Abstract
Although SARS-CoV-2 viral attacks starts by the interaction of spike protein (S Protein) to ACE2 receptor located at the cell surface of respiratory tract and digestive system cells, different endocrine targets, endocrine organs and metabolic conditions are of fundamental relevance for understanding disease progression and special outcomes, in particular those of fatal consequences for the patient. During pandemic, moreover, a specific phenotype of COVID-19 metabolic patient has been described, characterized by being at particular risk of worse outcomes. In the present paper we describe the mechanism of viral interaction with endocrine organs, emphasizing the specific endocrine molecules of particular relevance explaining COVID-19 disease evolution and outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Endocrine targets are of particular relevance for either SARS-CoV-2 viral entrance to the cells as well as regarding modulation of disease expansion in a given host [1]. Lung cells are among others of the respiratory tract, those through which serious disease is initiated. Expression of different molecules in the respiratory tract cells surface is therefore crucial for SARS-CoV-2 viral attack. Besides this respiratory tropism, digestive epithelium is another entrance door for SARS-CoV-2 and part of the initial symptoms are clearly related to the viral invasion of the gut system. Once the disease has achieved this point, systemic involvement may happen and it is at this moment when endocrine organs involvement may take place, either as victims of the viral attack or as suicidal actors amplifying the viral damage, in particular cytokine storm expansion.
In this paper we aim to make an overview of these two pivotal positions of the endocrine organs and system in the COVID-19 sanitary earthquake.
2 COVID-19 and pathogenic mechanisms
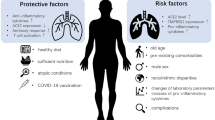
COVID-19 can alter the function of different endocrine glands and metabolic processes and put patients at risk of acute or late-onset endocrine or metabolic dysfunction. In addition, preexisting endocrine disorders or metabolic processes can increase the predisposition to develop COVID-19 or a more severe clinical presentation and outcome (Fig. 1).
SARS-Cov-2 infection has a similar mechanism of action than SARS-Cov-1 and this is by via binding to ACE2 protein, which has an important expression in several endocrine tissues including testis, thyroid, adrenal, pituitary, hypothalamus and adipose tissue [2]. The SARS-Cov-2 virus binds to the ACE2 receptor and uses the cellular serine protease TMPRSS2 for S protein priming. Both ACE2 and TMPRSS2 mRNA have been reported in different endocrine tissues [2]. The possible mechanisms by which the SARS-CoV-2 virus, after entering an endocrine gland and binding the ACE2 receptor, can produce damage include characteristically thrombosis and hypoxia that are typical of highly vascularized organs, such as endocrine organs particularly the pituitary. In addition, other mechanisms that can play a role include immune response against the virus and cytokine storm [2].
2.1 Pathogenic mechanisms involved in COVID-19 infection targeting different endocrine organs
The hypothalamic-pituitary (HP) axis may also be a target of the SARS-CoV-2 [3]. Coronavirus infections can also affect the central nervous system, including the hypothalamus and pituitary. It is still not well known whether the entry is via bloodstream or direct though the cribriform plate. Direct deleterious effect on these organs is suggested by the fact that SARS-CoV-1 viral particles have been detected in autopsy studies involving neuronal degenerated tissue [4]. In this regard, ACE2 and cellular serine protease-TMPRSS2 receptors, that are entries of the SARS-CoV-2 virus, are present in the hypothalamic-pituitary region [5]. SARS-CoV-2 has been reported in the cerebrospinal fluid and also in autopsy studies of the hypothalamus in COVID-19 patients [6, 7]. Another possible mechanism of pituitary injury during COVID-19 is the generation of an immune-mediated hypophysitis, which has also been previously reported in SARS-CoV-1. Moreover, functional hypopituitarism probably related to the increase in circulating cytokines produced by the viral infection has been reported in both SARS-CoV-1 and SARS-CoV-2 infections. It is interesting that abnormalities related to hypopituitarism can persist long-term after SARS-CoV-1 infection, even months after the infection [1]. This could also be the case in SARS-CoV-2, in which follow-up studies of pituitary function are ongoing.
Thyroid dysfunction is a frequent finding in COVID-19 patients that can be mediated by direct or indirect viral effects. In SARS-CoV-1 infection, destruction of the follicular epithelium and the parafollicular cells were reported [8]. ACE2 expression has been found in thyroid follicular cells, and cases of atypical subacute thyroiditis with negative autoantibodies have been found associated with SARS-CoV-2 infection [9,10,11,12]. This type of thyroiditis has been traditionally associated to a viral origin. A recent report showed scintigraphy findings typical of subacute thyroiditis in one third of patients three months after COVID infection, pointing to a much more prevalent phenomenon than previously thought and it is now considered as a sequela associated with COVID-19 [10]. The COVID-19 cytokine storm may eventually precipitate the development of autoimmune thyroid disorders including Graves’ disease, Graves’ ophthalmopathy, and Hashimoto thyroiditis [13]. Nevertheless, the most common thyroid manifestation in COVID-19 patients, mostly in hospitalized patients, is a kind of euthyroid sick syndrome, including decrease in T3 and T4 in some occasions, which run in parallel with an increase in cytokines. These abnormalities could also be very persistent in time as it was also reported in SARS-CoV-1 [14]. Follow-up studies regarding these abnormalities are still awaiting.
A direct cytopathic effect on adrenal cortical cells with generation of diverse lesions, including necrosis of these cells, has been reported in autopsies from SARS-CoV-1 patients [4]. A similar effect could happen in SARS-CoV-2 virus, as ACE2 receptors are present in the adrenal gland. Another possible mechanism that has been described in SARS-CoV-1 is the homology between certain amino acid sequences of the virus and have with ACTH. In this regard, antibodies that are primarily produced against SARS-CoV-1 could also cross-react and destroy ACTH [15]. This mechanism could happen not only in SARS-CoV-1, as has been described, but also in SARS-CoV-2 as SARS-CoV-2 is structurally more than 95% homologous to SARS-CoV-1. However, this mechanism of production of adrenal insufficiency has not been proved yet in SARS-Cov-2. Moreover, another possible mechanism that could provoke adrenal insuficciency in severe forms of COVID-19 is a critical illness related corticosteroid insufficiency (CIRCI). This condition is directly related to the severity of the stress situation generated during a critical illness. In this regard, severe forms of COVID-19 could produce CIRCI and cause inadequate stress corticosteroid mediated response [16].
There is no data on the potential direct effect of COVID-19 on the parathyroid glands or the bones. Nevertheless, hypocalcaemia is a frequent complication and is a predictor of more severe forms of COVID-19 and an unexpected high frequency of silent fractures has been described in these patients [17].
Severity and fatality related to COVID-19 have been observed more in males than in females [18]. Regarding the testis, ACE2 and TMPRSS2 are expressed both in spermatogonia and somatic (Leydig and Sertoli) cells. The testes are probably a high-risk organ for SARS-CoV-2 infection. Destruction of germ cells with reduced sperm cell count [19] and lymphocytic infiltrates in Sertoli and Leydig cells [19, 20] has been reported in the testis from autopsies of SARS-CoV-1 patients, pointing to an immune-mediated damage. SARS-CoV-2 viral particles have also been observed in testis autopsies of these patients [20]. Semen analyses of men with COVID-19 have shown the presence of SARS-CoV-2, but little is yet known about its potential relationship with infertility development [21]. In females ACE2 is also expressed in the ovary, but TMPRSS2 appears to be absent.
2.2 Pathogenic mechanisms, endogenous and exogenous molecules involved in COVID-19 infection in different metabolic and endocrine organs.
2.2.1 Diabetes
It is now accepted that diabetes is an important risk factor for COVID-19 infection and the severity of disease [22,23,24]. A significant part of this risk condition can be attributed solely to hyperglycemia. People with type 1 and type 2 diabetes have an increased risk of hospitalization, need of intensive care and mortality from COVID-19 due to bad glycemic control in a dose-dependent manner [25]. COVID mortality related to any type of diabetes has been associated with aging, mal gender, low socioeconomic conditions, non-white ethnicity, previous cardiovascular disorders, impaired renal function, poor glycemic control, as well as to obesity and underweight. According to this phenotype, a nationwide Swedish study [26], has found that type 2 diabetes people showed increased risk of hospitalization, admission to intensive care and death for COVID-19 in comparison to type 1 diabetes subjects. These later presented few admissions into intensive care and deaths compared to type 2. People with type 2 and type 1 diabetes have a higher risk of hospitalization, intensive care and mortality compared to control population. However, this excess of risk only remained significant in type 2 diabetes after adjustments for comorbidities and pharmacological treatment.
