Abstract
Many studies estimate individuals’ values for avoiding fatality risks; however, most value-of-statistical-life studies focus on accident-related deaths. Consequently, little is known about preferences for avoiding other fatal risks, such as cancer. Cancer may engender strong feelings of dread, leading to a “cancer premium,” but cancer latency periods may have the opposite effect. Using a national survey, we elicit relative preferences for avoiding fatal cancer and auto-accident risks. We find strong preferences for avoiding cancer risks. With a 5-year latency, they are valued roughly three times greater than immediate accident risks, declining to 50% greater for a 25-year latency.


Similar content being viewed by others
Notes
For evaluating the benefits of reductions in exposure, it is important to recognize a distinction between the concepts of latency period and cessation lag. The latter refers specifically to the time between reductions in exposure and reductions in risk, which for carcinogens may often be shorter than the latency period. For simplicity in this paper, we apply the term “latency” more broadly to refer to any delay between exposure changes and risk changes.
During focus group and cognitive interviews for this survey, several respondents indicated that this was a factor in choosing between avoiding cancer and auto accident risks.
There are also a number of recent studies that have estimated individuals’ WTP for improved cancer treatment or health care programs (Dranitsaris 1999; Gyldmark and Morrison 2001; Shackley and Donaldson 2002; Luchini, Protière and Moatti 2003; Protière et al. 2004); however, they provide somewhat limited insights regarding individuals’ ex ante WTP for preventive measures that reduce their risks of contracting fatal cancers in the future.
In fact, Eq. 1 is an approximation of E(U), which is more accurately specified as: \( E{\left( U \right)} = P_{D} U{\left( {D,Y} \right)} + {\left( {P_{C} - P_{C} P_{D} } \right)}U{\left( {C,Y} \right)} + {\left( {1 - P_{D} - P_{C} + P_{C} P_{D} } \right)}U{\left( {H,Y} \right)} \) (1.1)Since the values of PD and PC addressed in this study are generally equal to or less than 10−4, the interaction term PDPC is roughly four orders of magnitude smaller than these main risks. Dropping this interaction term, which results in Eq. 1, greatly simplifies the conceptual framework without significantly altering the empirical findings.
MVH derive a similar expression which they refer to as the cancer–auto death risk tradeoff rate.
Using a somewhat different framework, Hammitt and Liu (2004) also conclude that under most conditions, individuals’ willingness to pay for reducing latent risks will be lower than for reducing current risks by the same amount.
For the MER calculations, the values of CANCERRISK and CARRISK were set at 3—equal to the same risk as the average individual in their area—rather than at the sample means, which were somewhat smaller.
Details regarding the MVH survey text are presented in Magat, Viscusi, and Huber (1991).
Thirteen observations were excluded from the analysis due to missing values for the explanatory variables.
References
Alberini, Anna, Maureen Cropper, Alan Krupnick, and Nathalie B. Simon. (2004). “Willingness to Pay for Mortality Risk Reductions: Does Latency Matter?” National Center for Environmental Economics, Working Paper # 04-01.
Baron, Jonathan. (1997). “Confusion of Relative and Absolute Risk in Valuation,” Journal of Risk and Uncertainty 14, 301–309.
Cameron, Trudy A. and J.R. DeShazo. (2004). “An Empirical Model of Demand for Future Health States when Valuing Risk-Mitigating Programs,” University of Oregon, Economics Department Working Paper 2004–11.
Cameron, Trudy A. and Michelle D. James. (1987). “Efficient Estimation Methods for Contingent Valuation Surveys,” Review of Economics and Statistics 69(2), 269–276.
Chen, Chao W. and Herman Gibb. (2003). “Procedures for Calculating Cessation Lag,” Regulatory Toxicology and Pharmacology 38(2), 157–165.
Dranitsaris, George. (1999). “Pamidronate for the Prevention of Skeletal-Related Events in Multiple Myeloma. What Does the Public Think It Is Worth?” International Journal of Technology Assessment in Health Care 15(1), 108–122.
Falba, Tracy A. and Susan H. Busch. (2005). “Survival Expectations of the Obese: Is Excess Mortality Reflected in Perceptions?” Obesity Research 13(4), 754–761.
Featherstonhaugh, David, Paul Slovic, Stephen M. Johnson, and James Friedrich. (1997). “Insensitivity to the Value of Human Life: A Study of Psychological Numbing,” Journal of Risk and Uncertainty 14, 283–300.
Gyldmark, Marlene and Gwendolyn C. Morrison. (2001). “Demand for Health Care in Denmark: Results of a National Sample Survey Using Contingent Valuation,” Social Science and Medicine 53(8), 1023–1036.
