mediating role of pain, social support and sense of mastery. SSM – Population Health, 4, 153–163
Bambra, C., Fox, D., & Scott-Samuel, A. (2005). Towards a politics of health. Health Promotion International, 20(2), 187–193
Bartels, M. (2015). Genetics of wellbeing and its components satisfaction with life, happiness, and quality of life: A review and meta-analysis of heritability studies. Behavior Genetics, 45(2), 137–156
Bonini, A. N. (2008). Cross-national variation in individual life satisfaction: Effects of national wealth, human development, and environmental conditions. Social Indicators Research, 87(2), 223–236
Börsch-Supan, A., Brandt, M., Hunkler, C., Kneip, T., Korbmacher, J., Malter, F. … Zuber, S. (2013). Data resource profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). International Journal Of Epidemiology, 42(4), 992–1001
Brandmaier, A. M., Ram, N., Wagner, G. G., & Gerstorf, D. (2017). Terminal decline in well-being: The role of multi-indicator constellations of physical health and psychosocial correlates. Developmental Psychology, 53(5), 996–1012
Chen, C. M., Mullan, J., Su, Y. Y., Griffiths, D., Kreis, I. A., & Chiu, H. C. (2012). The longitudinal relationship between depressive symptoms and disability for older adults: A population-based study. Journals Of Gerontology. Series A, Biological Sciences And Medical Sciences, 67(10), 1059–1067
Clark, A. E., & Oswald, A. J. (1996). Satisfaction and comparison income. Journal Of Public Economics, 61(3), 359–381
Davern, M., Gunn, L., Whitzman, C., Higgs, C., Giles-Corti, B., Simons, K. … Badland, H. (2017). Using spatial measures to test a conceptual model of social infrastructure that supports health and wellbeing. Cities Health, 1(2), 194–209
Deaton, A. (2008). Income, health and wellbeing around the world: Evidence from the Gallup World Poll. Journal Of Economic Perspectives, 22(2), 53–72
Destatis (2022). NUTS classification: The hierarchical categorisation of EU territories and regions. Online (last access: 26.01.2022): https://www.destatis.de/Europa/EN/Methods/Classifications/OverviewClassification_NUTS.html
Diener, E. (1994). Assessing subjective well-being: Progress and opportunities. Social Indicators Research, 31, 103–157
Diener, E., Lucas, R. E., & Scollon, C. N. (2006). Beyond the hedonic treadmill: Revising the adaptation theory of well-being. American Psychologist, 61(4), 305–314
Diener, E., & Ryan, K. (2002). Subjective well-being: A general overview. South African Journal of Psychology, 39(4), 391–406
Diener, E., & Seligman, M. E. P. (2018). Beyond money: Progress on an economy of well-being. Perspectives on Psychological Science, 13(2), 171–175
Eid, M., & Diener, E. (2004). Global judgments of subjective well-being: Situational variability and long-term stability. Social Indicators Research, 65, 245–277
Eurostat (2019). Population age structure by major age groups, 2008 and 2018. Online (last access: 26.01.2022): https://ec.europa.eu/eurostat/statistics-explained/images/b/bd/Population_age_structure_by_major_age_groups%2C_2008_and_2018_%28%25_of_the_total_population%29.png
Eurostat (2021). Regional statistics by NUTS classification. Online (last access: 26.01.2022): https://ec.europa.eu/eurostat/web/regions/data/database
Federal Statistical Office Switzerland (2021). Sozialmedizinische Institutionen: Alters- und Pflegeheime - Anzahl Plätze. Online (last access: 26.01.2022): https://www.bfs.admin.ch/bfs/de/home.html
Ferrer-i-Carbonell, A. (2005). Income and well-being: An empirical analysis of the comparison income effect. Journal Of Public Economics, 89(5–6), 997–1019
Floridi, G., Quashie, N., Glaser, K., & Brandt, M. (2022). Partner care arrangements and well-being in mid- and later life: The role of gender across care contexts. Journals Of Gerontology. Series B, Psychological Sciences And Social Sciences, 77(2), 435–445
Gana, K., Bailly, N., Saada, Y., Joulain, M., Trouillet, R., Hervé, C., & Alaphilippe, D. (2013). Relationship between life satisfaction and physical health in older adults: A longitudinal test of cross-lagged and simultaneous effects. Health Psychology, 32(8), 896–904
Gariépy, G., Honkaniemi, H., & Quesnel-Vallée, A. (2016). Social support and protection from depression. Systematic review of current findings in western countries. British Journal Of Psychiatry, 209(4), 284–293
Graham, C. (2011). Does more money make you happier? Why so much debate? Applied Research In Quality Of Life, 6(3), 219–239