Different hypotheses have been formulated to causally explain such an association; one plausible explanation that the generalized multisystemic inflammation process observed in SARS-CoV-2 infection potentiates a hyperglycemic state and vice-versa, and this phenomenon possibly favors viral replication [27]. Additionally, abnormal acute glycosylation of the SARS-CoV-2 virus has been suggested as a potentiator of viral pathogenesis through modification of viral epitopes that otherwise would have been targeted by the immune system [28]. And also, glycosylated ACE2 on target cells enhances viral tropism and penetration, leading to a higher intensity of COVID‐19 infection and severity in hyperglycemic people [28].
The virus infects peripheral monocytes in a more efficient way under hyperglycemic conditions and upregulates ACE2. After this happens, improved cytokine production by immunocompetent cells take place and can turn to an overexaggerated production of what has been denominate “cytokine storm”. Thus, an adequate insulin treatment is required to control the glucose availability for activated M1 macrophage and the glycolytic flux that feds the viral replication process. In this regard, the viral enhancement of hypoxia-inducible factor-1a (HIF-1a) is a critical regulator of glycolysis in this situation, in a way that a metabolic rewiring is produced at the monocyte levels which is beneficial for the viral replication and shedding.
In addition, it has been proposed that complementing the treatment with an eucaloric ketogenic diet could be a potential metabolic tool for reducing adenosine triphosphate production from aerobic glycolysis in the M1 macrophage phenotype [29]. This combined therapeutic option could theoretically reduce the overproduction of cytokines and, consequently, the accumulation of neutrophils, monocytes, and platelets from the blood. In addition, it could be advantageous for the metabolism of anti-inflammatory M2 macrophages because these cells predominantly express oxidative phosphorylation enzymes and are best fed by the oxidation of fatty acids in the mitochondria.
Finally, it has been demonstrated that human β-cells express viral entry proteins and SARS-CoV-2 indeed infects and replicates in cultured human islets. Infection of endocrine pancreas leads to morphological and functional changes, including reduced numbers of insulin-secretory granules in β-cells and impaired glucose-stimulated insulin secretion [30].
2.2.2 Obesity
Obesity is an important risk factor for contracting COVID-19, as it is also for other infections either of viral or bacterial origin and also for developing more severe forms of the disease [31]. Obesity is usually causally associated with pulmonary dysfunction, thus facilitating viral and bacterial infections. Several mechanisms have been proposed to explain the higher risk of obesity to contracting COVID-19. One feasible option is related to the higher expression of ACE2 in adipocytes which may facilitate prolonged viral shedding [32, 33]. Another important mechanism involved in the increased severity in obese people is associated to the COVID-19 driven cytokine storm, which is characterized by an overproduction of pro-inflammatory cytokines and an increase in inflammatory cells with a decrease in anti-inflammatory cytokines and regulatory cells [34, 35]. The cytokine storm identified in multiple respiratory viral infections including COVID-19 exhibits an overproduction of interferon, tumor necrosis factor α, interleukins, and different chemokines. Considering that subjects with obesity have also a pre-set proinflammatory milieu, it is feasible that COVID-19 could further exacerbate this basal obesity-related inflammation, exposing them to an absolute higher level of circulating inflammatory molecules compared to lean human subjects. This seems a plausible mechanistic explanation of the increased risk of severe complications of COVID-19 in subjects with obesity [36].
Obese individuals may exhibit greater viral shedding suggesting potential for enhanced viral exposure, especially if several family members are overweight. This may be aggravated in overcrowded multigenerational households, which are more common in the socioeconomically deprived communities in which obesity is prevalent [37]. In addition, as it has been described for influenza infection, obesity not only increases the severity but also enhances viral diversity. The altered microenvironment associated with obesity supports the emergence of a more virulent influenza virus population capable of inducing greater disease severity. This could be related to an impaired interferon response in obese subjects, which has been demonstrated in experimental models, both in obese mice and obesity-derived human bronchial epithelial cells [38]. The same could happen in COVID-19 infection in humans.
3 General mechanisms involving endocrine molecules as SARS-CoV-2 viral targets
SARS-CoV-2 viral entry requires at least two host proteins [39]: the angiotensin converting enzyme-2 (ACE2) and the TMPRSS2 protease. Angiotensin-converting enzyme 2 (ACE2) is the only recognized human homologue of ACE, the key regulator of blood pressure, and has approximately 42% identical protein sequences. Since its discovery in 2000 [40, 41], ACE2 has been implicated in heart function, hypertension, and diabetes, with its effects being mediated, in part through its ability to convert angiotensin II to angiotensin. ACE2 biology and crucial contribution to SARS-CoV-2 viral disease development will be extensively covered in another chapter of the present issue. SARS-CoV-2 targets cells through the viral structural spike protein (S protein) that binds to the ACE2 receptor. ACE2 is expressed in human pancreas, and coronavirus could enter beta-cells binding to its receptor, causing acute beta-cell dysfunction, hyperglycemia and transient diabetes [42]. A chapter in this monograph focuses on the study of this mechanism and COVID-19 infection. The transmembrane serine protease type 2 (TMPRSS2) in the host cell activates viral S protein and cleaves ACE2 receptor, further promoting viral binding to host cell membrane [39].
Other endocrine molecules have been described as virus targets, as neuropilin-1 (NRP1) or human dipeptidyl peptidase 4 (DPP-4) (Fig. 2). Table 1 summarizes the endocrine targets effects on COVID-19 of each molecule reported in this chapter.
Possible endocrine and metabolic targets that have been considered for COVID-19 therapy. Different hormones and drugs have been included as possible targets for COVID-19 including melatonin, oxytocin, DPP-4 (human dipeptidyl peptidase 4) inhibitors, GLP-1 (glucagon-like peptide-1) agonists, ACE-2 (angiotensin converting enzyme-2) inhibitors, corticosteroids, estrogens, anti-androgens and statins
3.1 TMPRSS2 protease
Transmembrane serine protease type 2 (TMPRSS2) is a cell surface protein primarily expressed across the respiratory and digestive tracts. SARS-CoV-2 requires TMPRSS2 as well as ACE2 receptor for entry into epithelial host cells. Both ACE2 and TMPRSS2 are present in nasal and bronchial epithelium and pneumocytes, described as SARS-CoV-2 primary target cells in the early infection phase. Furthermore, coronavirus replication in the lungs needs TMPRSS2. Experimental studies showed that TMPRSS2-/- knockout mice infected with coronavirus reduced the severity of the infectious disease with lower viral replication in lungs than wild-type mice [43], indicating the critical role of this pathway in coronavirus disease initiation.
Gastrointestinal symptoms, such as diarrhea and abdominal pain, are observed in COVID-19 patients, often preceding respiratory symptoms. TMPRSS2 is also expressed in intestinal epithelial cells across the gastrointestinal tract, which is the target for many enteric viruses. Some studies have shown that SARS-CoV-2 infects intestinal enteroids cells and TMPRSS2 as well as TMPRSS4 promotes SARS-CoV-2 active infection in these cells [44]. Many endocrine tissues and organs, such as pancreas, thyroid, testis or pituitary, express TMPRSS2 and this could be related to endocrine manifestations of COVID-19 disease [45].
Androgens upregulate the transcriptional activity of the TMPRSS2 gene which could contribute to the male predominance observed in severe infections [46]. TMPRSS2 is also expressed in prostate epithelial cells and, different mutations in its gene, particularly its fusion, represents one of the most frequently biologic defects observed in primary prostate cancer. Confirming the hypothesis that androgenic upregulation may be of importance in disease severity, it has been described that patients with prostate cancer treated with androgen deprivation seem to be partially protected from SARS-CoV-2 infection [47]. In this sense, as TMPRSS2 inhibitors are currently available for treating prostate cancer, this could represent an appealing target for the prevention or treatment of COVID-19 disease [39, 46].
3.2 Neuropilin-1
Neuropilin-1 (NRP1) is a pleiotropic type 1 transmembrane protein cell surface receptor involved in angiogenesis, tumorigenesis, viral entry, axonal guidance and immune function [48] and has been considered as a potential therapeutic target in differents pathologies as cancer or autoimmune diseases. NRP1 has been recently described in experimental studies to be a complimentary entry mediador factor of SARS-CoV-2 into host cells, in addition to ACE2 and TMPRSS2, thus acting as a potentiator of SARS-CoV-2 infectivity [49, 50]. SARS-CoV-2 S protein, which is instrumental for the binding and fusion with host cell membrane, is to get bound to NRP1 after its cleavage [49].
