Abstract
Background
Since the end of the industrial revolution, advances in public health and clinical medicine have contributed to dramatic decreases in infant and childhood mortality, improvements in health-related quality of life (HRQoL), increases in overall life expectancy (LE), and rectangularization of survival curves.
Objectives
In this article, we focus on disability that has occurred with the overall lengthening of LE in many populations and the implications this has for decreased HRQoL.
Methods
We utilize the concept of rectangularization of population survival to depict the rising prevalence of disability associated with increased LE, especially among racial and ethnic minorities and people of low socioeconomic status (SES) and relate this to HRQoL.
Results
Disability-free life expectancy (DFLE) and healthy life expectancy (HLE) are defined in terms of HRQoL. Specific attention is focused on disability experienced by disparate populations around the globe. By focusing on disparities in DFLE, and the need to expand LE to include HLE as a central component of HRQoL, this work provides an important counterpoint to the attention that has been paid to LE disparities according to race, gender, ethnicity, education, and SES.
Discussion
By calling attention to those factors that appear to be the most important drivers of the differences in quality and length of DFLE between different groups (i.e., the components of the social gradient, exposure to chronic stress, systemic inflammation, and the psychological and biological mechanisms associated with the gut–brain axis) and, by logical extension, HRQoL, we hope to promote research in this arena with the ultimate goal of improving DFLE, HLE, and overall HRQoL, especially in disparate populations around the globe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain English summary
Over the last 150 years, we have seen huge decreases in overall death rates, especially in infancy and early childhood and overall life expectancy (LE) at birth has nearly doubled. While many people will live much longer lives than their great grandparents, not all of the extra years of life are free of physical pain and other disability that determine physical, mental, emotional, and social functioning that are the essential components of health-related quality of life (HRQoL). In this article, we focus on the rising prevalence of disability that has occurred with the overall lengthening of LE. Racial and ethnic minorities and people of low socioeconomic status (SES) tend to have both shorter lifespans and more disability across the lifespan, with important implications for HRQoL. With our focus on HRQoL, this work provides important balance to the attention that has been paid to disparities in LE according to race, gender, ethnicity, education, and socioeconomic status.
Public health advances have led to reduced mortality and longer life expectancies
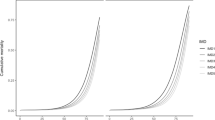
Public health protections undertaken in the latter half of the nineteenth century into the early twentieth century led to dramatic reductions in overall mortality, infant mortality rates (IMR), and extension of life expectancy (LE) [1,2,3,4,5]. This has resulted in the “rectangularization” of population survival curves in which infant and childhood mortality rates fall and more individuals live to their genetic potential for longevity [6]. The “rectangularization” of the curve literally refers to the shift of overall population survival curves upwards and to the right. This transformation is thought to be a result of either delay in mortality (increase in LE), compression of mortality (concentration of deaths around the mean or modal age of death), or a combination of the two; though postponement of mortality is the primary reason [7, 8]. Both the delay and compression of mortality are attributable to (1) reduced IMR; (2) decreases in accidental deaths, particularly during adolescence; and (3) decreases in mortality later in life due to improved treatment of chronic diseases of adulthood [7].
During public health’s century-long evolution, other disciplines have been added to create a myriad of inter-disciplinary perspectives ranging from nutrition and diet [9,10,11], to psychosocial stress [9, 12, 13], environmental health [12, 14], geospatial effects [15, 16], gerontology and geriatrics [17], and psychoneuroimmunology [10]. Over the past three decades, these inter-disciplinary perspectives have aided researchers and practitioners in understanding and addressing health inequities between groups of different racial, ethnic, biological sex, socioeconomic, and geographical backgrounds [12, 18, 19] (Fig. 1).
Historically, the fight for fair policies aimed at providing equal access to the broad determinants of health and improvements in healthcare have allowed developed countries to make great strides in decreasing IMRs and extending overall LE [20]. This transition from high mortality and low LE has been global in scope; e.g., since 1900, the worldwide average LE has more than doubled [5]. Over this transition, additional scrutiny has been brought to bear on the effect of these factors beyond simply extending life, for example, to consider effects on disability-free life expectancy (DFLE), quality-adjusted life expectancy (QALE), and on their important correlate, health-related quality of life (HRQoL). While DFLE is calculated simply by subtracting the number of years an individual is affected by disability or poor health from total LE, QALE affords us the opportunity to measure health decline as it relates to LE on a continuum based on the relative amount of disability an individual experiences [2, 21]. Even more comprehensive is HRQoL which encompasses physical, mental, emotional, and social functioning and, therefore, has the potential to provide important insights into how various drivers of health decline affect individuals’ abilities to successfully complete basic daily acts of living [22]. As such, it has achieved a prominent place in the Healthy People 2020 objectives, including as they relate to immigrant health [23], and in the Healthy People 2030 objectives, with their heightened focus on social determinants of health [24, 25]. Also, it has been used to describe the effects of the global obesity pandemic, which has caused disability at progressively younger ages all over the world [26]. While concern about the global upsurge in childhood obesity is of legitimate concern, the current Covid 19 pandemic underscores that older adults often have comorbidities related to unhealthy aging and poor diet that place them at elevated risk of increased disability and death [27].