Hajek, A., Lehnert, T., Wegener, A., Riedel-Heller, S., & König, H. H. (2017). Factors associated with preferences for long-term care settings in old age: Evidence from a population-based survey in Germany. BMC Health Services Research, 17(1), 156
Helliwell, J., Layard, R., Sachs, J., & de Neve, J. E. (Eds.). (2020). World happiness report 2020. New York: Sustainable Development Solutions Network
Huxhold, O., & Fiori, K. L. (2019). Do demographic changes jeopardize social integration among aging adults living in rural regions? Journals Of Gerontology. Series B, Psychological Sciences And Social Sciences, 74(6), 954–963
Huxhold, O., Fiori, K. L., Webster, N. J., & Antonucci, T. C. (2020). The strength of weaker ties: An underexplored resource for maintaining emotional well-being in later life. Journals Of Gerontology. Series B, Psychological Sciences And Social Sciences, 75(7), 1433–1442
Jang, Y., Haley, W. E., Small, B. J., & Mortimer, J. A. (2002). The role of mastery and social resources in the associations between disability and depression in later life. The Gerontologist, 42(6), 807–813
Jorm, A. F., & Ryan, S. M. (2014). Cross-national and historical differences in subjective well-being. International Journal Of Epidemiology, 43(2), 330–340
Killingsworth, M. A. (2021). Experienced well-being rises with income, even above $75,000 per year. Proceedings Of The National Academy Of Sciences Of The United States Of America, 118(4), e2016976118
Kristoffersen, I. (2018). Great expectations: Education and subjective wellbeing. Journal Of Economic Psychology, 66, 64–78
Lucas, R. E. (2007). Long-term disability is associated with lasting changes in subjective well-being: Evidence from two nationally representative longitudinal studies. Journal Of Personality And Social Psychology, 92(4), 717–730
Lucas, R. E. (2018). Exploring the associations between personality and subjective well-being. In E. Diener, S. Oishi, & L. Tay (Eds.), Handbook of well-being. UT: DEF Publishers
Luhmann, M., Hofmann, W., Eid, M., & Lucas, R. E. (2012). Subjective well-being and adaptation to life events: A meta-analysis. Journal of Personality and Social Psychology, 102(3), 592–615
Maas, C. J. M., & Hox, J. J. (2004). Robustness issues in multilevel regression analysis. Statistica Neerlandica, 58, 127–137
Margelisch, K., Schneewind, K. A., Violette, J., & Perrig-Chiello, P. (2017). Marital stability, satisfaction and well-being in old age: Variability and continuity in long-term continuously married older persons. Aging & Mental Health, 21(4), 389–398
Marmot, M. (2005). Social determinants of health inequalities. Lancet, 365(9464), 1099–1104
Martinez-Martin, P., Prieto-Flores, M. E., Forjaz, M. J., Fernandez-Mayoralas, G., Rojo-Perez, F., Rojo, J. M., & Ayala, A. (2012). Components and determinants of quality of life in community-dwelling older adults. European Journal Of Ageing, 9(3), 255–263
Mroczek, D. K., & Spiro, A. (2005). Change in life satisfaction during adulthood: Findings from the veterans affairs normative aging study. Journal Of Personality And Social Psychology, 88(1), 189–202
Ng, E. C. W., & Fisher, A. T. (2013). Understanding well-being in multi-levels: A review. Health, Culture And Society, 5(1), 308–323
Pinquart, M., & Sörensen, S. (2000). Influences of socioeconomic status, social network, and competence on subjective well-being in later life: A meta-analysis. Psychology And Aging, 15(2), 187–224
Pinquart, M., & Sörensen, S. (2001). Gender differences in self-concept and psychological well-being in old age: A meta-analysis. Journals Of Gerontology. Series B, Psychological Sciences And Social Sciences, 56(4), 195–213
Powdthavee, N., Lekfuangfu, W. N., & Wooden, M. (2015). What’s the good of education on our overall quality of life? A simultaneous equation model of education and life satisfaction for Australia. Journal of Behavioral Experimental Economics, 54, 10–21
Rowe, J. W., & Kahn, R. L. (1997). Successful aging. The Gerontologist, 37, 433–440
Schmitz, A. (2021). Gendered experiences of widowhood and depression across Europe: The role of loneliness and financial resources from a longitudinal perspective. Journal Of Affective Disorders, 280, 114–120
Schmitz, A., & Brandt, M. (2019). Gendered patterns of depression and its determinants in older Europeans. Archives Of Gerontology And Geriatrics, 82, 207–216
Schmitz, A., & Lazarevič, P. (2020). The gender health gap in Europe’s ageing societies: Universal findings across countries and age groups? European Journal Of Ageing, 17(4), 509–520