NRP1 is also used as a surface receptor by different proteins, as the vascular endothelial growth factor (VEGF) or semaphorin 3 family [51]. NRP1 is expressed in vascular endothelial cells and may contribute to the organ tropism of COVID-19 disease beside the respiratory tract [49, 50]. Severe and later stages of the disease are related to vascular dysfunction as arterial injury, increased coagulation or sepsis and could be possibly due to NRP1 [52, 53].
NPR1 has been found also to show different degrees of expression in parathyroid, adrenal and testis and a lower expression in thyroid gland compared to the former endocrine organs. Indeed, it is possible that NRP1 could participate in SARS-CoV-2 attack to the pituitary gland as VEGF receptors are also present in the pituitary [54].
Hyperglycemia, ketosis and diabetic ketoacidosis have been observed in non-previously diabetic patients with COVID-19 [55]. An abnormal allele of NRP1 has been described in pancreatic beta cells [56] that could modify the binding of the S protein of SARS-CoV-2 to NRP1 in the islets and could potentially cripple the insulin secretory pathway causing hyperglycemia or even diabetic ketoacidosis. The upregulation of NRP1 in diabetic kidney cells suggests the importance of this protein in SARS-CoV-2 cell entry as a contributing factor and explains the increased risk of this infection in patients with diabetes [50].
As previously mentioned, a direct effect of SARS-CoV-2 virus on adipose tissue is plausible but not well known. In vitro studies have described NRP1 [57], ACE2 protein [58] and TMPRSS2 expression [45] in adipocytes and adipose tissues. Indeed, human adipose tissues present the highest level of NPR1 expression among all human tissues examined and high levels of ACE2 protein and TMPRSS2 expression [59], suggesting a possible direct role of SARS-CoV2 in adipose tissue that might explain the severity of the infection in obese patients.
A recent study has observed a reduction of the entry and infectivity of SARS-CoV-2 in the cell by inhibiting the interaction between virus S1 protein and NRP1 [49] suggesting a new therapeutic target pathway.
3.3 Pineal gland
Melatonin, a well-known anti-inflammatory and anti-oxidative molecule, can protect against acute respiratory distress syndrome caused by viral and other pathogens through their known enhancement of increased inflammatory cytokines and reactive oxygen species generation. There are several mechanisms by which melatonin could have potential benefits in COVID-19 infection. In the first place, it could have antiviral activity. In studies performed through pharmacology-based platforms, melatonin has been found to be a potential drug with anti-CoV viruses’ activity [60]. Moreover, melatonin can inhibit angiotensin II activation and facilitate angiotensin 1–7 action [61]. Melatonin has also very potent anti-inflammatory and antioxidant effects that could reduce and/or counteract proinflammatory cytokines during the cytokine storm observed in severe COVID-19 cases [62]. Notably, there is a well-known decrease of melatonin synthesis and secretion with aging condition, thus favoring a much severe COVID-19 clinical form, as the endogenous antioxidant and antiviral action of melatonin is naturally impaired. Moreover, long standing diabetes can be associated with autonomic neuropathy which impairs profoundly melatonin secretion [63]. Thus, melatonin impairment related to aging and/or diabetes may be an important risk factor contributing to suffer COVID-19 infection and to develop a more severe outcome.
In addition, melatonin regulates the circadian rhythm. During the lockdown periods, disruption of the circadian rhythmicity has been very frequently described, especially in aged individuals. Chrono-disruption is also very common in hospitalized and critically ill patients. In this regard, treatment with melatonin in intensive care units has been found to improve sleep and shorten ICU stay [64]. In a recent retrospective study melatonin exposure after intubation was significantly associated with a positive outcome in COVID-19 and non-COVID-19 patients requiring mechanical ventilation [65].
Furthermore, melatonin can have neuroprotective properties. Cognitive deficits have been reported during COVID-19 infection [66]. Confusion, forgetfulness, fatigue and low mental energy may be some of the sequela of COVID-19 infection. Melatonin could have potential benefits in these patients as it can improve the quality of sleep and cognitive performance, mostly if they have required ICU support [67,68,69].
In summary, melatonin could have potential benefits in relation to its anti-inflammatory and anti-oxidative properties; it could also ameliorate chrono-disruption and have neuroprotective properties that could improve outcomes in COVID-19 patients. Notably, melatonin has a high safety profile, however the specific doses by which melatonin may reduce the severity of COVID-19 are not defined to date and further placebo-controlled randomized clinical trials are needed.
3.4 Oxytocin
There is probably a dysfunction on the oxytocin (OXT) secreting system related to SARS-CoV-2 infection. In this regard, situations that are known to increase the risk of developing COVID-19 and also of developing more severe forms, such as age and menopause, are associated with a decline in OXT [70]. In addition, evidence of an involvement of the hypothalamic-pituitary region characterized by an abnormal hyperintensity signal in mammillary bodies and hypothalamus has been reported in T-2 magnetic resonances of 2 COVID-19 patients [71]. Since the mammillary bodies are the center of OXT production, infection of these areas could probably lead to changes in OXT activity and secretion in COVID-19 patients.
OXT exerts different roles in the immune system. First, OXT can decrease different cytokines including IL-1 and IL-6 in the early phases of infectious diseases [72]. Thus, this could ameliorate COVID-19-related cytokine storm [70]. In addition, OXT could also prevent SARS-CoV-2infection itself, inducing γ-interferon production [73] and reversing lymphocytopenia, as it can promote differentiation of T-lymphocytes in the thymus [74]. Therefore, both mechanisms, if sufficiently activated, can be very beneficial, ameliorating and protecting from COVID-19 infection.
In addition to its effects on the immune system, OXT can enhance endothelial integrity [75] and has cardio-protective properties that could reduce inflammation and promote angiogenesis. These actions are probably very important in COVID-19 patients as OXT could thus reduce thromboembolisms and protect the cardiovascular system, which is a major target of this virus [76]. Of particular interest, it is the possible modulation of nitric oxide production by OXT, which is a key signaling molecule acting as a host response modulator in viral infections.
OXT could also have a role in some of the comorbidities that have been associated with a higher risk of more severe forms of COVID-19. OXT could reduce hyperlipemia and could also prevent weight gain and attenuate hypertension [70]. In addition, OXT has also been involved in the regulation of glucose metabolism and the development of diabetes mellitus [77]. In summary, if OXT could ameliorate these comorbidities, it could improve COVID-19 morbidity and mortality burden. As there are currently no specifically effective treatments for COVID-19, OXT could be a safe and cheap option and a clinical trial is warranted in these patients.
3.5 Corticosteroids
Corticosteroids have been used as an anti-inflammatory and immunosuppressive treatment for different diseases of different nature. Severe COVID-19 disease is characterized by an inflammatory organ injury and a high production of inflammatory endogenous molecules known as cytokine storm, which may progress to an Acute Respiratory Distress Syndrome (ARDS) as well as to other different organs damage, as i.e. vasculitis, kidney damage and myocarditis among other. Under the basis of its previous utilization in a variety of diseases, in which a high degree of endogenous inflammation concurs, corticosteroids were postulate as potentially useful and in fact they have demonstrated to contribute to reduce or attenuate the overactivation of the immune system in COVID-19 patients [78, 79].
Data reported regarding the effectiveness of glucocorticoids for COVID-19 treatment are somehow contradictory [80, 81], probably due to the heterogeneous characteristics of the patients and different classes of glucocorticoids used among the studies. However, the Recovery study, published in July 2020, showed that glucocorticoids, particularly daily 6 mg of dexamethasone treatment up to 10 days, reduced mortality in severe inpatients with COVID-19 receiving invasive mechanical ventilation or oxygen therapy [79]. These promising data led to the modification of the standard of care guidance for COVID-19, as shown in the last recommendations of the World Health Organization (WHO) [82] that introduced systemic glucocorticoids in the treatment of severe and critical COVID-19 patients but not in patients with mild symptoms. Nowadays, many clinical studies are ongoing to check the effectiveness of glucocorticoids treatment in severe COVID-19 patients.
The preferred choice is a compound with a high glucocorticoid effect and no mineralocorticoid action, such as dexamethasone. Dexamethasone has a potent anti-inflammatory action, but also a very well-known hyperglycaemic effect. As mineralocorticoid action could be harmful due to the enhancement of RAAS, it may potentially stimulate the viral spread through ACE2 and also has detrimental effects on hypertension and cardiac and pulmonary function, therefore dexamethasone is a convenient option [83, 84].