While HRQoL is a helpful conceptual tool to describe physical, mental, emotional, and social health status, measures such as the QALY (quality-adjusted life years) can quantify one’s health status in a single score by assigning a numeric value based on current health status and years lived in that physical state [28]. DFLE, QALE, HRQoL, and QALY are related concepts that can help describe and quantify disability in relation to overall LE and quality of life as it pertains to health decline over time. Each term provides a different level of detail and focus and therefore is suited to a particular conceptualization or way of measuring individual and population health.
Over the wide geographic and temporal arc of the “golden age of public health,” disparities by race, socioeconomic status (SES), and geographical region have persisted and, in many cases, even widened both in the US [15, 29,30,31] and globally [4, 32]. Although populations are now living longer, this does not necessarily mean that individuals are enjoying good HRQoL and little disability throughout their longer lifespans. Disability and degradation in HRQoL also are on the rise, and are impacting racial and SES minorities disproportionally. The decades-long trend toward increased concentration of wealth and educational opportunity experienced globally [27, 33,34,35] portends even greater disparities in the future.
HRQoL and social determinants of health as they relate to disability
Healthcare spending is not the primary determinant of better health. For example, despite spending the most money on healthcare of all countries in the world (17·9% of its GDP in 2016) [36], the US ranks only 37th in terms of IMR, LE, and other important indicators of population health [37]. Various analyses have highlighted the relatively large healthcare costs associated with end-of-life care and life-sustaining measures, partly as a result of the growing proportion of the aging population [38] and the disability and poor HRQoL seen late in life in many places around the world [21, 39,40,41].
Though poorly documented, to some extent end-of-life costs are exacerbated by the relative unfitness of the population [9, 13]. More importantly, the literature reflects that relatively little attention is being paid to lifelong disability resulting from poor lifestyle choices in combination with the aging of the population [42], with dire implications for HRQoL [21, 43]. Often, individuals experience disability without, or in advance of, an actual disease diagnosis [13, 44]. Clearly, relying only on overall LE and IMR is insufficient for quantifying the general health of a population, as these statistics tell us virtually nothing about the health of a population as it ages into adolescence, and then into early, middle, and late adulthood. It is appropriate to consider HRQoL, which is a more all-encompassing/holistic concept that is related to other metrics such as DFLE, disabled life expectancy (DLE), and healthy life expectancy (HLE) [10, 45].
Depicting disability using the traditional survival curve allows us to consider HRQoL, or one of its correlates such as DFLE or QALE, by visualizing the effect of disability resulting from chronic conditions that cause disability and subtract from DFLE in advance of actual mortality [8]. A similar approach was taken over 30 years ago by the World Health Organization’s Scientific Group on the Epidemiology of Aging [46]; however, given the shifts in psychosocial, dietary, and societal influences on health in the last 30 years and an obesity epidemic that has afflicted the population at much earlier ages [26], it seems reasonable to revisit this issue now.
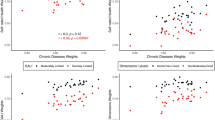
By the mid-twentieth century, the populations of virtually all economically advanced countries had experienced an epidemiologic shift to chronic, degenerative non-infectious diseases, with disability shifting toward middle adulthood [47]. More people are now living with and dying from conditions such as coronary heart disease (CHD), cancer, and diabetes. We also have begun to understand many of the underlying, non-hereditary causes of these chronic diseases. Two of the most important of these are inflammation [48] and stress [12, 14, 30], which affect HRQoL by compromising physical, mental, emotional, and social functioning. While research efforts have focused on these related factors, there has been an explosion of interest in the social determinants of health. Likewise, there has been a growing research focus on the terms ‘health disparities’ and ‘health inequities,’ both of which became much more prevalent in the literature between 2000 and 2004 [15]. The variability in the scale of LE surges over the last 50 years reflects widening gaps in health disparities in different racial and ethnic groups, with colorectal cancer being a good example because of both its relative virulence and its effects on quality of life [15, 31].
It can be misleading to examine LE without considering that a proportion of total years may be lived with poor HRQoL [45], which now afflicts people at progressively younger ages [10, 49]. Indeed, in U.S. women disability now accounts for more than DFLE through middle life [10]. By investigating how to match the increases in LE for the more disadvantaged groups, we hope to close the gap in DFLE with corollary improvements in HRQoL. While there is some biological vulnerability at the root of these inequalities, the scientific focus has shifted to the social inequalities which, theoretically at least, are largely avoidable or reversible through social and environmental change and contribute to preventable chronic illnesses [34, 50].
As noted, when populations transition from high fertility and high mortality to lower fertility and mortality, their survival curves become more rectangular. As more individuals are living to the modal age of death in the population, this produces a sharp drop in survival beginning at around 78 years of age [7, 8]. While this is a dependable feature of the transition, scant attention is paid to quality (as opposed to quantity) of life and the related matter of disability. If DFLE is seen as one of the primary measures of population health and an important correlate of HRQoL [2], we must determine the most promising courses of action so as to decrease disability throughout life and thereby produce a rightward shift in the disability-free LE curve, with attendant improvements in HRQoL.
Previous studies have verified that a rightward shift in the DFLE results from decreases in newly incident disability and increases in instances of individuals recovering from disability (i.e., overall reduced prevalence) [51]. Currently, most of the leading causes of morbidity and mortality are chronic diseases [52,53,54,55]. This is true even during the Covid 19 pandemic whose effect is seen most acutely in people with existing comorbidities and disability [27]. Given that chronic, low-grade, systemic inflammation has been consistently shown to be highly predictive of chronic disease [56] and disability [42], it can be hypothesized that by treating chronic inflammation we may initiate that rightward shift in the DFLE curve and improvements in HRQoL.
