Abstract
Purpose
Health related quality of life (HRQoL) is rarely routinely measured in the clinical setting. In the absence of patient reported data, clinicians rely on proxy and informal estimates to support clinical decisions. This study compares clinician estimates (proxy) with patient reported HRQoL in patients with advanced heart failure and examines factors influencing discrepancies.
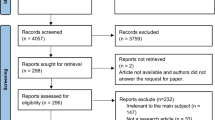
Methods
Seventy-five patients with heart failure, (22 females, 53 males) completed the EQ-5D-5L questionnaire. Thirty-nine clinicians (11 medical, 23 nursing, 5 allied health) completed the proxy version (V1) producing 194 dyads. Correlation was assessed using Spearman’s rank tests, systematic bias was examined with Bland–Altman analyses. Inter-rater agreement at the domain level, was investigated using linear weighted Kappa statistics while factors influencing the IRG were explored using independent student t-tests, analysis of variance and regression.
Results
There was a moderate positive correlation between clinician HRQoL estimates and patient reported utility (r = 0.38; p < .0005). Mean clinician estimates were higher than patient reported utility (0.60 vs 0.54; p = 0.008), with significant underestimation of reported problems apparent in three of the five EQ-5D-5L domains. Patient sex (female), depressed mood and frailty were all associated with an increased inter-rater gap.
Conclusion
Clinicians in this sample overestimated HRQoL. Factors affecting the inter-rater gap, including sex and depression, support formal HRQoL screening to enhance clinical conversations and decision making. The discrepancy also supports regulatory restriction on the use of expert opinion in the development of QALYs in health economic analysis.


Similar content being viewed by others
References
Ishaque, S., Karnon, J., Chen, G., Nair, R., & Salter, A. B. (2019). A systematic review of randomised controlled trials evaluating the use of patient-reported outcome measures (PROMs). Quality of Life Research, 28(3), 567–592.
Cavanagh, C. E. (2019). Quality of life in heart failure: Screening alone is insufficient. European Heart Journal - Quality of Care and Clinical Outcomes, 5(3), 191–192.
Rand, S., & Caiels, J. (2020). Using proxies to assess quality of life: A review of the issues and challenges. Discussion Paper. University of Kent; 2015. Retrieved May 22, 2020, from https://www.pssru.ac.uk/pub/4980.pdf.
Arora, J., & Tavella, R. (2020). Implementing ICHOM’s standard sets of outcomes: Coronary artery disease in the coronary angiogram database of South Australia (CADOSA). International Consortium for Health Outcomes Measurement (ICHOM), 2017. Retrieved May 22, 2020 from https://www.ichom.org/wp-content/uploads/2013/10/CADOSA-Case-Study-Draft-vF_Jan17.pdf.
Foster, A., Croot, L., Brazier, J., Harris, J., & O’Cathain, A. (2018). The facilitators and barriers to implementing patient reported outcome measures in organisations delivering health related services: A systematic review of reviews. Journal of Patient-Reported Outcomes, 2, 46.
Philpot, L. M., Barnes, S. A., Brown, R. M., Austin, J. A., James, C. S., Stanford, R. H., et al. (2018). Barriers and benefits to the use of patient-reported outcome measures in routine clinical care: A qualitative study. American Journal of Medical Quality, 33(4), 359–364.
Nelson, E. C., Eftimovska, E., Lind, C., Hager, A., Wasson, J. H., & Lindblad, S. (2015). Patient reported outcome measures in practice. BMJ, 350, g7818.
Kim, D. H. (2018). Incorporating quality of life prediction in shared decision making about transcatheter aortic valve replacement. Circulation: Cardiovascular Quality and Outcomes, 11(10), e005097.
Pickard, A. S., & Knight, S. J. (2005). Proxy evaluation of health-related quality of life: A conceptual framework for understanding multiple proxy perspectives. Medical Care, 43(5), 493–499.
Robertson, S., Cooper, C., Hoe, J., Hamilton, O., Stringer, A., & Livingston, G. (2017). Proxy rated quality of life of care home residents with dementia: A systematic review. International Psychogeriatrics, 29(4), 569–581.
Coucill, W. B., Bentham, S., Buckley, P., & Laight, A. (2001). EQ-5D in patients with dementia. An investigation of interrater agreement. Medical Care, 39(8), 760–777.
Devine, A., Taylor, S. J., Spencer, A., Diaz-Ordaz, K., Eldridge, S., & Underwood, M. (2014). The agreement between proxy and self-completed EQ-5D for care home residents was better for index scores than individual domains. Journal of Clinical Epidemiology, 67(9), 1035–1043.