The use of high doses of glucocorticoids may cause hyperglycemia in a high percentage of patients by increasing hepatic gluconeogenesis [85] and decreasing peripheral glucose use [86]. Indeed, high doses of glucocorticoids exacerbate hyperglycemia in patients with diabetes, previously diagnosed or undiagnosed, and may precipitate hyperglycemia and steroid-induced diabetes in those patients at risk [87]. Glycemic control in severe COVID-19 in patients treated with glucocorticoids is a challenge, especially in patients with previous diabetes treated with insulin due to the aforementioned effects upon glucose metabolism as well as the impact of high circulating concentrations of cytokines present in severe COVID-19 cases. Diabetes UK has published a clinical guideline for the hyperglycemia management in COVID-19patients treated with dexamethasone [87], recommending glucose monitoring to all patients and an initial insulin dose of 0.3 ui/kg/day, which should be quickly adjusted according to daily glucose levels. In our personal experience, these patients need high insulin doses of about 1–1.3 ui/kg/day on average, and active daily medical supervision to achieve glycemic goals between 7.7–10 mmol/l.
3.6 Antiandrogens and estrogens
Gender is one of the determinants for the evolution of severe forms of SARS-CoV-2 infection [88]. Men are more severely affected by COVID-19 than women, even after adjustments for age, BMI and comorbidities [89, 90]. A possible explanation of the worse prognosis in men could be the androgenic-enhanced expression of TMPRSS2 that facilitate SARS-CoV-2 cell entry. However, young men have better outcomes than older men despite having higher levels of testosterone. Among young men, those with androgenic alopecia present a higher risk of severe COVID-19 forms and worse outcomes [91], presumably due to increased intracellular conversion from testosterone to 5-alpha dihydrotestosterone, thus facilitating SARS-CoV-2 to increase infectivity.
Last but not least, low testosterone levels have also been associated to a poor prognosis and mortality in severe SARS-CoV-2 men cases [92]. A recent report indicates that in a cohort in which the mean age of men was 63 years, circulating testosterone was consistently low in those developing a more severe form of the disease [93]. On the other hand, a polymorphism of the androgen receptor gene has been described predisposing some men to develop more severe COVID-19 forms. These patients showed high circulating testosterone levels indicating receptor resistance [94]. Finally, low testosterone could also be related to hypothalamic hypogonadism, as observed in other metabolic, inflammatory diseases and severe COVID-19 forms. Therefore, the information published so far indicates that different factors interplay in the severity of COVID-19 disease in men, either in association with high or low circulating androgens.
Antiandrogenic treatment, particularly androgen receptor inhibitors as cyproterone, spironolactone, eplerenone or flutamide and 5-alpha-reductase inhibitors, as well as finasteride and dutasteride, seem to protect from COVID-19 in men. However, this question remains very controversial at the moment [95]. Spironolactone and eplerenone have both an antiandrogenic and an antagonistic mineralocorticoid effect, contributing to cardiovascular protection on these patients, as aldosterone represents the bioactive RASS end-product [96]. Dutasteride and finasteride are 5-alpha-reductase inhibitors that block the conversion of testosterone to 5-alpha DHT and mitigate TMPRSS2 expression in prostate cancer [97]. For these effects, they have been proposed as an adjuvant treatment for SARS-CoV-2 infection, particularly in men with androgenic alopecia. Different clinical trials using antiandrogen, aldosterone antagonist or TMPRSS2 inhibitors treatments trials are underway [92]. But, at the moment, results are not yet available. Male patients on previous antiandrogenic therapy for prostate cancer should continue the therapy with a careful evaluation and follow-up.
Concerning women, the increased risk of developing severe forms and complications of COVID-19 infections is mostly related to menopause age [98]. Indeed, estrogens may have a favorable effect against viral infections due to their protective action on endothelial function, the stimulation of the humoral immune response and the modulation of the inflammatory response [99,100,101,102]. Furthermore, the RASS is favorably modulated by estrogens in women [103, 104], while TMPRSS2 expression has a dual correlation with estrogens [105, 106]. In conclusion, estrogens, particularly estradiol, could be eventually protective against COVID-19 and may prevent severe complications. There are ongoing clinical trials using estrogens, progesterone and anti-androgens compounds, but no final data are currently available [92]. However, it is also crucial to remind that COVID-19 is associated to the development of micro and/or macro thrombotic events [107, 108], and this could represent a limitation for estrogens utilization in this disease. Regarding women under menopausal hormone replacement therapy (MHT), it has been recommended to continue treatment, although adding low molecular weight heparin treatment in hospitalized cases [109]. However, the general advice on hormonal contraception treatment is to discontinue the therapy or switch to progesterone-only contraceptives in hospitalized women.
3.7 DPP-4
Human dipeptidyl peptidase 4 (DPP-4)/CD26 has also been identified as a functional receptor of the S protein of MERS-Co-V [110]. MERS-CoV binds to the DPP-4 receptor-binding domain and interacts with T cells and nuclear factors, such as NF-kB, which is critical in the pathogenesis of inflammatory disorders. DPP-4 is a known regulator of the immune system by activating T cells and enhancing the NF-kB pathway [111]. Transgenic mouse models expressing human DPP-4 exposed to MERS-CoV had an impaired monocyte/macrophage phenotype, CD4 + T cells, and lower TNF alpha, IL-6 and Arg1 [112]. The human DPP-4/CD26 may also interact with the S1 domain of the viral spike glycoprotein of SARS-CoV-2, thus allowing an additional way for virus entry into the cell [113].
Therefore, the question is whether DPP-4 inhibitors used currently for type 2 diabetes treatment may not just improve metabolic control in these patients but also contribute to modify COVID-19 attack, either inducing protection or progression of infection. It is tempting to postulate that inhibition of DPP-4 with the current antidiabetic drugs targeting this molecule may impair the virus/DPP-4 interaction, thereby enhancing the cell's self-defense from virus entrance. However, the binding of SARS-CoV-2 compared to MERS-CoV occurs at residues not located near the DPP-4 binding pocket of current gliptin drugs; thus, more studies are required to clarify this question [114].
It is also known that DDP-4 inhibition modulates inflammation and has anti-fibrotic effects. Depending on the potency of these properties, DPP-4 inhibitors may eventually have some protective effects in case of severe COVID-19 infection. The potential decrease of the magnitude COVID-19 cytokines storm under DPP-4 inhibitor treatment action sounds attractive but, so far, no data are available to provide a consistent answer.
3.8 Statins
A systematic review and meta-analysis found that the use of statins was associated with improved clinical outcomes in patients with COVID-19 [115]. The results to date have been controversial, as some studies but not all have found a reduced risk of severe COVID-19 presentation [116,117,118,119]. In those positive studies, although patients had multiple comorbid conditions mainly associated with an increased cardiovascular risk, statins were associated to a reduction of poor outcomes of COVID-19 disease [8, 9]. Mechanistically, there is evidence that cholesterol present in the cell membrane and the viral envelope could enhance SARS-CoV-2 cell entry as it does for other coronaviruses [120,121,122].
The known statins cardioprotective effects may have probably been implicated in the protection of COVID-19 cardiac injury, as recently reported in a series in which cardiac complications, including myocardial injury was only observed in 7% in those treated and 30% in non-statin treated patients [123]. Possible mechanisms implicated a greater plaque instability related to the COVID-19 inflammation milieu, especially when cytokine storm is present [120], thus treatment with statins in these patients could promote additional plaque stability. Moreover, statins have also immune and anti-inflammatory effects that could contribute to mitigate the cytokine storm. As a consequence of these reports, the recommendation for patients on statins, is to keep on the statins treatment in case of getting infected with COVID-19. In patients who haven’t received this therapy previously, results of ongoing clinical trials are needed to make a firm recommendation on the initiation of statins. Nevertheless, their possible actions in cardiac protection, plaque stabilization, anti-inflammatory and immunomodulatory properties make them good candidates for high-risk COVID-19 patients [120].
4 Conclusions
COVID-19 pandemic has dramatically impacted the whole society worldwide and almost broken the health care system of some countries. Since the beginning of the pandemic, a metabolic and endocrine phenotype of patient has emerged and required quick adaptation and protection of these patients trough specific medical treatment of endocrine nature. With accumulating evidence generated in the last 18 months we now know that virtually all endocrine organs and systems may be affected by the SARS-cov-2 virus. As a consequence, the knowledge of the main features of endocrine nature that can be present in everyday patient is crucial for an adequate and successful therapeutic approach. From ACE2, TMPRSS2 to NRP1, many endocrine targets and molecules of endocrine nature are at the entrance of the viral attack and can contribute to its expansion and magnification of systemic lesions through amplification of cytokine storm. In this regard, optimization of glycaemic control and diminution of glycaemic excursions contribute to better outcomes in these patients. In addition, other relevant hormonal products, such as thyroid hormones, melatonin, oxytocin, sex hormones and corticosteroids have been either been impacted by their organ lesion or as potential or demonstrated beneficial therapeutic agent.