Because of variations in preclinical symptomology and reporting, disability does not necessarily track with morbidity [9, 10]. That this can become very complicated and nuanced is indicated by the fact that risk of developing most chronic diseases is increased by stress and inflammation [13]. However, disability from stress and inflammation, which represent an important component of HRQoL [39], may precede an actual diagnosis of depression or type II diabetes mellitus by decades [47]. Evidence has accumulated linking inflammation and stress to socioeconomic/social class such that there is an inverse gradient (i.e., as SES goes down, chronic systemic inflammation and psychosocial stress go up) [15]. It is well known that more well-educated, affluent individuals tend to live longer, disability-free lives with better HRQoL [13, 15, 30].
Social determinants of health and disease and disparities in disability and HRQoL
Social determinants of health and the disparities that exist between demographically distinct groups are driven by factors related to race, ethnicity, economic status, education, and geographic location (including neighborhood-level factors) [14, 15]. These factors are potential confounders and effect modifiers in epidemiologic studies of disease causation [57]. Their effects may be additive or multiplicative and either positive (synergistic) or negative (antagonistic). Understanding how these factors interact to cause disability and death and detract from HRQoL depends on the careful design of studies that incorporate measurements that are valid and sufficiently accurate and precise. The attempt, of course, is to answer fundamental questions about what drives HRQoL throughout life, who is at greatest risk for developing disability during life, critical periods for developing disability, and what steps can be taken in the future to increase HRQoL and DFLE in parallel with the increase we have seen in LE over the past century. Increasing HRQoL will be associated with decreased healthcare spending, improved productivity, and narrowing the gap in health inequities across demographic groups [2, 13, 40, 58]. At the same time, we need to remain cognizant that life expectancies are falling in many places, including the United States, where there have been 3 consecutive years of decreases driven mainly by disparities in marginalized groups that experience record-high deaths from drug overdose and suicide [59].
The concept of the social gradient, introduced by Michael Marmot in the original Whitehall Study [11], asserts that individuals occupying higher positions in a social hierarchy are less likely to develop CHD [16, 60]. Since its inception, the social gradient has been linked to CHD [11] and variety of other chronic conditions such as cancer [61], cognitive decline [15, 60], dementia [42, 62], obesity [11], and type II diabetes mellitus [63]. What is it about lower hierarchal position that puts an individual at an increased risk of such conditions? Mediating biological variables such as blood pressure, plasma total cholesterol, body mass index, plasma glucose, and smoking account for less than one-third of the social gradient [18]. Furthermore, there appear to be other factors, aside from biological markers, which increase risk [16]. Different racial, ethnic, socioeconomic, and geographic groups face different contextual stressors, financial stressors, occupational stressors, discrimination, and assimilation stressors than their non-diverse counterparts, and these also accumulate with age [12, 30, 64]. There is evidence that changes in the inflammatory capacity of diet can have an effect on telomere length, an important indicator of aging [65], and this effect is seen over a period as short as one year in older, apparently healthy women [66].
SES plays an important role in determining levels of risk factors known to influence aging such as diet [57], physical activity [67], and residential location [68] (with all that it implies in terms of environmental exposures and educational opportunity). We know that chronic stress, inflammation, poor diet, sedentary lifestyle, and the demographic factors that fuel these conditions are primary predictors of chronic disease [14, 60].
Education level, SES, occupation level, and geographical location often determine the amount of control individuals have over their ability to pursue positive self-care practices and, in turn, mediate most of this variability [15]. We speculate that by addressing these topics we may be able to increase DFLE and HRQoL across populations.
Chronic stress: who is most susceptible?
Stress links to decrements in DFLE and HRQoL and increases in chronic disease risk both directly (biologically) and indirectly (via bio-behavioral risk factors such as poor diet, physical inactivity, depression) [14]. Individuals who are in lower-status positions also tend to suffer greater stress due to low-control occupations and neighborhood disorder and dysfunction [14]. It is important to recognize that the type of stress that is being referred to as having negative health outcomes is chronic in nature, or repeated, habitual occurrences of stress in day-to-day life [69]. These stresses accumulate as one ages, resulting in increased allostatic load and both premature aging and greater disability and decreasing HRQoL with age [70]. It is the chronicity of stress that is so harmful to optimal mental health and biological functioning—and it clearly can accumulate over age, with extremely deleterious consequences with respect to disability [71].
SES and associated financial resources play a role in mediating stress in most individuals’ lifestyles; however, those who occupy lower positions on the social gradient are faced with particularly harsh effects of low SES. In most societies, lower income dictates the quality of food individuals can buy for themselves and their families, where they can live, the stress they are under to provide financial support for themselves and their families, their feelings of self-esteem and worth, their education, their access to medication and general healthcare, and their overall autonomy in society [14]. The numerous factors that are limited by income can further cause long-term problems, as from a habitually poor diet that can lead to inflammation, obesity, and compromised mental health, all of which degrade HRQoL and have been shown to be risk factors for chronic disease [16]. Children who grow up in socioeconomically disadvantaged or abusive households are exposed to chronic stress that can follow them throughout life in many ways, including their microbiome, disordered eating behaviors and obesity [19], and their mental health [72]. The psychosocial and biological effects of living in a socioeconomically disadvantaged household can actually manifest quickly and very early in life [15]. Epigenetic imprinting also may help to ensure that these ill effects may persist across generations [73]. Unfortunately, this is an area that also is affected by racial disparities, as we see adverse events such as abuse and maltreatment occurring in much higher frequencies among Black and Hispanic children in the U.S. when compared to their non-Hispanic White peers [19].