Schmidt, S., Power, M., Green, A., Lucas-Carrasco, R., Eser, E., Dragomirecka, E., et al. (2010). Self and proxy rating of quality of life in adults with intellectual disabilities: Results from the DISQOL study. Research in Developmental Disabilities, 31(5), 1015–1026.
Simoes, C., & Santos, S. (2016). The quality of life perceptions of people with intellectual disability and their proxies. Journal of Intellectual & Developmental Disability, 41(4), 311–323.
Roydhouse, J. K., Gutman, R., Keating, N. L., Mor, V., & Wilson, I. B. (2018). Proxy and patient reports of health-related quality of life in a national cancer survey. Health and Quality of Life Outcomes, 16(1), 6.
Kutner, J. S., Bryant, L. L., Beaty, B. L., & Fairclough, D. L. (2006). Symptom distress and quality-of-life assessment at the end of life: The role of proxy response. Journal of Pain and Symptom Management, 32(4), 300–310.
Lv, Essen. (2009). Proxy ratings of patient quality of life factors related to patient–proxy agreement. Acta Oncologica, 43(3), 229–234.
Ponikowski, P., Voors, A. A., Anker, S. D., Bueno, H., Cleland, J. G. F., Coats, A. J. S., et al. (2016). 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal, 37(27), 2129–2200.
Vitale, C., Spoletini, I., & Rosano, G. M. (2018). Frailty in heart failure: Implications for management. Cardiac Failure Review, 4(2), 104–106.
Thombs, B. D., De Jonge, P., Coyne, J. C., Whooley, M. A., Frasure-Smith, N., Mitchell, A. J., et al. (2008). Depression screening and patient outcomes in cardiovascular care. JAMA, 300(18), 2161–2171.
Hoekstra, T., Jaarsma, T., van Veldhuisen, D. J., Hillege, H. L., Sanderman, R., & Lesman-Leegte, I. (2013). Quality of life and survival in patients with heart failure. European Journal of Heart Failure, 15(1), 94–102.
Quinn, C., Dunbar, S. B., & Higgins, M. (2010). Heart failure symptom assessment and management: Can caregivers serve as proxy? Journal of Cardiovascular Nursing, 25(2), 142–148.
Heo, S., Lennie, T. A., Okoli, C., & Moser, D. K. (2009). Quality of life in patients with heart failure: Ask the patients. Heart and Lung, 38(2), 100–108.
Haas, M., & Gonzalez, T. (2014). How oncology studies obtain QALY weights: A literature review. Cancer Research Economics Support Team. Retrieved May 22, 2020, from https://www.uts.edu.au/sites/default/files/2019-04/crest-factsheet-qaly-weights.pdf.
Devlin, N. J., Shah, K. K., Feng, Y., Mulhern, B., & van Hout, B. (2018). Valuing health-related quality of life: An EQ-5D-5L value set for England. Health Economics, 27(1), 7–22.
Payakachat, N., Ali, M. M., & Tilford, J. M. (2015). Can The EQ-5D detect meaningful change? A systematic review. Pharmacoeconomics, 33(11), 1137–1154.
Dyer, M. T. D., & Goldsmith, K. A. (2010). A review of health utilities using the EQ-5D in studies of cardiovascular disease. Health and Quality of Life Outcomes, 8(13), 1–12.
Calvert, M. J., Freemantle, N., & Cleland, J. G. (2005). The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. European Journal of Heart Failure, 7(2), 243–251.
Scuffham, P. A., Whitty, J. A., Mitchell, A., & Viney, R. (2008). The use of QALY weights for QALY calculations. Pharmacoeconomics, 26(4), 297–310.
Norman, R., Cronin, P., & Viney, R. (2013). A pilot discrete choice experiment to explore preferences for EQ-5D-5L health states. Applied Health Economics and Health Policy, 11(3), 287–298.
Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., et al. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699.
Jha, S. R., Hannu, M. K., Chang, S., Montgomery, E., Harkess, M., Wilhelm, K., et al. (2016). The prevalence and prognostic significance of frailty in patients with advanced heart failure referred for heart transplantation. Transplantation, 100(2), 429–436.
Jha, S. R., Hannu, M. K., Gore, K., Chang, S., Newton, P., Wilhelm, K., et al. (2016). Cognitive impairment improves the predictive validity of physical frailty for mortality in patients with advanced heart failure referred for heart transplantation. Journal of Heart and Lung Transplantation, 35(9), 1092–1100.