Endocrinology of COVID-19 has revealed the existence of a specific phenotype including a high frequency of obese type 2 diabetic aged males, with all the concurrent metabolic components, but also with a high prevalence of hypovitaminosis D and hypocalcemia, hypogonadal function and multiple endocrine organs damage, including the hypothalamus. Thus, endocrinologists and physicians taking care of COVID-19 patients require to evaluate these conditions and implement the most appropriate support to achieve survival and prevent excessive mortality.
References
Puig-Domingo M, Marazuela M, Yildiz BO, Giustina A. COVID-19 and endocrine and metabolic diseases. An updated statement from the European Society of Endocrinology. Endocrine. 2021;72:301–16. https://doi.org/10.1007/s12020-021-02734-w.
Lazartigues E, Qadir MMF, Mauvais-Jarvis F. Endocrine Significance of SARS-CoV-2's Reliance on ACE2. Endocrinology. 2020 Sep 1;161(9):bqaa108. https://doi.org/10.1210/endocr/bqaa108.
Frara S, Allora A, Castellino L, di Filippo L, Loli P, Giustina A. COVID-19 and pituitary. Pituitary. 2021;24:465–81. https://doi.org/10.1007/s11102-021-01148-1.
Leow MK, Kwek DS, Ng AW, Ong KC, Kaw GJ, Lee LS. Hypocortisolism in survivors of severe acute respiratory syndrome (SARS). Clin Endocrinol (Oxf). 2005;63(2):197–202. https://doi.org/10.1111/j.1365-2265.2005.02325.x.
Pal R, Banerjee M. COVID-19 and the endocrine system: exploring the unexplored. J Endocrinol Invest. 2020;43:1027–31. https://doi.org/10.1007/s40618-020-01276-8.
Zhou Z, Zhang M, Wang K, Gao J. SARS-CoV-2: underestimated damage to nervous system. Travel Med Infect Dis. 2020;36: 101642. https://doi.org/10.1016/j.tmaid.2020.101642.
Nampoothiri S, Sauve F, Ternier G, Fernandois D, Coelho C, Imbernon M et al. The hypothalamus as a hub for SARS-Cov-2 brain infection and pathogenesis. bioRxiv. 2020. https://doi.org/10.1101/2020.06.08.139329. https://www.biorxiv.org/content/10.1101/2020.06.08.139329v2.
Yao XH, Li TY, He XC, Ping YF, Liu HW, Yu SC, et al. A pathological report of three COVID-19 cases by minimal invasive autòpsies. Zhonghua Bing Li Xe Za Zhi. 2020;49:411–7. https://doi.org/10.3760/cma.j.cn112151-20200312-00193.
Lania A, Sandri MT, Cellini M, Mirani M, Lavezzi E, Mazziotti G. Thyrotoxicosis in patients with COVID-19: the THYRCOV study. Eur J Endocrinol. 2020;183:381–7. https://doi.org/10.1530/EJE-20-0335.
Muller I, Cannavaro D, Dazzi D, Covelli D, Mantovani G, Muscatello A, et al. SARS-CoV-2-related atypical thyroiditis. Lancet Diabetes Endocrinol. 2020;8:739–41. https://doi.org/10.1016/S2213-8587(20)30266-7.
Rotondi M, Coperchini F, Ricci G, Denegri M, Croce L, Ngnitejeu ST, et al. Detection of SARS-CoV-2 receptor ACE-2 mRNA in thyroid cells: a clue for COVID-19-related subacute thyroiditis. J Endocrinol Invest. 2021;44:1085–90. https://doi.org/10.1007/s40618-020-01436-w.
Brancatella A, Ricci D, Viola N, Sgrò D, Santini F, Latrofa F. Subacute Thyroiditis After Sars-COV-2 Infection. J Clin Endocrinol Metab. 2020;105:dgaa276. https://doi.org/10.1210/clinem/dgaa276.
Jiménez-Blanco S, Pla-Peris B, Marazuela M. COVID-19: a cause of recurrent Graves’ hyperthyroidism? J Endocrinol Invest. 2021;44:387–8. https://doi.org/10.1007/s40618-020-01440-0.
Wang W, Su X, Ding Y, Fan W, Su J, Chen Z, et al. Thyroid function abnormalities in COVID-19 patients. Front Endocrinol (Lausanne). 2021;11:623792. https://doi.org/10.3389/fendo.2020.623792.
Wheatland R. Molecular mimicry of ACTH in SARS - implications for corticosteroid treatment and prophylaxis. Med Hypotheses. 2004;63:855–62. https://doi.org/10.1016/j.mehy.2004.04.009.
Isidori AM, Arnaldi G, Boscaro M, Falorni A, Giordano C, Giordano R, et al. COVID -19 infection and glucocorticoids: update from the Italian Society of Endocrinology Expert Opinion on steroid replacement in adrenal insufficiency. J Endocrinol Invest. 2020;43:1141–7. https://doi.org/10.1007/s40618-020-01266-w.
di Filippo L, Doga M, Frara S, Giustina A. Hypocalcemia in COVID-19: Prevalence, clinical significance and therapeutic implications. Rev Endocr Metab Disord. 2021 Apr 13:1–10. https://doi.org/10.1007/s11154-021-09655-z. Epub ahead of print.
Viveiros A, Rasmuson J, Vu J, Mulvagh SL, Yip CYY, Norris CM, et al. Sex differences in COVID-19: candidate pathways, genetics of ACE2, and sex hormones. Am J Physiol Heart Circ Physiol. 2021;320:H296–304. https://doi.org/10.1152/ajpheart.00755.2020.
Xu J, Qi L, Chi X, Yang J, Wei X, Gong E, et al. Orchitis: a complication of severe acute respiratory syndrome (SARS). Biol Reprod. 2006;74:410–6. https://doi.org/10.1095/biolreprod.105.044776.
Ming Y, Chen S, Huang B, Zhong J-M, Su H, Chen Y-J, et al. Pathological findings in the testes of COVID-19 patients: Clinical Implications. Eur Urol Focus. 2020;6:1124–9. https://doi.org/10.1016/j.euf.2020.05.009.
Li D, Jin M, Bao P, Zhao W, Zhang S. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw Open. 2020;3: e208292. https://doi.org/10.1001/jamanetworkopen.2020.8292.
Burn E, Tebé C, Fernandez-Bertolin S, Aragon M, Recalde M, Roel E, et al. The natural history of symptomatic COVID-19 during the first wave in Catalonia. Nat Commun. 2021;12:777. https://doi.org/10.1038/s41467-021-21100-y.
Holman N, Knighton P, Kar P, O’Keefe J, Curley M, Weaver A, et al. Risk factors for COVID-19-related mortality in people with type 1 and type 2 diabetes in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2020;8:823–33. https://doi.org/10.1016/S2213-8587(20)30271-0.
Andreano A, Murtas R, Tunesi S, Gervasi F, Andreano A, Murtas R, et al. Development of a multivariable model predicting mortality risk from comorbidities in an Italian cohort of 18,286 confirmed COVID-19 cases aged 40 years or older. Epidemiol Prev. 2021;45:100–9. https://doi.org/10.19191/EP21.1-2.P100.044.
Handayani DR, Juliastuti H, Nawangsih EN, Kusmala YY, Rakhmat II, Wibowo A, et al. Prognostic value of fasting hyperglycemia in patients with COVID-19 - Diagnostic test accuracy meta-analysis. Obes Med. 2021;23: 100333. https://doi.org/10.1016/j.obmed.2021.100333.
Rawshani A, Kjölhede EA, Rawshani A, Sattar N, Eeg-Olofsson K, Adiels M, et al. Severe COVID-19 in people with type 1 and type 2 diabetes in Sweden: A nationwide retrospective cohort study. Lancet Reg Health Eur. 2021;4: 100105. https://doi.org/10.1016/j.lanepe.2021.100105.
Icard P, Lincet H, Wu Z, Coquerel A, Forgez P, Alifano M, et al. The key role of Warburg effect in SARS-CoV-2 replication and associated inflammatory response. Biochimie. 2021;180:169–77. https://doi.org/10.1016/j.biochi.2020.11.010.