The Whitehall II study, which looked closely at the employment gradient within the social gradient, showed that 51% of the social gradient in CHD could be eliminated by reducing the likelihood of metabolic syndrome and improvements in self-controlled behavioral variables [16]. Furthermore, 50% of the risk for CHD based on the social gradient is explained by dietary and other behavior choices that one has the autonomy to make; however, when an individual occupies a lower position on the SES gradient, their autonomy to make those conscious decisions often is constrained. As Michael Marmot states, ‘it is not what a person has that is important, it is what he or she can do with what he or she has’ [11]. Ultimately, those who are lower on the social gradient do not always have the opportunity to consume an anti-inflammatory diet (or even know what that means), get sufficient sleep on a regular schedule, participate in a job which has personal meaning and purpose, or have control over other aspects of their life. Low levels of control have been proven to be strongly associated with poorer physical and mental health outcomes [11, 15]. In addition, psychosocial stressors that may be unique to those lower on the social gradient and those belonging to specific racial and ethnic groups are things such as perceived racism, discrimination, and access to health protecting resources.
Chronic stress: biological and behavioral pathways
Stress can have both direct and indirect relationship with disease. In phase 5 of the Whitehall II study, both men and women were more likely to suffer from metabolic syndrome if they occupied the lower ends of the social or occupational gradient [16]. The stress associated with these low-grade occupations is often manifested as chronic stress and has been categorized into either 0, 1, 2, or \(\ge\) 3 exposures for the purpose of this study. Of those who reported presence of chronic occupational stress (defined as \(\ge\) 3 exposures of feeling isolated or chronically stressed > 75% of the time while at work during a 14-year reporting period), men were almost two times as likely to develop metabolic syndrome and women were over five times as likely to develop metabolic syndrome. In addition to developing metabolic syndrome, the study showed that prolonged exposures to work stress can cause disruptions in the activities of the autonomic nervous and neuroendocrine systems [74]. Additionally, chronic psychosocial stress has been linked to disturbances in immune function, often prolonging healing and increasing risk of infection, and disturbing overall homeostasis [75, 76]. Altered adrenocortical and hypothalamic–pituitary–adrenal axis function is accompanied by its own assortment of metabolic dysfunctions [11]. Chronic stress is known to promote oxidative stress, which activates the NF-\(\kappa\) B pathway, and can boost pro-inflammatory cytokine and adipokine production, even in the absence of illness or injury-related inflammation [75, 77,78,79].
Fundamentally, sustained amounts of stress have the power to disturb the homeostatic baselines of the metabolic, immune, cardiovascular, and endocrine systems by way of altering biologically set points. This puts extra physiological stress on the body, which can produce unfavorable long-term effects, thereby increasing an individual’s risk for decreasing HRQoL and developing chronic disease [15].
Aside from the direct effects that stress can have in modulating metabolic pathways, even more common are its effects on mental health and dietary patterns. Both quantitative and qualitative data show that heightened stress levels drive unhealthier food choices [75, 77, 78]. In one study performed on Chinese college students, elevated levels of stress and depression while in school led to students incorporating few or no fruits and vegetables into their diet and displayed increased unhealthy snacking. Similar studies performed on students in Germany, Poland, and Bulgaria, have produced similar results, with stronger effects seen in females compared to males [80]. A poor, i.e., pro-inflammatory, diet will not only affect many biological markers of health such as BMI, cholesterol, and blood pressure but it also will alter day-to-day mood, energy level, composition of the microbiota and microbiome, and the potential for developing depression [14].
Inflammation causes biological as well as mental upset: diet, the microbiome, and the gut–brain axis
Diet affects important determinants of health, including weight [81], BMI and adiposity [82], serum lipids [83, 84], and cytokines [48, 85] that, in turn, determine levels of systemic inflammation. While focusing on the role of specific nutrients on physical health outcomes, we often fail to recognize the effect that diet can have on mood and overall mental health. Consumption of a pro-inflammatory diet leads to the release of cytokines such as interleukin-6 and C-reactive protein which can contribute to increased CNS inflammation [48]. Inflammatory markers also have been shown to hinder the action of some neurotransmitters such as dopamine and serotonin, both of which play a crucial role in modulating mood [86]. Higher circulating levels of cytokines have been shown to play a role in inducing some forms of depression or depressive symptoms [48], which have profound effects on mental, emotional, and social functioning crucial in determining HRQoL [2, 21]. According to the National Health and Nutrition Examination Survey, as many as a third of patients who are clinically depressed have elevated levels of inflammatory biomarkers [87]. Inflammation caused by increased levels of inflammatory biomarkers is expressed as a myriad of symptoms including, but not limited to, negative mood, fatigue, and increased pain sensitivity [48]. These problems may be more acute among the elderly, especially those who are frail and who have low levels of physical activity and, therefore, consume relatively few calories. In this group, very low levels of total food intake and low energy flux increase the likelihood micronutrient deficiencies [88]. Inevitably, these nutrient deficiencies are associated with increased diet-associated inflammation [89] and, with that, increased “inflammaging” [90].