Hamermesh, Daniel S. (1985). “Expectations, Life Expectancy, and Economic Behavior,” The Quarterly Journal of Economics 100(2), 389–408.
Hammitt, James K. and Jin-Tan Liu. (2004). “Effects of Disease Type and Latency on the Value of Mortality Risk,” Journal of Risk and Uncertainty 28(1), 73–95.
Krupnick, Alan J. and Maureen Cropper. (1992). “The Effect of Information on Health Risk Valuations,” Journal of Risk and Uncertainty 5(1), 29–48.
Krupnick, Alan, Anna Alberini, Maureen Cropper, Nathalie Simon, Bernie O’Brien, Ronald Goeree, and Martin Heintzelman. (2002). “Age, Health and the Willingness to Pay for Mortality Risk Reductions: A Contingent Valuation Survey of Ontario Residents,” Journal of Risk and Uncertainty 24(2), 161–186.
Luchini, Stéphane, Christel Protière, and Jean Paul Moatti. (2003). “Eliciting Several Willingness to Pay in a Single Contingent Valuation Survey: Application to Health Care,” Health Economics 12(1), 51–64.
Magat, Wesley A., W. Kip Viscusi, and Joel Huber. (1991). “Issues in Valuing Health Risks: Applications of Contingent Valuation and Conjoint Measurement to Nerve Diseases and Lymphoma.” In Draft Report to the U.S. EPA: Incorporating Uncertainty in Risk Communication, W. Kip Viscusi and Wesley A. Magat, Principal Investigators.
Magat, Wesley A., W. Kip Viscusi, and Joel Huber. (1996). “A Reference Lottery Metric for Valuing Health,” Management Science 42(8), 1118–1130.
Protière, Christel, Cam Donaldson, Stéphane Luchini, Jean Paul Moatti, and Phil Shackley. (2004). “The Impact of Information on Non-Health Attributes on Willingness to Pay for Multiple Health Care Programmes,” Social Science and Medicine 58(7), 1257–1269.
Ries, L. A. G., D. Melbert, M. Krapcho, A. Mariotto, B. A. Miller, E. J. Feuer, L. Clegg, M. J. Horner, N. Howlader, M. P. Eisner, M. Reichman, and B. K. Edwards (eds). (2007). SEER Cancer Statistics Review, 1975–2004, National Cancer Institute. Bethesda, MD. http://seer.cancer.gov/csr/1975_2004/, based on November 2006 SEER data submission, posted to the SEER Web site.
Shackley, Phil and Cam Donaldson. (2002). “Should We Use Willingness to Pay to Elicit Community Preferences for Health Care? New Evidence from Using a ‘Marginal’ Approach,” Journal of Health Economics 21(6), 971–991.
Siegel, Michele, Elizabeth H. Bradley, and Stanislav V. Kasl. (2003). “Self-Rated Life Expectancy as a Predictor of Mortality: Evidence from the HRS and AHEAD Surveys,” Gerontology 49(4), 265–271.
Smith, V. Kerry, Donald H. Taylor, Jr., and Frank A. Sloan. (2001). “Longevity Expectations and Death: Can People Predict Their Own Demise?” The American Economic Review 91(4), 1125–1134.
Tsuge, Takahiro, Atsuo Kishimoto, and Kenji Takeuchi. (2005). “A Choice Experiment Approach to the Valuation of Mortality,” Journal of Risk and Uncertainty 31(1), 73–95.
Viscusi, W. Kip and Joseph E. Aldy. (2003). “The Value of a Statistical Life: A Critical Review of Market Estimates throughout the World,” Journal of Risk and Uncertainty 27(1), 5–76.
Viscusi, W. Kip, Wesley A. Magat, and Joel Huber. (1991). “Pricing Environmental Health Risks: Survey Assessments of Risk–Risk and Risk–Dollar Tradeoffs for Chronic Bronchitis,” Journal of Environmental Economics and Management 21(1), 32–51.