Mehdipour AR, Hummer G. Dual nature of human ACE2 glycosylation in binding to SARS-CoV-2 spike. Proc Natl Acad Sci U S A. 2021;118: e2100425118. https://doi.org/10.1073/pnas.2100425118.
Codo AC, Davanzo GG, Monteiro LB, de Souza GF, Muraro SP, Virgilio-da-Silva JV, et al. Elevated Glucose Levels Favor SARS-CoV-2 Infection and Monocyte Response through a HIF-1α/Glycolysis-Dependent Axis. Cell Metab. 2020;32:437-46.e5. https://doi.org/10.1016/j.cmet.2020.07.007.
Müller JA, Groß R, Conzelmann C, Krüger J, Merle U, Steinhart J, et al. SARS-CoV-2 infects and replicates in cells of the human endocrine and exocrine pancreas. Nat Metab. 2021;3(2):149–65. https://doi.org/10.1038/s42255-021-00347-1.
Kimura T, Namkoong H. Susceptibility of the obese population to COVID-19. Int J Infect Dis. 2020;101:380–1. https://doi.org/10.1016/j.ijid.2020.10.015.
Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordijn SJ, et al. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol. 2020;251(3):228–48. https://doi.org/10.1002/path.5471.
Moriconi D, Masi S, Rebelos E, Virdis A, Manca ML, De Marco S, et al. Obesity prolongs the hospital stay in patients affected by COVID-19, and may impact on SARS-COV-2 shedding. Obes Res Clin Pract. 2020;14:205–9. https://doi.org/10.1016/j.orcp.2020.05.009.
Sharma JR, Yadav UCS. COVID-19 severity in obese patients: Potential mechanisms and molecular targets for clinical intervention. Obes Res Clin Pract. 2021;15:163–71. https://doi.org/10.1016/j.orcp.2021.01.004.
Pasquarelli-do-Nascimento G, Braz-de-Melo HA, Faria SS, Santos IO, Kobinger GP, Magalhães KG. Hypercoagulopathy and Adipose Tissue Exacerbated Inflammation May Explain Higher Mortality in COVID-19 Patients With Obesity. Front Endocrinol. 2020;11:530. https://doi.org/10.3389/fendo.2020.00530.
Wolf M, Alladina J, Navarrete-Welton A, Shoults B, Brait K, Ziehr D, et al. Obesity and Critical Illness in COVID-19: Respiratory Pathophysiology. Obesity (Silver Spring). 2021;29(5):870–8. https://doi.org/10.1002/oby.23142.
Azzolino D, Cesari M. Obesity and COVID-19. Front Endocrinol. 2020;11: 581356. https://doi.org/10.3389/fendo.2020.581356.
Ritter A, Kreis NN, Louwen F, Yuan J. Obesity and COVID-19: Molecular Mechanisms Linking Both Pandemics. Int J Mol Sci. 2020;21:5793. https://doi.org/10.3390/ijms21165793.
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271-80.e8. https://doi.org/10.1016/j.cell.2020.02.052.
Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, et al. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circ Res. 2000;87:E1–9. https://doi.org/10.1161/01.res.87.5.e1.
Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275:33238–43. https://doi.org/10.1074/jbc.M002615200.
Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47:193–9. https://doi.org/10.1007/s00592-009-0109-4.
Yoshikawa, et al. TMPRSS2 Contributes to Virus Spread and Immunopathology in the Airways of Murine Models after Coronavirus Infection. J Virol. 2019;93(6):e01815-e1818. https://doi.org/10.1128/JVI.01815-18.
Zang R, Gomez Castro MF, McCune BT, Zeng Q, Rothlauf PW, Sonnek NM, et al. TMPRSS2 and TMPRSS4 promote SARS-CoV-2 infection of human small intestinal enterocytes. Sci Immunol. 2020;5:eabc3582. https://doi.org/10.1126/sciimmunol.abc3582.
Baughn LB, Sharma N, Elhaik E, Sekulic A, Bryce AH, Fonseca R. Targeting TMPRSS2 in SARS-CoV-2 Infection. Mayo Clin Proc. 2020;95:1989–99. https://doi.org/10.1016/j.mayocp.2020.06.018.
Stopsack KH, Mucci LA, Antonarakis ES, Nelson PS, Kantoff PW. TMPRSS2 and COVID-19: Serendipity or Opportunity for Intervention? Cancer Discov. 2020;10:779–82. https://doi.org/10.1158/2159-8290.CD-20-0451.
Montoppoli M, Zumerle S, Vettor R, Rugge M, Zorzi M, Catapano CV, et al. Androgen-deprivationt herapies for prostate càncer and risk of infection by SARS-CoV-2: a population-based study (n=4532). Ann Oncol. 2020;31(8):1040–5. https://doi.org/10.1016/j.annonc.2020.04.479.
Soker S, Takashima S, Miao HQ, Neufeld G, Klagsbrun M. Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell. 1998;92:735–45. https://doi.org/10.1016/s0092-8674(00)81402-6.
Daly JL, Simonetti B, Klein K, Chen K-E, Williamson MK, Antón-Plágaro C, et al. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020;370:861–5. https://doi.org/10.1126/science.abd3072.
Cantuti-Castelvetri L, Ojha R, Pedro LD, Djannatian M, Franz J, Kuivanen S, et al. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020;370:865–960. https://doi.org/10.1126/science.abd2985.
Abebe EC, Ayele TM, Muche ZT, Dejenie TQ. Neuropilin 1: a novel entry factor for SARS-CoV-2 infection and a potential therapeutic target. Biologics. 2021;15:143–52. https://doi.org/10.2147/BTT.S307352.
Gu C, Limberg BL, Whitaker GB, Perman B, Leahy DJ, Rosenbaum JS, et al. Characterization of neuropilin-1 structural features that confer binding to semaphoring 3A and vascular endothelial growth factor 165. J Biol Chem. 2002;277:18069–76. https://doi.org/10.1074/jbc.M201681200.
Ackermann M, Verleden SE, Kuehnel M, Haverich A, Welte T, Laenger L, et al. Pulmonary vascular endothelialitis, Thrombosis, and Angiogenesis in Covid-19. N Engl J Med. 2020;383:120–8. https://doi.org/10.1056/NEJMoa2015432.
Onofri C, Theodoropoulou M, Losa M, Uhl E, Lange M, Arzt E, et al. Localization of vascular endothelial growth factor (VEGF) receptors in normal and adenomatous pituitaries: detection of a non-endothelial function of VEGF in pituitary tumours. J Endocrinol. 2006;191:249–61. https://doi.org/10.1677/joe.1.06992.
Grupta A, Madhavan MV, Sehgal K, Nair N, Mahajan S, Seharwat TS, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26:1017–32. https://doi.org/10.1038/s41591-020-0968-3.
Hasan NM, Kendrick MA, Druckenbrod NR, Huelsmeyer MK, Warner TF, MacDonald MJ. Genetic association of the neuropilin-1 gene with type 1 diabetes in children: neuropilin-1 expression in pancreatic islets. Diabetes Res Clin Pract. 2010;87:e29–32.
Giordano A, Cesari P, Capparuccia L, Castellucci M, Cinti S. Sema3A and neuropilin-1 expression and distribution in rat white adipose tissue. J Neurocytol. 2003;32:345–52. https://doi.org/10.1023/B:NEUR.0000011328.61376.bb.
Grupte M, Boustany-Kari CM, Bharadwaj K, Police S, Thatcher S, Gong MC, et al. ACE2 is expressed in mouse adipocytes and regulated by a high-fat diet. Am J Physiol Regul Integr Comp Physiol. 2008;295(3):R781–8. https://doi.org/10.1152/ajpregu.00183.2008.
Uhlen M, Oksvold P, Fagerberg L, Lundberg E, Jonasson K, Forsberg M, et al. Towards a knowledge-based Human Protein Atlas. Nat Biotechnol. 2010;28:1248–50. https://doi.org/10.1038/nbt1210-1248.
Zhou Y, Hou Y, Shen J, Kallianpur A, Zein J, Culver DA, et al. A Network Medicine Approach to Investigation and Population-based validation of Disease Manifestations and Drug Repurposing for COVID-19. PLoS Biol. 2020;18: e3000970. https://doi.org/10.1371/journal.pbio.3000970.
Rahman A, Hasan AU, Kobori H. Melatonin in chronic kidney disease: A promising chronotherapy targeting the intrarenal renin–angiotensin system. Hypertens Res. 2019;42:920–3. https://doi.org/10.1038/s41440-019-0223-9.
Hardeland R. Melatonin and inflammation—Story of a double-edged blade. J Pineal Res. 2018;65: e12525. https://doi.org/10.1111/jpi.12525.