While a poor diet or another physical stressor can lead to higher production of pro-inflammatory cytokines which can, in turn, trigger these many depressive symptoms [48, 91], we see contextual and psychosocial stressors having a similar effect [13]. Not only do factors such as low SES, shift work, and racial discrimination have the power to directly affect dietary choices and thereby influence systemic inflammation, but the stresses associated with these factors have themselves been shown to directly cause inflammation [14, 48]. Regardless of the form of stress, physical or mental, significant damage can be inflicted on the composition of the microbiota [92]. Imbalances within the microbiota also have been linked to obesity and depression [48].
Conclusion
This paper emphasizes that using DFLE and HLE to expand the understanding of HRQoL can transform the way in which we evaluate population health and both length and quality of life. Research conducted over the past several decades makes clear that we must take into account the full range of risk factors that affect DFLE and HRQoL. While diet and stress have each been strongly linked to higher levels of chronic systemic inflammation (which, in turn, put an individual at elevated risk for developing various chronic diseases), it is the complex blend of numerous factors that determines the overall health of an individual. Chronic, systemic inflammation and its root causes in chronic stress, poor diet, physical inactivity, low SES, racial discrimination, and insufficient education all intersect to increase disease risk and disability, thus detracting from HRQoL. Meaningful intervention on these factors—not only on an individual level but at the community and organizational level—using evidence-based implementation science practices with an emphasis on addressing social determinants of health and health equity—would contribute toward lowering the incidence of chronic disease and produce a rightward shift in the disability curve. If a shift were to occur, HRQoL would improve and we would expect to see a decrease in healthcare spending by mitigating the care that individuals require during their lifespan, and especially at the end of life. Doing so also would aid in clinical decision making as HRQoL is a concept to which practitioners can relate when attempting to influence patient outcomes [93].
Abbreviations
- CHD:
-
Coronary heart disease
- DFLE:
-
Disability-free life expectancy
- HRQoL:
-
Health-related quality of life
- HLE:
-
Healthy life expectancy
- IMR:
-
Infant mortality rate
- QALE:
-
Quality-adjusted life expectancy
- SES:
-
Socioeconomic status
References
Rosenkrantz, B. (1972). Public health and the state: Changing views in Massachusetts, 1842–1936. Harvard University.
Love-Koh, J., Asaria, M., Cookson, R., & Griffin, S. (2015). The social distribution of health: estimating quality-adjusted life expectancy in England. Value Health, 18(5), 655–662.
Modig, K., Drefahl, S., & Ahlbom, A. (2013). Limitless longevity: Comment on the Contribution of rectangularization to the secular increase of life expectancy. International Journal of Epidemiology, 42(3), 914–916.
Chirinda, W., & Chen, H. (2017). Comparative study of disability-free life expectancy across six low- and middle-income countries. Geriatrics & Gerontology International, 17(4), 637–644.
Roser, M., Ortiz-Ospina, E., Ritchi, H. (2020) “Life Expectancy”. Retrieved from: https://ourworldindata.org/life-expectancy [Online Resource]. Oxford, UK: University of Oxford.
Schalkwijk, F. H., Koopman, J. J., Ghariq, E., de Beer, J. A., van Bodegom, D., & Westendorp, R. G. (2016). Disentangling rectangularization and life span extension with the moving rectangle method. Annals of Epidemiology, 26(3), 218-221.e212.
de Beer, J., & Janssen, F. (2016). A new parametric model to assess delay and compression of mortality. Population Health Metrics, 14, 46.
Leigh, J. P., & Fries, J. F. (1994). Education, gender, and the compression of morbidity. International Journal of Aging and Human Development, 39(3), 233–246.
Sudore, R. L., Karter, A. J., Huang, E. S., et al. (2012). Symptom burden of adults with type 2 diabetes across the disease course: Diabetes & aging study. Journal of General Internal Medicine, 27(12), 1674–1681.
Crimmins, E. M., Zhang, Y., & Saito, Y. (2016). Trends over 4 decades in disability-free life expectancy in the United States. American Journal of Public Health, 106(7), 1287–1293.
Marmot, M. G. (2006). Status syndrome: A challenge to medicine. JAMA, 295(11), 1304–1307.
Saban, K. L., Mathews, H. L., DeVon, H. A., & Janusek, L. W. (2014). Epigenetics and social context: Implications for disparity in cardiovascular disease. Aging and Disease, 5(5), 346–355.
Lehnert, T., Sonntag, D., Konnopka, A., Riedel-Heller, S., & Konig, H. H. (2013). Economic costs of overweight and obesity. Best Practice & Research Clinical Endocrinology & Metabolism, 27(2), 105–115.
Hebert, J. R., Braun, K. L., Kaholokula, J. K., Armstead, C. A., Burch, J. B., & Thompson, B. (2015). Considering the role of stress in populations of high-risk, underserved Community Networks Program Centers. Progress in Community Health Partnerships, 9(Suppl), 71–82.
Adler, N. E., & Rehkopf, D. H. (2008). U.S. disparities in health: descriptions, causes, and mechanisms [Review] [108 refs]. Annual Review of Public Health, 29, 235–252.
Marmot, M., Shipley, M., Hemingway, H., Head, J., & Brunner, E. (2008). Biological and behavioural explanations of social inequalities in coronary heart disease: The Whitehall II study. Diabetologia, 51(11), 1980–1988.
Assmann, K. E., Adjibade, M., Shivappa, N., et al. (2018). The inflammatory potential of the diet at midlife is associated with later healthy aging in French adults. Journal of Nutrition, 148(3), 437–444.