Ferguson, C. J. (2009). An effect size primer: A guide for clinicians and researchers. Professional Psychology: Research and Practice, 40(5), 532–538.
Shrout, P. E., & Fleiss, J. L. (1979). Intraclass correlations : Uses in assessing rater reliability. Psychological Bulletin, 86(2), 420–428.
Reichenheim, M. E. (2004). Confidence intervals for the kappa statistic. The Stata Journal, 4(4), 421–428.
Greenwood, B. N., Carnahan, S., & Huang, L. (2018). Patient-physician gender concordance and increased mortality among female heart attack patients. Proceedings of the National Academy of Sciences USA, 115(34), 8569–8574.
Tsugawa, Y., Jena, A. B., Figueroa, J. F., Orav, E. J., Blumenthal, D. M., & Jha, A. K. (2017). Comparison of hospital mortality and readmission rates for medicare patients treated by male vs female physicians. JAMA Internal Medicine, 177(2), 206–213.
McClure, N. S., Sayah, F. A., Xie, F., Luo, N., & Johnson, J. A. (2017). Instrument-defined estimates of the minimally important difference for EQ-5D-5L index scores. Value Health, 20(4), 644–650.
Allen, L. A., Stevenson, L. W., Grady, K. L., Goldstein, N. E., Matlock, D. D., Arnold, R. M., et al. (2012). Decision making in advanced heart failure: A scientific statement from the American Heart Association. Circulation, 125(15), 1928–1952.
Thomas, S. A., Wince Chapa, D., Friedmann, E., Durden, C., Ross, A., Lee, M. C. I., et al. (2008). Depression in patients with heart failure: Prevalence, pathophysiological mechanisms, and treatment. Critical Care Nurse, 28(2), 40–55.
Rutledge, T., Reis, V. A., Linke, S. E., Greenberg, B. H., & Mills, P. J. (2006). Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. Journal of the American College of Cardiology, 48(8), 1527–1537.
Yang, X., Lupon, J., Vidan, M. T., Ferguson, C., Gastelurrutia, P., Newton, P. J., et al. (2018). Impact of frailty on mortality and hospitalization in chronic heart failure: A systematic review and meta-analysis. Journal of the American Heart Association, 7(23), e008251.
Carver, C. S., & Scheier, M. F. (2000). Scaling back goals and recalibration of the affect system are processes in normal adaptive self-regulation: Understanding ‘response shift’ phenomena. Social Science and Medicine, 50, 1715–1722.
Aimo, A., Vergaro, G., Barison, A., Maffei, S., Borrelli, C., Morrone, D., et al. (2018). Sex-related differences in chronic heart failure. International Journal of Cardiology, 255, 145–151.
Tadic, M., Cuspidi, C., Plein, S., Belyavskiy, E., Heinzel, F., & Galderisi, M. (2019). Sex and heart failure with preserved ejection fraction: From pathophysiology to clinical studies. Journal of Clinical Medicine, 8(6), 792.
Tsao, C. W., Lyass, A., Enserro, D., Larson, M. G., Ho, J. E., Kizer, J. R., et al. (2018). Temporal trends in the incidence of and mortality associated with heart failure with preserved and reduced ejection fraction. JACC: Heart Failure, 6(8), 678–685.
Lam, C. S. P., Arnott, C., Beale, A. L., Chandramouli, C., Hilfiker-Kleiner, D., Kaye, D. M., et al. (2019). Sex differences in heart failure. European Heart Journal, 40, 3859–3868.
Magnussen, C., Bernhardt, A. M., Ojeda, F. M., Wagner, F. M., Gummert, J., de By, T., et al. (2018). Gender differences and outcomes in left ventricular assist device support: The European Registry for Patients with Mechanical Circulatory Support. Journal of Heart and Lung Transplantation, 37(1), 61–70.
National Institute for Health and Care Excellence. (2020). Guide to the methods of technology appraisal 2013. United Kingdom 2013. Retrieved May 22, 2020, from https://www.nice.org.uk/process/pmg9/chapter/foreword.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Prichard, R.A., Zhao, FL., Mcdonagh, J. et al. Discrepancies between proxy estimates and patient reported, health related, quality of life: minding the gap between patient and clinician perceptions in heart failure. Qual Life Res 30, 1049–1059 (2021). https://doi.org/10.1007/s11136-020-02722-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-020-02722-z