Webb SM, Puig-Domingo M. Role of melatonin in health and disease. Clin Endocrinol. 1995;42:221–34. https://doi.org/10.1111/j.1365-2265.1995.tb01869.x.
Zhang R, Wang X, Ni L, Di X, Ma B, Niu S, et al. COVID-19: Melatonin as a potential adjuvant treatment. Life Sci. 2020;1(250): 117583. https://doi.org/10.1016/j.lfs.2020.117583.
Ramlall V, Zucker J, Tatonetti N. Melatonin is significantly associated with survival of intubated COVID-19 patients. medRxiv [Preprint]. 2020:2020.10.15.20213546
Hampshire A, Trender W, Chamberlain SR, Jolly A, Grant, JE, Patrick F, et al. Cognitive deficits in people who have recovered from COVID-19 relative to controls: An N = 84,285 online study. medRxiv 2020. https://doi.org/10.1101/2020.10.20.g. https://www.medrxiv.org/content/10.1101/2020.10.20.20215863v1.
Zhang Q, Gao F, Zhang S, Sun W, Li Z. Prophylactic use of exogenous melatonin and melatonin receptor agonists to improve sleep and delirium in the intensive care units: A systematic review and meta-analysis of randomized controlled trials. Sleep Breath. 2019;23:1059–70. https://doi.org/10.1007/s11325-019-01831-5.
Wongchitrat P, Shukla M, Sharma R, Govitrapong P, Reiter RJ. Role of Melatonin on Virus-Induced Neuropathogenesis- A Concomitant Therapeutic Strategy to Understand SARS-CoV-2 Infection. Antioxidants. 2021;10:47. https://doi.org/10.3390/antiox10010047.
Cardinali DP, Brown GM, Pandi-Perumal SR. Can Melatonin Be a Potential “Silver Bullet” in Treating COVID-19 Patients? Diseases. 2020;8:44. https://doi.org/10.3390/diseases8040044.
Wang P, Yang H-P, Tian S, Wang L, Wang SC, Zhang F, et al. Oxytocin-secreting system: a major part of the neuroendocrine center regulating immunologic activity. J Neuroimmunol. 2015;289:152–61. https://doi.org/10.1016/j.jneuroim.2015.11.001.
Pascual-Goni E, Fortea J, Martinez-Domeno A, Rabella N, Tecame M, Gomez-Oliva M, et al. COVID-19-associated ophthalmoparesis and hypothalamic involvement. Neurol Neuroimmunol Neuroinflamm. 2020;7:e823. https://doi.org/10.1212/NXI.0000000000000823.
Soumier A, Sirigu A. Oxytocin as a potential defence against COVID-19? Med Hypotheses. 2020;140: 109785. https://doi.org/10.1016/j.mehy.2020.109785.
Johnson HM, Torres BA. Regulation of lymphokine production by arginine vasopressin and oxytocin: modulation of lymphocyte function by neurohypophyseal hormones. J Immunol. 1985;135:773s–5s.
Hansenne I, Rasier G, Péqueux C, Brilot F, Renard Ch, Breton C, et al. Ontogenesis and functional aspects of oxytocin and vasopressin gene expression in the thymus network. J Neuroimmunol. 2005;158:67–75. https://doi.org/10.1016/j.jneuroim.2004.08.007.
Houshmand F, Faghihi M, Imani I, Kheiri S. Effect of different doses of oxytocin on cardiac electrophysiology and arrhythmias induced by ischemia. J Adv Pharm Technol Res. 2017;8:131–7. https://doi.org/10.4103/japtr.JAPTR_178_16.
Chatzis DG, Magounaki KT, Pantazopoulos IN, Johnson EO, Tsioufis KP. COVID-19 pandemic and cardiovascular disease: where do we stand? Minerva Cardioangiol. 2020;68:347–58. https://doi.org/10.23736/S0026-4725.20.05298-6.
Klement J, Ott V, Rapp K, Brede S, Piccinini F, Cobelli C, et al. Oxytocin improves beta-cell responsivity and glucose tolerance in healthy men. Diabetes. 2017;66:264–71. https://doi.org/10.2337/db16-0569.
Saghazadeh A, Rezaei N. Towards treatment planning of COVID-19: Rationale and hypothesis for the use of multiple immunosupressive agents: anti-antibodies, immunoglobulins and corticosteroids. Int Immunopharmacol. 2020;84: 106560. https://doi.org/10.1016/j.intimp.2020.106560.
Horby P, Lim WS, Emberson JR, Mafham M, Bel JL, Linsell L, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. https://doi.org/10.1056/NEJMoa2021436.
Mokra D, Mikolka P, Kosutova P, Mokry J. Corticosteroids in Acute Lung Injury: The Dilemma Continues. Int J Mol Sci. 2019;20(19):4765. https://doi.org/10.3390/ijms20194765.
Tang BM, Craig JC, Eslick GD, Seppelt I, McLean AS. Use of corticosteroids in acute lung injury and acute respiratory distress syndrome: a systematic review and meta-analysis. Crit Care Med. 2009;37(5):1594–603. https://doi.org/10.1097/CCM.0b013e31819fb507.
World Health Organization. Corticosteroids for COVID-19. 2020, Sept 3. WHO/2019-nCoV/Corticosteroids/2020.1. https://www.who.int/publications/i/item/WHO-2019-nCoV-Corticosteroids-2020.1 (consulted in April 2021).
Wyrwoll CS, Mark PJ, Wadell BJ. Developmental programming of renal glucocorticoid sensibility and the renin-angiotensin system. Hypertension. 2007;50(3):579–84. https://doi.org/10.1161/HYPERTENSIONAHA.107.091603.
Kino T, Chrousos GP. Glucocorticoid and mineralocorticoid receptors and associated diseases. Essays Biochem. 2004;40:137–55. https://doi.org/10.1042/bse0400137.
Binder C. The physiology and pharmacology of the glucocorticoids. Acta Med Scand Suppl. 1969;500:9–16. https://doi.org/10.1111/j.0954-6820.1969.tb16717.x.
Alessi J, de Oliveira GB, Schaan BD, Telo GH. Dexamethasone on the era of COVID-19: friend or foe? An essay on the effects of dexamethasone and the potential risks of its inadvertent use in patients with diabetes. Dibaetol Metab Syndr. 2020;12:80. https://doi.org/10.1186/s13098-020-00583-7.
Tayman G, Lumb AN, Kennon B, Cottrell C, Nagi D, Page E, et al. Dexamethasone therapy in COVID-19 patients: implications and guidance for the management of blood glucose in people with and without diabetes. Diabet Med. 2020;38: e14378. https://doi.org/10.1111/dme.14378.
Brandi ML, Giustina A. Sexual dismorphism of Coronavirus 19 morbidity and lethality. Trens Endocrinol Metab. 2020;31:918–27. https://doi.org/10.1016/j.tem.2020.09.003.
Pozzilli P, Lenzi A. Commentary: testosterone, a key hormone in the context of COVID-19 pandemic. Metabolism. 2020;108: 154252. https://doi.org/10.1016/j.metabol.2020.154252.
Salonia A, Corona G, Giwercman A, Maggi M, Minhas S, Nappi RE, et al. SARS-CoV-2, testosterone and frailty in males (PROTEGGIMI): a multidimensional research project. Andrology. 2021;9:19–22. https://doi.org/10.1111/andr.12811.
Wambier CG, Vaño-Galván S, McCoy J, Gomez-Zubiaur A, Herrera S, Hermosa-Gelbard Á, et al. Androgenetic alopecia present in the majority of patients hospitalized with COVID-19: The "Gabrin sign". J Am Acad Dermatol. 2020;83:680–2. https://doi.org/10.1016/j.jaad.2020.05.079.
Wray S, Arrowsmith S. The physiological mechanisms of the sex based difference in outcomes of COVID-19 infection. Front Physiol. 2021;12: 627260. https://doi.org/10.3389/fphys.2021.627260.
Dhindsa S, Zhang N, McPhaul MJ, Wu Z, Ghoshal AK, Erlich EC, et al. Association of circulating sex hormones with inflammation and disease severity in patients with COVID-19. JAMA Netw Open. 2021;4: e2111398. https://doi.org/10.1001/jamanetworkopen.2021.11398.
Baldassami M, Picchiotti N, Fava F, Fallerini C, Benetti E, Daga S, et al. Shorter androgen receptor polyQ alleles protect against life-theratening COVID-19 disease in European males. EBioMedicine. 2021;65: 103246. https://doi.org/10.1016/j.ebiom.2021.103246.