Hasson, B. R., Apovian, C., & Istfan, N. (2015). Racial/ethnic differences in insulin resistance and beta cell function: relationship to racial disparities in type 2 diabetes among African Americans versus Caucasians. Current Obesity Reports, 4(2), 241–249.
Haughton, C. F., Wang, M. L., & Lemon, S. C. (2016). Racial/ethnic disparities in meeting 5-2-1-0 recommendations among children and adolescents in the United States. Journal of Pediatrics, 175(188–194), e181.
United States Census Bureau. (2011). Life expectancy trends in the United States: Table 102. Expectation of life at birth, 1970 to 2007, and projections, 2010 to 2020. United States Census Bureau.
Dijkstra, A., Hakverdioglu, G., Muszalik, M., Andela, R., Korhan, E. A., & Kedziora-Kornatowska, K. (2015). Health related quality of life and care dependency among elderly hospital patients: an international comparison. Tohoku Journal of Experimental Medicine, 235(3), 193–200.
WHOQOL Group. (1993). Study protocol for the World Health Organization project to develop a Quality of Life assessment instrument (WHOQOL). Quality of life Research, 2(2), 153–159.
Berge, J. M., Fertig, A., Tate, A., Trofholz, A., & Neumark-Sztainer, D. (2018). Who is meeting the Healthy People 2020 objectives? Comparisons between racially/ethnically diverse and immigrant children and adults. Families, Systems, & Health, 36(4), 451–470.
Pronk, N., Kleinman, D. V., Goekler, S. F., Ochiai, E., Blakey, C., & Brewer, K. H. (2020). Promoting health and well-being in healthy people 2030. Journal of Public Health Management and Practice. https://doi.org/10.1097/phh.0000000000001254
Saha, S., Cohen, B. B., Nagy, J., Mc, P. M., & Phillips, R. (2020). Well-being in the nation: a living library of measures to drive multi-sector population health improvement and address social determinants. Milbank Quarterly, 98(3), 641–663.
Tsiros, M. D., Tian, E. J., Shultz, S. P., et al. (2020). Obesity, the new childhood disability? An umbrella review on the association between adiposity and physical function. Obesity Reviews, 21(12), e13121.
Barazzoni, R., Bischoff, S. C., Breda, J., et al. (2020). ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clinical Nutrition, 39(6), 1631–1638.
Weyant, C., Brandeau, M. L., & Basu, S. (2019). Personalizing medical treatment decisions: Integrating meta-analytic treatment comparisons with patient-specific risks and preferences. Medical Decision Making, 39(8), 998–1009.
Robbins, A. S., Siegel, R. L., & Jemal, A. (2012). Racial disparities in stage-specific colorectal cancer mortality rates from 1985 to 2008. Journal of Clinical Oncology, 30(4), 401–405.
Das, A. (2013). How does race get “under the skin”? Inflammation, weathering, and metabolic problems in late life. Social Science and Medicine, 77, 75–83.
Siegel, R. L., Miller, K. D., & Jemal, A. (2020). Cancer statistics, 2018. CA: A Cancer Journal for Clinicians, 70(1), 7–30.
Cai, J., Coyte, P. C., & Zhao, H. (2017). Decomposing the causes of socioeconomic-related health inequality among urban and rural populations in China: A new decomposition approach. International Journal for Equity in Health, 16(1), 128.
An, R. (2015). Educational disparity in obesity among U.S. adults, 1984–2013. Annals of Epidemiology, 25(9), 637–642.
Huda, T. M., Hayes, A., & Dibley, M. J. (2018). Examining horizontal inequity and social determinants of inequality in facility delivery services in three South Asian countries. Journal of Global Health, 8(1), 010416.
Abiri, B., & Vafa, M. (2020). The role of nutrition in attenuating age-related skeletal muscle atrophy. Advances in Experimental Medicine and Biology, 1260, 297–318.
Centers for Disease Control and Prevention. (2017). Health expenditures. Retrieved February 11, 2019 from https://www.cdc.gov/nchs/fastats/health-expenditures.htm.
Tandon, A., Murray, C. J. L., Lauer, J. A., & Evans, D. B. (2018). Measuring overall health system performance for 191 countries. World Health Organization.
Aldridge, M. D., & Kelley, A. S. (2015). The myth regarding the high cost of end-of-life care. American Journal of Public Health, 105(12), 2411–2415.
Le, Q. A., Doctor, J. N., Zoellner, L. A., & Feeny, N. C. (2018). Effects of treatment, choice, and preference on health-related quality-of-life outcomes in patients with posttraumatic stress disorder (PTSD). Quality of Life Research, 27(6), 1555–1562.
Rezaei, S., Hajizadeh, M., Khosravipour, M., Khosravi, F., & Rezaeian, S. (2018). Socioeconomic inequalities in poor health-related quality of Life in Kermanshah, Western Iran: A decomposition analysis. Journal of Research in Health Sciences, 18(1), e00405.
Tajvar, M., Arab, M., & Montazeri, A. (2008). Determinants of health-related quality of life in elderly in Tehran, Iran. BMC Public Health, 8(1), 323.
Tomata, Y., Shivappa, N., Zhang, S., et al. (2018). Dietary inflammatory index and disability-free survival in community-dwelling older adults. Nutrients, 10(12), E1896.