Schmitz, A. L., & Pförtner, T. K. (2017). Health inequalities in old age: The relative contribution of material, behavioral and psychosocial factors in a German sample. Journal Of Public Health, 40(3), e235–343
Schwartz, E., & Litwin, H. (2019). The reciprocal relationship between social connectedness and mental health among older European adults: A share-based analysis. Journals Of Gerontology. Series B, Psychological Sciences And Social Sciences, 74(4), 694–702
SHARE Team. (2019). SHARE release guide 7.0.0. Munich Center for the Economics of Aging
Siapush, M., Spittal, M., & Singh, G. K. (2008). Happiness and life satisfaction prospectively predict self-rated health, physical health, and the presence of limiting, long-term health conditions. American Journal Of Health Promotion,23(1), 18–26
Stanga, V., Turrina, C., Valsecchi, P., Sacchetti, E., & Vita, A. (2019). Well-being in patients with schizophrenia, mood and personality disorders attending psychiatric services in the community. A controlled study. Comprehensive Psychiatry, 91, 1–5
Statistics Denmark (2021). Living conditions: Social conditions - Elderly people - Dwellings for eldery persons. Online (last access: 26.01.2022): https://www.statbank.dk/10048
Steptoe, A., Deaton, A., & Stone, A. A. (2015). Subjective wellbeing, health, and ageing. Lancet, 385(9968), 640–648
Tay, L., & Diener, E. (2011). Needs and subjective well-being around the world. Journal Of Personality And Social Psychology, 101(2), 354–365
Tomini, F., Tomini, S. M., & Groot, W. (2016). Understanding the value of social networks in life satisfaction of elderly people: A comparative study of 16 European countries using share data. BMC Geriatrics, 16(1), 203
Veenhoven, R., & Erhardt, J. (1995). The cross-national pattern of happiness: Test of predictions implied in three theories of happiness. Social Indicators Research, 34(1), 33–68
Verbakel, E. (2014). Informal caregiving and well-being in Europe: What can ease the negative consequences for caregivers? Journal Of European Social Policy, 24(5), 424–441
Von dem Knesebeck, O., Vonneilich, N., & Lüdecke, D. (2017). Income and functional limitations among the aged in Europe: A trend analysis in 16 countries. J Epidemiol Community Health, 71(6), 584–591
Wagner, M., & Brandt, M. (2018). Long-term care provision and the well-being of spousal caregivers: an analysis of 138 European regions. Journals Of Gerontology. Series B, Psychological Sciences And Social Sciences, 73(4), e24–e34
Acknowledgements
We are grateful to Claudius Garten, Artur Król, Ellam Kulati, Michal Myck, Monika Oczkowska and two anonymous reviewers for very helpful comments on our analyses and prior versions of the manuscript.
This paper uses data from SHARE Waves 1, 2, 3, 4, 5, 6, 7 and 8 (DOIs: https://doi.org/10.6103/SHARE.w1.710, https://doi.org/10.6103/SHARE.w2.710, https://doi.org/10.6103/SHARE.w3.710, https://doi.org/10.6103/SHARE.w4.710, https://doi.org/10.6103/SHARE.w5.710, https://doi.org/10.6103/SHARE.w6.710, https://doi.org/10.6103/SHARE.w7.711, https://doi.org/10.6103/SHARE.w8.100, https://doi.org/10.6103/SHARE.w8ca.100), see Börsch-Supan et al., (2013) for methodological details.(1)
The SHARE data collection has been funded by the European Commission, DG RTD through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) and Horizon 2020 (SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628, SERISS: GA N°654221, SSHOC: GA N°823782) and by DG Employment, Social Affairs & Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04–064, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged (see www.share-project.org).
Funding
This work was funded by the German Science Foundation (DFG, project: BR 38.6816-1) within the DFG-NCN Beethoven Classic 3 Programme (joint project with a team at the Centre for Economic Analysis, supported by the National Science Centre, Poland, project number: 2018/31/G/HS4/01511). Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interests.
Ethical Approval
Until July 2011, the Survey of Health, Ageing and Retirement in Europe (SHARE) was reviewed and approved by the Ethics Committee of the University of Mannheim. Since then, the Ethics Council of the Max Planck Society for the Advancement of Sciences (MPG) is responsible for ethical reviews and the approval of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schmitz, A., Brandt, M. Health Limitations, Regional Care Infrastructure and Wellbeing in Later Life: A Multilevel Analysis of 96 European Regions. Soc Indic Res 164, 693–709 (2022). https://doi.org/10.1007/s11205-022-02967-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11205-022-02967-w