Trüeb RM, Régnier A, Caballero-Uribe N, Reis Gavazzoni Dias MF, Dutra Rezende H. Extraordinary claims without extraordinary evidence: controversy on anti-androgen therapy for COVID-19. J Eur Acad Dermatol Venereol. 2021;35:e494–5. https://doi.org/10.1111/jdv.17249.
Cadegiani FA. Can spironolactone be used to prevent COVID-19-induced acute respiratory distress syndrome in patients with hypertension? Am J Physiol Endocrinol Metab. 2020;318(5):E587–8. https://doi.org/10.1152/ajpendo.00136.2020.
Tindall DJ, Rittmaster RS. The rationale for inhibiting 5alpha-reductase isoenzymes in the prevention and treatment of prostate cancer. J Urol. 2008;179:1235–42. https://doi.org/10.1016/j.juro.2007.11.033.
Ding T, Zheng J, Wang T, Ciu P, Chen Z, Jiang J, et al. Potential influene of menstrual status and sex hormones on female severe acute respiratory syndrome coronavirus 2 infection: a cross-sectional multicenter study in Wuhan. China Clin Infect Dis. 2021;72:e240–8. https://doi.org/10.1093/cid/ciaa1022.
Glinsky GV. Tripartite combination of candidate pandemic mitigation agents: vitamin D, quercetin, and estradiol manifest properties of medicinal agents for targeted mitigation of the COVID-19 pandemic defined by genomics-guided tracing of SARS-CoV-2 targets in human cells. Biomedicines. 2020;8(5):E129. https://doi.org/10.3390/biomedicines8050129.
Breithaupt-Faloppa AC, de Jesus CC, Máximo Prado C, Sessa Srilhano R, Portes Ureshino R, Pinho Moreira LF. 17-beta-estradiol, a potential ally to alleviate SARS-CoV-2 infection. Clinics. 2020;75: e1980. https://doi.org/10.6061/clinics/2020/e1980.
Grandi G, Facchinetti F, Bitzer J. The gendered impact of the coronavirus disease (COVID-19): do estrogens play a role? Eur J Contracept Reprod Health Care. 2020;25:233–4. https://doi.org/10.1080/13625187.2020.1766017.
Suba Z. Prevention and therapy of COVID-19 via exogenous estrogen treatment for both male and female patients. J Pharm Pharm Sci. 2020;23:75–85. https://doi.org/10.18433/jpps31069.
Komukai K, Mochizuki S, Yoshimura M. Gender and the renin-angiotensinaldosterone system. Fundam Clin Pharmacol. 2010;24(6):687–98. https://doi.org/10.1111/j.1472-8206.2010.00854.x.
O’Donnell E, Floras JS, Harvey PJ. Estrogen status and the renin angiotensin aldosterone system. Am J Physiol Regul Integr Comp Physiol. 2014;307(5):R498-500. https://doi.org/10.1152/ajpregu.00182.2014.
Kim H, Datta A, Talwar S, Saleem SN, Mondal D, Abdel-Mageed AB. Estradiol-ERβ2 signaling axis confers growth and migration of CRPC cells through TMPRSS2-ETV5 gene fusion. Oncotarget. 2016;8(38):62820–33. https://doi.org/10.18632/oncotarget.11355.
Bonkhoff H, Berges R. The evolving role of oestrogens and their receptors in the development and progression of prostate cancer. Eur Urol. 2009;55(3):533–42. https://doi.org/10.1016/j.eururo.2008.10.035.
Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135(23):2033–40. https://doi.org/10.1182/blood.2020006000.
The Lancet Haematology. COVID-19 coagulopathy: an evolving story. Lancet Haematol. 2020;7:e425. https://doi.org/10.1016/S2352-3026(20)30151-4.
Ramírez I, De la Viuda E, Baquedano L, Coronado P, Llaneza P, Mendoza N, et al. Managing thromboembolic risk with menopausal hormone therapy and hormonal contraception in the COVID-19 pandemic: Recommendations from the Spanish Menopause Society, Sociedad Española de Ginecología y Obstetricia and Sociedad Española de Trombosis y Hemostasia. Maturitas. 2020;137:57–62. https://doi.org/10.1016/j.maturitas.2020.04.019.
Raj VS, Mou H, Smits SL, Dekkers DHW, Müller MA, Dijkman R, et al. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature. 2013;495:251–4. https://doi.org/10.1038/nature12005.
Julián MT, Alonso N, Colobran R, Sánchez A, Miñarro A, Pujol-Autonell I, et al. CD26/DPPIV inhibition alters the expression of immune response-related genes in the thymi of NOD mice. Mol Cell Endocrinol. 2016;426:101–12. https://doi.org/10.1016/j.mce.2016.02.014.
Li K, Wohlford-Lenane CL, Channappanavar R, Park JE, Earnest JT, Bair TB, et al. Mouse-adapted MERS coronavirus causes lethal lung disease in human DPP4 knocking mice. Proc Natl Acad Sci USA. 2017;114:E3119–28. https://doi.org/10.1073/pnas.1619109114.
Raha AA, Chakraborty S, Henderson J, Mukaetova-Ladinska E, Zaman S, Trowsdale J, et al. Investigation of CD26, a potential SARS-CoV-2 receptor, as a biomarker of age and pathology. Biosci Rep. 2020;40:BSR20203092. https://doi.org/10.1042/BSR20203092.
Roussel R, Darmon P, Pichelin M, Goronflot T, Abouleka Y, Ait Bachir L, et al. Use of dipeptidyl peptidase-4 inhibitors and prognosis of COVID-19 in hospitalized patients with type 2 diabetes: A propensity score analysis from the CORONADO study. Diabetes Obes Metab. 2021;23:1162–72. https://doi.org/10.1111/dom.14324.
Pal R, Banerjee M, Yadav U, Bhattacharjee S. Statin use and clinical outcomes in patients with COVID-19: An updated systematic review and meta-analysis. Postgrad Med J. 2021 Feb 4:postgradmedj-2020-139172. https://doi.org/10.1136/postgradmedj-2020-139172.
Gupta A, Madhavan MV, Poterucha TJ, DeFilippis EM, Hennessey JA, Redfors B, et al. Association Between Antecedent Statin Use and Decreased Mortality in Hospitalized Patients with COVID-19. Res Sq. 2020: rs.3.rs-56210. https://doi.org/10.21203/rs.3.rs-56210/v1.
Zhang X-J, Qin J-J, Cheng X, Shen L, Zhao Y-C, Yuan Y, et al. In-Hospital use of statins is associated with a reduced risk of mortality among individuals with COVID-19. Cell Metab. 2020;32:176-87.e4. https://doi.org/10.1016/j.cmet.2020.06.015.
Daniels LB, Sitapati AM, Zhang J, Zou J, Bui QM, Ren J, et al. Relation of Statin Use Prior to Admission to Severity and Recovery Among COVID-19 Inpatients. Am J Cardiol. 2020;136:149–55. https://doi.org/10.1016/j.amjcard.2020.09.012.
Hariyanto TI, Kurniawan A. Statin therapy did not improve the in-hospital outcome of coronavirus disease 2019 (COVID-19) infection. Diabetes Metab Syndr. 2020;14:1613–5. https://doi.org/10.1016/j.dsx.2020.08.023.
Radenkovic D, Chawla S, Pirro M, Sahebkar A, Banach M. Cholesterol in Relation to COVID-19: Should We Care about It? J Clin Med. 2020;9:1909. https://doi.org/10.3390/jcm9061909.
Vandermeer ML, Thomas AR, Kamimoto L, et al. Association between use of statins and mortality among patients hospitalized with laboratory-confirmed influenza virus infections: a multistate study. J Infect Dis. 2012;205:13–9. https://doi.org/10.1093/infdis/jir695.
Frost FJ, Petersen H, Tollestrup K, et al. Influenza and COPD mortality protection as pleiotropic, dose-dependent effects of statins. Chest. 2007;131:1006–12. https://doi.org/10.1378/chest.06-1997.
Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan. China JAMA Cardiol. 2020;5:802–10. https://doi.org/10.1001/jamacardio.2020.0950.
Author information
Authors and Affiliations
Contributions
all authors reviewed current scientific publication regarding COVID-19 and endocrine systems, wrote differents parts of the paper and reviewed the whole manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing financial interests exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Soldevila, B., Puig-Domingo, M. & Marazuela, M. Basic mechanisms of SARS-CoV-2 infection. What endocrine systems could be implicated?. Rev Endocr Metab Disord 23, 137–150 (2022). https://doi.org/10.1007/s11154-021-09678-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11154-021-09678-6