Dankel, S. J., Loenneke, J. P., & Loprinzi, P. D. (2016). Physical activity and diet on quality of life and mortality: The importance of meeting one specific or both behaviors. International Journal of Cardiology, 202, 328–330.
Care Diabetes. (2018). Economic costs of diabetes in the U.S. in 2017. Diabetes Care, 41(5), 917–928.
Freedman, V. A., Wolf, D. A., & Spillman, B. C. (2016). Disability-free life expectancy over 30 years: a growing female disadvantage in the US population. American Journal of Public Health, 106(6), 1079–1085.
World Health Organization. (1984). The uses of epidemiology in the study of the elderly. Report of a WHO Scientific Group on the Epidemiology of Aging. World Health Organization Technical Report Series, 706, 1–84.
McKeown, R. E. (2009). The epidemiologic transition: Changing patterns of mortality and population dynamics. American Journal of Lifestyle Medicine, 3(1 Suppl), 19S-26S.
Kiecolt-Glaser, J. K., Derry, H. M., & Fagundes, C. P. (2015). Inflammation: Depression fans the flames and feasts on the heat. American Journal of Psychiatry, 172(11), 1075–1091.
Pont, S. J., Puhl, R., Cook, S. R., Slusser, W., & Section on Obesity and the Obesity Society. (2017). Stigma experienced by children and adolescents with obesity. Pediatrics, 140(6), e20173034.
Friel, S., Marmot, M., McMichael, A. J., Kjellstrom, T., & Vagero, D. (2008). Global health equity and climate stabilisation: A common agenda. Lancet, 372(9650), 1677–1683.
Crimmins, E. M., Hayward, M. D., Hagedorn, A., Saito, Y., & Brouard, N. (2009). Change in disability-free life expectancy for Americans 70 years old and older. Demography, 46(3), 627–646.
Mathers, C. D., & Loncar, D. (2006). Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine/Public Library of Science, 3(11), e442.
Murray, C. J., Vos, T., Lozano, R., et al. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010.[Erratum appears in Lancet. 2013 Feb 23;381(9867):628 Note: AlMazroa, Mohammad A [added]; Memish, Ziad A [added]]. Lancet, 380(9859), 2197–2223.
Vos, T., Flaxman, A. D., Naghavi, M., et al. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010.[Erratum appears in Lancet. 2013 Feb 23;381(9867):628 Note: AlMazroa, Mohammad A [added]; Memish, Ziad A [added]]. Lancet, 380(9859), 2163–2196.
Garcia-Arellano, A., Martinez-Gonzalez, M. A., Ramallal, R., et al. (2019). Dietary inflammatory index and all-cause mortality in large cohorts: The SUN and PREDIMED studies. Clinical Nutrition, 38(3), 1221–1231.
Phillips, C. M., Chen, L. W., Heude, B., et al. (2019). Dietary inflammatory index and non-communicable disease risk: A narrative review. Nutrients, 11(8), E1873.
Dubowitz, T., Heron, M., Basurto-Davila, R., Bird, C. E., Lurie, N., & Escarce, J. J. (2011). Racial/ethnic differences in US health behaviors: A decomposition analysis. American Journal of Health Behavior, 35(3), 290–304.
Martinez, D. J., Turner, M. M., Pratt-Chapman, M., et al. (2016). The effect of changes in health beliefs among African-American and rural white church congregants enrolled in an obesity intervention: A qualitative evaluation. Journal of Community Health, 41(3), 518–525.
Devitt, M. (2020). CDC data show US life expectancy continues to decline. American Academy of family physicians (AAFP).
McEwen, B. S. (1998). Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences, 840, 33–44.
Pearce, N., Susser, M., & Boffetta, P. (1997). Social inequalities and cancer. IARC Scientific Publications, 138, 1–15.
Hayden, K. M., Beavers, D. P., Steck, S. E., et al. (2017). The association between an inflammatory diet and global cognitive function and incident dementia in older women: The Women’s Health Initiative Memory Study. Alzheimer’s & Dementia, 13(11), 1187–1196.
Gary-Webb, T. L., Suglia, S. F., & Tehranifar, P. (2013). Social epidemiology of diabetes and associated conditions. Current Diabetes Reports, 13(6), 850–859.
Watkins, D. C. (2012). Depression over the adult life course for African American men: Toward a framework for research and practice. American Journal of Men’s Health, 6(3), 194–210.
Garcia-Calzon, S., Zalba, G., Ruiz-Canela, M., et al. (2015). Dietary inflammatory index and telomere length in subjects with a high cardiovascular disease risk from the PREDIMED-NAVARRA study: Cross-sectional and longitudinal analyses over 5 y. American Journal of Clinical Nutrition, 102(4), 897–904.
Puterman, E., Lin, J., Krauss, J., Blackburn, E. H., & Epel, E. S. (2015). Determinants of telomere attrition over 1 year in healthy older women: Stress and health behaviors matter. Molecular Psychiatry, 20(4), 529–535.
McAlexander, K. M., Banda, J. A., McAlexander, J. W., & Lee, R. E. (2009). Physical activity resource attributes and obesity in low-income African Americans. Journal of Urban Health, 86(5), 696–707.
Liao, Y., Bang, D., Cosgrove, S., et al. (2011). Surveillance of health status in minority communities—Racial and Ethnic Approaches to Community Health Across the U.S. (REACH U.S.) Risk Factor Survey, United States, 2009. Morbidity and Mortality Weekly Report. Surveillance Summaries., 60(6), 1–44.