Acknowledgments
This paper is dedicated to the memory of our dear friend and colleague, Elizabeth McClelland. Financial support for this research was provided by the U.S. Environmental Protection Agency (EPA) under cooperative agreement CR824861-01-0. Thanks are due to John Bennett, Alan Krupnick, Jim Hammitt, Mark Dickie, Maureen Cropper, Clark Nardinelli, Mary Evans, and two anonymous referees for their helpful comments and suggestions and to the Department of Economics at Tilburg University. We also acknowledge research assistance provided by Jui-Chen Yang and Cate Corey. Any opinions, findings, conclusions, or recommendations expressed in this paper are those of the authors and do not necessarily reflect the views of the U.S. EPA.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix A: Proofs of latency and survival probability effects on MER
1.1 The effect of cancer latency on MER
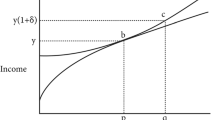
As shown in Eq. 3, the effect on MER of increasing latency (t) depends on how it affects the lifetime utility of the cancer profile. Expanding on Eq. 4, the effect on U(C(t), Y) of increasing latency by one period, from t to t + 1, can be written as
For simplicity, the duration of each time period, as indexed by i, is the same as the duration of cancer morbidity (i.e., between diagnosis and death). The first term in Eq. 11 will be positive as long as the utility of a period in normal health, uh(y), is greater than with cancer, uc(y). Even if the utility of a period (t or t + 1) with cancer is negative, the second term in this expression will also be less in absolute value terms than the first, as long as uh(y) is positive (and yt + 1 is not substantially less than yt). Consequently, an increase in latency should increase U(C(t),Y) and decrease MER. This result is consistent with the intuition that extending cancer latency will reduce aversion to cancer risks.
1.2 The effect of survival probability on MER
In contrast to a change in cancer latency, an increase in survival probability, st, will affect MER through both the cancer and the normal health utility profiles. To examine the effect of increasing st on the MER, we must examine its effect on the ratio U(C,Y)/U(H,Y). To do this we first define the following expressions:
Where
- sij :
-
probability of surviving to period j conditional on surviving to period t.
Differentiating the lifetime utility ratio R with respect to st, we get:
These results imply that as long as the healthy state provides positive utility, and this utility is greater than the utility in the cancer state, then, for a given latency t, increasing the probability of survival to t, will decrease U(C(t),Y) and increase MER. In other words, for a given cancer latency, increasing the probability of survival for that period will increase aversion to cancer risks.
Appendix B: Survey descriptions of cancer morbidity
Depending on the type of cancer, respondents were presented with the following descriptions of symptoms due to cancer illness (the duration of cancer illness, which also varied across respondents, was illustrated using a time line):
-
When liver cancer develops it causes symptoms that include discomfort in the upper abdomen on the right side, pain around the right shoulder blade, and yellowing of the skin (jaundice). Liver cancer also causes bloating, weight loss, fatigue, and general weakness. These symptoms usually become much worse as the illness progresses.
-
When brain cancer develops it causes symptoms that include nausea, vomiting, headaches and seizures. Brain cancers can also lead to mental changes such as problems with memory, speech, and concentration, as well as to severe intellectual problems and confusion. These symptoms usually become much worse as the illness progresses.
-
When stomach cancer develops it causes symptoms that include severe and constant stomach pain (especially after eating), nausea, vomiting, weight loss and general weakness. These symptoms usually become much worse as the illness progresses.
All respondents were presented with the following description of morbidity associated with cancer treatment:
-
Treatment with radiation, chemotherapy, or surgery can often help to slow the progress of the disease, but they can also cause side effects such as pain, nausea, vomiting, diarrhea, and hair loss. They also weaken the immune system, which makes one more vulnerable to other illnesses like pneumonia. In cases of fatal [stomach/liver/brain] cancer, these treatments do not cure the disease. Even with treatment, most patients survive for only a few years after the first symptoms appear.
Appendix C: Sample selection model
Table 4 reports the results of a Heckman sample selection probit model applied to the main model reported in Table 3. The sample for the selection equation is the group of households in the KN panel who were invited to take the survey, and the sample for the main analysis is the subset of respondents who completed the survey, indicated a preference for Location A or B in the choice task, and did not contradict their own choice in a follow up question.Footnote 9 The main probit equation is adapted from model (3) in Table 3—it excludes the demographic variables age, gender, race, education, and household size, which are jointly not significant. These five variables plus the income and urban variables are included in the sample selection equation because they are available for the full KN sample. Although age, race, education, household income, and household size are all statistically significant at a 0.10 level in the selection probit, the Wald test for independence of the two equations can not be rejected at a 0.10 level. This result indicates that the main probit equation does not suffer from sample selection bias.
Rights and permissions
About this article
Cite this article
Van Houtven, G., Sullivan, M.B. & Dockins, C. Cancer premiums and latency effects: A risk tradeoff approach for valuing reductions in fatal cancer risks. J Risk Uncertainty 36, 179–199 (2008). https://doi.org/10.1007/s11166-008-9032-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11166-008-9032-2