Jackson, J. S., Knight, K. M., & Rafferty, J. A. (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100(5), 933–939.
McEwen, B. S. (2004). Protection and damage from acute and chronic stress: Allostasis and allostatic overload and relevance to the pathophysiology of psychiatric disorders. Annals of the New York Academy of Sciences, 1032, 1–7.
Laditka, J. N., & Laditka, S. B. (2016). Unemployment, disability and life expectancy in the United States: A life course study. Disability and Health Journal, 9(1), 46–53.
Goff, P. A., Jackson, M. C., Di Leone, B. A., Culotta, C. M., & DiTomasso, N. A. (2014). The essence of innocence: Consequences of dehumanizing Black children. Journal of Personality and Social Psychology, 106(4), 526–545.
Simons, R. L., Lei, M. K., Beach, S. R., et al. (2016). Economic hardship and biological weathering: The epigenetics of aging in a U.S. sample of black women. Social Science & Medicine, 150, 192–200.
Chandola, T., Brunner, E., & Marmot, M. (2006). Chronic stress at work and the metabolic syndrome: Prospective study. BMJ: British Medical Journal, 332(7540), 521–525.
Kiecolt-Glaser, J. K. (2010). Stress, food, and inflammation: Psychoneuroimmunology and nutrition at the cutting edge. Psychosomatic Medicine, 72(4), 365–369.
McEwen, B. S. (1998). Stress, adaptation, and disease. In S. M. McCann, E. M. Sternberg, J. M. Lipton, G. P. Chrousos, P. W. Gold, & C. C. Smith (Eds.), Neuroimmunomodulation: Molecular aspects, integrative systems, and clinical advances (pp. 33–44). The New York Academy of Sciences.
Adam, T. C., & Epel, E. S. (2007). Stress, eating and the reward system. Physiology & Behavior, 91(4), 449–458.
Wardle, J., Steptoe, A., Oliver, G., & Lipsey, Z. (2000). Stress, dietary restraint and food intake. Journal of Psychosomatic Research, 48(2), 195–202.
Kiecolt-Glaser, J. K., McGuire, L., Robles, T. F., & Glaser, R. (2002). Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology, 53, 83–107.
Liu, C., Xie, B., Chou, C. P., et al. (2007). Perceived stress, depression and food consumption frequency in the college students of China Seven Cities. Physiology & Behavior, 92(4), 748–754.
Munsters, M. J., & Saris, W. H. (2014). Body weight regulation and obesity: Dietary strategies to improve the metabolic profile. Annual Review of Food Science & Technology, 5, 39–51.
Caracciolo, B., Xu, W., Collins, S., & Fratiglioni, L. (2014). Cognitive decline, dietary factors and gut-brain interactions. Mechanisms of Ageing and Development, 136–137, 59–69.
Lee, D., Hwang, W., Artan, M., Jeong, D. E., & Lee, S. J. (2015). Effects of nutritional components on aging. Aging Cell, 14(1), 8–16.
Volek, J. S., Fernandez, M. L., Feinman, R. D., & Phinney, S. D. (2008). Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Progress in Lipid Research, 47(5), 307–318.
Shivappa, N., Godos, J., Hebert, J. R., et al. (2018). Dietary inflammatory index and cardiovascular risk and mortality—A meta-analysis. Nutrients, 10(2), E200.
Gidron, Y., & Ronson, A. (2008). Psychosocial factors, biological mediators, and cancer prognosis: A new look at an old story. Current Opinion in Oncology, 20(4), 386–392.
Raison, C. L., & Miller, A. H. (2011). Is depression an inflammatory disorder? Current Psychiatry Reports, 13(6), 467–475.
Rarick, K. R., Pikosky, M. A., Grediagin, A., et al. (2007). Energy flux, more so than energy balance, protein intake, or fitness level, influences insulin-like growth factor-I system responses during 7 days of increased physical activity. Journal of Applied Physiology, 103(5), 1613–1621.
Hebert, J. R., Shivappa, N., Wirth, M. D., Hussey, J. R., & Hurley, T. G. (2019). Perspective: The Dietary Inflammatory Index (DII®): Lessons learned, improvements made and future directions. Advances in Nutrition, 10(2), 185–195.
SzarcvelSzic, K., Declerck, K., Vidakovic, M., & VandenBerghe, W. (2015). From inflammaging to healthy aging by dietary lifestyle choices: Is epigenetics the key to personalized nutrition? Clinical Epigenetics, 7(1), 33.
Shivappa, N., Hebert, J. R., Veronese, N., et al. (2018). The relationship between the Dietary Inflammatory Index (DII®) and incident depressive symptoms: A longitudinal cohort study. Journal of Affective Disorders, 235, 39–44.
Hofseth, L. J., Hebert, J. R., Chanda, A., et al. (2020). Early-onset colorectal cancer: Initial clues and current views. Nature Reviews Gastroenterology & Hepatology, 17(6), 352–364.
Wilson, I. B., & Cleary, P. D. (1995). Linking clinical variables with health-related quality of life: A conceptual model of patient outcomes. JAMA, 273(1), 59–65.
Acknowledgements
All authors (AEG, DBF, JRH) have read and approved of this submitted version of the manuscript.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Galvin, A.E., Friedman, D.B. & Hébert, J.R. Focus on disability-free life expectancy: implications for health-related quality of life. Qual Life Res 30, 2187–2195 (2021). https://doi.org/10.1007/s11136-021-02809-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-021-02809-1